ABSTRACT
Tetanus toxoid vaccination is freely available for most women in developing countries, yet maternal and neonatal tetanus are still prevalent in 13 countries, 9 of which are in sub-Saharan Africa. We evaluated whether providing cash incentives increases the uptake of tetanus toxoid vaccination among women of childbearing age in rural northern Nigeria. We randomized amounts of cash incentives to women in three groups: 5 Nigerian naira (C5), 300 naira (C300), and 800 naira (C800) (150 naira = 1 U.S. dollar). Overall, of 2,482 women from 80 villages, 1,803 (72.6%) women successfully received the vaccination (419 of 765 [54.8%] women in C5, 643 of 850 [75.7%] women in C300, and 741 of 867 [85.5%] women in C800). Women in C300 and C800 were significantly more likely to receive the vaccine than women in C5. We further found that transportation costs are one of the significant barriers that prevent women from receiving vaccination at clinics, and that cash incentives compensate for transportation costs unless such costs are large.
1. Introduction
Organizations such as the World Health Organization (WHO), the United Nations Children’s Fund (UNICEF), and the United Nations Population Fund (UNFPA) have been committed to eliminating maternal and neonatal tetanus (MNT).Citation1 With the international efforts, 46 out of 59 countries that had not eliminated MNT in 1999 achieved this goal by 2018, but 13 countries, 9 of which are in Africa, still have not eliminated MNT. In 2015 alone, 34,000 newborns around the globe died of tetanus, and there were a significant number of maternal deaths due to tetanus as well.Citation2
Nigeria is one of 13 countries where tetanus is still a major public health problemCitation1 and tetanus contributes to a high neonatal mortality rate.Citation3 Fatality from neonatal tetanus reaches almost 100% without medical treatment, which is difficult to obtain in rural Africa.Citation4 Providing tetanus toxoid vaccines to mothers is the most effective way to protect mothers and their children. If the correct vaccination schedule is followed, the vaccine prevents neonatal tetanus with efficacy of at least 80% and with five years of protection. Despite this seemingly obvious benefit, however, vaccine uptake is low in Nigeria. Among countries that have eliminated MNT, the proportion of newborns protected against tetanus has reached 86%, while only 40% of newborns are protected in Nigeria.Citation5 Despite international and national efforts to eliminate MNT in Nigeria, only 55% of newborns receive at least two doses of the tetanus vaccine, and there has not been significant progress since 2000.Citation5
There is extensive literature that evaluates demand-side interventions as a way to increase the vaccination rate in low- and middle-income countries.Citation6–Citation8 One potentially effective way to increase the vaccination rate is to offer cash incentives. Findings on the effectiveness of cash incentives on the rate of immunization, however, are mixed. Oyo-Ita et al.Citation6 and Bassani et al.Citation9 conducted a meta-analysis on the effect of cash incentives and concluded that monetary incentives have little or no effect on children’s immunization coverage. Johri et al.,Citation7 Ranganathan and Lagarde,Citation10 and Lagarde et al.,Citation11 on the other hand, found that cash incentives, especially conditional cash transfers (CCTs), promoted uptake of preventive services by children and pregnant women. Many of these CCT programs, however, have multiple conditionality instead of single conditionality. A cash transfer with multiple conditionality means that one can receive the cash transfer only after one meets multiple requirements, while a cash transfer with single conditionality means that one can receive the cash transfer after one meets a lone requirement. A common example of multiple conditionality among CCT programs is the combination of regular health checkups, child vaccination, and school attendance.Citation12–Citation14 Under such CCT programs, it is difficult to examine which condition affects the increase in vaccinations. Thus, although many studies show the small and limited effects of CCT on vaccination in developing countries in this context,Citation13–Citation16 multiple conditionality might have made it difficult to capture the actual effect of cash incentives on vaccine uptake.
