 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
A recent measles importation-related outbreak in the China-Myanmar border region required outbreak response immunization to stop the outbreak, raising the question of measles immunity in the area. We conducted two measles serological surveys to develop a seroepidemiological profile of native Chinese citizens and registered Myanmar immigrants to identify strategies to promote measles elimination in the border region.
Methods
We conducted a clinic-based measles serosurvey of Myanmar registered immigrants (n = 300) and a population-based serosurvey of Chinese Lincang residents (n = 355). Serum samples were tested with enzyme-linked immunosorbent assays to assess immunity to measles.
Results
We found that Myanmar immigrants had a seropositivity rate of 85.3% (95% CI: 81.3–89.4) with a GMT of 924.9 mIU/ml, and Lincang Chinese nationals had a seropositivity rate of 94.6% (95% CI:92.3–97.0) with a GMT of 1363.3 mIU/ml. Myanmar children 2–6 years of age and 7–14 years of age were more likely to be susceptible to measles than same-aged Chinese children: odds ratios 23.00 (95% CI: 5.10–103.69, P < .001) and 7.95 (95% CI: 1.66–38.01,P = .009), respectively.
Conclusions
We recommend conducting a catch-up vaccination program for Myanmar children ≤15 years old.
Introduction
Yunnan Province is in southwest China and has an area of 394,000 km2, sharing 4,060 km of international border with Myanmar in the west and southwest and Vietnam and Laos PDR in the south. Six of Yunnan’s 16 prefectures together share a nearly 2,000 km-long border with Myanmar. According to the notifiable infectious disease reporting system in Yunnan, the locally reported measles incidence decreased from 1,478.21 cases per 100,000 population prior to 1965, the pre-vaccine era, to 678.58 cases per 100,000 population in 1965–1985, when measles vaccine was licensed but not in widespread use. In 1986–2005, following implementation of the Expanded Program on Immunization (EPI) that included measles as a free vaccination, the average reported measles incidence declined to 17.75 per 100,000 population in Yunnan. An accelerated measles elimination plan was initiated in 2006,Citation1 with key elements of the plan being achieving and maintaining two-dose measles-containing-vaccine (MCV) coverage above 95% through routine immunization, conducting supplementary immunization activities (SIAs) among children to close immunity gaps, employing a sensitive and specific measles surveillance system, and responding rapidly to outbreaks. The incidence of measles in Yunnan decreased by more than 95% between 2006 and 2016.
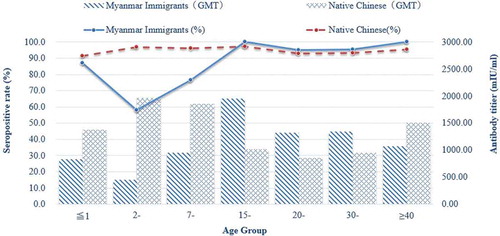
Figure 1. Geometric mean titers (GMTs) and prevalence of measles antibodies in different age groups by nationality. Myanmar immigrants data are from the clinic-based survey; Chinese resident data are from the population-based survey.
Myanmar EPI was launched in 1978 in 104 townships and was expanded to cover almost all areas of the 305 townships by 1997.Citation2 Myanmar’s EPI is supported by WHO, UNICEF, and Gavi, the vaccine alliance. Measles vaccine coverage level was 77% in 2016, with coverage in rural areas of 76%. Myanmar’s health infrastructure has challenges with high out-of-pocket expenditures, significant population movement, and difficult-to-traverse terrain.Citation3 Across the Myanmar border in Lincang city, Yunnan province, there were several recent outbreaks of measles and other infectious disease that included Myanmar nationals, raising the question of population immunity in the border region. We conducted two measles serological surveys to help understand population immunity and to develop local immunization strategies to promote elimination of measles in the border area. We report results of our surveys.
Results
Six hundred and sixty individuals (360 native Chinese in the population-based survey and 300 Myanmar immigrants in the clinic-based survey) were recruited for this study. Among these subjects, 350 (54.2%) native Chinese individuals and 300 (45.8%) Myanmar immigrants with adequate serum samples for virus IgG serology testing were included in our final analysis.
