ABSTRACT
Objectives: To assess the prevalence of hepatitis B virus (HBV) infection among married individuals and to analyze the associated risk factors of HBV infection in vaccinated and unvaccinated groups in 2006 and 2014.
Methods: Information of married individuals aged over 16 y with a clear HBV vaccination status was extracted from the database constructed by the Beijing Center for Disease Prevention and Control from population-based investigation.
A structured questionnaire was employed to collect demographic information, vaccinated history, and other related influence information of HBV of participants. Pearson chi-square test, Fisher's test, and logistic regression were used to explore the risk factors of HBV infection.
Results: A total of 2874 individuals in 2006 and 1622 individuals in 2014 were enrolled in our study. The mean age of individuals was 49.30 and 46.68 y in 2006 and 2014, respectively. The overall positive rates of HBsAg, anti-HBc, and single anti-HBs were 4.80%, 43.01%, and 5.78% in 2006, which were 4.69%, 38.22%, and 14.18% in 2014, respectively. For vaccinated individuals, age was significantly correlated with anti-HBc in 2014 (40 < age ≤50 versus age ≤30, relative risk (RR) = 3.03, 95% confidence interval (95%CI) = 1.04–8.84). Gender [male versus female, RR = 0.60, 95%CI = 0.36–1.00 (2006); RR = 0.71, 95%CI = 0.52–0.97 (2014)] and age (in 2006) were found to be significantly associated with single anti-HBs.
For unvaccinated individuals, HBsAg positivity was statistically significant correlated with gender [RR = 1.47, 95%CI = 1.04–2.06, in 2006], residence (urban versus rural, RR = 0.40, 95%CI = 0.24–0.67, in 2006; RR = 0.58, 95%CI = 0.34–0.99, in 2014), sharing syringes [RR = 3.75, 95%CI = 1.33–10.63 (in 2006); RR = 2.07, 95%CI = 1.26–3.41 (in 2014)], infected wives (RR = 1.97, 95%CI = 1.28–3.05, in 2006), and infected husbands (RR = 2.19, 95%CI = 1.25–3.82, in 2006). Anti-HBc positivity was significantly associated with gender [RR = 1.19, 95%CI = 1.10–1.30 (in 2006); RR = 1.24, 95%CI = 1.09–1.40 (in 2014)], age (in 2006 and 2014), endoscopic medicine treatment [RR = 1.16, 95%CI = 1.03–1.32 (in 2006), RR = 1.21, 95%CI = 1.01–1.45 (in 2014)], sharing syringes (RR = 1.43, 95%CI = 1.25–1.64, in 2014), body piercing (RR = 0.84, 95%CI = 0.75–0.93, in 2006), infected wives (RR = 1.32, 95%CI = 1.18–1.47, in 2006), and infected husbands (RR = 1.39, 95%CI = 1.22–1.59, in 2006). Anti-HBs positivity was associated with age (in 2006 and 2014).
Conclusions: Prevalence of HBV infection was lower in 2014 than in 2006 according to HBsAg and anti-HBc positivity. Unvaccinated individuals faced much more risk of HBV infection than those of vaccinated.
