ABSTRACT
Introduction: Vaccines are vital to reducing childhood mortality, and prevent an estimated 2 to 3 million deaths annually which disproportionately occur in the developing world. Overall vaccine coverage is typically used as a metric to evaluate the adequacy of vaccine program performance, though it does not account for untimely administration, which may unnecessarily prolong children's susceptibility to disease. This study explored a hypothesized positive association between increasing vaccine hesitancy and untimeliness of immunizations administered under the Expanded Program on Immunization (EPI) in Addis Ababa, Ethiopia.
Methods: This cross-sectional survey employed a multistage sampling design, randomly selecting one health center within five sub-cities of Addis Ababa. Caregivers of 3 to 12-month-old infants completed a questionnaire on vaccine hesitancy, and their infants' vaccination cards were examined to assess timeliness of received vaccinations.
Results: The sample comprised 350 caregivers. Overall, 82.3% of the surveyed children received all recommended vaccines, although only 55.9% of these vaccinations were timely. Few caregivers (3.4%) reported ever hesitating and 3.7% reported ever refusing a vaccine for their child. Vaccine hesitancy significantly increased the odds of untimely vaccination (AOR 1.94, 95% CI: 1.02, 3.71) in the adjusted analysis.
Conclusions: This study found high vaccine coverage among a sample of 350 young children in Addis Ababa, though only half received all recommended vaccines on time. High vaccine hesitancy was strongly associated with infants' untimely vaccination, indicating that increased efforts to educate community members and providers about vaccines may have a beneficial impact on vaccine timeliness in Addis Ababa.
Introduction
Vaccines are critical in reducing childhood morbidity and mortality, preventing an estimated 2–3 million deaths per year.Citation1 Despite overwhelming evidence that childhood vaccines yield significant health and economic benefits, less than half of children under five are fully vaccinated worldwide.Citation2 Childhood vaccination coverage is particularly low in sub-Saharan Africa, leaving many young children unnecessarily vulnerable to both endemic and epidemic transmission of vaccine-preventable diseases (VPDs).Citation3 Ethiopia suffers from some of the lowest vaccination rates on the continent, leading to an unnecessarily high burden of potentially preventable diseases.Citation4,Citation5 As the second-most populous country in Africa, and one of only two African countries to never be colonized, Ethiopia faces unique public health challenges in addressing low vaccination rates in light of lacking health systems infrastructure.Citation4,Citation6
The 2011 Ethiopian Demographic and Health Survey (DHS) estimated full vaccination coverage to be 24.3% for children 12–23 months of age, and found health service utilization to be significant at the individual level.Citation7 Conversely, access to maternal and child health information, maternal education, and delivery place and community level utilization of antenatal care were significantly associated at the community level.Citation8,Citation9 Full vaccination coverage in Ethiopia improved to 38.5% with the 2016 Ethiopian DHS report, reflective of the Ministry of Health's efforts and investments to reach higher vaccination targets, but nonetheless represents a small fraction of eligible children and is sufficiently low to permit ongoing disease transmission.Citation5 Vaccination coverage is also characterized by dramatic variations across Ethiopia's ethnically distinct and geographically separate regions, with extremely low levels in the Somali regionCitation10 in contrast to improved performance in the OromiaCitation11 and Amhara regions.Citation12,Citation13
The WHO established the Expanded Program on Immunization (EPI) in 1974, and Ethiopia's Ministry of Health launched a country-specific EPI in 1980, which continues to provide government-sponsored vaccines free of charge to children under 5 years of age.Citation4 Their recommended EPI schedule () currently includes 10 antigens, comprising Bacillus Calmette-Guérin (BCG) at birth, polio at birth, 6, 10, and 14 weeks, pentavalent vaccine (containing diphtheria-tetanus-pertussis, Hepatitis B, and Haemophilus Influenza Type B) and pneumococcal conjugate vaccine at 6, 10, and 14 weeks, rotavirus vaccine at 6 and 10 weeks, and measles vaccine at 9 months.Citation4 Despite having a fairly robust EPI compared to the rest of Africa, with additional plans in place to add measles-mumps-rubella vaccine (MMR), meningococcus, Yellow Fever, and Inactivated Polio Vaccine (IPV), Ethiopia's EPI performance fails to achieve coverage levels high enough to interrupt disease transmission.
