?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
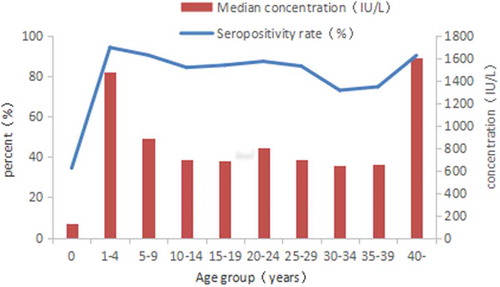
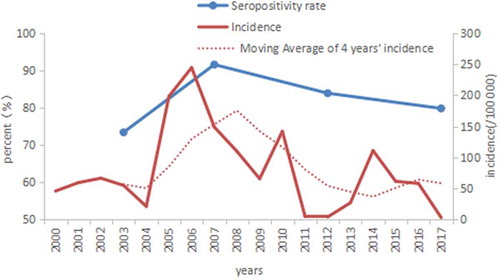
The aim of this study was to assess the seroprevalence of measles and identify the high risk of measles infection in the general population of Beijing. A total of 2144 subjects aged 0–76 years old were selected using a multi-stage stratified sampling method. Socio-demographic characteristics, vaccination history, and disease history of measles were collected by questionnaire. Serum samples were tested for measles-specific IgG by using commercial ELISA kits. The overall seropositivity rate of measles was 79.80% (95% CI 78.1–81.5%) and standardized seropositivity rate was 84.61% (95% CI 84.12–87.10%), with the median concentration of 773.40IU/L. The area of Beijing with the highest seroprevalence was the central area [81.79% (95% CI 80.16–83.42%) and 855.84IU/L]. There were no significant differences in seropositivity rates of different genders (P = 0.074), history of measles infection (P = 0.421) and registered population (P = 0.598). The 1–4 age group had the highest seropositivity rate [94.06%(95% CI 93.06–95.06%)] and children below the age of 1 (0–12 months) had the lowest seropositivity rate [34.42% (95% CI 32.41–36.43%)]. The 30–34 and 35–39 age groups were relatively lower with 72.90% (95% CI 71.02–74.78%) and 74.65% (95% CI 72.81–76.49%) respectively. Seropositivity rates changed along with the incidence rates of measles periodically by years. As shown in the present study, the seroprevalence of measles antibody in Beijing have not yet met the threshold required to achieve measles elimination and therefore the risk of an epidemic of measles will be existing. Appropriate targeted immunization strategies and measures should be considered and carried out.
KEYWORDS:
Introduction
In 2003, a measles elimination goal was declared formally by the World Health Organization (WHO) Regional Committee of the Western Pacific Region (WPR),Citation1 and in 2005 the specific time point for achieving this was set for 2012.Citation2 The Chinese government responded to it positively, and a variety of vaccination strategies have been used to strengthen the population immunity, including a two-dose vaccination program and a series of supplemental immunization activities (SIAs). During 2005–2017, China annual reported measles incidence declined by 95.5% from 94.7 to 4.3 per million population,Citation3,Citation4 however, it is still more than the target of 1 per million and far from achieving the elimination goal. Having experienced this delay, the target date for regional measles elimination has been changed to 2020 by the WPR committee.Citation5 After that, the WPR committee urged the countries across the region to update the national strategies or action plans relating to measles elimination. Thus the government of China encourage that each provinces can confirmed elimination independently to achieve the target as soon as possible.