Introduction
As one of the most serious public health issues worldwide, hepatitis B virus (HBV) infection could cause lifelong chronic HBV carrier or lead to cirrhosis or hepatocellular carcinoma (HCC).Citation1,Citation2 It was estimated that HBV had affected at least 257 million people worldwide,Citation3 and about 90 million people suffered from HBV-related diseases in China.Citation4
Liver cancer and other chronic diseases caused by HBV could be effectively prevented by HBV vaccine. In order to control the ascending tendency of HBV infection, the World Health Organization (WHO) encouraged all member countries to popularize HBV vaccine immunization.Citation3 As one of the member countries with high HBV prevalence, China responded to WHO strategy actively by recommending HBV vaccine immunization for newborns in 1992 and took HBV vaccination into Expanded Program on Immunization (EPI) in 2002. HBV vaccination for newborns was free of charge after 2005.Citation5 China also launched a HBV vaccination project for adolescents and adults since 2006.Citation6 To realize the goal of better controlling hepatitis B transmission, China government even encouraged some conditional districts to take effective measures promoting adult hepatitis B vaccine. For example, free vaccination of adult hepatitis B vaccine was executed in the Chaoyang District of Beijing since 2017.Citation7
Nevertheless, the number of HBV-infected people was growing year by year.Citation8 HBV had threatened public health and induced serious social panic in China.Citation9,Citation10 It is well known that risk behaviors such as dialysis, blood transfusion, or tattooing were shown to be related to HBV infection in earlier studies.Citation11–Citation13 In addition, HBV was vertically transmitted from mother to child or horizontally transmitted by transfusion of HBV-infected blood or body fluid.Citation14 Sexual contact is one of the most common routes of horizontal HBV transmission.Citation15 Similarly, intimate behaviors of spouses such as kissing and sharing things with each other may also lead to HBV infection.Citation16 It still remains unclear that whether marriage is a risk factor of HBV infection or not for those who have been vaccinated. Although a study in Gambia reported that marriage was not a risk factor of HBV infection for vaccinated females;Citation17 there were contradictory evidence that people who had a HBV-infected spouse were at high risk for acquiring HBV.Citation18,Citation19
Majority studies on risk factors of HBV infection among married people were cross-sectional studies with small sampling, and subjects in some studies were unvaccinated population.Citation13,Citation20 In China, there were some studies reporting the prevalence and risk factors of HBV infection among couples in rural area.Citation21,Citation22 However, study on risk factors of HBV focusing on the vaccinated individuals who were married is rare. Our study explores the risk factors of HBV infection for vaccinated and unvaccinated married people aiming to examine (1) the prevalence of HBV among married individuals in 2006 and 2014; (2) the risk factors of HBV infection, especially infected spouses, in vaccinated and unvaccinated groups; and (3) changes in prevalence rate, risk factors, and relative risk (RR) value of HBV infection among vaccinated and unvaccinated individuals between 2006 and 2014.
Materials and methods
Study design
A cross-sectional study was designed to examine the risk factors of HBV in married individuals. All of these individuals were divided into vaccinated or unvaccinated groups according to “whether vaccinated or not.”
Data collection
We employed data drawn from the serological surveys conducted by the Beijing Center for Disease Prevention and Controlin 2006 and 2014.Citation23 The surveys mentioned above covered 5078 (in 2006) and 6705 individuals (in 2014), and participants over 1 y old were randomly selected from 20 communities in 10 districts (10/18). A total of 1523 (in 2006) and 1047 couples (in 2014) were included in our study for the purpose of analyzing the effect of HBV vaccine immunization in spouses ().
All of the vaccinated individuals were screened for HBsAg, anti-HBs, and anti-HBc before HBV vaccine immunization until 2012. After 2012, the technical guide for adult hepatitis B immunization in China recommended that screening before vaccination was unnecessary.Citation24,Citation25
The status of HBV infection of spouses was diagnosed with a serological test. Furthermore, 172 individuals in 2006 and 472 individuals in 2014 whose “vaccination history” were “uncertain” or “missing” in the questionnaire were excluded from the study. Finally, a total of 2874 and 1622 participants were enrolled in our study in 2006 and 2014, respectively. Information on demographic features and risk factors were collected by questionnaires.
Laboratory tests
HBsAg, anti-HBs, HBeAg, anti-HBe, and anti-HBc were tested by microparticle enzyme immunoassay (AXSYM Plus; Abbott America).
Measures
Definition of HBV-infected individuals
Based on the prognosis of HBV infection of HBV infection, we defined people as HBV-infected individuals when one or more of their HBsAg, HBeAg, anti-HBe, and anti-HBc was positive.Citation5,Citation26 Meanwhile, we considered HBsAg, anti-HBc,Citation27 and anti-HBs as outcome indicators to examine the risk factors of HBV infection.