Table 1. Ethiopian expanded program on immunization vaccination schedule, 2017.
Overall vaccination coverage or levels of vaccination for individual antigens by age group are often utilized to evaluate the effectiveness of an immunization system and population-level susceptibility. However, assessing coverage alone does not provide information on whether vaccines were timely, in accordance with the recommended schedule. The recommended schedule for childhood vaccinations varies from country to country, although WHO provides guidance on age-appropriate vaccination and recommended intervals between doses.Citation14 Failure to adhere to these guidelines places children at higher risk for not receiving all doses for all recommended vaccines, unnecessarily prolonging susceptibility to disease, and undermining herd immunity to VPDs.Citation15-17 More recent studies have provided early evidence that measles vaccination may also have an impact on reducing all-cause mortality, indicating that delayed or missed measles vaccination could have significant consequences beyond just protecting against measles.Citation18 Consequently, timely vaccination is an important complementary measure to standard metrics of vaccine coverage, and provides important indicators in the context of both disease control and population immunity.
Prior research regarding predictors and barriers to vaccine uptake in Ethiopia exists, with maternal education and antenatal care recurring as significant predictors.Citation9,Citation12 However, within Africa there is a dearth of studies examining maternal and caregiver vaccine hesitancy, defined by the WHO Strategic Advisory Group of Experts on Immunization (SAGE) as a continuum of beliefs about vaccines and associated behaviors which range from total refusal of vaccines to total acceptance.Citation19 A systematic review of vaccine hesitancy in low- and middle-income countries generally found a great deal of concern about adverse events following immunization and distrust in health systems.Citation20 Given the challenges of both low vaccination coverage and untimely receipt of vaccines in Ethiopia, it is possible that vaccine hesitancy may contribute to poor immunization outcomes.Citation7,Citation21 The authors are not aware of any previous studies in Africa which assess the association between caregiver vaccine hesitancy and timely vaccination, illustrating an important research gap which should be addressed. As such, this study aims to address this topic by quantifying timeliness, establishing the prevalence of vaccine hesitancy, and examining the impact of vaccine hesitancy on timeliness in Addis Ababa.
Results
Demographics
350 caregivers of children aged 3–12 months were surveyed among five centers in Addis Ababa (, ). All caregivers who were approached agreed to participate in the survey (i.e. no refusals). Of those surveyed children, the majority were from Nifas Silk (37.43%) and Bole (31.71%) sub-cities. The majority of surveyed caregivers were mothers (97.71%) with much smaller numbers of fathers (1.72%) and aunts (0.57%). Most caregivers had some level of educational attainment; 37.28% with an elementary school education, 27.75% high school education, 17.92% college or higher, and the remaining 17.05% had none. The majority of surveyed individuals were Ethiopian Orthodox (72.33%), with 18.16% Muslim and very few Protestants (8.93%) and only 2 Catholics (0.58%). Most children were born in a government hospital (41.26%) or a Health Center (42.41%), with the remaining children born in a private hospital (11.17%), or an NGO facility (2.87%), and a small fraction at home (2.29%). Means of transportation to the health center was predominantly on foot (69.34%), with some driving (30.09%) and very few taking the bus (0.57%).
Figure 1. Map of Addis Ababa with administrative sub-city designations. Highlighted sub-cities (Arada, Gulele, Yeka, Bole, and Nifas Silk) were selected randomly as clusters for analysis.
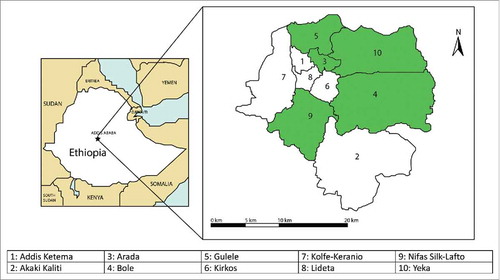
Table 2. Demographic descriptors of caregivers and 3–12-month-old children at 5 health centers in Addis Ababa, Ethiopia, 2017.