As the capital of China, Beijing has a total area of 16,808 square kilometers and a population of 19.6 million, including 7 million migrants from other provinces.Citation6 Since 2005 the vaccination schedule has recommended 3-dose measles-containing vaccine (MCV) at 8 months, 1.5 and 6 years of age. In addition, SIAs implemented for pre-school children per quarter since 2000 and school entry immunization checks provided for new enrolled school students per year since 2005. In 2010, a synchronized nationwide SIA targeting children aged 8 months to 14 years was conducted. All of these immunization strategies may have helped to elevate the herd immunity level of the Beijing, leading to a dramatic decline (98.5%) in measles, dropped from 198.3 per million population in 2005 to a historic low 3.0 in 2017.7
Some theories of measles elimination have concluded that if the percentage of the of population who are immune is below about 95%, that is to say the susceptible proportion surpasses 5%, it is possible to have outbreaks or ongoing transmission of the virus.Citation8,Citation9 A mathematical model has estimated that the herd immunity threshold necessary to interrupt measles transmission in the United States is 93–95%.Citation10 Thereby whether the measles has been eliminated or not, it is essential to investigate population immunity level of measles antibody regularly. So during the year 2017, we carried out a population-based, cross-sectional survey for measles seroprevalence in Beijing, in order to identify the sub-populations at risk and predict the trend of measles epidemic in the resident population, also to provide scientific evidence for measles elimination and to give relevant strategies to help achieve measles elimination.
Results
Characteristics of study population
A total of 2144 subjects were enrolled in the study with the age range of 3 days to 76 years. The ratio of male to female was 1:1.08 (1032:1112) and the ratio of native residents and immigrant residents was 1:1.00 (1074:1070). The population with disease history made up 0.47% (10/2144) and the population with vaccination history made up 41.56% (891/2144). Ninety point three percent (121/134) 8–23 months old children had received at least 1 dose of MCV, and 98.46% (640/650) 2–14 years old children had received at least 2 doses. The overall seropositivity rate of measles antibodies was 79.80% (95% CI 78.1–81.5%) and standardized seropositivity rate was 84.61% (95% CI 84.12–87.10%), with the median concentration was 773.40IU/L.
Antibody levels in different districts
Compared with central and suburban areas, both seropositivity rates and median concentration in rural area were the lowest, with 75.60% (95% CI 73.78–77.42) and 711.29IU/L respectively. Central area were relative high [81.79% (95% CI 80.16–83.42) and 855.84IU/L] and differences between different districts were significant with 0.022 and 0.019 P values respectively ().
Table 1. Characteristics of seroepidemiological profiles of measles in Beijing 2017.
Antibody levels in different population
There was no significant difference between seropositivity rates of genders (P = 0.074), but was a significant difference of median concentration between males and females (P = 0.014), with females being higher than males. Similarly, there was a significant the difference between median concentration regarding history of measles infection (P = 0.036), but there was no significant difference between seropositivity rates (P = 0.421).
Compared with subjects without measles vaccination or whose measles vaccinations are unknown, those with measles vaccination had a higher level of seropositivity rates and median concentration (both P values less than 0.001).
Migrant residents had similar seropositivity rates and median concentration levels as native residents, there were no significant differences between them (P values were 0.598 and 0.101 respectively) ().
The seropositivity rate and median concentration level of measles differed among different age groups (both P values less than 0.001). The 1–4 age group had the highest seropositivity rate [94.06%(95% CI 93.06–95.06%)] and 0 age group had the lowest seropositivity rate [34.42% (95% CI 32.41–36.43%)], then 30–34 and 35–39 age groups were relative lower with 72.90% (95% CI 71.02–74.78%) and 74.65% (95% CI 72.81–76.49%) respectively. The seropositivity rate of 0–7 months old was 9.38% (12/128, 95% CI 8.15–10.61%), and in 8–11 months old was 71.26% (62/87, 95% CI 69.34–73.18%). The lowest concentration level also occurred in 0 age group (130.55IU/L), which in 0–7 months old was 81.86IU/L and in 8–11 months old was 1432.04IU/L. The highest level appeared in over 40 age group (1600.84 IU/L) ( and ).
Antibody levels and incidence of measles during 2000–2017
A seroepidemiologic surveillance of measles has been carried out every few years in Beijing ever since the 1970s and the involved population and laboratory methods fixed since 2003. This provides background evidence of the periodic changes in seropositivity and incidence rates of measles. The seropositivity rates (non-standardlized) in 2003, 2007 and 2012 were 73.38%, 91.57% and 83.88% respectively and the incidence of measles between 3.9 and 244.5 per million during 2000–2017 ().