It is a common sense that anti-HBs positivity might be induced by vaccinated immunity,Citation28 and so we did not consider it as an indicator when defining whether individuals were infected or not. However, it was also known that single anti-HBs positivity was a symbol of recovery from previous HBV infection without HBV vaccination, and so we regarded it as an outcome indicator of HBV infection in the unvaccinated group.
Definition of risk behaviors of HBV infection
Risk behaviors including history of endoscopic treatment, sharing syringes, ear or body piercing, dialysis, surgery, dental treatment, blood transfusion, and tattooing were derived from the results of the questionnaire.
Statistical analysis
Pearson chi-square test and Fisher's test were used to identify the association between serological markers of HBV and independent variables. Logistic regression analysis was employed to identify the association between age and serological markers of HBV. RR value along with 95% confidence intervals (CIs) of each risk factor was reported. P-value (two-tailed) less than 0.05 was considered as statistically significant. All the analyses were performed by SPSS22.0.
Results
Characteristics of socio-demographic variables
A total of 2874 and 1622 participants were investigated in 2006 and 2014, respectively. There were three subjects who had experienced dialysis, lack of the adequate amount of analysis. There were 54 males and 78 females in the vaccinated group, 1374 males and 1368 females in the unvaccinated group in 2006, 86 males and 95 females in the vaccinated group, and 724 males and 717 females in the unvaccinated group in 2014. The mean age of individuals was 49.30 and 46.68 y in 2006 and 2014. A total of 138 (4.80%) and 294 (18.13%) individuals were living in rural area in 2006 and 2014, respectively ( and ).
Table 1. Correlation between independent variables and viral serological markers in the vaccinated group.
Table 2. Correlation between independent variables and viral serological markers in the unvaccinated group.
Seroprevalence of HBV markers
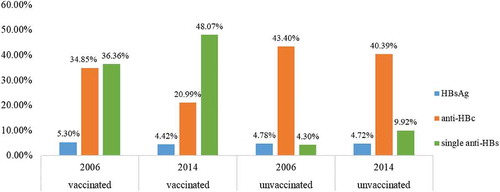
In 2006, the overall number of HBsAg, anti-HBc, and single anti-HBs positive subjects was 138 (4.80%), 1236 (43.01%), and 166 (5.78%) respectively, which was 76 (4.69%), 620 (38.22%), and 230 (14.18%) in 2014, and the positive rates of these three serological markers in vaccinated and unvaccinated group are presented in . The number of individuals who had HBV vaccine immunization history was 132 (4.59%) and 181 (11.16%) in 2006 and 2014, respectively.
Risk behaviors of HBV infection
In 2006 and 2014, 311 (10.84%) and 174 (10.76%) individuals had experienced endoscopic medicine treatment, 19 (0.66%) and 269 (16.62%) individuals had shared syringes with others, 730 (25.42%) and 420 (25.91%) individuals had body piercing experience, 999 (34.78%) and 510 (31.54%) individuals had undergone surgeries, 1646 (57.29%) and 825 (50.96%) individuals had received dentist treatment, 214 (7.45%) and 110 (6.79%) individuals had a history of tattooing, and 196 (6.82%) and 68 (4.20%) individuals had a history of blood transfusion, respectively ( and ).
Information on spouses' infected status
In 2006, there were 15 (27.78%) infected wives and 40 (51.28%) infected husbands in the vaccinated group and 544 (39.59%) and 644 (47.08%) in the unvaccinated group. The number of infected wives and husbands were 30 (34.88%) and 37 (38.95%) in the vaccinated group, which were 241 (33.29%) and 244 (34.03%) in the unvaccinated group in 2014 ( and ).
Table 3. Correlation between infected spouses and viral serological markers in the vaccinated group.
Table 4. Correlation between infected spouses and viral serological markers in the unvaccinated group.