Banerjee et al.Citation17 used the completed child vaccination as the only condition under which one could receive a small in-kind transfer (single conditionality) and found the incentive had a large effect. Gibson et al.Citation18 offered another example with single conditionality that provided cash incentives combined with SMS reminders to achieve full immunization among children in Kenya. They found that while SMS reminders did not increase the vaccination completion rate among children, 200 Kenyan shillings (85 shillings = 1 U.S. dollar) combined with SMS reminders increased the completion rate by 8 percentage points from the control rate of 82%. Their treatment effect was small, given the high completion rate among the control group.
Most extant studies have focused exclusively on the effectiveness of cash incentives on full immunization among children. This paper, on the other hand, evaluates the effect of cash incentives on one-time tetanus toxoid vaccine uptake among women of childbearing age. This paper contributes to the literature by focusing on women’s decisions regarding their own vaccination against tetanus rather than their children’s immunization. We examined the effect of one-time cash incentives on one-time vaccine uptake instead of the effect of repeated incentives on repeated vaccine uptakes to simplify the design, which enabled us to clearly see the one-to-one relationship between cash incentives and a vaccine decision. Finally, we selected study sites where the vaccination uptake was low, expecting cash incentives to have a larger effect.
2. Methods
2.1. Study design
The study was a three-arm individual-level randomized controlled trial, facilitated by Adamawa State Primary Health Care Development Agency (ADSPHCDA) in Jada. ADPHCDA operates under the National Primary Health Care Development Agency (NPHCDA), the governmental organization that is in charge of any immunization-related activities in the country.
2.2. Study area, sampling, and randomization
This study was conducted in the Jada local government area of Adamawa State, in the northeastern region of Nigeria. Three-stage sampling was employed. First, 10 main health clinics out of 11 in the area were selected. We excluded one main health clinic that was close to another clinic with a better facility because the catchment area of these two clinics overlapped and the better-equipped facility could accommodate more visitors. Second, 80 villages with more than 10 households that were within the catchment areas of the 10 health clinics were selected. We followed ADSPHCDA guidelines to define catchment areas.
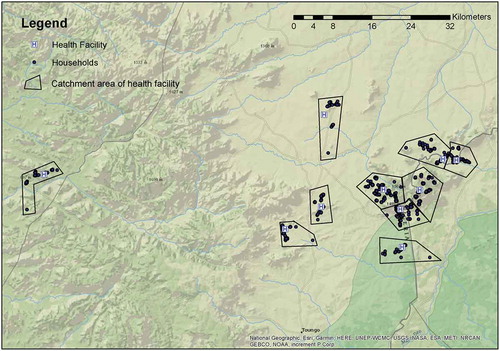
Third, one woman from each household was selected in each of the 80 villages.Footnotea Our interviewers visited all the households in each of these 80 villages to find eligible women. The eligibility criteria were age (15–35 years) and tetanus vaccine status (not received within 6 months). Our interviewers asked each woman about her vaccination status and also inspected, when available, the antenatal care card with the vaccine record to determine the status of tetanus vaccine uptake. We selected a maximum of one woman from each household. If there were multiple eligible women in one household, we selected the woman whose first name was first alphabetically. However, if one of them was a pregnant woman, we selected her over the other eligible women. If there were no pregnant women but there was a non-pregnant woman who had never received the tetanus vaccine, we selected her over the other eligible women. Our sample included 2,530 women in 80 villages. presents the 10 health clinics and the locations of women from the 80 villages around the clinics.
This study targeted not only pregnant women, but also women of childbearing age. Although much of the focus has been on tetanus vaccine uptake among pregnant women, protecting all women of reproductive age is important. As recommended by the WHO,Citation2 multiple doses of tetanus toxoid vaccination over time should be given to all women of childbearing age, although the first dose is usually provided to pregnant women. Targeting non-pregnant women of childbearing age is important to protecting newborn babies in the long run, because it takes at least 6 months to get the recommended number of doses (three). Starting the tetanus vaccination series after getting pregnant might not give women sufficient time to receive all three doses for full protection.
At the time of the baseline study, our interviewers randomized eligible participants who consented to participate in the study to receive one of three different amounts of cash incentive with equal probability: 5 Nigerian naira (C5), 300 naira (C300), and 800 naira (C800) (150 naira = 1 U.S. dollar). Randomization was done using a paper questionnaire that indicated the amount of the cash incentive (C5, C300, or C800) pre-printed in the middle of the page. The pre-printing was based on a randomization scheme generated by a computer algorithm.
