ABSTRACT
In many countries, those at risk for complications due to influenza are invited for influenza vaccination, to prevent serious consequences for themselves and those around them. However, vaccination rates are decreasing. The first invitation for vaccination may provide an opportunity to convey ample information about the (dis)advantages of vaccination. We aimed to identify subgroups less likely to be vaccinated after their first invitation. Using data from 87 general practices participating in NIVEL Primary Care Database, we selected persons invited for vaccination for the first time because of their 60th birthday. Of 3.238 included persons, 78% were not vaccinated after their first invitation and in the vast majority (84%) this decision remained consistent over the next years. Men and those with fewer GP contacts were less likely to be vaccinated. This latter group is not easily reached by the GP, so maybe other ways should be considered to convey information about influenza vaccination.
KEYWORDS:
Introduction
Each year about 5% to 10% of adults get influenza.Citation1 In many cases the disease is self-limiting,Citation1 but complications related to influenza are estimated to lead to 250,000 to 500,000 deaths per year worldwide.Citation2 Although complications can occur in previously healthy individuals, especially the elderly and those with chronic diseases are at riskCitation3
In many countries, groups at increased risk for complications due to influenza are advised to receive vaccination. The underlying rationale is that vaccination reduces the risk of influenzaCitation4 and if someone does get ill, it reduces the risk of complications.Citation4,Citation5 The criteria for risk groups differ per country, but in all European countries they include the elderly and persons with chronic diseases.Citation6
Although influenza vaccination is an individual and voluntary decision, the World Health Assembly and European Union have set as a goal that 75% of the elderly population is vaccinated against influenza.Citation7,Citation8 In most European countries this goal is not reached.Citation6 In the season of 2014–15, on average 42% of the elderly population received vaccination, ranging from 1% in Estonia to 76% in the UK. In the Netherlands the vaccination rate dropped from 77% in 2007–08 to 60% in 2014–15.Citation6,Citation9,Citation10
In order to increase the vaccination rate, it may seem logical to aim at the most vulnerable within the target group for vaccination, i.e. the oldest persons with a chronic disease. However, it may be hard to further increase the already relatively high vaccination rate in this group.Citation11 Aiming at those without a chronic disease who receive their first invitation for vaccination may be more profitable. These persons may not be at a high risk for complications themselves, but they are likely to come in contact with relatives and friends who are. Besides, if they start vaccination now they may be more likely to keep being vaccinated if they develop a chronic illness.
We therefore aimed to see how people without a medical indication react to the first invitation for influenza vaccination, whether there are subgroups more/less likely to reject vaccination and whether the decision to accept/reject is consistent in the years thereafter. This may guide informational campaigns (i.e. should campaigns be aimed at a specific subgroup, should they still be targeted at people who have accepted vaccination before?)
Results
We included data from 87 GP practices. In these practices, 3.238 persons were enlisted who were 60 on April 1st 2012 or 2013 and had no medical indication for vaccination. Twenty-two percent of them was vaccinated.
Those with more GP contacts were more likely to be vaccinated (17% in those with no GP contacts v.s. 28% in those with 5 or more contacts). This was irrespective of the type of visit (office visits, telephone visits or home visits) (). Women were more likely to be vaccinated than men (25% vs. 20%). () However, differences were not large, as even in women with more than 5 contacts, only 31% was vaccinated (data not shown).
Table 1. Characteristics of 60 year olds without a medical indication for influenza vaccination according to their response to the first invitation for vaccination.
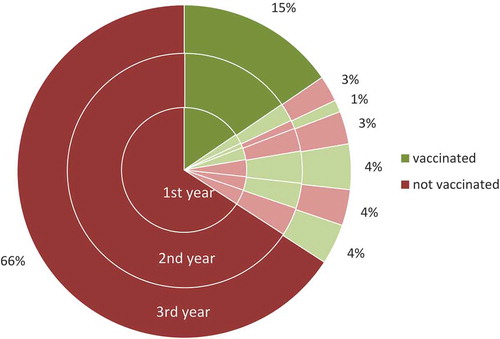
Of those who were vaccinated after their first invitation, 69% was also vaccinated in the subsequent two years. Of those who were not vaccinated after their first invitation, 84% was also not vaccinated in the subsequent two years. () Ultimately, 65% was never vaccinated, 15% was always vaccinated and 13% was sometimes vaccinated. Men and those without face-to-face or telephone consultations in the previous year were more likely to have never been vaccinated. Those with many telephone consultations or a home visit from the GP were more likely to have been vaccinated in all three years. ()
Table 2. Characteristics of those vaccinated in all three years, not vaccinated in all three years and those switching.
