ABSTRACT
Background: Despite long standing recommendations of pneumococcal and influenza vaccination for adults age 65 years and older and wide-spread availability to vaccination services, vaccination coverage in the United states is low. We sought to explore reasons patients reportedly did not receive these vaccines.
Methods: We used publicly available data from the Medicare Current Beneficiary Survey, a continuous panel survey of a representative sample of the Medicare population, as well as Medicare enrollment data. We explored questions pertaining to influenza and pneumococcal vaccination status, self-reported reasons for being unvaccinated and patient perspectives toward health care utilization.
Results: The majority of the respondents who did not receive vaccines for influenza or pneumococcal disease reported that they did not know it was needed or that their doctor did not recommend it. Respondents who were not vaccinated against influenza reported concerns about side effects. Coverage for both vaccines was lower among respondents in the Southeast region and among those who are dual-eligible or less engaged in healthcare utilization. Little difference was observed by gender, urban status, or Part C enrollment for influenza respondents. Higher pneumococcal vaccine coverage was found among females as well as those living in urban settings or enrolled in Medicare Part C.
Conclusions: Implementation of the national guidelines calling for all health care professions – whether they provide vaccinations or not – to take steps to help ensure adults are fully immunized is critical. Tailored communication to beneficiaries that addresses the importance of both vaccines as well as key barriers, like side effects, is also needed.
Introduction
Federal vaccine recommendations for older adults date back to 1960 when the availability of inactivated influenza vaccine and the recurring burden of influenza and its complications led the U.S. Surgeon General to issue the first recommendation for routine annual influenza vaccination of older adults, pregnant women, and others with chronic conditions.Citation1 Two decades later – in 1983 – the Advisory Committee on Immunization Practices (ACIP) recommended the pneumococcal polysaccharide vaccine for adults aged ≥65 years.Citation2 Recently, in 2014, the ACIP updated the recommendation to include the routine use of 13-valent pneumococcal conjugate vaccine (PCV13) in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23).Citation3 These two routinely recommended vaccines comprise an important part of the adult vaccination schedule and components of prevention that support healthy aging.Citation4
Adhering to the ACIP’s recommendations is critically important for older adults. Older adults are more likely to have chronic health conditions that increase the risk of life-threatening infections and severe health outcomes that these vaccines serve to prevent. For example, older adults comprise only 15% of the U.S. population; however, they account for more than half of influenza-associated hospitalizations and pneumonia and influenza deaths.Citation5 Additionally each year in the United States, pneumococcal disease kills an estimated 16,000 adults age 65 years or older with thousands hospitalized because of associated infections of the lungs, bloodstream and lining of the brain and spinal cord.Citation6
Vaccination is the best way to prevent influenza and pneumococcal disease.Citation6,Citation7 ACIP recommendations, Medicare insurance coverage with no out-of-pocket cost to the Medicare beneficiary, and multiple access points for vaccination services create an enabling environment so support vaccination. However, vaccination coverage in the 2014–2015 influenza season, according to the National Health Interview Survey, was estimated at 73.5% of adults age 65 years and older, with room to improve.Citation8 In 2015, pneumococcal vaccination coverage was estimated at 63.6%, with coverage among white beneficiaries (68.1%) exceeding that of blacks (50.2%), Hispanics (41.7%), and Asians (49.0%).Citation8 Healthy People 2020 has established science-based national targets for immunization to improve coverages rates and the health of all Americans.Citation9 Such targets include increasing the percentage of institutionalized adults aged 18 years and older in long-term or nursing homes who are vaccinated annually against seasonal influenza to 90%. Recent 2015–2016 estimates for influenza vaccination were at 74.8%.Citation10 The Healthy People 2020 target for increasing the percentage of noninstitutionalized adults aged 65 years and older who are vaccinated against pneumococcal disease is 90%. Recent 2016 estimates were at 66.9%.Citation11 Vaccination coverage rates for these ACIP-recommended vaccines can be improved.
