ABSTRACT
Background and method: Despite their proven effect, the rates of vaccinations are low. The aim of this study was to determine the rates and associated factors of influenza and pneumonia vaccinations in patients who were hospitalized because of acute respiratory failure. Patients hospitalized because of acute hypoxemic or hypercapnic respiratory failure were recruited for this retrospective study. A survey was conducted with 97 patients. Primary diagnoses, ages, reasons of hospitalizations, education status, vaccination rates, information resources, and thoughts about vaccinations were recorded.
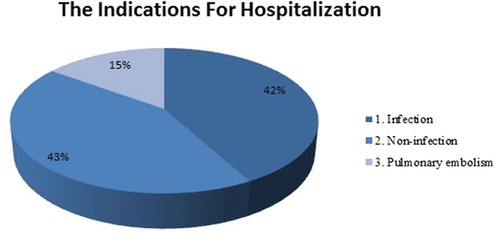
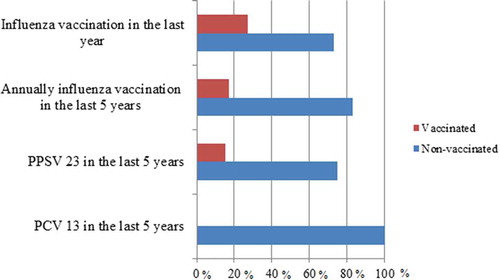
Results: In total 45 (46%) of the patients were female, and 52 (54%) were male. The mean age was 67 ± 12 years. The primary diagnoses were lung disorders (n = 77, 79%), cardiac disorders (n = 16, 17%), and neuromuscular disorders (n = 5, 4%). In total 72 (74%) patients had chronic obstructive pulmonary disease (COPD) with primary lung disorders. All patients were hospitalized due to acute respiratory failure. The main reason for acute respiratory failure was infection in 40 patients (42%). The overall influenza and pneumococcal vaccination rates were 26% and 15%, respectively; for patients with COPD it was 30% and 17%, respectively. The main providers of information were doctors (42%). Vaccination status was not associated with infections or other reasons of hospitalization, age, sex, educational status, and number of hospital admissions in the previous year. A total of 51 patients (52%) had no belief in the benefits of vaccinations.
Conclusion: Vaccination rates were found to be low in patients who were frequently hospitalized. Vaccination status was not related with hospitalization due to infections and history of hospitalization; awareness of vaccinations should be improved both in doctors and patients.
Introduction
The number of patients with chronic disease and the elderly population have an increasing trend all around the world. With this increase, healthcare costs and morbidity and mortality increase even more. Influenza and pneumococcal infections are one of the most important reasons for hospitalization and death in the elderly and patients with chronic disease. Most deaths due to influenza were found to occur among individuals aged over 65 years, especially those aged over 80 years with health problems living in care facilities for the elderly.Citation1 Vaccines are the only preventive medical tools available for reducing the risk of influenza infection, pneumococcal pneumonia, and the burden of disease in these patients.Citation2–Citation4 Approximately 50,000 adults die from vaccine-preventable diseases in the United States of America (USA) each year. Vaccine-preventable diseases, especially influenza infection, and pneumococcal pneumonia have been shown to be great expensive.Citation5 As a result, many strategies have been established and target rates have been determined. In 2003, the World Health Assembly (WHA) stated that it aimed to determine and apply strategies to increase influenza vaccination coverage of all people at high risk, including the elderly and persons with diseases, with the goal of attaining vaccination coverage of at least 75% in the elderly population by 2010.Citation6 Furthermore, the European Commission recommended enhancing the number of vaccinations among healthcare workers.Citation7 The World Health Organization (WHO) also recommends vaccinations for people at increased risk.Citation8 Health statistics data show that the influenza vaccination rates in America between 1999 and 2005 were 70% at the most, and the pneumococcal vaccination rates were <60%.Citation9 It was found that the influenza vaccinations’ rate of Turkey was 27.9% among people aged 65 years in two different studies.Citation10 In another study conducted in Turkey, during the last five years, only 27% and 9.8% of patients with diabetes mellitus were received influenza and pneumococcal vaccines.Citation11 Despite these recommendations and proven effects, vaccination rates are still low in Turkey. In June 2016 The Ministry of Health of Turkey identified risk groups in vaccine-preventable diseases, and started to apply immunization programs smiliar to the consensus of the Immunization Advisory Committee, consisting of adult vaccinations compatible with those of the updated U.S. Advisory Committee on Immunization Practices (ACIP) recommendations.Citation12,Citation13 Additionally, the surveillance of invasive pneumococcal diseases, which will be started in Turkey with a recently published circular, is included in the scope of the Program on Survival of Preventable Invasive Bacterial Diseases.Citation14
The aim of this study was to determine the rates, compliance factors with vaccinations, and effects of vaccination on hospitalization and emergency admission in the previous year in patients who were hospitalized because of acute respiratory failure.