Discussion
We found that, even in a country with one of the highest vaccination rates of the EU, four out of five 60-year olds without a medical indication for influenza vaccination decline their first invitation for vaccination. The decision to decline vaccination is consistent in the subsequent two years in over 80%. Moreover, a third of those who are vaccinated after the first invitation are not vaccinated in the subsequent two years.
Patients with fewer GP contacts are less likely to receive vaccination. Previous studies also found that those with more health care use are more likely to receive vaccinationCitation12,Citation13 This may be because they are in poorer health, but also because these contacts give health care providers the opportunity to provide information about influenza vaccination. Indeed, patients indicated that an important reason to accept vaccination is advice from a health care providerCitation12,Citation14–Citation17
We used a large primary care registry with routinely recorded data, thereby avoiding selection and response bias. Besides, data quality was checked thoroughly. A limitation of our study is that we only had a small number of background variables available. It would have been interesting for instance to study the difference between those who are working and those who are not.
Given the low vaccination rate and consistency of the decision not to receive vaccination that we found, healthy 60-year olds seem a good target audience to convey information about influenza vaccination. Informational campaigns should be targeted at the entire group of healthy 60-year olds, as we did not find subgroups with a relatively high vaccination rate and some of those who initially accept vaccination are not vaccinated in subsequent years. It is therefore important to further identify reasons to (not) receive vaccination.
Methods
We used data from GP practices participating in NIVEL Primary Care Database (NIVEL-PCD).Citation18 In this nationally representative Dutch network participating GPs routinely record data on all patient contacts, including diagnoses. Diagnoses are coded according to the ICPC-1 (International Classification of Primary Care) coding system.Citation19 For the analyses we only selected those practices who participated during the period 2012–2015 and provided complete and good quality data.Citation20
From these practices we selected patients who received their first invitation for influenza vaccination in the seasons 2012–2013 or 2013–2014. In the Netherlands all people who are aged 60 or older before the end of the yearly vaccination campaign, i.e. April 1st, or those who have one or more selected chronic conditions (i.e. abnormalities and functional disorders of the airways and lungs, chronic heart disorders, diabetes mellitus, chronic kidney disease, HIV infection, or reduced resistance to infection) in October receive a personal invitation letter from their GP for a free influenza vaccination at the general practice.
To identify people receiving their first invitation, we included those who were 60 years old on April 1st 2013 or 2014 and did not have a chronic condition for which they would have received an invitation for vaccination before their 60th birthday. They also had to be alive and enlisted with the GP practice during the three years after their first invitation.
Vaccination status was based on registration of the ICPC code R44 or ATC code J07BB02 in the electronic medical file. We calculated the percentage who were vaccinated in the first three years after the first invitation according to age, sex, and health care use (office visits, telephone consultations and home visits) and deprivation.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
References
- Hayward AC, Fragaszy EB, Bermingham A, Wang L, Copas A, Edmunds WJ, Ferguson N, Goonetilleke N, Harvey G, Kovar J, et al. Comparative community burden and severity of seasonal and pandemic influenza: results of the Flu Watch cohort study. Lancet Respir Med. 2014;2(6):445–454. doi:10.1016/S2213-2600(14)70034-7.
- WHO. Influenza (seasonal) Factsheet No 211. March 2014 ed. WHO; 2014.
- Lee N, Chan PK, Lui GC, Wong BC, Sin WW, Choi KW, Wong RYK, Lee ELY, Yeung ACM, Ngai KLK, et al. Complications and outcomes of pandemic 2009 Influenza A (H1N1) virus infection in hospitalized adults: how do they differ from those in seasonal influenza? J Infect Dis. 2011;203(12):1739–1747. doi:10.1093/infdis/jir187.
