ABSTRACT
In recent years, an increase in vaccine hesitancy has led to a decrease in vaccination coverage in several countries. We conducted a systematic review of studies that assessed knowledge of and attitudes toward pediatric vaccinations, and the vaccination choices and their determinants among pregnant women. A total of 6,277 records were retrieved, and 16 full texts were included in the narrative synthesis. The published literature on the topic shows that, overall, pregnant women believe that vaccines are important for the protection of their children and the community, but various concerns and misunderstandings persist around vaccine safety and efficacy, which reduce the trust of expectant mothers in immunization. Nevertheless, such attitudes and choices vary depending on the vaccine being considered and the corresponding determinants should therefore be studied in the context of each specific vaccination. Further research on this topic is needed, particularly in non-western countries.
Background
Although immunization can be considered one of the greatest achievements in public health, due to its capacity to reduce disease, disability, death and inequity worldwide,Citation1 there has been a marked recent decrease in confidence in vaccination, particularly in industrialized countries.Citation2 Concerns about vaccine safety have led to an increasing number of people seeking alternative vaccination programsCitation3,Citation4 or deciding to postpone or even refuse vaccination,Citation5 with a consequent impact on the maintenance of herd immunity and the spread of infectious diseases.Citation2,Citation6-Citation8 One of the most direct consequences of the decrease in vaccination uptake is the upsurge in measles outbreaks that is currently prevalent in several European countries, such as ItalyCitation9-Citation11 and Romania.Citation9,Citation12 In the USA, over 1,200 individual cases of measles have been confirmed so far in 2019 (to August), accounting for the greatest number of cases reported there since 1992 and since measles was declared eliminated in 2000.Citation13
To better understand the factors underlying the decision to decline current vaccination schedules, the World Health Organization (WHO) established in 2012, within its Strategic Advisory Group of Experts (SAGE) on Immunization, a specific working group (WG) on “Vaccine Hesitancy”,Citation14 which was defined as: “[a] delay in acceptance or refusal of vaccines despite availability of vaccine services”. Vaccine hesitancy has been addressed as “complex and context specific, varying across time, place and vaccines, influenced by factors such as complacency, convenience, and confidence”.Citation8 This definition – known as the “3Cs” model of hesitancy – encompasses the three main drivers of vaccine acceptance or refusal: complacency and convenience relate to the perceived risk of disease and the ease with which vaccine services can be reached (respectively), while vaccine confidence is defined as trust in the effectiveness and safety of vaccines and trust in the healthcare system that delivers them.Citation8
Several studies have been conducted to assess the extent and determinants of hesitancy among different populations and some of the available evidence has been synthesized in systematic reviews.Citation15-Citation19 The only published review of studies addressing hesitancy among expectant mothers has focused on the acceptance of recommended vaccines during pregnancy.Citation20 However, pregnant women have been recognized as an ideal target population in which to develop interventions for the promotion of pediatric vaccinations, considering that the antenatal period is the time when attitudes and beliefs about childhood vaccines first take shapeCitation21 and that pregnancy represents a strategic ‘‘teachable moment” for health promotion and behavior change.Citation22-Citation24 We therefore conducted a systematic review to assess the factors affecting the vaccination choices of pregnant women, searching for evidence on knowledge, attitudes and childhood immunization choices and their determinants, with the aim of supporting the development of interventions and promoting further research in this area.
Methods
This review was conducted according to the Cochrane Handbook for systematic reviews of interventions.Citation25
Inclusion criteria
We included primary studies of any type (qualitative or quantitative, experimental or observational, cross-sectional or longitudinal) that reported on knowledge of vaccine efficacy and safety, and/or attitudes toward pediatric vaccinations among pregnant women and/or the intention to vaccinate their children and/or vaccination uptake after birth. Studies were also included if they did not aim to assess the association between knowledge, attitudes and vaccination choices, but provided descriptive data on at least one of these items. Cohort studies and experimental studies were included if they provided baseline data on one of the outcomes of interest (knowledge of vaccine efficacy and safety, attitudes, intention to vaccinate). If studies were addressed at parents as the target population, they were included only if pregnant women were also included in the sample and if data on this population could be extracted from the published article or its supplementary material. RCTs aimed at assessing the impact of an educational intervention were excluded if they did not provide detailed information on knowledge of vaccine efficacy and safety or attitudes prior to the intervention; in case of inclusion, only baseline data were extracted for the purpose of the review. Similarly, in case of studies with a longitudinal design, only baseline data collected during pregnancy were extracted. We excluded articles that were not in English.
