ABSTRACT
Japanese encephalitis virus is the major cause of encephalitis in India. To control the increasing incidence and fatal outbreaks, SA 14-14-2 vaccine was introduced initially in 104 endemic districts in phased manner from 2006 to 2011. As there is no data available before 2008 on the number of Japanese encephalitis (JE) cases excluding cases of Acute Encephalitis Syndrome (AES), a four year average of the number of JE vs. AES cases reported during 2008– 2011 was calculated and the value was used to determine the percentage of JE cases out of AES cases for the period 1994 to 2007. The analysis of data for the period 1994 to 2017 showed that there was a substantial increase of JE cases after the initiation of vaccination in 2006. Since the JE vaccination was given only in selected districts, comparing the vaccinated district with non vaccinated district would be more appropriate to determine the impact of vaccination. However, the data available on JE is only at the state wide. Hence, Tamil Nadu state where, district-wise JE data is available from 1993 onwards was used as a model state to determine the impact of vaccination. Even though the data for entire Tamil Nadu state showed an increasing trend, the analysis of data for vaccinated districts reveals that, the increase was due to increase of JE cases in non-vaccinated districts. It shows that, there was a reduction in JE case incidences in the vaccinated districts of Tamil Nadu in particular and India as a whole following the introduction of SA 14-14-2 vaccination.
Introduction
Japanese encephalitis virus (JEV) is the most important cause of viral encephalitis in Asia.Citation1 The annual incidence of Japanese encephalitis (JE) varies both across and within endemic countries, ranging from <1 to >10 per 100 000 population or higher during outbreaks with approximately 68 000 cases and 13 600 to 20 400 deaths.Citation2 Infection leads to severe encephalitis in only 1 of 20–1,000 cases.Citation3 Some 50– 80% of children with clinical JE die and 45–50% of surviving patients exhibit long-term serious residual neurological disability.Citation4 The geographic distribution of JEV overlaps in Asia with the inhabitation of approximately 60% of the global population,Citation5,Citation6 where 3 billion people living, including 700 million children, who are at the risk of acquiring JE infection.Citation7 Among the affected Asian countries, 86–95% of the total cases had been reported from both China and India.Citation8,Citation9 As there is no cure, human vaccination to populations at-risk is the only effective long-term control measure.Citation7 Combined with the potential dispersal of the mosquito vector, owing to climate change and global warming, JE poses a great threat to the areas beyond its traditional geographical contours.Citation5 Due to poor and underreporting, the actual incidence of JE is estimated to be nearly 10 times higher than the reported.Citation10
Based on the recommendations of the Bi-Regional Consultation on Japanese EncephalitisCitation11 which coincided with the massive outbreak of JE during 2005 in the districts of Eastern Uttar Pradesh and the adjoining districts of Bihar,Citation12 the Government of India has made the decision to control JE by introducing a mass vaccination program in 104 endemic districts in 11 States of India in a phased manner for 5 years from 2006– 2011. The live attenuated SA 14–14–2 vaccine which was manufactured in Chengdu Institute of Biological Products (CDIBP), China was selected for vaccination in India based on its success in the neighbouring country Nepal.Citation13 Accordingly, the JE vaccination campaign was started in 2006 as a onetime mass immunization programme targeting all the children in the 1–15 years of age group living in the high-risk districts with a single subcutaneous dose using auto-disable syringes.Citation14 Following the campaign, SA 14–14–2 vaccine was introduced in 2011 in the routine immunization under Universal Immunization Program (UIP)Citation15 in 181 endemic districts as a single dose at the age of 16 to 18 months at the time of 1st booster of DTP vaccine.Citation12 In 2013, another dose of SA 14-14-2 vaccine was added at 9 months of age along with measles vaccine.Citation15 The Ministry of Health and Family Welfare (MoHFW) Government of India then launched Mission Indradhanush in December, 2014 as a special drive to vaccinate all unvaccinated and partially vaccinated children (who have received only one dose) below two years and pregnant women under Universal Immunization Programme.Citation15 The Mission focused on interventions to improve full immunization coverage for children in India from 65% in 2014 to more than 90% by 2020.Citation16