Risk factors associated with HBV infection among the vaccinated group
The results of chi-square test and logistic regression are presented in and . For the vaccinated group, no risk factor was found to be significantly correlated with HBsAg. But we observed a significant correlation between age and anti-HBc in 2014 (40< age ≤50 versus age ≤30, RR = 3.03, 95%CI = 1.04–8.84). Gender [male versus female, RR = 0.60, 95%CI = 0.36–1.00 (2006); RR = 0.71, 95%CI = 0.52–0.97 (2014)] and age (in 2006) were significantly correlated with single anti-HBs.
Risk factors associated with HBV infection among the unvaccinated group
For unvaccinated individuals, HBsAg positivity was correlated with gender (male versus female, RR = 1.47, 95% CI = 1.04–2.06, in 2006), residence (urban versus rural, RR = 0.40, 95%CI = 0.24–0.67, in 2006; RR = 0.58, 95%CI = 0.34–0.99, in 2014), sharing syringes [RR = 3.75, 95% CI = 1.33–10.63 (in 2006); RR = 2.07, 95%CI = 1.26–3.41 (in 2014)], infected wives (RR = 1.97, 95%CI = 1.28–3.05, in 2006), and infected husbands (RR = 2.19, 95%CI = 1.25–3.82,in 2006).
Anti-HBc positivity was associated with gender [male versus female, RR = 1.19, 95%CI = 1.10–1.30 (in 2006); RR = 1.24, 95% CI = 1.09–1.40 (in 2014)], age (in 2006 and 2014), endoscopic medicine treatment [RR = 1.16, 95%CI = 1.03–1.32 (in 2006); RR = 1.21, 95%CI = 1.01–1.45 (in 2014)], sharing syringes (RR = 1.43, 95%CI = 1.25–1.64, in 2014), body piercing (RR = 0.84, 95%CI = 0.75–0.93, in 2006), infected wives (RR = 1.32, 95%CI = 1.18–1.47, in 2006), and infected husbands (RR = 1.39, 95%CI = 1.22–1.59, in 2006). Anti-HBs positivity was associated with age (in 2006 and 2014) ( and ).
Discussion
In our study, the proportion of individuals who had accepted HBV vaccine immunization increased from 4.59% to 11.16% from 2006 to 2014. In 2006, the overall positive rates of HBsAg, anti-HBc, and single anti-HBs were 4.80%, 43.01%, and 5.78%, respectively, which were 4.69%, 38.22%, and 14.18% in 2014. The positive rate of HBsAg decreased in the vaccinated and unvaccinated groups as well as anti-HBc, which was attributed to newborn immunization policy launched in Beijing since the year 1992Citation29–Citation31 and immunization policy for adolescents and adults since 2006.Citation6
The prevalence of single anti-HBs positivity increased in the vaccinated group from 2006 to 2014, which might be caused by the lower cost of HBV vaccine, improvement of income, and promotion of complete vaccination rate during that period.Citation32,Citation33
However, we found that the positive rate of anti-HBs, in the unvaccinated group, was higher in 2014 than that in 2006, which was contradictory to the change of anti-HBc. In addition to the impact of sampling error, the possible explanation was that the number of individuals who were undergone naturally immunized after HBV infection was higher in 2014. A study reported that the naturally immunization of HBV infection might last for many years .Citation34 The reason should be figured by further study. Meanwhile, we found that there was little difference in the HBsAg-positive rate between the vaccinated and unvaccinated groups in our study. This result was contradictory to the fact that HBsAg-positive rate declined after vaccination. This might be due to different age structure and low response rate of HBV vaccine. In this study, the low response rate could be further explained by family history, drinking history, and the validity period of vaccine protection.Citation35,Citation36 For vaccinated individuals, there was no risk factor significantly correlating with HBsAg positivity. Anti-HBc positivity was found to be correlated with age by a study in 2014 (40< age ≤50), and it was possible that anti-HBc positivity could occur with the decline of anti-HBs.Citation28,Citation34 But this result did not occur in other older age groups, which could not be explained by our existing data, and needed to be further studied.