Myanmar registered immigrants’ seropositivity rate, based on the clinic survey, was 85.3% (95% CI:81.3–89.4%), with a GMT of 924.9 mIU/ml. Chinese citizens’ seropositivity rate, based on the population survey, was 94.6% (95% CI:92.3–97.0%), with a GMT of 1363.3 mIU/ml.
and show immunity levels among subjects in the two surveys. Among Myanmar immigrants, females were more likely to be seropositive to measles ( = 11.275, P = .001), as were individuals over 15 years of age; seropositivity was less than 65% for children 2 to 14 years of age (
= 53.482, P < .001). Among Chinese residents, seropositivity was 93% or above except for infants, at 91% (
= 0.112, P = .738). The GMT declined gradually from the highest level of 1970.1 mIU/ml among 2–6-year-olds to a low level of 851.1 mIU/ml among 20–29-year-olds (P < .001).
Table 1. Sero-epidemiological profiles by sex and age group among native Chinese residents and Myanmar immigrants.
shows susceptibility to measles and odds ratios of being susceptible between the Myanmar national population and the native Chinese population by sex and by age group. Overall, the odds of being susceptible to measles was 3 times higher for Myanmar immigrants than for Chinese citizens. The figure shows the seropositivity rates and GMTs by age group and nationality.
Table 2. Measles susceptibility and odds ratios of being susceptible by sex and age groups among native Chinese and Myanmar immigrants.
Discussion
Our study shows that (1) immunity against measles among Lincang city border-area residents was high – almost exactly at the 93% to 94% threshold necessary for measles elimination, (2) registered adult immigrants from Myanmar also had very high levels of immunity to measles, and (3) child-age registered immigrants from Myanmar had immunity levels less than 65%. Compared with same-age-group Lincang children, the odds of being susceptible to measles among registered Myanmar immigrant children was 7 to 23 times higher, posing a risk of measles importation and exportation when measles circulates in the border area.
Strengths of our study include that the laboratory testing was performed by a WHO Regional Reference Laboratory for measles and rubella, that the population-based survey was conducted via a house-to-house search for subjects, that the clinic-based survey was able to identify nationality of potential subjects, and that immunity was based on individual-level, objective, laboratory-based data. Limitations of our study are that the population-based survey was voluntary, potentially introducing bias in the sample frame; that reliable vaccination records were not available, precluding a study of concordance between serology and vaccination status; and that the clinic-based survey cannot be directly combined with the population-based survey because the proportion of Lincang residents who are Myanmar immigrants was not assessed in the study.
The Global Measles and Rubella Strategic Plan 2012–2020 states that serological surveys are useful tools to assess age-specific or population-specific measles susceptibility profiles and identify areas at risk of outbreaks.Citation4 In our study, we used serologic surveys to also assess potential risk of importation/exportation of measles.
Population immunity to measles has been assessed many times in China. For example, in 2008, Fu and colleagues found population immunity of 71% in southern China; Liu and colleagues found high and increasing immunity in Jiangsu province; and Xiong and colleagues found high immunity levels among children but lower levels among young adults.Citation5-Citation7 In our study, population immunity was high, but seropositive levels among registered immigrants were lower, at 85.3%, and immunity among immigrant children was much lower. National measles vaccination coverage in Myanmar was recently assessed to be 77%, which was below the national coverage target of 80%, and was less than 60% in some remote rural areas.Citation3
Measles has been eliminated in neither China nor Myanmar. According to World Health Organization measles surveillance data, Myanmar reported an incidence of 24.3 cases of measles per 100,000 in 2017,Citation8 significantly higher than the national incidence in China, estimated at two cases per 100,000 in 2013.Citation9 Our study is consistent with these population estimates and indicates a risk of measles importations across the Myanmar–China border. The high population-based immunity our study found in Lincang city indicates that the risk of further transmission may be moderate to low, but of concern is that clustering of susceptible individuals could facilitate measles transmission.