In this trial, we considered women in C5 as the control group, where 5 naira is equivalent to about 3 U.S. cents. We provided this lowest cash incentive to the control group for tracking purposes. We asked respondents to bring the voucher, which we provided with the baseline survey, to the clinic when they came for the vaccination. The voucher indicated the respondents’ names as well as the amount of cash incentive they could redeem. There was the risk that respondents in the control group would not have brought the voucher if there were no cash incentives, which would have made it difficult to track vaccination status. We selected 300 and 800 naira as the amounts for cash incentives based on the pilot study, which we conducted right before the initiation of this main study, to ensure that we would have variation in the vaccine uptake in response to cash incentives.
2.3. Procedures
The baseline questionnaire was administered to all women who agreed to participate in the study to capture their prior knowledge, beliefs, and attitudes about tetanus and tetanus vaccination, as well as their own and their household’s baseline characteristics, such as demographics, health, and economic status. We also asked about their transportation to the clinic, including the mode of transport and transportation costs.
Information about tetanus and tetanus toxoid vaccination was provided to the respondents immediately after they completed the baseline interview. They were then provided a voucher that they could redeem at the assigned health clinic. Respondents could receive the cash at the assigned clinic if they visited it for vaccination within one week of the baseline survey. Each respondent was assigned to a health clinic in the village where she resided. The voucher indicated the respondent’s name, her unique project ID, the date of the intervention, the name of the health clinic she was assigned to, and the amount of cash compensation she was to be provided (5, 300, or 800 naira).
At each health clinic, the endline questionnaire was administered only to the women who visited the clinic for the vaccination within one week of the baseline survey. Our enumerators verified the actual vaccination received by respondents and asked questions that were mainly about the transportation used to visit the clinic.
2.4. Outcomes
The primary outcome was the one-time tetanus toxoid vaccination at an assigned clinic within one week of the baseline survey. Provision of tetanus toxoid vaccines is part of the Nigerian Expanded Programme on Immunization.Citation19 The schedule of tetanus toxoid vaccination follows the recommendation from WHO that women of childbearing age and pregnant women receive three doses of the tetanus toxoid vaccine: the first at first contact or as soon as possible in pregnancy, followed by a second dose at least four weeks after the first and a third dose six months later.Citation2 A single dose can prevent only 43% of neonatal tetanus deaths.Citation20 It is also important to follow the vaccination schedule. Although receiving multiple doses of tetanus toxoid vaccine is crucial for its efficacy, our experiment focused on a single-dose uptake to measure the effect of one-time cash incentives without introducing complexities in repeated uptake decisions.
Our enumerators, who were stationed at each clinic during the study period, observed the actual vaccine uptake among respondents who visited the clinic. Enumerators administered an endline survey to the respondents when they attended their clinic visits. They recorded the vaccine uptake of each respondent after they observed it and also collected the submitted voucher. Although it was possible that vouchers were swapped or used by other people, we think that this was unlikely, both because of the population’s low literacy rate and because we asked for and confirmed each respondent’s name at her clinic visit, then matched it with the name written in the voucher.
We also evaluated the effect of cash incentives on the choice of transportation, including the mode of transport to the clinic and the cost of transport to the clinic, among respondents who visited the clinic for vaccination. We collected the information on transportation at both the baseline and endline visits.
2.5. Statistical analysis
Sample size calculations determined that about 740 individuals in each arm could detect a 12% absolute difference in the proportion of vaccinated respondents between the control group and any given intervention group, with the following assumption: The vaccine uptake in the control group (C5) was 60%, with type I error of 0.05 and power of 0.8. This assumption regarding baseline vaccination coverage was made based on the Nigeria Demographic and Health Survey conducted in 2013.Citation21
The odds ratio for the vaccine uptake was calculated for the intervention groups, C300 and C800, respectively, and compared with the control group, C5, using logistic regression, as the dependent variable (the vaccine uptake) was binary. All the regressions used village fixed effects (v) to control for village heterogeneity by including the dummy variable for each village in regressions. As all respondents in the same village were assigned to the same health clinic, village fixed effects also controlled for clinic heterogeneity such as supply-side factors. As a robustness check, we also considered a specification with covariates. Covariates controlled for baseline characteristics and behavior, such as respondent’s age, age squared, religion (Muslim or not), any education attained, marital status (single or married), pregnancy status, whether she had a child, whether she engaged in paid work, distance to the health clinic, past use of the assigned health clinic, and past tetanus vaccine experience. All the results were similar to those without the covariates. We also found consistent and robust results using OLS regression.