Discussion
Although the elimination level has not yet been achieved, a declining trend of measles incidence can be seen in Beijing over these years, resulting in a historical lowest level in 2017. The key point is whether this downward trend will keep going continuously until measles is fully eliminated. In the present study’s representative sample of the Beijing population, the overall standardized seropositivity rate of measles was 84.61% (95% CI 84.12–87.10%) in 2017, which approaching the survey in 2012 and lower than 2007 and that was just consistent with the changes of measles incidence in these years in Beijing. It was also similar to the rates found in other provinces in China with a range of 80–96%,Citation11–Citation13 but lower than the rates in US during 1999–2004 (95.9%),Citation14 a country which had declared it had eliminated the ongoing transmission of measles in 2000. According to the threshold of 93–95% that is needed for stopping measles transmission,Citation15 it probably can be concluded that the population immunity level of Beijing currently is not yet able to achieve the elimination criteria and further population immunity is still needed.
In terms of different age groups, the present study showed that the seropositivity rate of infants <1 year was just 34.42% (95% CI 32.41–36.43%), which was much lower than other age groups. This is consistent with the data that shows that the main cases are infants in Beijing.7,Citation16 It is noteworthy that the seropositivity rate of infants less than 7 months old, who had not yet reached the initial vaccination age of measles vaccine, was only 9.38% (95% CI 8.15–10.61%). At present, the recognized measure of measles control for children under immunized age is through the establishment of a high level of herd immunity to prevent and control the transmission of measles and reduce the existence of infectious sources In the meantime, measures need to be taken to reduce virus exposure opportunities for these individuals.Citation17 An important measure is to encourage child family members to be vaccinated to protect vulnerable infants from infection. After reaching immunization age of 8 months, the seropositivity rate of 8–11 months old was still lower than it should be. In the 8–23 months old age range nearly 10% subjects had not yet had t MCV, so the timeliness of vaccination should be emphasized in routine immunization program.
The seroprevalence in children increased and reached a peak at 94.06% (95% CI 93.06–95.06%) in 1–4 years old group has reached the threshold of 93–95% that is needed for stopping transmission. And next were 5–9 years old group and 40- years old group which both above 90%. It demonstrated that virus may transmit difficultly in those groups.
The cases of adults are also a problem we have faced in Beijing in recent years. There was a lower level of antibody seen in adults aged 30–39 years old, which seropositivity rates below 80%. Compared with the survey in 2012, a backward shift occurred (from around 20–29 years old in 2012 to 30–39 years old in 2017).Citation18 These groups of people were born approximately 1978–1988, just in the initial stage of the national Expanded Program on Immunization (EPI) which began in 1978. This group probably neither had effective vaccination nor natural infection. Considering the complexity of MCV vaccination for adults, it is recommended to carry out a supplementary immunization strategy for certain groups and areas, such as universities, military camps, health care institutions, large factories, prisons and other susceptible groups, instead of a large-scaled nationwide immunization activity.Citation19
Since the mid 1990s, the migrant population from other provinces has become the main group to have measles in Beijing, both the proportion of cases and the incidence rate were a few times higher than those of the native population.7,Citation20,Citation21 But in recent years, with the implementation of immunization strategies targeted at the migrant population in Beijing, the incidence and immunity level of the migrant population have gradually come close to the native population. The efficient strategies included free measles vaccination for migrant workers aged ≤40 years old and freshmen in University, as well as SIAs among migrant pre-school children. Furthermore, there was a great development of the EPI in China and a number of catch up MCV SIAs in each province covering all of 1995–2009 birth cohort of China (some provinces covered birth cohort from 1991),Citation22 which resulted in a considerable reduction of the number of people susceptible to measles. The outcome of this survey showed there was no significant difference in antibody level between the native population and the migrant population from other provinces. Another cosmopolitan Chinese city, Shanghai presented a similar transformation.Citation23
The present study has several limitations. Firstly, when selecting the respondents in the final step at the survey site, they were not enrolled randomly, which may result in selection bias. Secondly, the data regarding vaccination status of adults and all history of measles infection were collected by recall, so the the reliability of measles infection/vaccination history were not sure and recall bias were probably unavoidable.