Search strategy
The literature search was performed on the databases Medline, Scopus, and Web of Science in May 2019 and updated in August 2019. Two investigators conducted the literature search independently, to enhance sensitivity. The search terms used were: “(Immuniz* OR immunis* OR vaccin*) AND pregnan* AND (knowledge OR attitude OR trust OR mistrust OR perception OR hesitan* OR accept* OR concern* OR confidence)”. The strings were adjusted for each database while maintaining a common overall architecture. The search strategy for Medline included both MeSH terms and free texts of the primary search terms. The reference lists of retrieved articles were also searched to identify potentially relevant studies.
Selection of studies
Studies were selected according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) StatementCitation26 after identifying relevant articles through searches of electronic databases; duplicates were removed, and titles and abstracts of the returned citations were screened. Studies that clearly did not meet the inclusion criteria were excluded. Full texts of potentially relevant articles were retrieved and independently examined by two reviewers to determine eligibility. Disagreements were resolved through discussion, and the reasons for exclusion were recorded.
Data extraction and quality assessment
Data were extracted by two reviewers independently. Data extraction focused on details of the study population, tools used for the assessment and main outcomes assessed (knowledge and/or attitudes and/or vaccination choices). Additional information, such as authors, journal, year of publication, was also extracted. No data were recorded if they were collected after an intervention or after birth, except for data on vaccination uptake in children whose mothers’ knowledge of or attitudes toward vaccination had been assessed during pregnancy.
Quality was assessed using two tools: the Newcastle-Ottawa Scale (NOS) adapted for cross-sectional studiesCitation27 and the CASP (Critical Appraisal Skills Programme) Checklist for qualitative studies.Citation28 The NOS checklist was also used for RTCs and longitudinal studies, taking only baseline characteristics into account. Two reviewers assessed the quality of studies using both checklists independently. Disagreement was resolved by discussion, resulting in a consensus on the quality of each study.
Data synthesis
A narrative synthesis of the studies included after eligibility checks was performed to summarize their key features and to compare study questions, interventions, methods, and results.
Results
Characteristics of the included articles
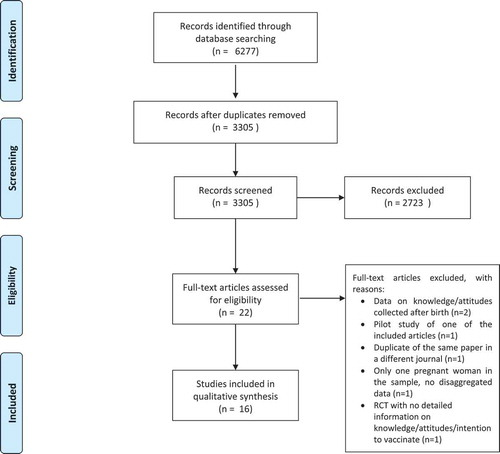
We retrieved a total of 6,277 studies. After removal of duplicates and screening of titles and abstracts, 22 full texts remained, of which 16 were included in the narrative synthesisCitation29-Citation44 (see ). The main features of the included studies are summarized in . All but one were quantitative studies,Citation30 and three had an experimental design: we included two randomized controlled trials (RCTs) that assessed the effectiveness of interventions at improving parental knowledge of and attitudes toward vaccination, with baseline data collected during pregnancy,Citation33,Citation40 and a pilot study that evaluated the impact of an education course on the attitudes of pregnant women toward childhood immunization.Citation44 We also included a cohort study aimed at exploring changes in attitudes toward vaccination over time, during pregnancy and 3, 6 and 14 months after childbirth.Citation43 Two studies focused on two specific vaccines, one against HPVCitation30 and one against rotavirus,Citation31 while all the others assessed childhood vaccinations in general. All studies were conducted in western nations, with the exception of one conducted in JapanCitation32 and one in Malaysia.Citation36
Table 1. Papers assessing the knowledge of and attitudes toward pediatric vaccinations and vaccination choices of pregnant women.
Figure 1. PRISMA Flow diagram. Legend: Number of studies identified by search strategy, number of studies excluded and included during primary and secondary (full -text) screening, and final number of studies included”.
Most quantitative studies made use of an ad hoc questionnaire specifically developed for the purpose of the research project, although three of themCitation36,Citation37,Citation40 used a version of the questionnaire developed by Opel et al. for the Parent Attitudes and Childhood Vaccines (PACV) survey,Citation45,Citation46 which was adapted for pregnant women. The original PACV survey was self-administered and contained 15 items in three domains (behavior, safety and efficacy, and general attitudes), and in the three studies cited it was slightly modified to include specific items relating to expectant mothers. All three studies used a cutoff value of 50 in the PACV score (range 0 to 100), defining a score >50 as hesitant. Of the other studies, only three had validated their questionnaire with a pilot study prior to its use.Citation31,Citation32,Citation43
Most quantitative studies were of moderate quality (see ), but two were rated low quality.Citation32,Citation44 The qualitative study by Dubé et al.Citation34 fulfilled the criteria of validity, relevance and quality of the results presented.