So far, 155 out of 181 identified JE endemic districts had been covered under JE immunization and overall 108 million children at the age of 9–12 months of age and 2nd dose at 16–24 months (6 month after first dose) had been immunized with live attenuated SA 14-14-2 vaccine.Citation15,Citation17 Despite successful vaccination in JE endemic districts covering around 108 million children, the incidence of JE is increasing in an alarming proportion, particularly after 2006Citation6,Citation18 is raising doubts in the success of vaccination. Data from the post marketing surveillance based on neutralization antibody titre showed that the effectiveness of the vaccine in India was only 62.5%Citation14 which was very low when comparing with Nepal where the efficacy was 98.5%.Citation14 It is not clear whether the continued increase in the incidence of JE is due to poor vaccination coverage, ineffectiveness of the vaccine, emergence of a strain against which the vaccine is poorly protective, or, perhaps, a combination of these factors. The results of previous studies on the efficacy of SA 14-14-2 vaccine are extremely conflicting in its success rate from as high as 94.5%Citation1 to 62.5%.Citation8 Hence, a vaccine impact study can provide information to sustain vaccine policy decisions; allow parents, health-care providers and decision-makers to appreciate the benefits of vaccination, and decide on which JE vaccine/s to use; assess the programmatic use and progress. But unfortunately, in India, there is no baseline data on confirmed cases of JE available prior to the introduction of vaccine.Citation19,Citation20 Till 2005, all AES cases were labelled as JE and only from 2006 onwards, the serum samples of suspected cases were tested for JEV.Citation18
The present analysis was made to measure the impact of SA 14-14-2 vaccination on the incidence of JE cases in India and using the data from Tamil Nadu State for comparing the diseases incidence between the vaccinated and non-vaccinated districts. The Tamil Nadu was selected as reference State for the analysis, because the data on JE incidence and death available from 1993 (for India, it is available only from 2008).Citation21 JE was first reported in Tamil Nadu in 1955Citation22 and one of the first affected state in India which then experienced several outbreaks of JE.Citation23
Results
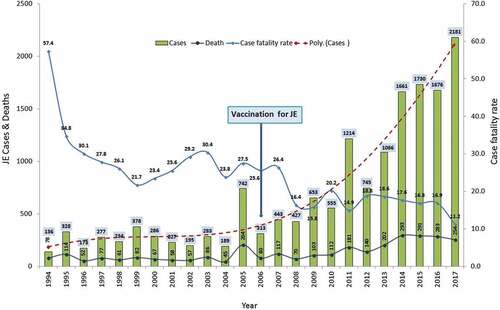
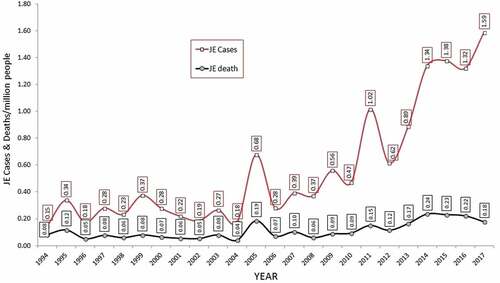
The temporal trend of JE incidence in India for the past 24 years shows a gradual increase in the number of cases from as low as 136 in 1994 to 2181 in 2017. In the past 24 years, the incidence of cases increased by 16 times (0.67 times = 67% per year). Paradoxically, the increase was comparatively steep after 2006, the starting year of JE vaccination in India. Although the JE deaths were increasing, the increase was slow when comparing with cases, from 78 in 1994 to 254 in 2017. There was a 3.3 times increase in deaths over 24 years. This is reflected in the case fatality rate, which came down drastically from as high as 57.4% in 1994 to 11.2% in 2017 (). The population statistics showed that there was an increase from 930.21 million in 1994 to 1285.50 in 2017 ie., 38% increase over 24 years. This increase is seems to be negligible when comparing with increase of JE cases which was 67% per year and hence the number of JE cases per million populations was not masked by the increasing population. The number of JE cases and deaths per million populations went from 0.15 and 0.08 in 1994 to 1.15 and 0.18 in 1997 (). It shows JE cases and deaths were increased by 10.6 and 2.25 times.