Vaccine coverage and timeliness outcomes
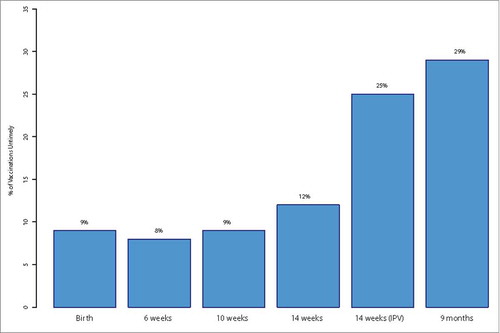
Vaccine coverage was generally high in the study sample (), with 82.32% of children fully immunized excluding measles, and 89.43% fully immunized including measles (restricting the analysis solely to those aged 9–12 months). Percentages for timely administration were not as high; 55.94% of children in the survey sample received all vaccines on time (67.96% of those who were fully immunized), and 50.41% of children were fully immunized when including measles (56.36% of those who were fully immunized). Over time, as children progress later into the immunization schedule, a greater proportion of vaccines were received in an untimely fashion ().
Table 3. Overview of vaccine coverage and timeliness in Addis Ababa, 2017.
Vaccine hesitancy perceptions and behaviors
Almost all caregivers (99.71%) agreed or strongly agreed that “Childhood vaccines are Effective”, “Childhood vaccines are important for my child's health”, and “Getting vaccines is as good way to protect my child from disease”. A large majority (∼97%) of caregivers believed that the information they “received about vaccines from the government vaccine program is reliable and trustworthy”, and that “having my child vaccinated is important for the health of others in the community”. On the whole, caregivers overwhelmingly agreed with the seven ‘positively’-phrased vaccine hesitancy questions (labeled 1–7 in ), which affirmed certain traits of the vaccines, such as their efficacy, importance, benefits to the community, and protective qualities. The three ‘negatively’-phrased questions (labeled 8–10 in ) yielded less uniform responses, with 11.88% agreeing that “My child does not need vaccines for diseases that are no longer common”. Additionally, 24.93% of the surveyed respondents replied “agree” or “strongly agree” that “New vaccines carry more risks than older vaccines” and 25.66% were concerned about serious adverse effects. (). Of the 349 participants who answered the question “Have you ever hesitated getting a vaccine for your child”, only 12 (3.44%) replied “Yes”, and only 13 (3.74%) replied they had ever refused a vaccine for their child. Of those who had hesitated or refused, 85.71% attributed their actions to fear of needles, and 14.29% to concern over side effects.
Figure 3. Overview of responses to SAGE working group vaccine hesitancy questionnaire questions in Addis Ababa, 2017.
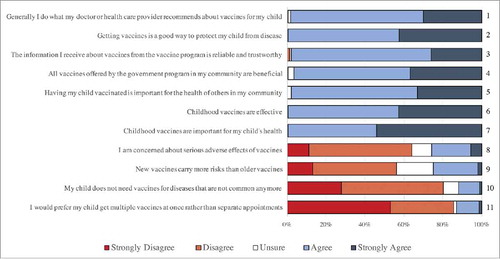
Table 4. Overview of vaccine hesitancy behaviors in Addis Ababa, 2017.
Multivariate model for hesitancy and subsequent timeliness
In the multivariate logistic regression () examining untimely vaccination as the outcome of interest, the most hesitant tertile of vaccine hesitancy led to a significant increase in odds of untimely vaccination (AOR 1.94, 95% CI: 1.02, 3.71). Additionally, Muslim and Protestant religions were both found to be significant predictors of untimely vaccination (AOR 3.01, 95% CI: 1.33, 6.82 and AOR 3.14, 95% CI 1.26, 8.03, respectively) compared to Ethiopian Orthodox religion. For maternal occupation, being a housewife was a significant predictor of untimely vaccination compared to the reference group of day laborers. Delivery place, birth order, and monthly income (dichotomized above and below 3,000 Birr) were not found to be significantly associated with untimely vaccination in the study sample.