Results
A total of 45 (46%) patients were female and 52 (54%) were male. The mean age of the patients was 67 ± 12 years. In total 73 (75%) patients were married, 24 (25%) were single. In total 51 (53%) patients had history of smoking with a median value of 15 pack-years (min: 0, max: 150). A total of 53 (55%) patients had graduated from primary school, 4 (4%) from middle school, 8 (8%) from high school, and 3 (3%) from university; 5 (5%) had no formal education schools but were literate and 24 (25%) were illiterate. The primary diagnoses were lung disorders (n = 77, 79%), cardiac disorders (n = 16, 17%), and neuromuscular disorders (n = 4, 4%) (). A total of 72 (74%) patients had COPD with primary lung disorders. The median FEV1 value in patients with COPD was 36 (min: 13, max: 91), FVC was 42 (min: 16, max: 99) and FEV1/FVC was 70 (min: 30, max: 70) of percent predicted. Other primary lung diseases were kyphoscoliosis, history of tuberculosis with sequelae, obesity-hyperventilation, and asthma.
Table 1. Demographic features of all patients.
All patients had acute hypoxemic or hypercapnic respiratory failure on admission to hospital. The indications for hospitalization were infection (n = 40, 42%), non-infectious reasons such as non-adherence to treatment and social problems that resulted in acute respiratory failure (n = 41, 43%), and pulmonary embolism (n = 16, 15%) (). In patients hospitalized with infections, sputum culture results were normal flora (n = 19, 47%), P. Aeruginosa (n = 5, 13%), M. Cataralis (n = 3, 8%), H. Influenzae (n = 2, 5%), S. Pneumonia (n = 2, 5%); other pathogenic agents were S. Aureus, S. Marcenses, E. Coli, E. Aerogenes, E. Cloacae, and A. baumannii. Nasopharyngeal swab tests were performed when viral infections were considered. No patients had positive nasopharyngeal swab tests. In the assessment of chest X-ray findings, in patients hospitalized with infections, 31 (32%) of them had consolidation, 9 (9%) had reticulonodular/nodular infiltration, in other patients 45 (46%) patients had normal findings and 12 (13%) had pleural effusion.
Two (2%) patients had no history of hospitalization in the last year. A total of 61 (63%) patients were hospitalized once, and 34 (35%) patients were hospitalized twice or more. Nine (9%) patients had no history of emergency department admission in the last year, 39 (40%) patients one, and the remainder had two and more emergency department admissions because of infection or acute exacerbation of primary disease.
A total of 26 (27%) patients received influenza vaccinations in the last year and 17 (18%) were vaccinated annually for the last 5 years. In total 15 (15%) patients had polysaccharide pneumococcal vaccinations (PPSV23), and none received conjugate pneumococcal vaccines (PCV13) in the last 5 years (). Eight (8%) patients, all of whom had diagnoses of COPD, had an influenza vaccination in last year and PPSV23 in the last 5 years. Among the patients with COPD, 22 (30%) patients were vaccinated against influenza in the previous year and 12 (17%) had pneumococcal vaccinations (PSSV23) in the last 5 years.