The >95% population-based seropositive rate provides some evidence of the impact of routine measles vaccination and SIAs in Yunnan province. Since 1986, reported coverage for the first MCV dose has been maintained at a high level, and second dose MCV coverage has reached 95% in Yunnan province since 2004, including in border areas. To accelerate measles elimination and address risk assessments showing potential for outbreaks, catch-up SIAs targeting children 8 months to 14 years were conducted province-wide in 2008 and 2010. In these SIAs, 8 806 673 children were vaccinated; SIA vaccination coverage of 97.9% was achieved in 2008, and 98.21% coverage was achieved in 2010.Citation10
Despite relatively high seropositive rates among young adults aged 20–39 years, our study showed that GMTs declined with age. Individuals in this age group were born after the 1978 implementation of EPI in China, but the oldest in this age group were born before the two-MCV-dose recommendation that was made in 1986. Our findings provide seroepidemiological evidence consistent with the shift in age distribution of measles cases in Lincang. Whether this is due to primary or secondary vaccine failure cannot be determined from our study, but as Ni and colleagues noted, outbreaks still occur in communities with high measles vaccine coverage, and susceptible adults may need to be vaccinated.Citation11
There are few natural barriers between Myanmar and China, and the border area has many highly mobile and migratory people. China currently has no measles vaccination requirements for entry to or return from other countries. Recently, there has been an increase in the number of Myanmar children to attend kindergarten and primary school in China, but there are no vaccination programs for cross-border children and school entry vaccination checks have not been effectively conducted among cross-border school children. Of additional concern, the population-dense settings of schools, factories, and refugee camps in which some migrants live or visit may create an environment conducive to transmission of measles and other infectious diseases. As an example, in 2009, an imported measles outbreak occurred in temporary shelters in the China-Myanmar border area.Citation12
We believe that our study supports several recommendations. First, catch-up vaccination with measles-rubella or measles-mumps-rubella vaccine should be conducted among susceptible cross-border children. Second, catch-up vaccination guidance for protecting cross-border children from vaccine-preventable diseases should be developed. Finally, establishment of a collaboration mechanism across this international border is crucial for improving immunization efforts. Such a mechanism should include sharing vaccination coverage data and conducting regular cross-border information sharing and planning meetings.
Materials and methods
We conducted two serological surveys – a population-based survey of Chinese citizens in two counties of Lincang city, and a clinic-based survey of Myanmar nationals visiting one of the six health centers in Lincang city who had blood drawn for reasons unrelated to measles.
Setting and subjects
Lincang city is an underdeveloped city of 2.5 million people in southwest Yunnan Province, adjacent to Kokang Special Administrative Region, with limited support from the Myanmar central government. An estimated 100,000 registered Myanmar immigrants enter China every year in Lincang city for a variety of reasons, including visiting friends and relatives, working in factories, construction, or agriculture; most come from underdeveloped areas of Myanmar with limited access to vaccination services.
We conducted the clinic-based serological survey in Gengma and Zhenkang counties of Lincang city from June to October in 2017. We selected three community health centers from each county; health-care providers in these six clinics recruited subjects who were Myanmar immigrants, 60 years of age or younger, who have been in China for at least 3 months, and whose visit included a blood draw for reasons other than measles.
We conducted a cluster sampling survey to assess measles immunity among Chinese citizens in Gengma and Zhenkang counties at the same time as the clinic-based survey. We selected nine villages at random from each county, and within each of the 18 villages, we selected an age-group-stratified sample of subjects. According the list of household registration of selected village in 2016, 20 households were randomly chosen within each village by systematic sampling, with a total of 965 individuals in 355 households which eligible subjects, 60 years of age or younger, were invited to participate. Three hundred sixty individuals participated and provided blood samples and completed the questionnaires.
In both surveys, subjects were excluded if they had an immunosuppressive condition or had an acute infection. Subjects were grouped into 7 age groups: ≤1year, 2–6years, 7–14years, 15–19 years, 20–29 years, 30–39 years, and ≥40years. Participants were asked to complete a questionnaire about demographic information, including sex, date of birth, residency status, and vaccination status. Serum samples were prepared and sent to Lincang Center for Disease Control and Prevention for laboratory analysis.
Laboratory assays
Anti-measles antibody (IgG) was assessed using commercially available ELISA kits (VirionSerion). Laboratory results were interpreted according to the manufacturer’s instructions. ELISA results were expressed quantitatively as optical density (OD) measured at 405 nm. Antibody activity (titers, mIU/ml) was calculated using software from SERION, and antibody titers were categorized as negative, equivocal, or positive using fixed cutoff values that were in agreement with international standards.Citation13 The positive cutoff value was 200 mIU/mL, and weakly positive samples (150–200mIU/mL) were considered equivocal. A value of <150mIU/mL was considered negative.
Statistical analysis
Data from the questionnaires were double entered into Epidata software, version 3.1 with edit and validation checks. Analyses were performed with SPSS, version 21.0. Subjects were categorized by nationality, sex, and age group. Seropositive rates among different groups were compared using Chi-square tests; 95% confidence intervals (CI) for proportions were calculated by exact binomial method. Geometric mean titers (GMT) were calculated using log-transformed titers and were reported as back-transformed titers. The significance of differences between GMT levels in the different subgroups was determined using unpaired t-tests. A linear regression model was used to test the trend of declining titers. Odds ratios (OR) were calculated for measles susceptibility in native Chinese and Myanmar immigrant residents. For all analyses, P values less than 0.05 were regarded as statistically significant.