Table 5. Multivariate logistic regression for non-timely vaccination vs. timely vaccination based on vaccine hesitancy and other sociodemographic variables in Addis Ababa, 2017.
Discussion
This study found that 82% of children aged 3–12 months had received all their recommended vaccines, though only 56% of children received these vaccines adhering to the recommended schedule, numbers not sufficiently high as to interrupt disease transmission (with the measles requiring upwards of 94% vaccination coverage to interrupt transmission, for example).Citation22 This finding indicates that significant numbers of children in Addis Ababa are receiving their recommended immunizations, but doing so with significant delay. This finding accords with that of recent studies evaluating vaccine timeliness in low- and middle-income countries (LMICs), which have found significant delays in Pakistan, Nepal, and India, and begins to characterize the breadth of the problem of untimely vaccination in LMICs, leaving vulnerable children susceptible to unnecessary, preventable causes of morbidity and mortality.Citation23-25 Additionally, the data revealed that vaccinations become more untimely as the child ages progressively, indicating dropoff from the recommended schedule as the child ages, highlighting the need to maintain adherence to the schedule from birth and promote ongoing health communication regarding the importance of vaccinations for older children.
Ethiopia's full vaccination coverage is persistently low, despite improving from 24.3% to 38.5% between the 2011 and 2016 DHS surveys.Citation5,Citation7 This low coverage is particularly significant in light of the size of Ethiopia's population, over 100 million individuals, with a birth cohort of over three million in 2014.Citation6,Citation26 Studies have not yet assessed the potential additional susceptibility burden that may accompany untimely vaccination in Ethiopia, and the low timeliness estimates derived from this study may be especially difficult to overcome given the immense logistical challenge of employing vaccination services to such a large birth cohort, with minimal health infrastructure. As of 2013, Ethiopia's human development index (HDI) score was 0.435, ranking it 173rd out of 187 countries and territories.Citation27
Additionally, beyond developmental and access-related factors, there may be attitudinal and perceptual factors which influence certain elements of vaccine uptake and timeliness. While the concept of vaccine hesitancy is fairly nascent, with the SAGE Working Group's scale for quantifying vaccine hesitancyCitation19 just formulated in 2015, understanding the attitudes and perceptions that contribute to vaccine acceptance is a necessary component of understanding the full picture of untimely vaccination outcomes in LMICs. Vaccine hesitancy was independently identified as a predictor of untimely vaccination in this study sample, providing an important insight as to one of the factors which may contribute to untimely immunization in Addis Ababa, and one of the first studies to examine the role of vaccine hesitancy in the context of actual vaccination outcomes.
Little research has been done regarding the potential role of vaccine hesitancy in vaccination outcomes in LMICs. Our study's finding that caregivers among the highest tertile of vaccine hesitancy had significantly increased odds of untimely vaccination sets the stage for future, more rigorous studies to confirm this finding in other settings and broaden the scope of literature investigating the consequences of vaccine hesitancy. Two studies in Nigeria have examined how perceptions of vaccinations may impact vaccine receipt. Nigeria is similarly positioned to Ethiopia in terms of vaccination uptake, maintaining 25% full vaccination coverage in 2013.Citation28 The first Nigerian study found that vaccine hesitancy was related to OPV refusal, and further clarified that some of the potential reasons for this negative vaccine perception and behavior were founded in strained relationships (perceived or real) between communities and their governing agencies who administer vaccinations.Citation28 The second, a qualitative study, identified attitudes, poor communication skills among health workers, and lack of motivation as affecting vaccine perceptions, with many clinic-level factors such as availability of seats, ventilation, and waiting times affecting a caregiver's desire to pursue immunization services for their child.Citation29 Additionally, some authors have attributed unmeasured confounding and residual vaccine defaulting behaviors to vaccine hesitancy without identifying a root cause or exploring the potential linkages between hesitancy and vaccination outcomes.Citation30 It is important to note that vaccine hesitancy is unlikely to be the sole factor explaining untimely vaccination, and other factors, including health literacy, may play a significant role. Nearly 50% of the surveyed respondents had an elementary education or less, indicating that level of schooling and insufficient health literacy may have explained some of the hesitancy or untimeliness of vaccinations.