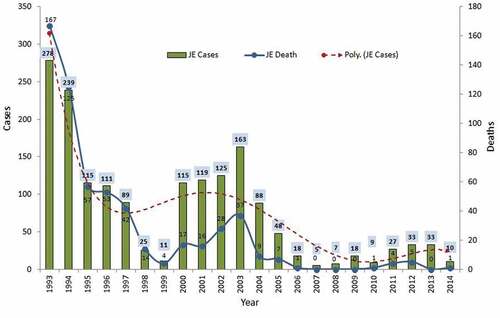
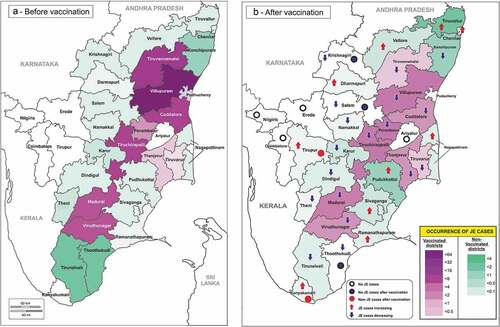
The temporal trend of JE cases in Tamil Nadu shows that the number of JE cases had reached a peak in 1993 with 278 cases and 167 deaths and the same was came down to 10 and one in 2014 (). Even though the vaccination was started in 2007, the decline in the number of cases started much before in 2004, when the cases came down from 163 to 88, 48 in 2005 to 5 in 2007. However, this scenario has changed in 2011 when the number of cases increased to 27 followed by 33 in 2012 and the same was maintained in 2013. This unexpected raise in the number of JE cases as observed in data for India raised a doubt in the success of JE vaccination. In non vaccinated JE reporting districts, the JE cases and deaths were fluctuating with a peak in 1993 (38 cases) and 1997 (36 cases) and then 5 cases and 8 cases during 1999 and 2003 respectively (). After 2003, there was a gradual decline in the incidence of JE reaching 0 incidences in 2008. Surprisingly, after 2008, there was a slow increase in the number of cases to 21 in 2013. The polynominal trendline showed a steep increase in the number of cases and deaths. In contrast to the non vaccinated districts, the vaccinated districts showed a clear trend of decline (). The unequal t-test showed that there is a significant difference in JE cases (t-3.65; df 20; p < 0.05) and deaths (t-2.38; df 20; p < 0.05) in pre and post vaccination periods in vaccinated districts. In non vaccinated districts, the unequal t-test showed no significant difference in the cases (t-0.15; df 20; p > 0.05– 0.88) and deaths (t-1.44; df 20; p > 0.05–0.16) before and after the year 2007, when the vaccination started in neighbouring districts. The statistical analysis showed that there is a clear-cut reduction in the incidence of JE cases and deaths in vaccinated districts when comparing with non-vaccinated districts where the effect of increasing JE case incidences after 2007 was nullified by the high JE case incidence before 1998 and shows like the condition was similar before and after the vaccination period. The JE case density map () showed that there is a decline in the annual incidence of JE case in all the 9 vaccinated districts (marked as ![]() in the map). Whereas, 7 districts out of 16 non vaccinated JE districts showed an increase in the cases after vaccination year of 2007 (
in the map). Whereas, 7 districts out of 16 non vaccinated JE districts showed an increase in the cases after vaccination year of 2007 (![]() ). Six non vaccinated JE district showed decline in the cases after vaccination year. After the vaccination year 2007, two districts were newly affected by JE (
). Six non vaccinated JE district showed decline in the cases after vaccination year. After the vaccination year 2007, two districts were newly affected by JE (![]() ) and three JE affected non vaccinated district showed no case of JE (
) and three JE affected non vaccinated district showed no case of JE (![]() ). Three districts which are not bordering and located away from the vaccinated districts are still free from JE (
). Three districts which are not bordering and located away from the vaccinated districts are still free from JE (![]() ).
).