Ethical considerations
Approval for the study was obtained from the Medical Ethics Committee of the Yunnan Provincial Center for Disease Control and Prevention. We obtained written informed consent prior to blood draws. Participant questionnaires were linked only by subject identifier.
Disclosure of potential conflicts of interest
The authors report no potential conflicts of interest.
Acknowledgments
We would like to thank the enrollees and staff in Lincang Center for Disease Control and Prevention (CDC), Gengma County CDC, Zhenkang County CDC for their effort in this study. We also thank Lance Rodewald for his suggestions and English polishing of our manuscript.
References
- National Health Commission of the People’s Republic of China. National plan of measles elimination in China 2006–2012; [accessed 2019 May 27]. http://www.nhc.gov.cn/xxgk/pages/viewdocument.jsp?dispatchDate=&staticUrl=/zwgkzt/wsbysj/201008/48328.shtml.
- Ministry of Health the Republic of the Union of Myanmar. Expanded program on immunization Myanmar multiyear plan 2012–2016. Ministry of Health The Republic of the Union of Myanmar; 2012.
- Han SM, Rahman MM, Rahman MS, Swe KT, Palmer M, Sakamoto H, Nomura S, Shibuya K. Progress towards universal health coverage in Myanmar: a national and subnational assessment. Lancet Glob Health. 2018;6(9):e989–e997. PMID: 30056050. doi:10.1016/S2214-109X(18)30318-8.
- World Health Organization. Global measles and rubella strategic plan 2012–2020. Geneva (Switzerland): WHO; 2012.
- Xiong Y, Wang D, Lin W, Tang H, Chen S, Ni J. Age-related changes in serological susceptibility patterns to measles. Hum Vaccines Immunotherapeutics. 2014;10(4):1097–103. PMID:24448194. doi:10.4161/hv.27734.
- Fu C, Xu J, Liu W, Zhang W, Wang M, Nie J, Rüdiger V. Low measles seropositivity rate among children and young adults: a sero-epidemiological study in southern China in 2008. Vaccine. 2010;28(51):8219–23. PMID: 20688039. doi:10.1016/j.vaccine.2010.07.071.
- Liu YB, Lu P, Hu Y, Wang Z, Deng X, Ma F, Tao H, Jia C, Ding X, Yang H, et al. Cross-sectional surveys of measles antibodies in the Jiangsu Province of China from 2008 to 2010: the effect of high coverage with two doses of measles vaccine among children. PLoS One. 2013 Jun 25;8(6):e66771. PMID: 23825562. doi:10.1371/journal.pone.0066771.
- World Health Organization. Measles and rubella surveillance data; [accessed 2019 Mar 15]. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/.
- Ma C, Hao L, Zhang Y, Su Q, Rodewald L, An Z, Yu W, Ma J, Wen N, Wang H, et al. Monitoring progress towards the elimination of measles in China: an analysis of measles surveillance data. Bull World Health Organ. 2014;92:340–47. PMID: 24839323. doi:10.2471/BLT.13.130195.
- Yu W, Huang GF, Luo M, LQ L, Zhang J, Li H, Ding ZR. Effect evaluation on supplementary immunization activities of measles attenuated live vaccine in Yunnan Province. Chin J Vaccine Immun. 2013;19:127–31.
- Ni JD, Xiong YZ, Li T, Yu XN, Qian BQ. Recent resurgence of measles in a community with high vaccination coverage. Asia Pac J Public Health. 2015;27(2):NP808–15. PMID: 22815303. doi:10.1177/1010539512451852.
- Zhang Y, Ding Z, Wang H, Li L, Pang Y, Brown KE, Xu S, Zhu Z, Rota PA, Featherstone D, et al. New measles virus genotype associated with outbreak, China. Emerg Infect Dis. 2010;16(6):943–47. PMID: 20507744. doi:10.3201/eid1606.
- Christenson B, Böttiger M. Measles antibody: comparison of long-term vaccination titres, early vaccination titres and naturally acquired immunity to and booster effects on the measles virus. Vaccine. 1994;12(2):129–33. PMID: 8147093. doi:10.1016/0264-410x(94)90049-3.
