 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background: This paper examines the association between access to a health facility and the continuum of child vaccination behaviors, which include: uptake of each vaccine, dropout, and timing of vaccine take-up in Nigeria.
Methods: The health facility census data (2014) were merged into the Nigeria Demographic and Health Survey (2013) to calculate the distance between respondents’ locations and the nearest health facility, and to evaluate its impact on the series of vaccination behaviors, using logistic and OLS regression.
Results: Among 21,369 children aged 12 to 59 months old, 78.2% of them were ever vaccinated. An additional distance of 1 km to the nearest clinic reduces the likelihood that one receives a vaccine by about 5% [OR: 0.952, 95% CI = 0.935–0.969]. Distance to the nearest clinic is mostly not associated with dropout rates in the vaccination series, but it delays the timing of vaccination, especially in the later stages of the vaccination series and Polio vaccination which require the mobilization from the supply side.
Conclusion: A longer distance to the nearest health facility is associated with lower vaccine take-up and delayed timing of vaccinations, but not with vaccine dropout. More studies should focus on the dynamics of vaccination decisions, in particular, the different determinants of vaccine take-up and dropout.
Introduction
Child vaccination is a proven tool to protect a population from deadly diseases. For example, in the U.S., the number of cases of measles decreased from 3 million before the invention of the measles vaccine to less than 100 cases per year after the introduction of the vaccine.Citation1 Although measles remains one of the leading causes of child mortality in Africa at present, the elimination of measles has been debated as a possibility, with the successful implementation of measles vaccination campaigns.Citation2
Despite the proven benefit of vaccines, child vaccination rates in African countries lag behind other regions of the world. Global coverage of the three-dose diphtheria-pertussis-tetanus (DPT3) vaccine has been stagnant at 85% since 2015, while DPT3 coverage in Africa has remained at 72% since 2010, partially due to rapid population growth.Citation3 The distribution of unvaccinated children is disproportionate: out of about 20 million infants around the world who are not fully vaccinated, more than 20% of them reside in three countries, one of which is Nigeria, the study site. Furthermore, Nigeria is one of the few countries where DPT coverage has decreased over time, from 54% in 2010 to 42% in 2017, although reasons of the decline are not clear.Citation3
Child vaccination is not a one-time behavior; rather, it involves repeated actions within a specific timeframe. In Nigeria, child vaccination means that a child receives 10 different vaccines in total, at different time points: at birth, and 6, 10, 14 weeks, and 9 months after birth.Citation4 Not only are the vaccination rates low, but high dropout rates and high proportions of delayed vaccinations are also prevalent in Africa.Citation5-Citation7 In Nigerian context, some studies examined the prevalence of full vaccination, partial (or under) vaccination, and never vaccination.Citation8,Citation9
Several studies found that access to a health facility is associated with a greater likelihood of vaccinations in African countries.Citation10-Citation12 This paper contributes to the literature by comparing the impact of distance on multiple vaccination outcomes, namely, the take-up of each vaccine, the dropout from one dose to another, and the timeliness of vaccine take-up by linking multiple datasets, household survey and health facility census data.Citation13 This study evaluates the association between access to a health facility and the continuum of vaccination behaviors, using a health facility census and a household survey from Nigeria.
Methods
Data
The analysis uses two data sets. One is the health facility census data, which include all the clinics in Nigeria. The data is publicly available online from the Nigeria MDGs (Millennium Development Goals) Information System (NMIS) health facility database (2014). The data have a complete list of health facilities existing in Nigeria in 2013. The database includes 34,120 clinics that have valid location information. The NMIS health facility database contains information for each clinic about the location, facilities, and services provided, and personnel employed. The information regarding location includes state, local government area (LGA), and GPS coordinates. This health census data do not contain the information whether each health clinic provides vaccination services or not. The analysis is conducted under the assumption that all health facilities provide vaccination services.
The other dataset used in the analysis is the Nigeria Demographic and Health Survey (DHS) conducted in 2013,Citation14 which contains various pieces of information on respondents, including GPS coordinates for clusters where respondents reside. From the DHS data, vaccination records of respondents’ children for each vaccine are used. The data contain information on the month and year of vaccination for each dose of vaccine that children aged between 0 and 59 months old received within 5 years prior to the survey.