Access to health facilities is often a strong determinant of health care use, including vaccination. This study also evaluated the differential effect of cash incentives on vaccine uptake by considering transportation costs to the health facility. We conducted the sub-group analysis according to the size of those costs, and evaluated how the effect of cash incentives (as compared to C5) was different for each sub-group. Finally, we also evaluated how the cash incentives (as compared to C5) determined the type and use of transportation used to visit the clinic.
3. Results
3.1. Descriptive statistics
Of the 2,530 women included in the sample, 2,482 women who were not missing information on important variables were used for the analysis. We enrolled respondents and conducted the experimental study from March 2013 to May 2013.
presents the demographic characteristics of respondents overall (column 1), as well as by study arm (columns 2–4). On average, respondents were 25 years old. About half of the sample were Muslim, almost half (48.3%) had never received any education, 15.3% had never gotten married, 18.0% were pregnant, and 76.5% had at least one child. Many respondents (43.5%) engaged in paid work, including selling agricultural produce, and the average amount of household earnings per capita in the past month was about 6,000 naira (approximately 40 U.S. dollars). On average, the distance to the assigned health clinic, as measured by GPS coordinates, was 1.7 kilometers, while the transportation costs to the clinic (both ways) were around 124 naira (83 U.S. cents).Footnoteb
Table 1. Demographics of participants by study arm
The majority of respondents (72.2%) had visited the assigned health clinic before, and 39.8% had received the tetanus toxoid vaccination at least once. These characteristics and health behaviors of women in the sample are comparable to those of the nationally representative sample.Citation21,Footnotec
The balance of baseline characteristics and health behaviors was checked; the results are noted in (column 5). The results indicate that the randomization performed well: We found that most respondent characteristics of women were similar across the study arms. The exceptions were age and transportation costs to the clinic, but the magnitude of the difference was not large for either variable.
3.2. Effect of cash incentives on vaccine uptake
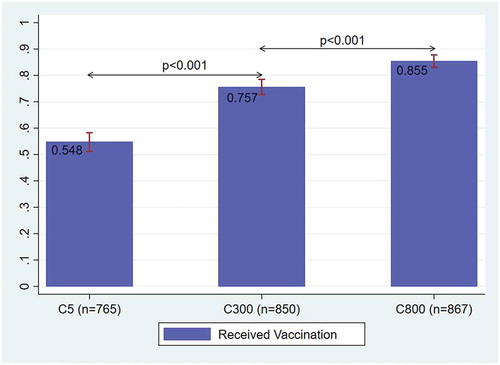
Out of 2,482 women, 1,803 (72.6%) women successfully received the vaccination: 419 of 765 (54.8%) women in C5, 643 of 850 (75.7%) women in C300, and 741 of 867 (85.5%) women in C800 ().
Women in C300 and C800 were significantly more likely to receive the vaccine than women in C5 ( and column 1). The odds of the vaccine uptake under C300 were 3.36 times [95% CI: 2.60–4.35, p < .001] more likely than under C5, and the odds ratio for C800 compared with C5 was 7.58 [95% CI: 4.51–10.97, p < .001]. C800 achieved a significantly higher vaccine uptake than C300 as well (, column 3).