A total of 41 (42%) patients received information about vaccinations from doctors, 5 (5%) from healthcare personnel, (7%) 7 from the media, and 7 (7%) from relatives; the others (39%) had not received any information about vaccines. A total of 29 (30%) patients believed in the effectiveness of vaccines; however, 51 (52%) had no belief and 17 (18%) had no certain ideas about vaccination.
Pneumococcal and influenza vaccination status was not associated with age (p = .223, p = .188), sex (OR 1.3; 95% CI:[0.4–4.1]; p = .589 and OR 1.5; 95% CI:[0.6–3.8]; p = .343), being married (OR 1.3; 95% CI:[0.3–5.3]; p = .643 and OR 5.3; 95% CI:[1.1–24.8]; p = .019), smoking status (p = .398, p = .033), history of being former smoker (OR 0.7; 95% CI: [0.2–2.2]; p = .618 and OR 3.3; 95% CI: [1.2–8.8]; p = .014), amount of cigarette smoking (p = .059, p = .203), educational status in terms of being illiterate (OR 0.1; 95% CI: [0.02–1.4]; p = .078 and OR 0.3; 95% CI: [0.08–1.1]; p = .068), infections or other reasons for hospitalization (p = .607, p = .297), hospitalization due to infection (OR 1.2; 95% CI: [0.4–3.9]; p = .642 and OR 1.3; 95% CI: [0.5–3.2]; p = .552), primary lung disease (OR 3.7; 95% CI: [0.4–30.3]; p = .192 and OR 3.5; 95% CI: [0.7–16.6]; p = .091), and history of hospitalization (p = .182, p = .330) or admission to the emergency service (p = .410, p = .615) in the last one year ( and ).
Table 2. Recorded parameters in patients received PPSV23 in the last 5 years.
Table 3. Recorded parameters in patients received influenza vaccinations in the last year.
Discussion
This study showed that among inpatients with a history of frequent emergency department admission and hospitalization, the rate of influenza vaccination was 26% in the last year, and with lower rates for both regular influenza and polysaccharide pneumococcal vaccinations (17% and 15%, respectively) in the last 5 years. Eight percent of patients received both vaccines. The rates were also similar among patients with COPD. Vaccination status was not associated with age, sex, active smoking, infections or other reasons of hospitalizations, educational status, primary disease, and history of hospitalization or admission to the emergency department in the last one year. Former smokers and married patients were vaccinated against influenza more frequently. Furthermore, it was shown that vaccination was only recommended to 42% of patients by doctors, and most patients did not believe in the effectiveness of vaccinations.
The target rate of vaccination for patients with indications for vaccination is 80–90%.Citation15 Studies have shown lower rates against both influenza and pneumococcal infections. A recent study in which a total of 552.942 adults aged 19–64 years with chronic conditions were identified, it was found that 20% of adults who were newly diagnosed as having one of four chronic conditions received a pneumococcal vaccination after 5 years of follow-up in the USA.Citation16 In another recent study, the influenza vaccination rate was found as 53% among patients with COPD.Citation17 In Turkey in 2011, the rate of influenza vaccination in the previous year was 37%, and the rate of pneumococcal vaccination at least once was 15% in patients with COPD.Citation18 In one single-center study, both pneumococcal and influenza vaccination rates were 51%.Citation19 In a recent multi-center study from Turkey, the influenza and pneumococcal vaccination rates were 36.5% and 14.1% in patients with COPD, respectively.Citation20 Similarly, in our study, the influenza vaccination rate was 26% in the previous year, and 17% had been vaccinated annually in the last 5 years. The PPSV23 rate was 15% and none had received PCV13 in the last 5 years. In patients with COPD, the influenza vaccination rate was 30% and PSSV23 was 17%. The rate of vaccinations in other countries was found higher than in our study, but similar to our national rates. We suggest that the reason for the lack of vaccinations with PCV13 was that reimbursement only began two years ago in Turkey.