Many factors contribute to low adult immunization rates, including limited awareness about vaccine recommendations, a lack of tools that assist providers in implementing complex vaccine schedules, and gaps in routine vaccine needs assessments during health care visits.Citation12–Citation14An individual’s capacity to undertake certain activities and other characteristics, like patient perspectives on healthcare utilization, may also factor into health-related and vaccine-related knowledge. The World Health Organization “3Cs” model on the determinant categories to vaccine hesitancy – confidence, convenience, and complacency – describe factors that affect decision-making for vaccination.Citation15 Vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite availability of vaccine services. This concept is complex and context specific varying across time, place and vaccines and is influenced by factors such as confidence, complacency, and convenience.Citation15 Confidence is trust in not only the effectiveness and safety of vaccines, but the system that delivers vaccinations and the motivations of policy-makers who recommend them. Many dimensions of convenience, the second C in the model, such as availability of vaccine and affordability do not pose as barriers to vaccination for the Medicare beneficiary as there are no shortages of adult vaccines (for influenza and pneumococcal vaccines; there is currently a shortage of a newly licensed shingles vaccine) and no cost-sharing (i.e., co-payment, co-insurance, or deductible) to the patient. However, other dimensions of convenience such as health literacy are factors that may play into decision making to vaccinate. Complacency, the perceived risk of vaccine preventable disease and that vaccination is deemed as unnecessary, is the third C that comprises the 3Cs model. Other life and health factors may be a higher priority in an individual’s life, thus again, affecting whether or not a beneficiary sees a vaccinator and consequently the decision making to vaccinate. Understanding why patients do not receive vaccines can inform the development of targeted vaccination strategies, interventions, and communications. This paper explores pneumococcal and influenza vaccinations coverage including differences among demographic groups among Medicare beneficiaries and reasons beneficiaries cite for not receiving these routinely recommended vaccines.
Methods
For this study we used publicly-available data from the Medicare Current Beneficiary Survey (MCBS) spanning the years 2001–2013. Administered by the Centers for Medicare and Medicaid Services (CMS), the MCBS is a continuous, longitudinal panel survey of a representative sample of the Medicare population. It contains questionnaires covering demographic and socioeconomic characteristics, household information, health status and functioning, preventive services, and access to and satisfaction with medical care. Overall, the MCBS is designed to better understand the utilization and quality of CMS services by capturing beneficiary information beyond what is available in administrative claims data.
For this study in particular, we focused on self-reported answers to questions about the influenza and pneumococcal vaccination status of both facility and community respondents. Among community patients who report being unvaccinated, MCBS includes follow-up questions identifying the reason(s) for being unvaccinated. For this study we also investigated MCBS questions about health care utilization and patients’ perspectives on visiting their doctors (e.g., “Do you avoid going to the doctor?”) and assessed the correlation between these responses and patient vaccination status. Data from the Medicare Enrollment Database were also used to further assess and validate demographic characteristics. This study was subset to patients ages ≥65 years who represent the broad older adult population. Medicare beneficiaries younger than 65 tend to be covered due to disability or end-stage renal disease and therefore are characteristically different than their older counterparts; for this reason they are excluded from the study population. We used a minimum 500 respondents and a > 5% difference heuristic as means to identify differences between demographic groups. For responses on the Health Literacy questions we used greater than 1000 respondents for both Yes and No responses and a > 5% difference from the overall vaccinated/unvaccinated distribution to identify important differences between responses.
Results
Respondent cohort
Each year, approximately 14,000 community patients (i.e., those non-institutionalized) and 1,000 facility patients (e.g., those in a long-term care facility) participate in the MCBS (). The survey is a representative national sample of the Medicare population and the demographics of the survey respondents have been described elsewhere.Citation16 For example a majority of Medicare beneficiaries are between the ages of 65 and 84 (71%); more than half of beneficiaries (55%) are female, but women account for an even larger share of beneficiaries at older ages; and more than three-quarters (77%) of beneficiaries are white.Citation16 The analyses were restricted to beneficiaries age 65 years and older. Beneficiaries under age 65 and permanently disabled (16%) were excluded.Citation16
Table 1. Demographics characteristics of respondents who received influenza and pneumococcal vaccinations, 2013
Influenza and pneumococcal responses
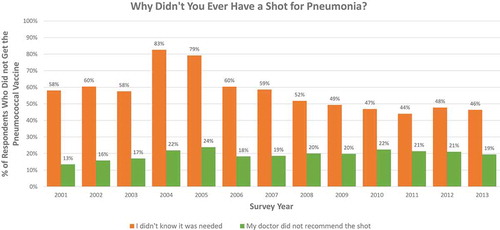
Annual influenza vaccination rates increased from 68% in 2001 to 75% in 2013 among community respondents and from 76% to 81% among facility respondents. In 2013, 24% of community respondents (n = 2,738) reported not receiving the vaccine during the prior influenza season. Three common reasons were “The shot could have side effects or cause disease” (23%), “I didn’t know it was needed” (12%), and “The shot could cause influenza” (10%). Throughout the study period these are the three most frequent responses; > 10% of unvaccinated respondents provided this response in every year of the study. Not knowing the shot was needed and concerns of the shot causing the flu have become less common, whereas concerns about side effects have increased ().