Outcome variables
The paper uses three different indicators to characterize the vaccination behavior: 1) vaccine take-up for each type of vaccine: any vaccine, BCG, DPT, Polio, and measles, 2) dropout from one dose to the subsequent dose for DPT and Polio 3) timing of vaccination (the number of months and days from birth to the vaccination) for BCG, DPT, Polio, and measles. The analysis focuses on children aged 12 to 59 months old. The analysis on vaccine take-up and dropout relies on self-reported responses for this information, regardless of records in vaccination cards. The analysis on timing of vaccinations focuses on all the children aged 12 to 59 months who already had received each type of vaccine with valid vaccination records on the date of vaccination. The number of months and days from birth to vaccination for a child is calculated using his/her birthdate and the date when he/she received each vaccination. This analysis does not define the delay, rather simply evaluates the number of months since birthCitation15,Citation16
Main independent variable
The main independent variable is the distance between a respondent’s location and the nearest health facility. This distance is measured by merging DHS data that contain the GPS coordinates of clusters where respondents reside, and the health facility census data, which contain accurate GPS coordinates of each health facility in Nigeria. Using these GPS coordinates, the distance from each respondent’s location in the DHS data to all the existing health facilities in the facility census data is calculated. Then, out of all the distances from each respondent’s location calculated, the minimum distance is identified and is used as the distance to the nearest health facility.
Statistical analysis
To evaluate the association between distance to the nearest health facility and vaccination behaviors, logistic regression is employed in the following regression framework:
where is an outcome, in this case either vaccine take-up or dropout, of a respondent’s child i in a cluster j;
indicates the distance in kilometers from a respondent i’s cluster to the nearest health facility. Various sociodemographic characteristics of women, their households, and their children are controlled for, such as: women’s age, education level, marital status, number of household members, number of children under 5 years old, wealth level, child’s gender, and birth order. Strata fixed effects (v) which refer to the interactions between the state and type of residence (urban or rural) are also controlled for. The strata fixed effect controls for any observable and unobservable characteristics at the strata level that is correlated with vaccination rates within the strata.
Similarly, to evaluate the association between the distance to the nearest health facility and the timing of vaccination (the number of months from birth to vaccination), a negative binominal regression within the same regression framework as EquationEquation (1)(1)
(1) is employed, with
being the count variable that represents the timing of the vaccine take-up (months since birth).
Results
There was a total of 28,364 children aged 0 to 59 months old. The number of children aged 12 to 59 months was 22,173. From this pool, the analytical sample of 21,369 children with no missing information on their vaccine take-up of each vaccine was drawn. (Panel A) presents the vaccination rates of children in the analytical sample by the type of vaccine and by the timing of the vaccination schedule. Overall, 78.2% of the children ever received at least one vaccination. Children are recommended to receive certain types of vaccines at certain times. Here is a summary of the vaccine schedule for each vaccine with the current vaccination rate in parentheses: at birth for BCG (53.5%) and Polio0 (45.4%), at 6 weeks for DPT1 (52.4%) and Polio1 (75.1%), at 10 weeks for DPT2 (48.2%) and Polio2 (70.3%), at 14 weeks for DPT3 (41.9%) and Polio3 (53.9%), and at 9 months for measles (47.3%).
Figure 1. Vaccination rate
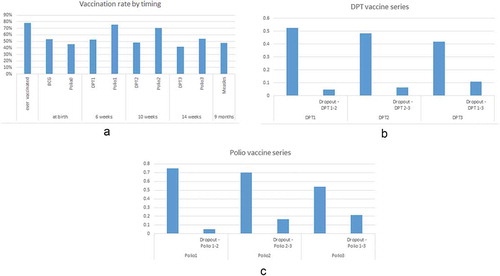
(Panel B) presents the vaccination and dropout rates of the DPT vaccine series. The take-up of DPT1 is 52.4% and the dropout rate from the first (DPT1) to second (DPT2) dose is 4.5%. For DPT2, the take-up is lower and the dropout from DPT2 to DPT3 is higher, at 48.2% and 6.4%, respectively. The take-up of DPT3 is 41.9% and the dropout from the first (DPT1) to the third (DPT3) is 10.8%. Similarly, Panel C presents the vaccination and dropout rates of the Polio vaccination series. The pattern of the Polio vaccination series is similar to that of the DPT vaccination series, but with higher take-up and dropout rates.
presents descriptive statistics for the sample of children aged 12 to 59 months. Respondents are referred to as mothers. The average age of mothers is 29.9 years old, and 45.5% of the mothers have no educational attainment, while only 6.6% of them have an educational attainment higher than secondary school. More than half of mothers are Muslim (57%) while the others are Christian. More than 90% (92.4%) of mothers are married. The average number of household members is 7.1 and the number of children under the age of five in the household is 2.2. The sampled households are almost equally divided into five categories in terms of wealth level (poorest, poorer, middle, richer, and richest), with a higher proportion of households belonging to the poorest (21.5%) and poorer (22.3%) levels and a smaller proportion belonging to the richest (16.9%) level. In the sample, the average age of children is 34 months and their average birth order is 3.9. About half of the children in the sample are girls (49.8%). The average distance between a respondent’s location and the nearest health facility is 2.04 km.