Table 2. Logistic regression analysis of CCT by transportation costs
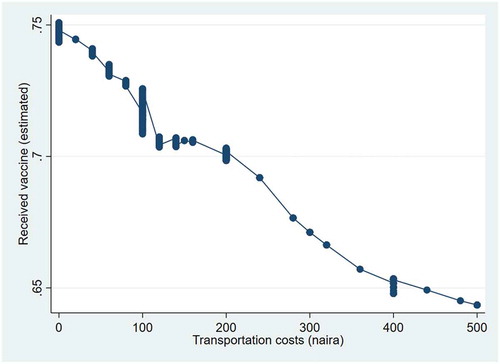
presents the association between transportation costs measured at baseline and the vaccine uptake using a locally weighted regression. Higher transportation costs were strongly associated with a lower likelihood of vaccine uptake. (columns 2 to 4) presents the effect of cash incentives (comparison group = C5) for each range of transportation costs measured at baseline. (column 3) shows that, if the transportation costs were non-zero but below 300 naira, the odds of the vaccine uptake were 5.77 times higher under C300 than under C5 [95% CI: 3.43–9.70, p < .001] and the odds ratio for C800 compared with C5 was 14.59 [95% CI: 8.12–26.17, p < .001]. These ratios were significantly larger than the odds ratio for each cash incentive when there were no transportation costs (column 2), and when the transportation costs were more than 300 naira (column 4).
Figure 3. Relationship between transportation costs and vaccination
presents the effect of cash incentives on the mode of transport and transportation costs at the endline visit among respondents who received the vaccine at an assigned clinic after controlling for the baseline transportation. Panel A presents the logistic regression for the effect of cash incentives on the mode of transport to the clinic. The odds of walking to the clinic under C300 and C800 were lower than under C5; the odds ratios were 0.817 and 0.748, respectively, though insignificant. On the other hand, the odds ratio of using other transportation that was faster but more expensive, such as a motorcycle or car, was 1.34 (insignificant) for C300 and 1.46 [95% CI: 1.01–2.11, p = .045] for C800, as compared to C5. Panel B presents the OLS regression for the transportation time and costs. The transportation costs increased significantly if the respondents were offered some cash incentives – by 9.5 naira for C300 and 14.4 naira for C800 (column 4) – although the time required for the transportation did not change (column 3).
Table 3. Effects of CCT on transportation to clinic (Endline)
4. Discussion
We found that cash incentives significantly increased one-time tetanus vaccine uptake among women of childbearing age. A two-dollar cash incentive (C300) increased the odds of vaccine uptake more than three times (3.4) as compared to the control (C5). The vaccine uptake under the lowest cash incentive, which was considered the control, was 55%. The significant cash incentive effects found in this study are moderate compared to the effect of an in-kind transfer found by Banerjee et al. (2010); in their study, the relative risk of complete immunization for the conditional in-kind transfer (equivalent to about 435 naira) versus the control was 6.7 in rural India (odds ratio of about 10). There exist, however, substantial differences between our study and that conducted by Banerjee et al.Citation17 in terms of the study participants (women of childbearing age vs. children), the location of vaccination (health clinic vs. camp within village), the type of vaccination offered (one dose of tetanus vs. any immunization), and the provision of detailed vaccine information (yes vs. no). Distinct from our experiment, this very large treatment effect found in Banerjee et al. (2010) can also be attributed to the extremely low vaccination rate at the baseline (6%).Citation17
On the other hand, the effect of cash incentives found in this study was much larger than the one noted in the study by Gibson et al.,Citation18 where 2.40 U.S. dollars cash incentives plus SMS reminders only increased immunization rates by 9% in rural Kenya. This small effect could be due to the high baseline vaccination rate of 82%.
Our study also revealed that transportation cost is one of the major barriers that hinders vaccination uptake. In particular, the lack of a convenient mode of transport prevents women from visiting the clinic easily. The effect of a cash incentive is stronger if respondents face transportation costs that are less than the cash incentive offered. Cash incentives compensate for transportation costs unless such costs are large.
We found that women choose a more expensive mode of transport when they are offered a higher cash incentive. Although this analysis does not identify any causality because the sample is self-selected clinic-attendees, these results provide suggestive evidence that even if women visit the clinic, they are constrained to doing so using an undesirable mode of transport due to the high costs of a preferable alternative mode.