Untimely vaccinations have significant impact on immunization system functioning. The fact that only two-thirds of those fully vaccinated in the study sample were vaccinated with all recommended doses in a timely manner indicates that merely relying on vaccination coverage overestimates population immunity, as it does not account for delays in protection and extended susceptibility to preventable diseases. As such, untimely vaccinations are likely to contribute greatly to the preventable disease burden in Ethiopia, allowing for transmission among those in the age group at which they are the most vulnerable to severe disease with tragic consequences.
Generalizability of findings
It is important to contextualize the vaccination outcomes recorded in this study. These vaccine coverage and timeliness estimates represent the best-case scenario for immunization outcomes in Ethiopia. Addis Ababa has the highest recorded vaccination coverage rates in the country, with levels markedly lower in ethnic minority and pastoralist regions outside of the capital.Citation5 Additionally, the results of this survey represent the behaviors of an already health-seeking population due to the sampling strategy. Given that individuals were sampled from caregivers already attending a health center to receive immunizations for their children, we effectively controlled for active health-seeking behaviors in our study sample, thus further representing a ‘best-case scenario’ for vaccination. As such, it is necessary to realize that the proportion of timely vaccinations in the country as a whole is likely far lower than our findings of ∼56%. This necessitates additional study into vaccine hesitancy behaviors as it may drive and influence non-vaccination in settings with poorer vaccination outcomes among individuals with varied health-seeking behaviors.
Strengths and limitations
This study has several strengths. The survey utilized the SAGE Working Group's standard questionnaire questions on assessing vaccine hesitancy, and thus utilized a validated metric for assessing vaccine hesitancy in this context. Additionally, the survey was the first to characterize the relationship between vaccine hesitancy and timeliness of received vaccinations, paving the way for future studies to confirm the relationship between vaccine hesitancy and timely immunizations.
This study also has several limitations. Because timeliness was the primary outcome variable, vaccination status for children was only recorded when vaccination cards were available, which may not be a representative sample. Additionally, the survey we administered was cross-sectional, and thus inference about temporal associations between variables is limited, preventing the ability to infer causation. We did not capture historical variables on clinic-level factors which could influence vaccine co-administration or timeliness, such as vaccine stock-outs. We anecdotally determined that one of the health centers stocked-out of OPV3 during the study but were unable to capture historical stock-outs which may have influenced prior vaccine administration. It is thus important to note that there may be some drivers of delayed vaccination as well as sub-optimal co-administration levels which are not captured in the data provided.
Conclusions
Vaccine coverage estimates do not fully describe the immunization service functioning in Addis Ababa, as timeliness analyses reveal that only 2/3 of the children who are fully vaccinated are fully vaccinated according to the recommended schedule. Vaccine hesitancy, as measured by the SAGE Working Group scale, was found to significantly influence timeliness of received vaccinations, providing a potential intervention strategy to target educational campaigns around certain aspects of vaccine perceptions to mitigate hesitancy and subsequently hope to improve timeliness. These efforts will likely also contribute to improved disease burden as the untimely proportion of vaccinated individuals shrinks, reducing unnecessary susceptibility to disease among some of the most vulnerable age groups. Further studies are needed to explore the potential explanatory factors behind vaccine hesitancy among caregivers in Addis Ababa.
Methods
Study design
A multistage sampling design was employed with cluster sampling performed utilizing Addis Ababa's administrative unit, sub-cities, as the clustering variable. There are 10 sub-cities in Addis Ababa, which vary by ethnic composition, geographic size, and socioeconomic status (). We selected 5 of the 10 sub-cities (50%) in order to achieve a more representative sample of the city of Addis Ababa by maximizing heterogeneity among sampled sub-cities.