Factors that could affect vaccination rates have been investigated in several studies. Influenza vaccination rates were found higher in patients who had more frequent contact with their medical practitioners.Citation21 However, in another study that aimed to determine pneumococcal vaccination rates and affecting factors in patients with COPD, it was found that the number of general practitioner visits did not affect vaccination rates.Citation22 In our study, the rates were lower in spite of frequent emergency department admissions and hospitalizations. This could be linked to low recommendation rates. It was seen that approximately half of the patients were recommended vaccination by doctors and healthcare personnel. We suggest that the awareness of the benefits of vaccines should be increased in both patients and healthcare professionals. The number of educational programs could be increased among health professionals.
Other possible predisposing factors have been found to decrease vaccination rates were being Black or Hispanic. It was reported that patients of older age, former and never smokers, and those with health insurance had higher vaccination rates.Citation17 There are inconsistent data in which some studies found that sex did not affect vaccination rates, whereas others showed higher vaccination rates among women.Citation19,Citation23–Citation26 Additionally, being married was shown to have a positive effect on vaccination rates, whereas other studies failed to determine a relation with marital status.Citation6,Citation24 In another study, a high level of education among elderly patients with COPD was found to negatively affect vaccination rates.Citation6 Other studies have indicated that higher educational levels improved vaccination rates.Citation20,Citation26–Citation28 In our study, being married or a former smoker seemed to be positive factors for vaccination, whereas sex and education were not related with vaccination. It was suggested that being married and a former smoker could represent better lifestyle and self-care, but the non relationship between education and vaccination could be due to a lack of belief in the benefit of vaccines.
The results of vaccination have been investigated in several studies. Although there was insufficient evidence to prove the effectiveness of pneumococcal vaccines against all-cause pneumonia among adults in several meta-analysis,Citation29,Citation30 influenza, and pneumococcal vaccines have been shown to reduce hospital admissions, hospital stay duration, severe complications such as sepsis, and inpatient mortality in the elderly.Citation31–Citation36 In a multicenter study conducted in Turkey on hospitalized patients with community-acquired pneumonia, the influenza and pneumococcl vaccination rates were 10% and 3%, respectively, and the vaccination rate with both pneumococcal and influenza vaccines was found as 6%. Vaccinated patients had less consolidation in chest radiographs and were less symptomatic. However, the 30-day mortality and lower rates of intensive care unit (ICU) admission did not reach statistical significance between the vaccinated and unvaccinated groups. It was concluded that previous vaccination did not seem to significantly affect the clinical outcomes.Citation37 In our study, 8% patients had both vaccines, history of hospitalization in the last year, reasons for hospitalization, and even infection were not found to be related with vaccination. We assume that the reason for the lack of relationship between hospitalization for infection and vaccination could be linked to the fact that besides the low number of patients, the etiologic agents were heterogeneous.