In conclusion, this study demonstrated that the seroprevalence of measles antibody in Beijing has not yet met the threshold of measles elimination. With the accumulation of susceptible individuals, there is still a risk of an epidemic of measles. The main high risk populations are <1 years old and 30–39 years old population. Appropriate targeted immunization strategies and measures should be considered and carried out.
Material & methods
Study population
The study was conducted from April to June 2017. We selected 8/16 districts of Beijing using a multi-stage stratified sampling method based on the geographical location and demographic characteristics. 10 villages/communities were selected from each district using a systematic sampling method. Individuals who had resided in the study area for at least 6 months were selected by convenience sampling. The subjects would be excluded if he refused or did not respond. All subjects were divided into 10 age groups (<1, 1–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, ≥40 years) according to the pre-defined sample size. Native residents/migrant residents were controlled by 0.9–1.1 in each group. The calculation of sample size was based on the formula: . The positive rates of antibody were assumed at 50% (π = 50%) for each age group in both genders. A minimum sample size of 192 was required for each age group, with confidence level of 95% (a = 0.05) and an absolute precision of 10% (δ = 10%). Therefore, more than 200 subjects were enrolled for each age group, resulting in a total of 2144 subjects.
Vaccination history
History of vaccination against measles was obtained from recall for subjects older than 14 years. Information for children less than 14 years old was extracted from the Beijing Immunization Program Management Information System.
Disease history
History of measles was collected using questionnaire by asking whether the subjects had been diagnosed with measles by a medical institution.
Laboratory methods
2ml venous blood sample was collected from each subject and centrifuged for 10 minutes under 1500–2000 r/min, then got no less than 1ml serum samples stored at −20°C. ALL samples were tested at the laboratory of Beijing Centers for Disease Control and Prevention (CDC), a WHO-accredited laboratory that attained a perfect score on WHO’s proficiency testing (PT) program in 2016.Serum samples obtained were tested for measles virus–specific immunoglobulin G (IgG) with commercial ELISA kits (Euoimmun Medizinische Labordiagnostika AG, Germany) of the same lot number. According to the kit instruction, seropositivity for measles IgG was defined as an IgG concentration ≥275 IU/L, seronegativity was defined as a concentration <200 IU/L, ≥200 – <275IU/L was considered gray area and were categorized as negative when calculating seropositivity rates.
Statistical analysis
The database was set up using Epidata 3.1 software. Data analysis was performed using SPSS 19.0 software. 95% confidence intervals (CI) were calculated for the seropositivity rates for each group. Standardized population data from Beijing Statistical Yearbook 2017 were calculated for standardized seropositivity rates.Citation24 Medians were used to describe the concentrations of measles IgG as they did not conformed to normal distribution. According to measles recurs in epidemic cycles at 4- year intervals in Beijing,Citation16 a 4-year moving average incidence of measles in Beijing was calculated and compared with the seropositivity rates. The differences in the level of IgG antibodies between different groups were tested by rank sum test. The chi-square test was used to compare the seropositivity rates by different groups. A p value <0.05 was considered statistically significant.
Disclosure of potential conflicts of interest
No potential conflict of interest were disclosed.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We are grateful to the efforts made by staff of district centers for disease control and prevention in Beijing involved in this study, including Dongcheng District CDC, Caoyang District CDC, Haidian District CDC, Tongzhou District CDC, Changping District CDC, Daxing District CDC, Huairou District CDC and Yanqing District CDC. We also thank those participants who took part in the study and provided the samples.
References
- World Health Organization. Expanded programme on immunization: measles and hepatitis B. http://www.wpro.who.int/rcm/en/archives/rc54/rc_resolutions/wpr_rc54_r03.htm.
- English AI. Progress towards the 2012 measles elimination goal in WHO’s Western Pacific Region, 1990–2008[J]. Wkly Epidemiol Rec. 2009;84:271.
- Song QW, Su QR, Ma C, Hao LX, Wang HQ. Spatial autocorrelation analysis of measles in China, 2005–2014[J]. Zhonghua Yu Fang Yi Xue Za Zhi. Chinese J Preventive Medicine. 2016;50(7):615–19. doi:10.3760/cma.j.issn.0253-9624.2016.07.010.