One health center was subsequently selected from each selected sub-city by simple random sampling, utilizing a list of all health centers in Addis Ababa as a sampling frame. Subjects were sampled from each health center by systematic random sampling, utilizing sampling proportionate to size of each health center's catchment population. A sampling interval, or k, of 1.5 was chosen, and employed by selecting two eligible participants, skipping one patient, and then selecting another. Eligible participants were caregivers who presented at the health center with a child aged 3–12 months for immunizations during the survey period (June 1 – June 21, 2017). When calculating the sample size required for the study to have adequate power, mother's knowledge of immunization is taken to be 71.2%, as was found in a previous study.Citation8 Using OpenEpi online software, with p = 0.712 alpha = 0.05, non-response rate = 10% and effect size = 1, the required sample size was calculated as n = 350.
Nurses at the health centers served as data collectors and were trained to conduct participant selection and interviews according to study guidelines. Data collectors approached potential participants upon presentation in the health center and inquired about their interest in participating in a research study. If interested, the data collector obtained written or oral informed consent based on the participant's literacy, followed by administration of the questionnaire.
Study population
The target population for this study is all caregivers of young children eligible to receive immunization in Addis Ababa. The study population comprised caregivers of young children (aged 3 to 12 months) who brought their child to one of the five sampled health centers during the study period. The age-cutoff for eligible children was selected to capture children who have received most of their vaccines, but have not reached the age (i.e. > 12 months) after which they no longer present to health centers to receive EPI immunizations. Infants aged 3 to 12 months span the age range during which they receive the majority of immunizations, but also experience the highest morbidity and mortality burden, and thus delays in vaccination have significant health implications.
Study questionnaire and operational definitions
This survey covered basic sociodemographic questions, including marital status, educational attainment, monthly income, religion/ethnicity, employment status, and health-seeking behaviors such as place of delivery and place of immunization services. Vaccination status and timeliness were assessed by maternal recall and by transcribing the child's vaccination card with dates of received vaccines. The majority of the survey was focused on assessing vaccine hesitancy, which used standard questions developed by the WHO Strategic Advisory Group of Experts (SAGE) on Immunization, evaluated on a 5-point Likert scale, with each component of vaccine hesitancy broken down into disagree (1,2), don't know (3), or agree (4,5).Citation19 Subsequently, a sum score was calculated across all questions to create an overall measure of each participant's hesitancy toward vaccines. The negatively-posed, oppositely directed questions were re-coded such that lower sum scores indicated increased vaccine hesitancy. Based on the distribution of these sum scores, participants were categorized into tertiles of vaccine hesitancy, dividing the sum scores evenly into the bottom third, the middle third, and top third of hesitancy scores among caregivers. Due to small sample size among respondents of the Catholic Religion (n = 2), Catholics were collapsed into the religious majority and reference group, “Ethiopian Orthodox” for multivariate analyses.
The primary outcome was a two-way categorization of timely and untimely vaccinations relative to the vaccination milestones of birth, 6 weeks, 10 weeks, 14 weeks and 9 months. Age at vaccination was determined by subtracting the birthdate from the vaccination date as indicated on the child's immunization card. Incomplete/partial and negative vaccination dates, i.e. vaccination dates before a child's date of birth, were excluded from analysis. Timely vaccinations were defined by providing a 4 day “early” grace period ahead of the recommended milestone age and a 4 week “late” grace period after the recommended age according to CDC standard definitions,Citation31 based on the Ethiopian EPI schedule (). Untimely vaccinations were defined as any vaccines received outside of this interval. For an individual to have been considered timely as our outcome of interest, that child needed to have received each vaccine (i.e. four doses of OPV, one dose of IPV, three doses of pentavalent and PCV, two doses of rotavirus, and one doses of measles, all received in the timely window as defined above), otherwise he/she was classified as untimely.
Statistical analysis
The distribution of various socioeconomic, demographic, and clinical factors is presented using descriptive statistics. The associations between risk or preventive factors and timely and untimely vaccination status were assessed by multinomial logistic regression, with estimates of odds ratios (OR) and 95% confidence intervals (CI) for timely compared to untimely vaccination. While there were no exclusions to the data, and all 350 caregivers completed a survey document, missing data across individual responses to questions created smaller, different-sized subsets of observations within each variable. Significance was assessed at an α level of 0.05, and all analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC, USA).