Table 1. Socio-demographic characteristics of sample (n = 21,369)
presents the association between distance to the nearest health facility and vaccine take-up. Overall, an increase in distance to the nearest health facility by 1 km is associated with a reduction in the likelihood of receiving any vaccine by 5% [OR: 0.952, 95% CI = 0.935–0.969]. A robust and consistent result for other types of vaccines are observed as well: the further the nearest health facility is, the less likely that a child receives the vaccine. The odds ratio varies from 0.911 [95% CI = 0.890–0.933] for BCG to 0.954 for Polio 0 [95% CI = 0.937–0.971].
Table 2. Results of logistic regression for effect of distance on vaccine take-up
presents the association between distance to the nearest health facility and dropout from one dose to the subsequent dose for the DPT and Polio vaccinations. Contrary to its impact on vaccine take-up, distance is mostly not significantly associated with the likelihood of dropout. Rather, for DPT, distance is associated with a decreased likelihood of dropout from the second to the third dose by 3.3% [95% CI = 95% CI = 0.936–0.999] (column 2). Similarly, the dropout of Polio from the second to the third dose decreases as the distance increases by 1.4%, though this is insignificant.
Table 3. Results of logistic regression for effect of distance on vaccine dropout
presents the association between distance to the nearest health facility and the timing of vaccination (the number of months from birth to vaccination) among children who had already received the vaccination. The distance to the nearest health facility is not significantly associated with the timing of the following vaccination; BCG, DPT series, and Polio 3. On the other hand, for some vaccines especially measles and polio series, we find the positive association between distance and the vaccination timing. Among vaccinated children, an increase in distance to the nearest health facility by 1 km is associated with a delay in measles vaccination by about 1 month (column 8). A similar association is observed for Polio 0, 1, and 2.
Table 4. Results of negative binominal regression for effect of distance on timing of vaccination
Discussion
This paper evaluates the association between access to a health facility and the continuum of vaccination behaviors, which include: take-up of each vaccine, dropout, and timing of vaccination. The proportion of children who are vaccinated at least once is 78.2%. For both DPT and Polio vaccines, a dropout rate is more than 10% from the first dose to the third dose. The vaccine take-up of time-sensitive vaccines such as BCG and Polio 0, which are scheduled to be received at birth, as well as the vaccines that should be taken toward the later stages of the vaccination schedule such as DPT3 and measles, is particularly low.
Distance to the health facility is a significant barrier to vaccine take-up, regardless of the type of vaccine. This is consistent with findings from existing studies.Citation17 The largest impact of distance is on BCG: there is an almost 9% reduction per kilometer of distance to the health facility. Infants are scheduled to receive BCG at birth. Because a large proportion of women do not practice institutional delivery in Nigeria, BCG take-up might be more challenging and thus it may be low among women who deliver at home. Furthermore, BCG vaccines are not recommended after 12 months of age, while other vaccines do not have such an upper limit on age for the vaccine take-up.Citation18 It is possible that the time-sensitive nature of the BCG schedule augments the negative impact of distance on vaccine take-up, as compared to other vaccines.
The take-up of the Polio vaccine is much higher than that of the DPT vaccine, although the scheduled vaccination timing is the same. In Nigeria, Polio vaccines are usually given to children through door-to-door campaigns, thus there is no need for caregivers and children to travel to health facilities. This is presumably the reason why the vaccination rate of Polio vaccine series is much higher than that of DPT (). For the same reason, the impact of distance can be smaller for the Polio vaccines than the DPT vaccines. Indeed, while an additional distance of 1 km reduces the likelihood of DPT1 vaccine take-up by 7% [OR: 0.929, 95% CI = 0.909–0.951], the impact is 4.6% for Polio 1 [OR: 0.954, 95% CI = 0.937–0.971]. Nevertheless, a negative impact of distance on vaccination is observed regardless of the type of vaccine (Polio, DPT, or measles), although there are some differences in the magnitude of the impact. This result implies that the Polio vaccine take-up in remote areas, which are far from health facilities, is still hindered by distance from the health facility to the community. But in the case of Polio vaccinations, the barriers come rather from the supply-side: the distance from the health facility to the community is an obstacle faced by health workers.