Both in 2006 and in 2014, we observed that gender and age were significantly correlated with single anti-HBs positivity. Single anti-HBs positive rate was higher in females than in males, which was possible that females were more likely to develop anti-HBs than males after HBV vaccine immunization.Citation37 Positive rate of single anti-HBs decreased with age, which was consistent with the previous study.Citation34
Vaccinated individuals faced with nearly zero-level common risk factors of HBV infection than those unvaccinated, which might indirectly prove the conclusion that vaccination might effectively protect people from HBV infection.
For unvaccinated subjects, males were at high risk of HBsAg positivity,Citation38,Citation39 which might link to complicated lifestyle and increased risk of chronic HBV infection in males.Citation40,Citation41 Anti-HBc-positive rate was higher in older individuals owing to the decline of anti-HBs level with time or exposure to more risk factors with long duration of marriage.Citation34,Citation42 Single anti-HBs decreased with age, which was similar to the result in the vaccinated group.
Individuals living in the rural area accounted for a high proportion of HBsAg positivity, which could always be caused by imbalanced income, non-hospital delivery, less health awareness of HBV knowledge, lack of health service resource, and lower education levels of caregivers.Citation43,Citation44
Using unsafe medical devices might lead to HBV infection. Endoscopic medicine treatment was a risk behavior of HBV infection both in 2006 and in 2014, demonstrating that medical infection from endoscopy device should not be neglected.Citation45 Sharing syringes could also lead to HBV infection, which might link to unsafe vaccine injections, blood donation, and drug injection.Citation10,Citation46,Citation47
Body piercing was statistically significantly associated with anti-HBc in 2006, supporting the earlier finding that body piercing was a risk factor of HBV infection, but it could be avoided by safe piercing practice.Citation48
Sexual intercourse, kissing, and other close contacts such as sharing toothbrush were main routes of HBV transmission among spouses. Numerous previous studies had found that infected spouse was one of the causes of HBV infection.Citation13,Citation19,Citation22,Citation42 HBV vaccine immunization was an effective approach to prevent HBV transmission among infected spouses in some studies.Citation17,Citation49 In our study, infected spouse was significantly associated with HBsAg and anti-HBc only in the unvaccinated group in 2006, which meant that individuals who were hepatitis B patients or carriers would be a threat to their unvaccinated spouses. Additionally, infected spouse was not significantly correlated with HBV infection in 2014. The reason for this difference might be due to the promotion of national health literacy.
In this study, we found that there was no statistically significant correlation between positive HBV serological markers and risk factors such as history of surgery, dental treatment, blood transfusion, and tattooing. Our result was partly inconsistent with existing research.Citation47,Citation50,Citation51
In conclusion, this study illustrates the risk factors of HBV infection among married individuals in the vaccinated and unvaccinated groups. The transmission of HBV has been well controlled by the HBV vaccine immunity policy implemented in Beijing. Unvaccinated individuals face much more HBV infection risk than those vaccinated, and we tentatively conclude that HBV vaccine could effectively protect people from the risk of HBV infection among married people.
Limitation
To our best knowledge, our study is the largest population-based investigation in Beijing, the data was collected by investigation, and there may be recall bias in this study. Information about screening before vaccination was not investigated. Additionally, HBV-infected status of individuals before marriage was not investigated, which would lead to overestimation of the RRof infected spouses.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Recommend peer reviewer
Dawei Zhu1 Chuanxi Fu2
1 Center for Health Policy and Management, Institute of Medical Information & Library, Chinese
Academy of Medical Sciences & Peking Union Medical College, No. 3 Yabao Road, Chaoyang
District, 100020, Beijing, China;[email protected]
2 Guangzhou Center for Disease Control and Prevention, Guangzhou,China, [email protected]
Additional information
Funding
References
- Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, … Forouzanfour MH. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016; 388(10049): 1081–88. doi:10.1016/S0140-6736(16)30579-7
- Yuen MF, Lai CL. Natural history of chronic hepatitis B virus infection. J Gastroenterol Hepatol. 2000; 15: E20–E24.