Figure 1. Top three reasons reported for not getting the influenza vaccine
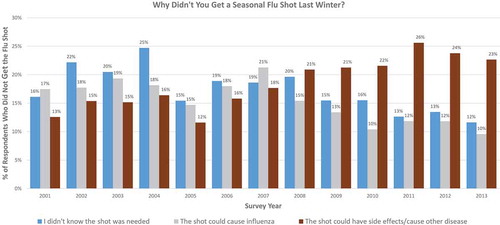
Pneumococcal vaccination coverage rates also increased from 65% in 2001 to 74% in 2013 among community respondents and from 60% to 79% among facility respondents. In 2013, 24% of community respondents (n = 2,764) reported not ever receiving the pneumococcal vaccination. The two most common reasons throughout the study period for community respondents for not having received a pneumococcal vaccine are “I didn’t know it was needed” (46% in 2013) and “Doctor did not recommend the shot” (19% in 2013) (). Similar to the influenza vaccine, a lack of beneficiary knowledge about the pneumococcal vaccine (i.e. not knowing it was needed) is declining over time. Meanwhile, citing a lack of doctor recommendation has slowly increased ().
Additional responses
Additional response options for both influenza and pneumococcal vaccines are not displayed in and because they were consistently uncommon among respondents (< 10%) and did not vary over time. These include, for example, “Didn’t think it would prevent the flu/pneumonia”, “Flu not serious/not at risk”, “Risk of catching flu/pneumonia”, “Doctor recommended against/allergic”, “Don’t like shots or needles”, “Inconvenient/Unable to get to location”, “Didn’t think about it/forgot”, “Cost of shot/not worth the cost”, and “Other.” Two additional responses were available exclusively for the influenza vaccine: “Had the shot before, don’t need it again,” and “Vaccine unavailable.”
Vaccination coverage rates by demographic and other variables
There was relatively little difference in influenza and pneumococcal vaccination rates by gender, Part C (Medicare Advantage) enrollment, and urban status among vaccinated beneficiaries (). Vaccination coverage was lower among Blacks, in comparison to Whites, those living in the southeast, compared to other regions (though less so for pneumococcal vaccination relative to influenza vaccination), and those who are dual-eligible for Medicare and Medicaid (). Additionally, patients who avoid going to the doctor are less likely to report being vaccinated than those who do not: 66% v. 79% for influenza and 67% v. 76% for pneumococcal ().
Table 2. Health care utilization of influenza and pneumococcal vaccine respondents by vaccination status, 2013
Discussion
Increases in vaccination coverage for both vaccines over the study period are promising for public health. We expect higher coverage in facilities given increased access to healthcare providers as beneficiaries reside in these institutions. National reporting of clinical quality and performance measure for influenza and pneumococcal are incentives programs that may have in part driven increases in vaccination coverage. However, this study supports the notion that many adults are not aware of recommended vaccines, a first step to getting vaccinated ( and ). Vaccines are now available across the lifespan beyond the early childhood series of vaccines often required for entry into daycare and school. Because adult vaccination coverage in general is well below national targets, concerted efforts have been launched to move beyond the belief that vaccines and vaccinations are primarily for children and to implement the National Vaccine Advisory Committee (NVAC) adult standards for providers.Citation8–Citation14
The NVAC recommendations state that all health care professionals, whether they provide vaccinations or not, can take steps to ensure all adults are fully vaccinated by providing vaccinations or referring individuals to places where patients can get vaccinated.Citation14 Moreover, providers should take a “presumptive” approach in communicating vaccination with patients which assumes patients will receive recommended vaccinations versus a “participatory” approach which invites involvement. The presumptive approach is proactive and a non-adversarial approach that guides patients and serves an important role in stressing that vaccination is the norm, while building public trust in vaccination.Citation17,Citation18 The results in this study highlight the importance of engaging in an approach that provides an effective recommendation that leads to vaccination as many beneficiaries are not aware of recommended vaccinations. While reasons reported for not receiving influenza vaccine included concerns about safety as well as not knowing vaccination was needed, the two most common reasons for not receiving a pneumococcal vaccine included not knowing it was needed and the lack of a doctor recommendation. The provider recommendation is critical because an effective interaction between the provider and beneficiary can address concerns of vaccine supportive patients and motivate hesitant patients to vaccine acceptance.Citation17,Citation18
The patient population in this study represents a cohort of older adults that has numerous contact points with providers, increasing the number of opportunities for providers who see these patients to assess and vaccinate or refer the patient for vaccination services. Optimizing each opportunity with a beneficiary is a central strategy to increasing awareness and knowledge about the importance and benefits of vaccines and the diseases that can be prevented as well as vaccination as an outcome of provider-patient engagement. This study points to the need for further research to explore how healthcare providers approach and frame vaccination recommendations and vaccination opportunities. Opportunities, including the Medicare Annual Wellness visit, are critical touchpoints between the patient and the healthcare system to assess vaccination status, and proactively recommend vaccination.Citation19 This study also showed that dual eligible beneficiaries with both Medicare and Medicaid insurance coverage have lower vaccination levels (). This may be in part attributed to attitudes on healthcare utilization and levels of health literacy of dual-eligible (versus non-dual eligible) Medicare beneficiaries among other factors such as social determinants of health (e.g., housing and income instability). Further research should be done to better understand the specific differences between dual-eligible and non-dual-eligible populations.