Figure 4. JE cases and deaths and their polynominal trendline in non-vaccinated districts of Tamil Nadu.
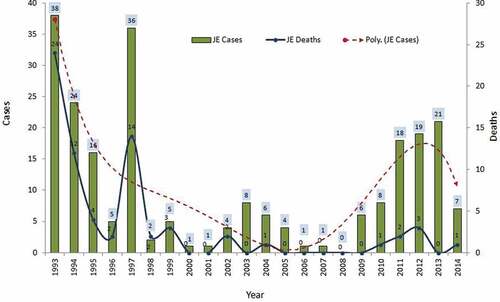
Figure 5. JE cases and deaths and their polynominal trendline in vaccinated districts of Tamil Nadu.
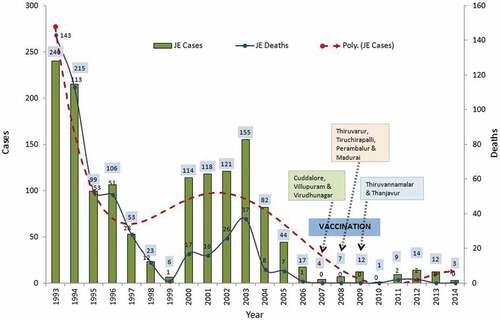
Figure 6. Occurrence of JE cases before and after SA 14-14-2 vaccination in Tamil Nadu, India. A. Before vaccination; B. After vaccination. Note the density of cases (violet) before and after vaccination in the first and second map respectively and declining of cases in all the vaccinated districts. In contrast, the density of cases (green) is increasing in many non vaccinated districts after the period of vaccination and in many districts new cases appeared and increasing.
Discussion
Although there are controversies in the assessment of the efficacy of SA 14-14-2 vaccine,Citation1,Citation14,Citation17 the present analysis shows that the SA 14-14-2 vaccine has reduced the incidence of JE cases in vaccinated districts to a great extent in Tamil Nadu (). While the increase of JE case incidences was at a low level in vaccinated districts, the same was much higher in non-vaccinated districts () and are responsible for the overall hike in the JE case incidences figure for Tamil Nadu ().Citation16 If the same kind of analysis done by comparing the case incidence of JE in vaccinated and non vaccinated districts of other vaccinated states such as Uttar Pradesh could reveal the success of SA 14-14-2 vaccine in those states. In general, the Tamil Nadu model shows a good impact of SA 14-14-2 vaccine in vaccinated districts and insists that, the vaccination to be given simultaneously in all the affected districts to reduce the case incidences in the state and India as a whole. The drastic increase in JE case incidence in India, particularly after the beginning of SA 14-14-2 vaccination was due to increase of case incidence in non-vaccinated districts that brought the overall case incidence high. Although the Govt. of India is committed to the elimination of JE and extended vaccination to 260 endemic districts (till 2017),Citation24 vaccination should also be given to newly emerging areas. Apart from SA 14-14-2 live attenuated vaccine and there are at least three other types of vaccines are also available such as Vero cell derived inactivated vaccines (JENVAC)Citation6, inactivated mouse brain-derived vaccines, and a live recombinant (chimeric) vaccineCitation7 can also be introduced in selected areas on trial basis to see the vaccine which give a better impact. New vaccines are better to be given to naive populations since older individuals who had received inactivated vaccine may have blunted immune responses to subsequent vaccination with live replicating JEV SA14-14-2 and this could impact observed efficacy. Younger individuals who were JEV-naïve and had only received the JEV SA14-14-2 vaccine might have better immune responses by comparison. The vaccine coverage has to be improved and properly monitored as the coverage was poor in Gorakhpur division of Uttar Pradesh state where 32.7% of eligible children missed JE vaccination.Citation25 Another possible reason for increasing JE cases might be due to enhanced reporting and improved diagnosis. In 2006, India strengthened AES surveillance efforts by expanding the network and increasing diagnostic capacity. As part of the programme, JE surveillance was conducted at 50 sites throughout the country, with four sentinel sites supported by WHO and US CDC.Citation26 The fall of case fatality rate from 58.1 in 1994 to 11.2 in 2017 indicates the improvement in health care facility and awareness in the management of JE cases.