Table 2. Critical appraisal of the quality of evidence based on the Newcastle-Ottawa Scale (NOS) adapted for cross-sectional studies*.
Knowledge of vaccine safety and efficacy and its determinants
Seven studiesCitation30-Citation33,Citation41,Citation43,Citation44 aimed to assess how much pregnant women know about pediatric vaccinations. Weiner et al.,Citation33 Betsch et al.Citation41 and Rosso et al.Citation43 assessed their respondents’ agreement with common vaccination-related messages and misconceptions, including items on vaccine efficacy and safety. The tools used and the number of items assessed differed across studies (12, 9 and 8 items respectively). Weiner et al.Citation31 found that knowledge of vaccines was generally high, with percentages of agreement over 73% for most items, with two exceptions: about one third (36%) of expectant mothers did not agree that “A baby’s immune system can handle several vaccines at one doctor’s visit”, and about a quarter (23.5%) did not agree that “Scientific studies and reviews show no relationship between vaccines and autism”. Conversely, Rosso et al.Citation43 found that knowledge of vaccine safety and efficacy in their sample of pregnant women was quite low: on average, women correctly responded to approximately half of the questions, with 5.5% not responding correctly to any of the statements included in the questionnaire. The authors pointed out that there was a high level of uncertainty about the proposed statements on vaccine safety and efficacy, with rates of “I don’t know” responses ranging from 20.3% to 57.7%.Citation43 High rates of uncertainty about common vaccine-related messages were found by Bechini et al.,Citation44 although they defined those items as “Attitudes of women towards the most frequent fake news about vaccinations”. Rosso et al. also investigated factors associated with higher levels of knowledge,Citation43 finding that being older, having a university degree, perceiving the quality of the NHS as good or excellent, and having received information on vaccinations from institutional websites or through education were all associated with a greater degree of knowledge. On the other hand, factors associated with a lower level of knowledge were choosing populist movements as political orientation, use of alternative medicine and having received information on vaccines by ‘‘word of mouth”.Citation43 Saitoh et al. reported low levels of knowledge in their sample: they assessed basic knowledge about vaccination and self-reported knowledge of the individual’s understanding of childhood vaccination, the first returning a score of 6.7 ± 2.9/13 and the second of 4.0 ± 3.9/12 in the pre-intervention, and of 5.6 ± 3.2/13 and 3.6 ± 3.0/12, respectively, in the control group.Citation32
Betsch et al. assessed how the sources of information on vaccination affected the knowledge of expectant mothers over time; they found that higher knowledge scores were associated with the use of physicians and television as sources of information, while midwives and books were associated with lower levels of knowledge.Citation41 The analysis revealed a significant effect of a medium level of education, consistent with the findings of Rosso et al.: women with a maximum of 10 years of school were less knowledgeable about vaccination than more highly educated women.Citation43
Morin et al. assessed specific knowledge of gastroenteritis (GE) and rotavirus infection and vaccination.Citation31 Most mothers were confident about their knowledge of GE, and correct response rates to questions on the causes of GE, and its transmission and prevention, were generally high. However, only 29% of the sample had already heard about rotavirus vaccination. Heyman et al. assessed familiarity with HPV infection and vaccination in their sample of pregnant women, finding prior knowledge in 79% and 72.3%, respectively, of the sample.Citation30
Five studies assessed the perceived level of knowledge of childhood vaccinations in their samples of pregnant women,Citation33,Citation34,Citation42-Citation44 showing that in most cases future mothers were not satisfied with their familiarity with the topic: the highest rate of positive perception of their knowledge was found by Danchin et al.,Citation42 where 50% of mothers strongly agreed that they had enough knowledge to make a decision about vaccinating their child. In the study by Weiner et al.,Citation33 42% of women reported being dissatisfied with their current knowledge level. Rosso et al.Citation43 found that only 30% of respondents rated their level of knowledge of vaccinations at least adequate, and in Bechini et al. 41% of women indicated a low level of knowledge.Citation44 In the qualitative study by Dubé et al.,Citation34 most vaccine-hesitant mothers said that they lacked sufficient knowledge to make “the right decision”.