Addressing vaccine hesitancy is individualized and must be a tailored approach.Citation15 How individuals respond to and interact with the health care system is critical to supporting vaccination seeking behavior and ultimately increase vaccination coverage rates. This study provides some exploratory insight into populations to prioritize and target for interventions, and begins to diagnosis some reasons for not receiving vaccines. Findings from this study indicate that Medicare beneficiaries are increasingly citing the reason for not receiving an annual influenza vaccination is due to concerns about side effects, an issue of confidence. Concerns about vaccine safety extend beyond childhood vaccinations as is the need to address these concerns. While it is unclear why this trend is increasing, it suggests more work can be done to better understand beneficiaries’ concerns about influenza vaccination, understand how these concerns may differ from concerns about vaccine safety for childhood vaccinations and other vaccines, and to address these concerns beyond communicating facts about the safety, efficacy, and impact of the influenza vaccine. Moreover, influenza vaccine is unique. Unlike other adult vaccines, influenza vaccination is recommended every year, and the effectiveness of the influenza vaccine varies each year depending on how well matched the vaccine is to the circulating influenza strains of the current season. The varying beneficiary responses to influenza and pneumococcal vaccines reinforce the notion that individual perceptions are often vaccine-specific. More research can be done to understand the impact of various behavior change and health communication interventions among different sub-groups to better understand what motivates behavior, particularly in this population of older adults who often have multiple chronic conditions and waning immune systems.
This study has a number of limitations. One limitation is recall bias as the study relies on self-reporting on behalf of the beneficiaries. This may have over- or under-estimated the high proportion of respondents who cited “did not know it was needed.” Additionally, responses were restricted only to community respondents as facility beneficiaries were not surveyed about reasons for not receiving influenza or pneumococcal vaccines.
Conclusion
This paper explored reasons for being unvaccinated and differences among vaccinated and unvaccinated Medicare beneficiaries in an effort to better understand where to address gaps in vaccination coverage. Given that these vaccines are covered as a Medicare benefit at no cost-sharing to the beneficiary, a better appreciation of barriers to vaccination can be insightful to developing and implementing strategies to raise vaccination coverage levels (e.g., enhance access and convenience through home visits; increase community demand through family incentive rewards and reminder recalls, support provider- and system-based interventions such as standing orders, provider reminders and provider assessment and feedback). Future research can address the effectiveness of beneficiary interventions such as education and outreach on vaccine and vaccination perceptions and the strength and effectiveness of the framing of provider recommendations and referrals.
How providers frame recommendations to patients matter as behavior is greatly influenced by context. Presumptive and effective recommendations can maximize intentions to vaccinate. Unlike with pediatric providers (e.g., pediatricians, family practice providers) where vaccinations are the norm and a central service for pediatric patients, adult providers (e.g., internists and specialists) have multiple competing priorities with adult patients and vaccinations are not often the center of an adult visit. Because many beneficiaries cite the lack of knowledge and provider recommendation for vaccinations, adult providers can increase awareness of the ACIP-recommended schedule of vaccines – which extend across the lifespan – to patients and stress the importance of getting vaccinated with all ACIP recommended vaccines. Providers can also counsel beneficiaries about the benefits of vaccination and address safety concerns. The granularity of beneficiary characteristics provided in this study provides a context to better target and tailor messages and strategies to support patient decision-making and provider engagement. Influenza and pneumococcal disease pose significant risk to older adults and those with chronic conditions, often triggering significant decline in health, disability and death.Citation5–Citation7,Citation20–Citation22 With vaccines widely available across multiple points in the health care delivery system (e.g., doctor’s office, pharmacy, community health clinic) and with no cost-sharing to Medicare beneficiaries, providers must do more to protect the health of older adults and support healthy aging.