Ethical consideration
Ethical review of this study was reviewed and approved by the University of Michigan Institutional Review Board and the St. Paul's Hospital Millennium Medical College Institutional Review Board, deemed exempt under Section II.
Disclosure of potential conflicts of interest
The authors have no potential, perceived, or real conflicts of interest relevant to this article to disclose. NBM wrote the first draft of the article.
Acknowledgments
We acknowledge the hard work of the data collectors and nurses at the health centers in Addis Ababa, without whom conducting this survey would have been impossible.
Additional information
Funding
References
- WHO. Immunization coverage. WHO. http://www.who.int/mediacentre/factsheets/fs378/en/. Published 2017. Accessed October 10, 2017.
- UNICEF. Levels and trends in child mortality. New York UNICEF. 2015:1–30. http://www.who.int/maternal_child_adolescent/documents/levels_trends_child_mortality_2013/en/.
- Canavan ME, Sipsma HL, Kassie GM, Bradley EH. Correlates of complete childhood vaccination in East African countries. PLoS One. 2014;9(4):1–7. doi:10.1371/journal.pone.0095709.
- Federal Ministry of Health. National Expanded Programme on Immunization: Comprehensive Multi-Year Plan 2011–2015. Addis Ababa, Ethiopia: Federal Ministry of Health; 2010.
- Central Statistical Agency and ICF International. Ethiopia Demographic and Health Survey 2016 Key Indicators Report. Maryland: ICF International; Addis Ababa: Ethiopia National Bureau of Statistics; 2016.
- Central Intelligence Agency. The World Factbook: Ethiopia. https://www.cia.gov/library/publications/the-world-factbook/geos/et.html. Published 2018. Accessed January 20, 2018.
- Central Statistical Agency and ICF International. Ethiopia Demographic and Health Survey 2011 Key Indicators Report. Maryland: ICF International; Addis Ababa: Ethiopia National Bureau of Statistics; 2012.
- Lakew Y, Bekele A, Biadgilign S. Factors influencing full immunization coverage among 12–23 months of age children in Ethiopia: evidence from the national demographic and health survey in 2011. BMC Public Health. 2015;15(1):728. doi:10.1186/s12889-015-2078-6. PMID:26224089.
- Abadura SA, Lerebo WT, Kulkarni U, Mekonnen ZA. Individual and community level determinants of childhood full immunization in Ethiopia: a multilevel analysis. BMC Public Health. 2015;15:972. doi:10.1186/s12889-015-2315-z. PMID:26415507
- Mohamud AN, Feleke A, Worku W, Kifle M, Sharma HR. Immunization coverage of 12 – 23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health. 2014;14(865):1–9. PMID:24383435.
- Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr. 2015;15(1):1–14. doi:10.1186/s12887-015-0345-4. PMID:25626628.
- Kassahun MB, Biks GA, Teferra AS. Level of immunization coverage and associated factors among children aged 12–23 months in Lay Armachiho District, North Gondar Zone, Northwest Ethiopia: a community based cross sectional study. BMC Res Notes. 2015;8(1):1–10. doi:10.1186/s13104-015-1192-y. PMID:25645429.
- Ebrahim Y, Salgedo WB. Childhood Immunization Coverage in Tehulederie District, Northeast of Ethiopia: a Community Based Cross-Sectional Study. Int J Curr Res. 2015;7(9):20234–40.
- World Health Organization. Summary of WHO Position Papers – Recommendations for Routine Immunization. http://www.who.int/immunization/policy/Immunization_routine_table1.pdf. Published 2017. Accessed September 7, 2017.
- Odutola A, Afolabi MO, Ogundare EO, Lowe-Jallow YN, Worwui A, Okebe J, Ota MO. Risk factors for delay in age-appropriate vaccinations among Gambian children. BMC Health Serv Res. 2015;15(1):346. doi:10.1186/s12913-015-1015-9. PMID:26315547.
- Sadoh AE, Sadoh WE, Uduebor J, Ekpebe P, Iguodala O. Factors contributing to delay in commencement of Immunisation in Nigerian infants. Tanzan J Health Res. 2013;15(3):1–8. doi:10.4314/thrb.v15i3.6. PMID:26591667.