Since the data used in this study was from Government health facilities such as National Health Profile,Citation18 it may have limitations in terms of its completeness as private medical and health care institutions still need to strengthen their reporting to their respective Government Health units. Since, adult JE (>15 years) is also slowly on the rise in India as in its nearby countries such as Nepal and Bangladesh, the vaccination programme has to be designed to cover adults in limited but high risk areas.Citation6 Vaccination has to be continued forever even at least low level or until the elimination of JE since the human infection does not contribute to transmission and human vaccination does not reduce transmission in reservoir community and hence no herd immunity would possibly develop.Citation27 Although, single dose of SA 14-14-2 vaccine can induce long term protection, administering two doses at an interval of one year is generally recommended to achieve 95% efficacy.Citation28 Indian efficacy analysis made the Government of India to recommend 2 dose of vaccine through UIP since 2013.Citation8 This could be the reason for the reduction in the number of cases from 33 in 2013 to 10 in 2014. Since pigs play a major role in the transmission cycles due to large scale viral amplification and relatively high viral titres, comparing with other domestic animals,Citation29 vaccination of pigs in areas where pig farming is popular may substantially reduce JE incidence in endemic areas. The JE annual case density map reveals that, the annual JE case incidence started increasing above normal level in all the districts neighbouring vaccinated districts indicates by the mechanism yet to be explored but somehow, the JEV managed to occupy the unoccupied or not well occupied niche. The two major contributors of JE, India and China are classified under Group 2 countries where national surveillance programs were established and JE vaccines were used in selected areas.Citation9 Even though, JE vaccination was started in China as early as in 1968 and successfully controlled JE in most of the regions of China, still JE is a major problem in southwest regions. JE cases started increasing in non vaccinated areas when comparing with vaccinated areas. In the regions such as Xinjiang, Tibet and Qinghai where JE was not prevalent since 1951 are now reporting seropositivity for JEV in healthy people and domesticated pigs and JEV isolated from Culex. tritaeniorhynchus mosquitoes.Citation30 In contrast to the experience of China where the overal JE cases decreased after vaccination despite the appearance of new cases and increase of cases in non vaccinated areas, the overall JE cases had substantially increased in India despite remarkable decline in the vaccinated districts. This might be due to the complex JE epidemiological pattern in India where JE occurs both epidemic and endemic form. Whereas in China, JE occurs in epidemic form and in south Asian countries such as in Thailand, Vietnam, Malaysia, Cambodia, Indonesia, Philippines, Sri Lanka and Singapore JE occurs as endemic form.Citation9 Since JE cases are emerging in newer area where JE had never been reported before and cases increasing in those areas where JE vaccine was not given before, more sentinel sites need to be established. Although the surveillance for JE cases had greatly been improved after 2006, around 130 sentinel sites [65(2007–08) + 13 (2011–12)+ 3 (2013), 4 (2014) and 45 (2015–16)] had been established exclusively for the surveillance of JE and AES cases, more such set up is still needed to cop up the increasing cases. JE test kit (MAC ELISA) had been supplied free of cost for testing JE infection at the sentinel sites and the negative samples were sent to Apex laboratories for testing non JE pathogens for AES cases.Citation24 There are few possible limitations which cannot be ruled out, such as the present study is based on the data generated by passive surveillance systems of government hospitals and treatment facilities where the cases reported would be several folds less than the actual number of cases and the data of Tamil Nadu state was used to presume the overall Indian scenario which may not be totally accurate.
Conclusion
Even though the number of JE cases is increasing after vaccination in Tamil Nadu State and India, the Tamil Nadu model shows that the overall increase in JE cases were due to increasing of JE cases in non-vaccinated districts and vaccinated district did not show any substantial increase in the number of cases. Hence, to achieve complete prevention/elimination of JE the following measures can be adapted. 1. SA 14-14-2 vaccine has to be given in all the JE reporting districts (not restricted only to endemic districts). 2. Expansion of surveillance system with facility to confirm JE and AES, virus detection in mosquitoes & human and assessing the prevalence of JEV antibodies in common population. 3. Case control studies are needed before making decision on extending the SA 14-14-2 vaccine usage. The possibility of vaccinating pigs in JE endemic areas, moving pig farms away from paddy fields and bringing adults of >15 years age group for vaccination are also need to be explored for the control JE outbreaks to a greater extend. The present study showed that the SA 14-14-2 vaccine has remarkably reduced the JE case incidences in selected endemic districts of India.