4.1. Limitations
Our study had several limitations. The study was conducted in one local government area in one of the northeastern states of Nigeria; thus, the result has limited generalizability to other regions (external validity). Although it is important to receive multiple doses of tetanus toxoid vaccines, our study focused only on the uptake of one dose. While measuring the effect of cash incentives on one-time uptake can identify a one-to-one relationship between one-time cash incentives and one-time vaccination behavior, its policy implications are less extensive. Future work should explore the sustainable effect of one-time cash incentives on the uptake of multiple doses.
Because all the respondents received information about tetanus, we cannot separate the effect of cash incentives and that of information on the vaccine uptake. However, this setting is practical because, in order for respondents to make informed decisions, it is natural and ethical to explain and give information about the vaccine that we provided cash incentives for. For the analysis, we can measure the marginal effect of cash incentives under the assumption that information affects the vaccine uptake in the same way, regardless of the amounts of the cash incentives offered. Future work should explore the potential interaction effect of information and cash incentives.
Finally, because the randomization was at the individual level, there could be contamination effects from cash incentives.
5. Conclusions
Cash incentives significantly increased the uptake of tetanus toxoid vaccine among women in Adamawa state, Nigeria. We also found that cash incentives relaxed budget constraints among women who needed to pay for the transportation costs to visit the health clinic for vaccination. Although the C800 group achieved an 85% vaccination rate, it was an expensive intervention. Further study is necessary to evaluate the sustainable design of cash incentives. At the same time, evaluating whether more cost-effective intervention is possible to ease the burden of transportation to the clinic and increase the vaccine uptake is critical to achieving high vaccination coverage in developing countries. For example, providing public transportation to the clinic can potentially increase the vaccine uptake by removing the barriers related to transportation.
Authors’ Contributions
RS conceived of the research design, collected data, analyzed the data, and wrote the manuscript. BF supervised the data collection. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Disclosure of potential conflicts of interest
The author declares that she has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
Ethics approval was obtained on November 2012 from University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (HUM00063832). Oral and written informed consents were obtained from all the respondents prior to their participation in the study.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Acknowledgments
I am grateful to Abdullahi Belel and the Adamawa State Primary Health Care Development Agency for their cooperation and support throughout the project implementation. We give special thanks to the field team who devoted themselves to the project. We appreciate Raj Arunachalam, Abhijit Banerjee, Hoyt Bleakley, Anne Fitzpatrick, Susan Godlonton, David Lam, Edward Norton, Hitoshi Shigeoka, and Rebecca Thornton for their valuable comments. This paper also benefited from feedback from seminar participants at the Informal Development Seminar at the University of Michigan, the Population Association of America, and the University of Tsukuba.
Additional information
Funding
Notes
1. In this study, our interviewers approached women within each village without the census list of eligible women, because of the high probability of misreporting of eligible women in the list, as well as the small size of each village. The study lacks information on the refusal to participate in the baseline survey among women who were approached by our interviewers. As there were no follow-up visits to respondents in this study, there was no attrition.
2. Transportation costs were self-reported costs to visit the assigned health clinic using the mode of transport the respondent would typically use.
3. While the Nigerian DHS sampled women aged 15 to 49, we restricted the DHS sample to women aged 15 to 35 to compare with our sample. In the DHS sample, over half of the women were Muslim (57.3%), about half (49.6%) had never received any education, 14% were pregnant, and 62% engaged in paid work. Distinct from our sample, only a very small proportion of women in the DHS sample were single (2%), and most of them (96.3%) had at least one child. In the DHS sample, 31.8% of women had received a tetanus vaccination. The means of most variables in the DHS sample are not statistically different from those in our sample (results not shown).
References
- World Health Organization. Immunization, vaccines and biologicals: maternal and Neonatal Tetanus Elimination (MNTE). Geneva (Switzerland): World Health Organization; 2018.
- World Health Organization. Protecting All Against Tetanus: guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations. Licence: CC BY-NCSA 3.0 IGO. Geneva (Switzerland): World Health Organization; 2019.
- Oruamabo S. Neonatal tetanus in Nigeria: does it still pose a major threat to neonatal survival? Arch Dis Child. 2007;92(1):9–10. doi:10.1136/adc.2006.102087.