- Calhoun LM, Van Eijk AM, Lindblade KA, Odhiambo FO, Wilson ML, Winterbauer E, Slutsker L, Hamel MJ. Determinants and coverage of vaccination in children in western Kenya from a 2003 cross-sectional survey. Am J Trop Med Hyg. 2014;90(2):234–41. doi:10.4269/ajtmh.13-0127. PMID:24343886.
- Mina MJ, Metcalf CJE, de Swart RL, Osterhaus ADME, Grenfell BT. Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science. 2015;348(6235):694–9. doi:10.1126/science.aaa3662. PMID:25954009.
- Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: The development of a survey tool. Vaccine. 2015;33(34):4165–75. doi:10.1016/j.vaccine.2015.04.037. PMID:25896384.
- Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low- and middle-income countries: a systematic review. Int J Public Health. 2015;60(7):767–80. doi:10.1007/s00038-015-0715-6. PMID:26298444.
- Zewdie A, Letebo M, Mekonnen T. Reasons for defaulting from childhood immunization program: a qualitative study from Hadiya zone, Southern Ethiopia. BMC Public Health. 2016;16(1):1240. doi:10.1186/s12889-016-3904-1. PMID:27938363.
- Fine PEM. Herd Immunity: History, Theory, Practice. Epidemiol Rev. 1993;15(2):265–302. doi:10.1093/oxfordjournals.epirev.a036121. PMID:8174658.
- Zaidi SMA, Khowaja S, Dharma VK, Khan AJ, Chandir S. Coverage, timeliness, and determinants of immunization completion in Pakistan: Evidence from the Demographic and Health Survey (2006–07). Hum Vaccines Immunother. 2014;10(6):1712–20. doi:10.4161/hv.28621.
- Shrivastwa N, Gillespie BW, Kolenic GE, Lepkowski JM, Boulton ML. Predictors of Vaccination in India for Children Aged 12–36 Months. Am J Prev Med. 2015;49(6 Suppl 4):S435–44. doi:10.1016/j.amepre.2015.05.008.
- Hughes MM, Katz J, Englund JA, Khatry SK, Shrestha L, LeClerq SC, Steinhoff M, Tielsch JM. Infant vaccination timing: Beyond traditional coverage metrics for maximizing impact of vaccine programs, an example from southern Nepal. Vaccine. 2016;34(7):933–41. doi:10.1016/j.vaccine.2015.12.061. PMID:26788880.
- Belete H, Kidane T, Bisrat F, Molla M, Mounier-jack S, Kitaw Y. Routine immunization in Ethiopia. Ethiop J Heal Dev. 2015;(1):1–34.
- Federal Ministry of Health. National Expanded Programme on Immunization: Comprehensive Multi-Year Plan 2016–2020. Addis Ababa, Ethiopia: Federal Ministry of Health; 2015.
- Taylor S, Khan M, Muhammad A, Akpala O, van Strien M, Morry C, Feek W, Ogden E. Understanding vaccine hesitancy in polio eradication in northern Nigeria. Vaccine. 2017;35(47):6438–43. doi:10.1016/j.vaccine.2017.09.075. PMID:29031691.
- Oku A, Oyo-Ita A, Glenton C, Fretheim A, Ames H, Muloliwa A, Kaufman J, Hill S, Cliff J, Cartier Y, et al. Perceptions and experiences of childhood vaccination communication strategies among caregivers and health workers in Nigeria: A qualitative study. PLoS One. 2017;12(11):1–21. doi:10.1371/journal.pone.0186733.
- Nagar R, Venkat P, Stone LD, Engel KA, Sadda P, Shahnawaz M. A cluster randomized trial to determine the effectiveness of a novel, digital pendant and voice reminder platform on increasing infant immunization adherence in rural Udaipur, India. Vaccine. 2017. doi:10.1016/j.vaccine.2017.11.023
- CDC. General Recommendations on Immunization. In: J H, A K, S W, eds. Epidemiology and Prevention of Vaccine-Preventable Diseases. 13th ed. Washington, D.C.: Public Health Foundation; 2015:9–31.