The possible and most important reasons for non-vaccinations shown in previous studies were a lack of belief in the benefit of vaccination and believing that vaccines triggered flu and adverse effects.Citation20,Citation38 In our study, the most important reason for non-vaccination was a lack of belief in vaccination, and 17% of patients had no certain idea about vaccines; however the patients had a frequent history of hospital addmission. We suggest that, to increase the belief in vaccination, both healthcare professionals and patients should be educated and the knowledge of the benefits of vaccination. In a recent study conducted in Turkey, it was shown that the influenza vaccination rate was 26.7% in healthcare professionals and one of the reasons for unvaccination was insufficient knowledge about vaccination.Citation39
The limitations of our study were the limited number of patients and the heterogeneous group owing to it being a cross-sectional study. In addition, although prescription, pharmacy, and hospital records were required in the history of vaccination, it is hard for patients to remember five-year period in terms of being accined or not and type of vaccine. Another limitation of the study was using nasopharyngeal swabs via only multiplex PCR and only for influenza A and B. It has been shown that identifing the viruses in nasopharyngeal swabs does not always present lower respiratory infections. In a study it was demonstrated that detection of viruses could be as low as 23.1% in patients with pneumonia despite of using sputum samples tested by multiplex PCR.Citation40 If multiple tests which could detect other kinds of viruses had been used, hospitalized patients due to viral infections would have been revealed. The results cannot be generalized because this was a single-center study. Further randomized controlled and multicentered studies are needed to explore the rates of vaccinations and related factors in patients hospitalized due to acute repiratory failure.
Material-method
Study design: observational cross-sectional study.
Patient Characteristics: Patients hospitalized because of acute hypoxemic or hypercapnic respiratory failure were recruited for the study between December 2016 and December 2017 in the respiratory failure service of a tertiary referral chest disease hospital in the capital city of Turkey. The patients received the survey according to the inclusion and exclusion criteria. The inclusion criteria were: having a history of chronic respiratory disease, chronic respiratory failure, cardiovascular disease or cigarette smoking for at least five years. Patients who were not able to give a history were uncooperative, unconscious, or did not want to participate in the survey were not included in the study. Patient and instructional review board approval were obtained before the study began.
Recorded parameters: the survey form, which questioned the number of influenza and pneumococcal vaccinations (both polysaccharide and conjugate) in the last one and five years, information sources, thoughts about vaccinations, and number of hospitalizations and emergency admissions in the previous year was given to eligible patients. The survey was administered by the same nurse. Primary diagnosis, age, reasons for hospitalization, education status, parameters of survey, and sputum culture results were recorded.
History of hospitalizations, emergency admissions, and vaccinations, which were obtained from the patients’ declarations, were also confirmed by our hospital records, prescriptions, and discharge reports from other hospitals.
COPD diagnoses were confirmed according to the Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) guideline.Citation41 Spirometry was performed to determine the forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and FEV1/FVC using a spirometer (AS-507, Minato Medical Science, Tokyo, Japan), in accordance with the ATS/ERS guidelines.Citation42 Pulmonary fuction tests were performed after bronchodilator treatment immediately before discharge from hospital, and in the morning in each patients with COPD patients. All patients with COPD were under triple-treatment containing long-acting beta agonists, long-acting muscarinic antagonists, and inhaler corticosteroids.
Diagnosis of infection was confirmed by history (such as cough, dyspnea, pleuritic pain, acute functional, cognitive decline, fever, tachycardia, and lung examination findings), laboratory tests such as high serum C-reactive protein (CRP) levels, procalcitonin, white blood cell counts, and positive chest X-ray findings with/without positive sputum or swab culture results.Citation43 Urinary antigen testing was not performed. Nasopharyngeal swabs were taken by the same doctor using a standard sterile culture rod with a rayon, dacron, or synthetic fiber tip. Multiplex PCR Assay was performed to discriminate viral pathogens (influenza A and B) via GeneXpert® System (Cepheid, Sunnyvale, CA, USA).
Plasma CRP, procalcitonin, and white blood cell counts were measured using a commercially available blood analyzer (Architect C8000, Abbott, Illinois, USA.)
Statistical analysis: SPSS version 18.0 (SPSS, Inc., Chicago, USA) for Microsoft Windows (Microsoft Corporation, Redmond, Washington) was used for statistical analysis. Variables were analyzed using the Shapiro-Wilk test to evaluate distribution. Results for descriptive statistics are expressed as mean ± standard deviation or median (minimum:maximum). Categorical variables are expressed as numbers and percentages (%). The Mann–Whitney U test was used to compare differences between two independent groups when the dependent variable was abnormally distributed and ordinal or continuous, and the Chi-square test was used to test relationships between categorical variables. Statistical significance was accepted as p < .05.