Methods
According to the WHO guideline (2015),Citation20 a vaccine impact study generally measures the fall in the incidence of the target disease in a population as a consequence of a vaccination programme, compared to what the incidence would have been in the absence of the programme. The present report analysed the impact of vaccination in terms of reduction in case incidence, if any, after vaccination by comparing the case incidence before and after vaccination. The data archived at National Health Profile of Central Bureau of Health Intelligence (CBHI)Citation18 for the period 1994–2017 and data collected from Department of Public Health and Preventive Medicine (DPH & PM),Citation21 Tamil Nadu on JE cases and deaths for the period 1993–2014 (unpublished data) were plotted on graph, to see if the temporal trends could be associated with the SA 14-14-2 vaccination in India. Although underreporting is a major problem in India and the actual number of cases would be several folds higher than the reported cases, the number of cases reported for each year in the study period is still assumed to be a fairly stable proportion of the actual number of cases which can reflect the trend of disease incidences.Citation24
Till 2005, all AES cases were being labelled as JE. From 2008 only, data on JE and AES separately was available at CBHI, Govt. of India. Therefore, a four year average proportion of JE cases among the total AES cases was calculated for the period 2008 to 2011 and was extrapolated on AES data for the period from 1994 to 2007 to extract the proportion of JE cases and deaths from the total reported cases and deaths which was used to draw the temporal trend. The proportion of JE cases and deaths were 9.97, 11.60, 9.7, 12.83 and 9.28, 11.68, 14.16, 13.41 respectively for four years from 2008 to 2011. The four year average was 11.02 and 12.13 for cases and deaths which was used to calculate JE cases and deaths out of total AES cases reported before 2008. Number of JE cases and deaths per million populations for the period 1994 to 2017 were also calculated and trendline was drawn. The population data and predicted data of population for the year 2021 available from census of India were utilized to estimate the JE cases and deaths per million populations from 1994 to 2017. The temporal trend of JE cases and deaths in Tamil Nadu was compared with that of JE cases and deaths in vaccinated and JE reporting non-vaccinated districts. Those districts where there is no JE cases reported so far were not included in the study. Unequal t-test was followed to compare the data and polynomial trendline was used to assess the trend of JE cases and deaths. Annual incidence of JE cases before and after vaccination was calculated for every districts of Tamil Nadu and a density map was drawn.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
The technical assistance of Dr. A. Venkatesh and Dr. S. Victor Jerold Leo in the analysis of data is gratefully acknowledged. The authors express sincere thanks to Dr. R. Paramasivan for giving valuable suggestions and Dr. P. Jambulingam, Director of Vector Control Research Centre, Pondicherry for giving permission to carry out this study and for his rigorous input in preparing the manuscript. We are also thankful to the Department of Public Health and Preventive Medicine, Govt. of Tamil Nadu for providing data on JE cases.
References
- Kumar R, Tripathi P, Rizvi A. Effectiveness of one dose of SA 14-14-2 vaccine against Japanese encephalitis. N Engl J Med. 2009;360:1465–66. PMID: 19339732. doi:10.1056/nejm2009.360.1465.
- World Health Organization. Japanese encephalitis. WHO Fact sheet; 2018 [accessed 2018]. http://www.who.int/mediacentre/factsheets/fs386/en.
- Verma R. Japanese encephalitis vaccine: need of the hour in endemic states of India. Hum Vaccin Immunother. 2012 Apr;8(4):491–93. Epub 2012 Feb 28. PMID: 22370517. doi:10.4161/hv.18925.