Although difficult access to a health facility is a significant barrier to vaccine take-up, dropout is not affected by distance to a health facility for most types of vaccinations. In other words, once people initiate the vaccination series, the longer distance to a health facility does not prevent them from completing the vaccination series. This result is not consistent with some of existing studies. For example, Haji et al.Citation19 found that distance to health facility is one of the challenges for minimizing the dropout.
In this study, on the contrary, the dropout from DPT2 to DPT3 rather decreases as the distance becomes longer. This counter-intuitive result might be due to the selection: among caregivers who reside further away from the health facility, only those with a higher willingness to have their children receive vaccines initiate the children’s vaccination series. As a result, among caregivers of children who initiated the DPT vaccination series, caregivers who are far from the clinic are more motivated than caregivers who are near the clinic. Then, distance might be negatively associated with dropout rate from the second to the third dose through its impact on their willingness to receive the vaccine. This result implies that access to a health facility is the barrier to the initiation of the vaccination series, but not to its continuation.
Difficulty in access to a health facility delays the timing of measles vaccine take-up: an additional 1 km to the health facility delays the measles vaccine take-up by about 1 month. A delay of 1 month for every kilometer is substantial, given that the average distance to the nearest health facility is about 2 km. Except for Polio vaccines that require the mobilization from supply-side, the timing of vaccinations at early stages (BCG, DPT series) is not associated with the distance. Difficult access to a health facility does not significantly influence the timing of vaccination at early stages (BCG and DPT series), while it has a significant negative impact on the vaccination that are scheduled later (measles). Because it is observed that further distance is significantly associated with the delay in Polio vaccinations, it might imply that health workers respond more sensitively to the difficult access than caregivers. A meta-analysis finds that the evidence of the impact of distance to health facility on the timeliness of vaccination is scarce.Citation16 Future studies should explore more on the impact of access on the timeliness.
Overall, distance to a health facility is a significant barrier to initiation of the vaccination series, but not to dropout from one dose to the subsequent one. Although difficult access to a health facility does not cause the dropout, it does delay the timing of vaccinations, especially toward the end of the vaccination series and Polio vaccinations which require the mobilization from the supply side. These results have an important policy implication. If children live far from the clinic, they are less likely to initiate the vaccine series. On the other hand, if they live near to the clinic, they are more likely to drop out in the middle of the vaccine series without completion. To increase vaccine take-up among children with difficult access to the clinic and to decrease dropout among children with relatively easy access to the clinic, policy interventions that can increase people’s willingness to receive the vaccination may be effective, as pointed out by existing studies.Citation20 Another realistic policy intervention can be to improve the road infrastructure to ease the transportation burden.Citation21
Limitations
There are some limitations in this study. A main limitation is that the GPS coordinates of the location where each respondent resides in the DHS data contain random errors. To protect respondents’ confidentiality, GPS coordinates for each respondent are first aggregated and only the GPS coordinates for the cluster where respondents reside are shown. Furthermore, GPS coordinates for each cluster are masked by adding random errors. The inaccuracy in household locations creates an attenuation bias for the estimated coefficient of the distance to the nearest health clinic. Another limitation of the study is the lack of causal interpretation. Because the location of the health clinic is likely to be endogenous, this study does not examine the causal effect of access to the health clinics: the results can be interpreted only as an association. For the analytical sample, children up to 59 months old are included instead of 24 months to increase the sample size as much as possible. While the analysis benefitted by expanding the sample in this way, it might be subject to recall and survival bias. Finally, children from the same respondents are likely to behave in a similar way. The regression analysis is unable to take this factor into account because distance measurements for these children have the same value. Finally, the analysis of vaccination timing suffers from the smaller sample size because many observations on the date of vaccination are missing in DHS data.
Conclusion
This study evaluates the association between access to a health facility and the continuum of vaccination behaviors including vaccine take-up, dropout, and timing of vaccination among Nigerian children. Distance to the nearest health facility is found to be negatively and significantly associated with vaccine take-up, while the dropout rate is mostly not influenced by access to a health facility. It is also found that delays in vaccine take-up due to difficult access to a health facility is prevalent especially toward the end of the vaccination series and Polio vaccinations which require the mobilization from the supply side. Future studies should focus on the continuum of vaccination decisions, in particular, the different determinants of vaccine take-up and dropout; which factors influence both the vaccine uptake and dropout and which factors influence the vaccine uptake but not dropout, and vice versa. Future studies should also evaluate policy interventions that can motivate caregivers toward vaccination initiation and continuation, separately or jointly.