Conclusion
Influenza and pneumococcal vaccination rates were found to be lower than expected even in patients with chronic illness who had frequent hospital admissions. Despite frequent contact with doctors and healthcare personnel, these patients may not be aware of vaccines and the benefits of vaccination. These results show the importance of recommendations by the healthcare professionals. Clear affecting factors were not revealed; however, being married or a former smoker could be positive factors. The most important issue is with regards education about vaccination for both doctors and patients; increasing the knowledge of both will enhance vaccination rates. The education of health care professionals seems to be more important. Further strategies should be implemented and the frequency of education programs should be increased.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- Nicholson KG, Wood JM, Zambon M. Influenza. Lancet. 2003;362:1733–45. doi:10.1016/S0140-6736(03)14776-9.
- Hak E, Nordin J, Wei F, Mullooly J, Poblete S, Strikas R. Influence of high-risk medical conditions on the effectiveness of influenza vaccination among elderly members of 3 large managed-care organizations. Clin Infect Dis. 2002;35:370–77. doi:10.1086/341403.
- Mangtani P, Cumberland P, Hodgson CR, Roberts JA, Cutts FT, Hall AJ. A cohort study of the effectiveness of influenza vaccine in older people, performed using the United Kingdom general practice research database. J Infect Dis. 2004;190:1–10. doi:10.1086/423326.
- Blank PR, Szucs TD. Increasing influenza vaccination coverage in recommended population groups in Europe. Expert Rev Vaccines. 2009;8:425–33. doi:10.1586/erv.09.7.
- National Foundation for Infectious Disease. 10 reasons to be vaccinated. [Accessed 17. Apr.12]. http://www.adultvaccination.org/10-reasons-to-be-vaccinated?css=print.
- World Health Assembly. Prevention and control of influenza pandemics and annual epidemics; 2003 Fifty-sixth World Health Assembly: Resolution WHA56.19. [Accessed 17. Apr.12]. http://www.evm-vaccines.org/pdfc/wha resolution ipd.pdf.
- Council recommendation of 2009 on seasonal influenzal vaccination. Official Journal of the European Union. L 348/71. 29.Dec.2009. [Accessed 17. Apr.12]. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2009:348:0071: 0072:EN:pdf.
- World Health Organization. Vaccine use. 2012; [Accessed 17. Apr.12]. http://www.who.int/influenza vaccines/use/en/
- Centers for Disease Control and Prevention (CDC). Influenza and pneumococcal vaccination levels among persons aged > or =65 years – United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:532–37.
- Oncel S, Turhan O, Huseyin PH, Yalcin AN. Status of influenza vaccination in patients presenting to two neighborhood primary health care clinics in Antalya. Infez Med. 2008;16:74–79.
- Satman I, Akalin S, Cakir B, Altinel S, diaVAX Study Group. The effect of physicians‘ awareness on influenza and pneumococcal vaccination rates and correlates of vaccination in patients with diabetes in Turkey: an epidemiological Study “diaV X”. Hum Vaccin Immunother. 2013;9:2618–26. 10.4161/hv.25826
- Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices—United States, 2018–19 influenza season. Recommendations and Reports. 2018 August 24;67(3):1–20. doi:10.15585/mmwr.rr6703a1.
- Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61(40):816–19.
- Şenol E, Azap A, Erbay A, Alp-Çavuş S, Karakuş R, Acar A. Pneumococcal vaccine as one of the immunization coverage targets for adulthood vaccines: A consensus report of the Study Group for Adult Immunization of the Turkish Society of Clinical Microbiology and Infectious Diseases. Klimik Derg. 2018;31(1):2–18. Turkish. doi:10.5152/kd.2018.2.