- Halstead SB, Jacobson J. Japanese encephalitis vaccines 311-352. In: Plotkins SA, Orenstein WA, Offit PA editors. Vaccines 5th Ed. W.B. Saunders Elsevier Co, China; 2008
- Fischer M, Lindsey N, Staples JE, Hills S. Japanese encephalitis vaccines: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep. 2010 Mar 12;59(RR–1):1–27. PMID: 20224546.
- Singh A, Mitra M, Sampath G, Venugopal P, Rao JV, Krishnamurthy B, Gupta MK, Sri Krishna S, Sudhakar B, Rao NB, et al. A Japanese encephalitis vaccine from India induces durable and cross-protective immunity against temporally and spatially wide-ranging global field strains. J Infect Dis. 2015 Sep 1;212(5):715–25. Epub 2015 Jan 18. PMID: 25601942. doi:10.1093/infdis/jiv023.
- Ginsburg AS, Meghani A, Halstead SB, Yaich M. Use of the live attenuated Japanese encephalitis vaccine SA 14-14-2 in children: A review of safety and tolerability studies. Hum Vaccin Immunother. 2017 Oct 3;13(10):2222–31. Epub 2017 Aug 25. PMID: 28841362. doi:10.1080/21645515.2017.1356496.
- IAP Guidebook on Immunization. Indian academy of pediatrics. Gwalior, India: National Publication House; 2013–14. https://www.iapindia.org/files/IAP%20Guidelines/IAP%20Guidebook%20on%20Immunization%202013-14.pdf.
- Wang H, Liang G. Epidemiology of Japanese encephalitis: past, present, and future prospects. Ther Clin Risk Manag. 2015 Mar 19;11:435–48. S51168. eCollection 2015. doi:10.2147/TCRM.
- Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, Marfin AA, Solomon T, Tsai TF, Tsu VD, et al. Estimated global incidence of Japanese encephalitis: A systematic review. Bull World Health Organ. 2011 Oct 1;89(10):766–74. Epub 2011 Aug 3. PMID: 22084515 PMCID: PMC3209971. doi:10.2471/BLT.10.085233.
- World Health Organization. Report of the Bi-Regional meeting on Japanese Encephalitis (WHO SEA/WPR AND/PATH’s JE Project). Bangkok (Thailand), 30 March – 1 April 2005. http://www.wpro.who.int/immunization/meetings/2005/je_biregional_2005_meeting_report.pdf.
- Operational Guide Japanese Encephalitis Vaccination in India. Immunization division department of family welfare ministry of health and family welfare government of India; 2010 Sept. http://www.nipccd-earchive.wcd.nic.in/sites/default/files/PDF/Operational%20Guide%20Japanese%20Encephalitis%20Vaccination%20in%20India%20-%202010-MOHFW.pdf.
- Bista MB, Banerjee MK, Shin SH, Tandan JB, Kim MH, Sohn YM, Ohrr HC, Tang JL, Halstead SB. Efficacy of single-dose SA 14-14-2 vaccine against Japanese encephalitis: a case control study. Lancet. 2001 Sep 8;358(9284):791–95. PMID: 11564484. https://www.ncbi.nlm.nih.gov/pubmed/11564484.
- Vashishtha VM. Japanese encephalitis vaccines. In: Choudhury P, Bansal CP, Yewale VN, Agarwal R, editors. IAP guidebook on immunization 2013-2014. Gwalior, India: National Publication House, Indian Academy of Pediatrics; 2014. https://www.iapindia.org/files/IAP%20Guidelines/IAP%20Guidebook%20on%20Immunization%202013-14.pdf.
- Universal Immunization Program, Immunization Division. Ministry of health and family welfare, government of India. [ accessed 2015 Jun 16. https://mohfw.gov.in/sites/default/files/5628564789562315.pdf.
- Policy Note 2017-18. Health and family welfare department. Demand No. 19 Government of Tamil Nadu; 2017. http://cms.tn.gov.in/sites/default/files/documents/hfw_e_pn_2017_18_0.pdf.
- Vashishtha VM, Ramachandran VG. Vaccination policy for Japanese encephalitis in India: tread with caution! Indian Pediatr. 2015 Oct;52(10):837–39. PMID: 26499003. https://www.indianpediatrics.net/oct2015/837.pdf.