- World Health Organization. Hepatitis B[EB/OL]. [accessed 2018 July 18]. https://www.who.int/news-room/fact-sheets/detail/hepatitis-b
- World Health Organization. Hepatitis B[EB/OL]. [accessed 2015 May 15]. http://www.wpro.who.int/china/topics/hepatitis/qa_20150515/en/
- Liao XY, Zhou ZZ, Wei FB, Qin HN, Ling Y, Li RC, … Zhuang H. Seroprevalence of hepatitis B and immune response to hepatitis B vaccination in Chinese college students mainly from the rural areas of western China and born before HBV vaccination integrated into expanded program of immunization. Hum Vaccin Immunother. 2014; 10(1): 224–31.
- DU N, MA JX, LIU YY, LI Q, LUO FJ. Epidemiological analysis of acute hepatitis B in Chaoyang district in Beijing from year 2008 to 2012. Chronic Pathematol J. 2014; (3): 1.
- Beijing Chaoyang District Community Health Service Management Center. Chaoyang District: Health Welfare Invasion - Free Hepatitis B Vaccination[EB/OL].[accessed 2017 Feb 10]. http://www.bjchs.org.cn/Html/News/Articles/5549.html
- Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015; 386(10003): 1546–55.
- Kan Q, Wen J, Xue R. Discrimination against people with hepatitis B in China. Lancet. 2015; 386(9990): 245–46.
- Liu J, Liang W, Jing W, Liu M. Countdown to 2030: eliminating hepatitis B disease, China. World Health Org. Bull World Health Org. 2019; 97(3): 230–38. doi:10.2471/BLT.18.219469
- Ozer A, Yakupogullari Y, Beytur A, Beytur L, Koroglu M. Risk factors of hepatitis B virus infection in Turkey: a population-based, case-control study: risk Factors for HBV Infection. Hepat Mon. 2011; 11(4): 263.
- Hayatbakhsh MM, Moghaddam SD, Zahedi MJ, GP MS, Zade MK, GP MA. Seroprevalence of hepatitis B before marriage: a study on marriage candidates in the southeast of Iran; is it worthy of consideration? Arch Iran Med. 2015; 18(1): 34. 015184/AIM.006
- Luksamijarulkul P, Piroonamornpun P, Triamchaisri SK. Hepatitis B seromarkers, hepatitis C antibody, and risk behaviors in married couples, a bordered province of western Thailand: hepatitis B seromarkers, hepatitis C antibody, and risk behaviors. Hepat Mon. 2011; 11(4): 273.
- Liaw YF, Chu CM. Hepatitis B virus infection. Lancet. 2009; 373(9663): 582–92. doi:10.1016/S0140-6736(09)60207-5
- Sun AW, Bi SL, Wang F, Wang FZ, Zhang S, Tu QF, … Miao N. Study on the risk of HBV infection among spouses of HBsAg carriers. Zhonghua Liu Xing Bing Xue Za Zhi= Zhonghua Liuxingbingxue Zazhi. 2013; 34(3):214–17.
- Lin J, He J. Clinical guideline inconsistency regarding the prevention of hepatitis B and C virus transmission. Infect Control Hosp Epidemiol. 2016; 37(6):744–45. doi:10.1017/ice.2016.50
- Mendy M, Peterson I, Hossin S, Peto T, Jobarteh ML, Jeng-Barry A, … Whittle H. Observational study of vaccine efficacy 24 years after the start of hepatitis B vaccination in two Gambian villages: no need for a booster dose. PLoS One. 2013; 8(3):e58029. doi:10.1371/journal.pone.0058029
- Katoonizadeh A, Motamed-Gorji N, Sharafkhah M, Ostovaneh M, Esmaili S, Eslami L, … Khuzani AS. Intra-familial transmission of chronic hepatitis B infection: a large population-based cohort study in Northern Iran. Arch Iran Med. 2018; 21(10):436–42.