Disclosure of potential conflicts of interest
The author declares that she has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Funding
References
- Meissner HC, Strebel PM, Orenstein WA. Measles vaccines and the potential for worldwide eradication of measles. Pediatrics. 2004;114:1065–69.
- Moss WJ, Griffin DE. Global measles elimination. Nat Rev Microbiol. 2006;4:900.
- UNICEF, and World Health Organization. Progress and challenges with achieving universal immunization coverage: 2016 estimates of immunization coverage WHO. 2017.
- World Health Organization. WHO vaccine-preventable diseases: monitoring system. 2018 global summary. World Health Organization; 2018.
- Kazungu JS, Adetifa IMO. Crude childhood vaccination coverage in West Africa: trends and predictors of completeness. Wellcome Open Res. 2017 Feb 15;2:12. doi:10.12688/wellcomeopenres.10690.1.
- Mbengue MA, Mboup A, Ly ID, Faye A, Camara FB, Thiam M, Ndiaye BP, Dieye TN, Mboup S. Vaccination coverage and immunization timeliness among children aged 12–23 months in Senegal: a Kaplan-Meier and Cox regression analysis approach. Pan Afr Med J. 2017 Jun 21;27(3):8. doi:10.11604/pamj.supp.2017.27.3.11534.
- Mutua MK, Kimani-Murage E, Ngomi N, Ravn H, Mwaniki P, Echoka E. Fully immunized child: coverage, timing and sequencing of routine immunization in an urban poor settlement in Nairobi, Kenya. Trop Med Health. 2016;44:13.
- Chido-Amajuoyi O, Greg CW, Mantey D. Perez A, Mcalister A. Prevalence and correlates of never vaccinated Nigerian children, aged 1–5 years. Vaccine. 2018;36:6953–60.
- McGavin ZA, Wagner AL, Carlson BF, Power LE, Eboreime E, Boulton ML. Childhood full and under-vaccination in Nigeria, 2013. Vaccine. 2018;36:7294–99.
- Jani JV, De Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health. 2008;8:161.
- Shemwell SA, Peratikos MB, González-Calvo L, Renom-Llonch M, Boon A, Martinho S, Cherry CB, Green AF, Moon TD. Determinants of full vaccination status in children aged 12–23 months in Gurùé and Milange districts, Mozambique: results of a population-based cross-sectional survey. Int Health. 2017;9:234–42.
- Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr. 2015 Apr 1;15:31. doi:10.1186/s12887-015-0345-4.
- Poorolajal J, Khazaei S, Kousehlou Z, Bathaei S, Zahiri A. Delayed vaccination and related predictors among infants. Iran J Public Health. 2012;41:65–71.
- National Population Commission (NPC) [Nigeria] and ICF International. Nigeria demographic and health survey 2013. Abuja (Nigeria, and Rockville, Maryland, USA): NPC and ICF International; 2014.
- Dolan SB, Carnahan E, Shearer JC, Beylerian EN, Thompson J, Gilbert SS, Werner L, Ryman TK. Redefining vaccination coverage and timeliness measures using electronic immunization registry data in low-and middle-income countries. Vaccine. 2019;37:1859–67.
- Masters NB, Wagner AL, Boulton ML. Vaccination timeliness and delay in low-and middle-income countries: a systematic review of the literature, 2007–2017. Hum Vaccin Immunother. 2019;1–16.
- Phillips DE, Dieleman JL, Lim SS, Shearer J. Determinants of effective vaccine coverage in low and middle-income countries: a systematic review and interpretive synthesis. BMC Health Serv Res. 2017;17:681.
- World Health Organization. Department of Immunization and Biologicals. Immunization in practice: A practical guide for health staff. World Health Organization; 2015
- Haji A, Lowther S, Ngan’ga Z, Gura Z, Tabu C, Sandhu H, Arvelo W. Reducing routine vaccination dropout rates: evaluating two interventions in three Kenyan districts, 2014. BMC Public Health. 2016;16:152.
- Jheeta M, Newell J. Childhood vaccination in Africa and Asia: the effects of parents’ knowledge and attitudes. Bull World Health Organ. 2008;86:419.
- Metcalf CJE, Tatem A, Bjornstad ON, Lessler J, O’REILLY K, Takahashi S, Cutts F, Grenfell BT. Transport networks and inequities in vaccination: remoteness shapes measles vaccine coverage and prospects for elimination across Africa. Epidemiol Infect. 2015;143:1457–66.