- Healthy people 2020. immunization and infectious diseases, objectives;.2010 Office of Disease Prevention and Health Promotion. USDHHS. [cited 2011 May 25]. Available from: http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- Petigara T, Zhang D. pneumococcal vaccine coverage in adults aged 19–64 years, newly diagnosed with chronic conditions in the US. Am J Preven Med. 2018;54:630–36. doi:10.1016/j.amepre.2018.01.033.
- Arabyat RM, Raisch DW, Bakhireva L. Influenza vaccination for patients with chronic obstructive pulmonary disease: implications for pharmacists. Res Social Adm Pharm. 2018;14:162–69. doi:10.1016/j.sapharm.2017.02.010.
- Özsu S, Uçar E, Arslan Y, Maden E, Bilgiç H. The frequency of influenza and pneumococcal vaccination in COPD. Solunum Dergisi. 2011;13:21–25. doi:10.5505/solunum.2011.88155.
- Cimen P, Unlu M, Kirakli C, Katgi N, Ucsular FD, Ayranci A, Guclu SZ. Should patients with copd be vaccinated? Respir Care. 2015;60:239–43. doi:10.4187/respcare.03350.
- Aka Aktürk Ü, Görek Dilektaşlı A, Şengül A, Musaffa Salepçi B, Oktay N, Düger M, Arık Taşyıkan H, Durmuş Koçak N. Influenza and pneumonia vaccination rates and factors affecting vaccination among patients with chronic obstructive pulmonary disease. Balkan Med J. 2017;34:206–11. doi:10.4274/balkanmedj.2016.1028.
- Chiatti C, Barbadoro P, Marigliano A, Ricciardi A, Di Stanislao F, Prospero E. Determinants of influenza vaccination among the adult and older Italian population with chronic obstructive pulmonary disease: a secondary analysis of the multipurpose ISTAT survey on health and health care use. Hum Vaccin. 2011;7:1021–25. doi:10.4161/hv.7.10.16849.
- Arinez-Fernandez MC, Carrasco-Garrido P, Garcia-Carballo M, Hernandez-Barrera V, de Miguel AG, Jimenez-Garcia R. Determinants of pneumococcal vaccination among patients with chronic obstructive pulmonary disease in Spain. Hum Vaccin. 2006;2:99–104.
- Montserrat-Capdevila J, Godoy P, Marsal JR, Cruz I, Solanes M. Effectiveness of influenza vaccination in preventing hospital admission due to exacerbations of chronic obstructive pulmonary disease. Enferm Infec Microbiol Clin. 2014;32:70–75. doi:10.1016/j.eimc.2013.02.009.
- Damiani G, Federico B, Visca M, Agostini F, Ricciardi W. The impact of socioeconomic level on influenza vaccination among Italian adults and elderly: a cross-sectional study. Prev Med. 2007;45:373–79. doi:10.1016/j.ypmed.2007.07.007.
- Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;7:4018–24. doi:10.1016/j.vaccine.2009.04.029.
- Ford ES, Mannino DM, Williams SG. Asthma and influenza vaccination: findings from the 1999–2001 National Health Interview Surveys. Chest. 2003;124:783–89.
- Lu PJ, Singleton JA, Rangel MC, Wortley PM, Bridges CB. Influenza vaccination trends among adults 65 years or older in the United States, 1989–2002. Arch Intern Med. 2005;165:1849–56. doi:10.1001/archinte.165.16.1849.
- Jiménez-García R, Hernández-Barrera V, Carrasco-Garrido P, de Andrés AL, de Miguel Diez J, de Miguel A. Coverage and predictors of adherence to influenza vaccination among Spanish children and adults with asthma. Infection. 2010;38:52–57. doi:10.1007/s15010-009-9069-4.
- Schiffner-Rohe J, Witt A, Hemmerling J, von Eiff C, Leverkus FW. Efficacy of PPV23 in preventing pneumococcal pneumonia in adults at increased risk—a systematic review and meta-analysis. PLoS One. 2016;11:e0146338. doi:10.1371/journal.pone.0146338.