- Zamir D, Zamir C, Rishpon S. Epidemiology of hepatitis B virus infection among family members of chronic carriers in Israel. Israel Med Assoc J: IMAJ. 2001; 3(5):338–40.
- Zervou EK, Gatselis NK, Ziciadis K, Georgiadou SP, Dalekos GN. Intrafamilial spread of hepatitis B virus infection in Greece. Eur J Gastroenterol Hepatol. 2005; 17(9):911–15. doi:10.1097/00042737-200509000-00005
- Liu J, Zhang S, Wang Q, Shen H, Zhang M, Zhang Y, … Liu M. Prevalence of HB sAg/HB eAg amongst 1 936 801 couples preparing for pregnancy in rural China: an observational study. J Viral Hepat. 2017; 24(8):679–86. doi:10.1111/jvh.12693
- Zhang L, Wang YY, Huang YJ, Wang QM, Nelson KE, Wang AQ, … Peng ZQ. Status of HBsAg seroprevalence in 15 million rural couples in China: a cross-sectional study. Sci Rep. 2017; 7:42822. doi:10.1038/srep42822
- Wang H, Gao P, Chen W, Bai S, Lv M, Ji W, … Wu J. Changing epidemiological characteristics of Hepatitis A and warning of anti-HAV immunity in Beijing, China: a comparison of prevalence from 1990 to 2017. Hum Vaccin Immunother. 2019; 15(2):420–25. doi:10.1080/21645515.2018.1529128
- Cui FQ. Technical guide for adult hepatitis B immunization in China. Chi J Epidemiol. 2011; 32(12):1199–203.
- Liao X, Zhuang H. Hepatitis B vaccination without screening is safe. Chi Prev Med. 2010; 11(10):973–74.
- Ko YC, Yen YY, Yeh SM, Lan SJ. Female to male transmission of hepatitis B virus between Chinese spouses. J Med Virol. 1989; 27(2):142–44.
- Alawi FB, Robertson PW, LePage AK, Jayamaha J, Baleriola C, Rawlinson WD. The reliability of HBV core antibody in serological screening for hepatitis B virus. Pathology. 2013; 45(5):501–05. doi:10.1097/PAT.0b013e3283631cf9
- Poorolajal J, Mahmoodi M, Haghdoost A, Majdzadeh R, Nasseri‐Moghaddam S, Ghalichi L, Fotouhi A. Booster dose vaccination for preventing hepatitis B. Cochrane Database Syst Rev. 2010; 11(11):CD008256.
- Liang X, Bi S, Yang W, Wang L, Cui G, Cui F, … Wang F. Epidemiological serosurvey of hepatitis B in China – declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009; 27(47):6550–57. doi:10.1016/j.vaccine.2009.08.048
- Yonghao G, Jin X, Jun L, Pumei D, Ying Y, Xiuhong F, … Wanshen G. An epidemiological serosurvey of hepatitis B virus shows evidence of declining prevalence due to hepatitis B vaccination in central China. Int J Infec Dis. 2015; 40:75–80. doi:10.1016/j.ijid.2015.10.002
- Lu FM, Li T, Liu S, Zhuang H. Epidemiology and prevention of hepatitis B virus infection in China. J Viral Hepat. 2010; 17:4–9. doi:10.1111/j.1365-2893.2010.01266.x
- Wang D, Wang X, Shi SW, LV M, Wu J, Bai Q, … Shi XF. Calculation and analysis of hepatitis B vaccine immunization cost among disease control and prevention institution in Beijing [J/OL]. Chi Prev Med: 1–4 [accessed 2019 May 24] http://kns.cnki.net/kcms/detail/11.4529.R.20181122.0929.002.html
- Wang H, Zhang W, Wu J, Han LL, Lin CY, Gao P, … Li H. Hepatitis B vaccination rate in adults of Beijing: a cross-sectional study. Chi J Public Health. 2010; 26:612–14.