- National Health Profile. Central bureau of health intelligence, Govt. of India; 2005–2011. http://www.cbhidghs.nic.in/index1.asp?linkid=267
- Indian Council of Medical Research. Minutes of the meeting of the core committee on vaccines; 2010 [ accessed 2018 Mar]. http://jacob.puliyel.com/download.php?id=288.
- World Health Organization. WHO guide to measuring effectiveness and impact of Japanese encephalitis vaccination. Document of WHO Expert Consultation on Measuring the Effectiveness and Impact of Japanese Encephalitis Vaccines, held 14-15 May in Geneva, Switzerland; 2015. http://www.who.int/immunization/diseases/japanese_encephalitis/JE_effectiveness.pdf.
- Department of Public Health and Preventive Medicine (DPH & PM). Tamil Nadu on JE cases and deaths for the period 1993-2017 [unpublished data collected by personal communication].
- Webb JKG, Pereira SM. Clinical diagnosis of arthropod borne type viral encephalitis in children in North Arcot district, Madras state.India. Indian J Med Sci. 1956;10:572.
- Carey DE, Myers RM, Pavri KM. Japanese encephalitis studies in Vellore, South India. II. Antibody response of patients. Indian J Med Res. 1968 Sep;56(9):1319–29. PMID: 4302907.
- Disease control programmes (NHM) Chapter 5. Annual Report 2016-17, Department of Health and Family Welfare, Ministry of Health and Family Welfare. New Delhi, India: Govt. of India, Nirman Bhawan. 110011. https://mohfw.gov.in/annual-report-department-health-and-family-welfare–2016-17.
- Murhekar MV, Oak C, Ranjan P, Kanagasabai K, Shinde S, Pandey AK, Mittal M, Gore M, Mehendale SM. Coverage & missed opportunity for Japanese encephalitis vaccine, Gorakhpur division, Uttar Pradesh, India, 2015: implications for Japanese encephalitis control. Indian J Med Res. 2017 Jan;145(1):63–69. PMID: 28574016 PMCID: PMC5460575. doi:10.4103/ijmr.IJMR_712_16.
- World Health Organization, Regional Office for South-East Asia. Fourth biregional meeting on the control of japanese encephalitis (JE): 7-8 June 2009. Bangkok (Thailand): WHO Regional Office for South-East Asia; 2010. http://www.who.int/iris/handle/10665/205120.
- Lord JS, Gurley ES, Pulliam JRC. Rethinking Japanese encephalitis virus transmission: a framework for implicating host and vector species. PLoS Negl Trop Dis. 2015 Dec;9(12):e0004074 1–7. doi:10.1371/journal.pntd.0004074.
- World Health Organization. Japanese encephalitis vaccines. Wkly Epidemiol Rec. 2006;81:331–40.
- Khan SU, Salje H, Hannan A, Islam MA, Bhuyan AA, Islam MA, Rahman MZ, Nahar N, Hossain MJ, Luby SP, et al. Dynamics of Japanese encephalitis virus transmission among pigs in Northwest Bangladesh and the potential impact of pig vaccination. PLoS Negl Trop Dis. 2014 Sep 25;8(9):e3166. eCollection 2014 Sep. doi:10.1371/journal.pntd.0003166.
- Gao X, Li X, Li M, Fu S, Wang H, Lu Z, Cao Y, He Y, Zhu W, Zhang T, et al. Vaccine strategies for the control and prevention of Japanese encephalitis in Mainland China, 1951-2011. PLoS Negl Trop Dis. 2014 Aug 14;8(8):e3015. eCollection 2014 Aug. doi:10.1371/journal.pntd.0003015.
- Muniaraj M, Paramasivan R, Mariappan T, Arunachalam N, Sinha PK. The treatment of visceral leishmaniasis (kala-azar) in India: no obvious signs of long-term success. Trans R Soc Trop Med Hyg. 2012 Dec;106(12):770–72. doi:10.1016/j.trstmh.2012.08.010.