- Beyer WE, McElhaney J, Smith DJ, Monto AS, Nguyen-Van-Tam JS, Osterhaus AD. Cochrane re-arranged: support for policies to vaccinate elderly people against influenza. Vaccine. 2013;31(50):6030–6033. doi:10.1016/j.vaccine.2013.09.063.
- Demicheli V, Jefferson T, Di Pietrantonj C, Ferroni E, Thorning S, Thomas RERivetti A. Vaccines for preventing influenza in the elderly. Cochrane Database Syst Rev. 2018 Feb 1;2:CD004876. doi:10.1002/14651858.CD004876.pub4.
- Seasonal influenza vaccination in Europe. Vaccination recommendations and coverage rates in the EU member states for eight influenza seasons. 2007-2008 to 204-2015. Stockholm, Sweden: ECDC; 2017.
- The Council of the European Union. Council recommendation of 22 December 2009 on seasonal influenza vaccination. Brussels, Belgium : European Union; 2009.
- World Health Assembly. Resolution WHA56.19. Prevention and control of influenza pandemics and annual epidemics. Geneva, Switzerland: 56th World Health assembly; 2003.
- Palache A, Oriol-Mathieu V, Fino M, Xydia-Charmanta M. Influenza Vaccine Supply task f. Seasonal influenza vaccine dose distribution in 195 countries (2004-2013): little progress in estimated global vaccination coverage. Vaccine. 2015;33(42):5598–5605. doi:10.1016/j.vaccine.2015.08.082.
- Tacken MA, Jansen B, Mulder J, Campbell SM, Braspenning JC. Dutch influenza vaccination rate drops for fifth consecutive year. Vaccine. 2015;33(38):4886–4891. doi:10.1016/j.vaccine.2015.07.052.
- Heins M, Hooiveld M, Davids R, Korevaar J. Vaccinatiegraad nationaal Programma Grieppreventie. Vol. 2016. Utrecht, Netherlands: NIVEL; 2017.
- Carrasco-Garrido P, De Andres AL, Hernandez-Barrera V, De Miguel AG, Jimenez-Garcia R. Patient’s perceptions and information provided by the public health service are predictors for influenza vaccine uptake. Hum Vaccin. 2009;5(12):839–842.
- Santibanez TA, Mootrey GT, Euler GL, Janssen AP. Behavior and beliefs about influenza vaccine among adults aged 50-64 years. Am J Health Behav. 2010;34(1):77–89.
- Blank PR, Schwenkglenks M, Szucs TD. Disparities in influenza vaccination coverage rates by target group in five European countries: trends over seven consecutive seasons. Infection. 2009;37(5):390–400. doi:10.1007/s15010-009-8467-y.
- Takahashi O, Noguchi Y, Rahman M, Shimbo T, Goto M, Matsui K, Asai A, Onishi M, Koyama H, Sawada I, et al. Influence of family on acceptance of influenza vaccination among Japanese patients. Fam Pract. 2003;20(2):162–166.
- Gauthey L, Toscani L, Chamot E, Larequi T, Robert CF. Influenza vaccination coverage in the geriatric population of the State of Geneva, Switzerland. Eur J Public Health. 1999;9(1):36–40. doi:10.1093/eurpub/9.1.36.
- Eilers R, De Melker HE, Veldwijk J, Krabbe PFM. Vaccine preferences and acceptance of older adults. Vaccine. 2017;35(21):2823–2830. doi:10.1016/j.vaccine.2017.04.014.
- NIVEL Zorgregistraties - Methoden. Uit: NIVEL Zorgregistraties eerste lijn [internet]. 2015 [Laatst gewijzigd op 02- 03-2016;geraadpleegd op 04- 07-2016]. www.nivel.nl/node/4293.
- Lamberts H, Wood M. ICPC: international classification of primary care. Oxford, UK: Oxford University Press; 1987.
- Nederlands Huisartsen Genootschap. NHG-richtlijn adequate dossiervorming met het elektronisch patiëntendossier (ADEPD), derde versie. Utrecht, Netherlands: NHG; 2013.