- World Health Organization. Regional office for the Western Pacific. Measles-Rubella Bull. Jan. 2018;12(1). http://iris.wpro.who.int/handle/10665.1/14006.
- Aspects G. Global measles and rubella strategic plan, 2012–2020 [J]. Genet Aspects. 2012:16.
- National Bureau of statistics. Main data bulletin of the sixth national census of Beijing in 2010. 2012 Feb 28. http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/dfrkpcgb/201202/t20120228_30381.html.
- Li J, Lu L, Liu DL, Ma R, Wu J, Pang XH. Measles epidemiology and elimination measure evaluation in Beijing, 2005–2010[J]. Dis Surveillance. 2012;46(9):353–57.
- Gay NJ. The theory of measles elimination: implications for the design of elimination strategies[J]. J Infect Dis. 2004;189(1):27–35. doi:10.1086/381592.
- Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52(7):911–16. doi:10.1093/cid/cir007.
- Hethcote HW. Measles and rubella in the United States. Am J Epidemiol. 1983;117:2–13. doi:10.1093/oxfordjournals.aje.a113511.
- Gidding HF, Quinn HE, Hueston L, Dwyer DE, McIntyre PB. Declining measles antibodies in the era of elimination: Australia’s experience[J]. Vaccine. 2018;36(4):507. doi:10.1016/j.vaccine.2017.12.002.
- Mcquillan GM, Kruszonmoran D, Hyde TB, Forghani B, Bellini W, Dayan GH. Seroprevalence of measles antibody in the US population, 1999–2004[J]. J Infect Dis. 2007;196(10):1459–64. doi:10.1086/522866.
- Tang J. Current status of serological research on measles antibody [J]. J Public Health Prev Med. 2010;21:48–49.
- Tang L, Zhou Y, Pan Y, Zhu H. Measles epidemics and seroepidemiology of population in Wujin, Changzhou city, Jiangsu province, China 2015[J]. Vaccine. 2017;35(22):2925–29. doi:10.1016/j.vaccine.2017.04.018.
- Orenstein WA, Gay NJ. The Theory of Measles Elimination: implications for the Design of Elimination Strategies [J]. J Infect Dis. 2004;189(1):27–35. doi:10.1086/381592.
- Zhang ZJZ, Suo LD, Ma R, Li J, Pan JB, Lu L. Epidemiological characteristics of measles in Beijing, 2011–2016[J]. International Journal of Virology. 2018;25(2):32–36. doi: 10.3760/cma.j.issn.1673-4092.2018.02.008
- Leuridan E, Sabbe M, Van DP. Measles outbreak in Europe: susceptibility of infants too young to be immunized.[J]. Vaccine. 2012;30(41):5905–13. doi:10.1016/j.vaccine.2012.07.035.
- Li J, Lu L, Chen M, Huang F, Zeng Y, Li X-M, Ma R, Pan J-B, Sun M, Sun H, et al. [Analysis of measles immunity level in persistent populations in Beijing, 2012][J]. Chinese J Preventive Medicine. 2013;47(10):916–919.
- Su QR, Xu AQ, Strebel P. National and international experts’ consensus on key technical issues of measles elimination in China[J]. Chinese Journal of Vaccines & Immunization. 2014(3):264–270.
- Lu L, Gu Y, Sun M. Epidemic characteristics of measles outbreak in floating population in Beijing and its control strategy[J]. Chin J Vaccines Immunization. 1999(2):69–71.
- Liu DL, Sun MP, Yang J. Analysis of epidemiology for measles in Beijing in 2003[J]. Chin J Vaccines Immunization. 2005, 11(1):30–32. doi: 10.3969/j.issn.1006-916X.2005.01.010.
- Ma C. Epidemiology of measles in China and immunization strategies for measles elimination[D]. Beijing, China: China Center for Disease Control and Prevention; 2014.
- Gao J. Investigation of measles antibody level of healthy people in Jing’an district of Shanghai City [J]. Chin J Dis Control Prev. 2010, 14(7):641–643.
- Beijing Statistics Bureau. Beijing statistical yearbook 2017[M], Beijing, China. 2018.