- Chan HLY. Changing scene in hepatitis B serology interpretation. Hospital Med. 2002; 63(1):16–19.
- Chun-Yan L, Yi L, Li-Li X. Misunderstanding of hepatitis B vaccination. Chi J Frontier Health Quarantine. 2014; 37(06):407, 408, 427. doi:10.16408/j.1004-9770.2014.06.008
- Dong-She Z, Lei D, Hai-Bin X. A research on risk factors of hepatitis B vaccination failure. Chi Prev Med. 2009; 10(12):1085–87. doi:10.16506/j.1009-6639.2009.12.026
- Wood RC, MacDonald KL, White KE, Hedberg CW, Hanson M, Osterholm MT. Risk factors for lack of detectable antibody following hepatitis B vaccination of Minnesota health care workers. Jama. 1993; 270(24):2935–39.
- Yang S, Wu J, Ding C, Cui Y, Zhou Y, Li Y, … Ruan B. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017; 17(7):716–25. doi:10.1016/S1473-3099(17)30227-X
- Blumberg BS. Sex differences in response to hepatitis B virus. Arthritis Rheumatism: Off J Am Colleg Rheumatol. 1979; 22(11):1261–66.
- Tozun N, Ozdogan O, Cakaloglu Y, Idilman R, Karasu Z, Akarca U, … Ergonul O. Seroprevalence of hepatitis B and C virus infections and risk factors in Turkey: a fieldwork TURHEP study. Clin Microbiol Infect. 2015; 21(11):1020–26. doi:10.1016/j.cmi.2015.06.028
- McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009; 49(S5):S45–S55. doi:10.1002/hep.22898
- Okamoto D, Nakayama H, Ikeda T, Ikeya S, Nagashima S, Takahashi M, … Okamoto H. Molecular analysis of the interspousal transmission of hepatitis B virus in two Japanese patients who acquired fulminant hepatitis B after 50 and 49 years of marriage. J Med Virol. 2014; 86(11):1851–60.
- Liu X, Yang C, Zhong Q, Song Q, Huang X, Yang Y, … Zhou H. Improved timely birth dose coverage of hepatitis B vaccine narrows the socio-economic inequality in western China in 2011–2016. Vaccine. 2018; 36(27):3901–07.
- Zhu D, Guo N, Wang J, Nicholas S, Wang Z, Zhang G, … Wangen KR. Socioeconomic inequality in hepatitis B vaccination of rural adults in China. Hum Vaccin Immunother. 2018; 14(2):464–70.
- Gulsen MT, Beyazit Y, Guclu M, Koklu S. Testing for hepatitis B and C virus infection before upper gastrointestinal endoscopy: justification for dedicated endoscope and room for hepatitis patients. Hepato-gastroenterology. 2010; 57(101):797–800.
- Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011; 378(9791):571–83.
- Huang Y, Guo N, Yu Q, Lv Y, Ma H, Yun Z, … Cao R. Risk factors for hepatitis B and C infection among blood donors in five Chinese blood centers. Transfusion. 2015; 55(2):388–94.
- Yang S, Wang D, Zhang Y, Yu C, Ren J, Xu K, … Li Y. Transmission of hepatitis B and C virus infection through body piercing: a systematic review and meta-analysis. Medicine. 2015; 94(47):e1893. doi:10.1097/MD.0000000000001893
- Hu Z. Observation on prevention of hepatitis B virus transmission between newly-married couples by HBsAg vaccine. Zhonghua Liu Xing Bing Xue Za Zhi= Zhonghua Liuxingbingxue Zazhi. 1991; 12(4):222–25.
- Yazdi MA, Baradaran H. HBV contamination of medicine instruments in surgery department. J Clin Virol. 2006; 36:S39.
- Haider J, Lufullah G, Nazli R, Akhtar T, Shah A. Screening of adult dental patients visiting Khyber College of Dentistry, Peshawar for HBV and HCV infections and identifying the associated risk factors. Pak J Med Sci. 2017; 33(3):615.