- Moberley S, Holden J, Tatham DP, Andrews RM. Vaccines for preventing pneumococcal infection in adults. The Cochrane Collaboration, editorCochrane Database Syst. Rev. Chichester (UK): John Wiley & Sons, Ltd; 2008. cited 2017 Oct 5. Available from10.1002/14651858.CD000422.pub2
- National Center for Health Statistics. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville (MD): US Government Printing Office; 2016.
- Simonsen L, Taylor RJ, Schuck-Paim C, Lustig R, Haber M, Klugman K. Effect of 13-valent pneumococcal conjugate vaccine on admissions to hospital 2 years after its introduction in the USA: a time series analysis. Lancet Respir Med. 2014;2:387–94. doi:10.1016/S2213-2600(14)70032-3.
- Fisman DN, Abrutyn E, Spaude KA, Kim A, Kirchner C, Daley J. Prior pneumococcal vaccination is associated with reduced death, complications, and length of stay among hospitalized adults with community-acquired pneumonia. Clin Infect Dis. 2006;42:1093–101. doi:10.1086/501354.
- Nordin J, Mullooly J, Poblete S, Strikas R, Petrucci R, Wei F, Rush B, Safirstein B, Wheeler D, Nichol KL. Influenza vaccine effectiveness in preventing hospitalizations and deaths in persons 65 years or older in Minnesota, New York, and Oregon: data from 3 health plans. J Infect Dis. 2001;184:665–70.
- Nichol KL, D’Heilly SJ, Greenberg ME, Ehlinger E. Burden of influenza-like illness and effectiveness of influenza vaccination among working adults aged 50–64 years. Clin Infect Dis. 2009;48:292–98. doi:10.1086/595842.
- Christenson B, Lundbergh P, Hedlund J, Örtqvist Å. Effects of a large-scale intervention with influenza and 23-valent pneumococcal vaccines in adults aged 65 years or older: a prospective study. Lancet. 2001;357:1008–11. doi:10.1016/S0140-6736(00)04237-9.
- Cetinoglu ED, Uzaslan E, Sayıner A, Cilli A, Kılınc O, Coskun AS, Hazar A, Kokturk N, Filiz A, Polatli M, the TURCAP Study Group 2017. Pneumococcal and influenza vaccination status of hospitalized adults with community acquired pneumonia and the effects of vaccination on clinical presentation. Hum Vaccin Immunother. 2017;13:2072–77. 10.1080/21645515.2017.1339851.
- Ciblak MA, Platformu G. Influenza vaccination in Turkey: prevalence of risk groups, current vaccination status, factors influencing vaccine uptake and steps taken to increase vaccination rate. Vaccine. 2013;31:518–23. doi:10.1016/j.vaccine.2012.11.022.
- Çiftci F, Şen E, Demir N, Çiftci O, Erol S, Kayacan O. Beliefs, attitudes, and activities of healthcare personnel about influenza and pneumococcal vaccines. Hum Vaccin Immunother. 2018;14(1):111–17. doi:10.1080/21645515.2018.1486156.
- Katsurada N, Suzuki M, Aoshima M, Yaegashi M, Ishifuji T, Asoh N, Hamashige N, Abe M, Ariyoshi K, Konosuke Morimoto and on behalf of the Adult Pneumonia Study Group-Japan. The impact of virus infections on pneumonia mortality is complex in adults: a prospective multicentre observational study. BMC Infec Dis. 2017;17:755. doi:10.1186/s12879-017-2858-y.
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2017; GOLD Updated. http://www.goldcopd.org
- Grassino A. (ATS co-chair), Moxham J (ERS co-chair) and subcommıttee of the assembly on respıratory structure and functıon.American Thoracic Society/European Respiratory Society Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624. doi:10.1164/rccm.166.4.518.
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, et al.; Infectious Diseases Society of America, American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(2):27.