Disclosure of potential conflicts of interest
The authors have no conflicts of interest or financial disclosures to declare.
Disclaimer
The opinions expressed in this manuscript are those of the authors and not intended to represent the opinions of the National Vaccine Program Office or the Centers for Medicare & Medicaid Services.
References
- Barney LE. Surgeon general’s advisory committee on influenza research influenza immunization. Public Health Rep. 1960;75:944.
- Recommendations of the immunization practices advisory committee (ACIP) update: pneumococcal polysaccharide vaccine usage – United States. Centers for Disease Control and Prevention, MMWR. 1984;33:273–6,281 [accessed 2018 July 13]. https://www.cdc.gov/mmwr/preview/mmwrhtml/00031107.htm.
- Tomczyk S, Bennett NM, Stoecker C, Gierke R, Moore MR, Whitney CG, Hadler S, Pilishvili T. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: recommendations of the advisory committee on immunization practices (ACIP). MMWR Morb Mortal Wkly Rep. 2014;63:822–25.
- Centers for Disease Control and Prevention. Recommended immunization schedule for adults aged 19 years or older, United States 2018; 2018 [accessed 2018 July 13]. https://www.cdc.gov/vaccines/schedules/hcp/adult.html.
- Centers for Disease Control and Prevention. Estimated influenza illnesses, medical visits, hospitalizations, and deaths averted by vaccination in the United States; 2017 [accessed 2017 Oct 30]. https://www.cdc.gov/flu/about/disease/2015-16.htm.
- Centers for Disease Control and Prevention. Adults: protect yourself with pneumococcal vaccines; 2017 [accessed 2018 July 13]. https://www.cdc.gov/features/adult-pneumococcal/index.html.
- Centers for Disease Control and Prevention. What you should know and do this Flu season if you are 65 years and older; 2018 [accessed 2018 July 13]. https://www.cdc.gov/flu/about/disease/65over.htm.
- Williams WW, Lu P, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE. Surveillance of vaccination coverage among adult populations — United States, 2015. MMWR Surveill Summ. 2017;66(SS–11):1–28. doi:10.15585/mmwr.ss6611a1.
- Office of Disease Prevention and Health Promotion. Immunization and infectious diseases; 2018 [accessed 2018 Aug 20]. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/national-snapshot.
- Office of Disease Prevention and Health Promotion. Immunization and infectious diseases. IID-12.8; 2018 [accessed 2018 Oct 26]. https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4667.
- Office of Disease Prevention and Health Promotion. Immunization and infectious diseases. IID-13.1; 2018 [accessed 2018 Oct 26]. https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4670.
- Gellin BG, Shen AK, Fish R, Zettle MA, Uscher-Pines L, Ringel JS. The national adult immunization plan. Am J Prev Med. 2016;51:1079–83. doi:10.1016/j.amepre.2016.04.014.
- A pathway to leadership for adult immunization: recommendations of the national vaccine advisory committee: approved by the national vaccine advisory committee on June 14, 2011. Public Health Rep. 2012;127(Suppl 1):1–42. doi:10.1177/00333549121270S101.
- National Vaccine Advisory Committee. Recommendations from the national vaccine advisory committee: standards for adult immunization practice. Public Health Rep. 2014;129:115–23. doi:10.1177/003335491412900203.
- MacDonald NE. The SAGE working group on vaccine hesitancy. vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. doi:10.1016/j.vaccine.2015.04.036.
- The Henry J. Kaiser Family Foundation. A primer on Medicare: key facts about the Medicare program and the people it covers. [accessed 2018 July 13]. https://www.kff.org/report-section/a-primer-on-medicare-what-are-the-characteristics-of-people-with-medicare/.
- Opel D, Mangoine-Smith R, Robinson JD, Heritage J, DeVere V, Salas HS, Zhou C, Taylor JA. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am J Public Health. 2015;105:1998–2004. doi:10.2105/AJPH.2014.302425.
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012;12:154. Published 2012 Sep 21. doi:10.1186/1471-2431-12-154.
- Shen AK, Warnock R, Kelman JA. Driving immunization through the medicare annual wellness visit: a growing opportunity. Vaccine. 2017;35:6938–40. doi:10.1016/j.vaccine.2017.10.055.
- Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infectious and cardiovascular disease mortality. JAMA Cardiol. 2016;1:274–81. doi:10.1001/jamacardio.2016.0433.
- Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infaction and influenza: a meta-analysis of case-control studies. Heart. 2015;101:1738–47. doi:10.1136/heartjnl-2015-307691.
- Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–53. doi:10.1056/NEJMoa1702090.