- Blencowe H, Lawn J, Vandelaer J, Roper M, Cousens S. Tetanus toxoid immunization to reduce mortality from neonatal tetanus. Int J Epidemiol. 2010;39(suppl_1):i102–i109. doi:10.1093/ije/dyq027.
- Ridpath D, Scobie M, Shibeshi E, Yakubu A, Zulu F, Raza AA, Masresha B, Tohme R. Progress towards achieving and maintaining maternal and neonatal tetanus elimination in the African region. Pan Afr Med J. 2017;27(Suppl):3. doi:10.11604/pamj.supp.2017.27.3.11783.
- Oyo‐Ita A, WiysongeC S, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low‐and middle‐income countries. Cochrane Database Syst Reviews. 2016;7.
- Johri M, Pérez C, Arsenault C, Sharma JK, Pai NP, Pahwa S, Sylvestre M-P. Strategies to increase the demand for childhood vaccination in low-and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. 2015;93:339–46. doi:10.2471/BLT.14.146951.
- Målqvist M, Yuan B, Trygg N, Selling K, Thomsen S, Middleton P. Targeted interventions for improved equity in maternal and child health in low-and middle-income settings: a systematic review and meta-analysis. PLoS One. 2013;8(6):e66453. doi:10.1371/journal.pone.0066453.
- Bassani G, Arora P, Wazny K, Gaffey MF, Lenters L, Bhutta ZA. Financial incentives and coverage of child health interventions: a systematic review and meta-analysis. BMC Public Health. 2013;13(3):S30. doi:10.1186/1471-2458-13-S3-S30.
- Ranganathan M, Lagarde M. Promoting healthy behaviours and improving health outcomes in low and middle income countries: a review of the impact of conditional cash transfer programmes. Prev Med. 2012;55:S95–S105. doi:10.1016/j.ypmed.2011.11.015.
- Lagarde M, Haines A, Palmer N. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database Syst Reviews. 2009;(4).
- Gertler P. Do conditional cash transfers improve child health? Evidence from PROGRESA’s control randomized experiment. Am Econ Rev. 2004;94:336–41.
- Barham T, Maluccio A. Eradicating diseases: the effect of conditional cash transfers on vaccination coverage in rural Nicaragua. J Health Econ. 2009;28(3):611–21. doi:10.1016/j.jhealeco.2008.12.010.
- Robertson L, Mushati P, Eaton W, Dumba L, Mavise G, Makoni J, Schumacher C, Crea T, Monasch R, Sherr L, et al. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster-randomised trial. Lancet. 2013;381(9874):1283–92. doi:10.1016/S0140-6736(12)62168-0.
- Morris S, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet. 2004;364(9450):2030–37. doi:10.1016/S0140-6736(04)17515-6.
- Salinas-Rodríguez A, Manrique-Espinoza S. Effect of the conditional cash transfer program Oportunidades on vaccination coverage in older Mexican people. BMC Int Health Hum Rights. 2013;13(1):30. doi:10.1186/1472-698X-13-30.
- Banerjee A, Duflo E, Glennerster R, Juszczak E, Joslin M, Alexander S. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ. 2010;340:c2220. doi:10.1136/bmj.c293.
- Gibson DG, Ochieng B, Kagucia EW, Were J, Hayford K, Moulton LH, Levine OS, Odhiambo F, O’Brien KL, Feikin DR. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): a cluster randomised controlled trial. Lancet Glob Health. 2017;5(4):e428–e438. doi:10.1016/S2214-109X(17)30072-4.
- Federal Ministry of Health Nigeria. Comprehensive EPI Multi-Year Plan 2016–2020. National primary health care development agency. Abuja (Nigeria); 2015.
- Demicheli V, Barale A, Rivetti A. Vaccines for women to prevent neonatal tetanus (Cochrane Review). Cochrane Lib. 2007;2.
- National Population Commission (NPC) [Nigeria] and ICF Macro. Nigeria Demographic and Health Survey 2008. Abuja (Nigeria): National Population Commission and ICF Macro; 2009.