Sources of information
The source of information on pediatric vaccination was investigated in eight studies.Citation30,Citation31,Citation33,Citation36,Citation38,Citation42-Citation44 Only Danchin et al.Citation42 reported healthcare professionals (mainly midwives and GPs) as the most highly accessed resource, while in all other studies the internetCitation32,Citation36,Citation42 or mediaCitation30,Citation31,Citation40,Citation41 were the most frequently used. Word of mouth was reported as one of the most common sources of information in all Italian studies,Citation38,Citation43,Citation44 as well as by Danchin et al.Citation42; the Italian studies also reported frequent use of non-institutional websites by pregnant women.Citation38,Citation43,Citation44 Studies reporting on the satisfaction of the information provided by healthcare professionals provided inconsistent results: Weiner et al. reported that only 15.5% of the 73 expectant mothers who had received information from their obstetricianecologistor midwife were very satisfied with the information,Citation33 while in Rosso et al.Citation43 and Bechini et al.Citation44 the information provided by healthcare professionals (including also GPs and pediatricians) was rated as at least adequate in 78.9% and 71% of cases, respectively. High levels of satisfaction and trust in healthcare providers were also reported by Danchin et al. (93–95%).Citation42
Attitudes
Thirteen studies described the attitudes of expectant women toward childhood vaccination.Citation29,Citation30,Citation32-Citation34,Citation36-Citation44 Three studies specifically assessed levels of vaccine hesitancy among expectant mothers through an adapted version of the PAVC questionnaire.Citation36,Citation39,Citation40 In the study conducted by Mohd Azizi et al., 25.5% of pregnant women were noted as vaccine-hesitant, compared to the overall rate of 11.6% for the whole sample, which also included parents.Citation36 In Daley et al., 14.1% were classified as vaccine-hesitant at baseline,Citation39 while Cunningham et al. found lower rates, with 8% of respondents classified as vaccine-hesitant.Citation38 In a multivariate analysis, Mohd Azizi et al. found that pregnant mothers expecting their first child were four times more likely to be vaccine-hesitant than those who already had one or more children.Citation37 Factors associated with vaccine hesitancy in the study by Cunningham et al. included holding a college level of education or less, compared with holding more than a four-year degree and not receiving an annual influenza vaccine.Citation38
The importance of vaccination in protecting individuals and the community against infectious diseases was acknowledged by most pregnant women included in those studies that assessed this issue.Citation29,Citation32-Citation35,Citation41-Citation44 The three Italian studies also explored the attitudes of mothers toward the introduction of compulsory vaccination: both Gualano et al.Citation38 and Bechini et al.Citation44 found that the majority of women interviewed were in favor of compulsory vaccination, with rates of 81.6% and 60%, respectively. In the study by Rosso et al.,Citation43 only 17.8% of respondents agreed that compulsory vaccination is against the right of citizens to make choices about their care.
Some studiesCitation42,Citation43 reported that not all vaccines against infectious diseases are perceived as equally important: despite the high overall level of support for childhood vaccines recorded in the survey of Danchin et al., these authors also found that 27% of respondents thought that vaccines are given to children to prevent diseases that are not common.Citation42 Rosso et al. specifically investigated the perceived benefit of vaccinating to protect against individual infectious diseases, finding high rates of uncertainty about the benefit of vaccination against diphtheria (41.8%), mumps (38.2%) and pertussis (33.4%), while recording high rates of negative opinion of the utility of influenza and varicella immunization (64.1% and 33.2 of respondents, respectively).Citation43
The most frequently stated reason against the acceptance of vaccination in the studies included were the (potential) side effects of the immunizations.Citation29,Citation30,Citation33,Citation36,Citation43,Citation44 In this regard, several studies reported that vaccinations are still seen as a possible cause of autism.Citation30,Citation42-Citation44 Another frequently reported concern was the idea that children are getting too many injections at the same time or too many vaccines during their first years of life.Citation33,Citation36,Citation42-Citation44 Indeed, some women thought that developing immunity by getting infections is preferable to being immunized through vaccinations.Citation29,Citation34,Citation36,Citation44
Other factors that hamper acceptance of pediatric immunization among pregnant women are the frequently reported negative attitudes toward pharmaceutical companies, seen as having an economic interest in promoting vaccination,Citation34,Citation38,Citation43,Citation44 and a lack of trust in the information provided on vaccination by public authorities and/or healthcare providers.Citation34,Citation38,Citation43 In their qualitative study, Dubé et al. found that many vaccine-hesitant mothers were looking for information on vaccination from different sources and many criticized the lack of “balance” or “neutral” information on vaccination.Citation34 Gualano et al.Citation38 and Rosso et al.Citation43 found that 35.5% and 45.6% of women, respectively, think that healthcare professionals do not provide complete information on vaccinations, mainly on their side effects.
Corben et al.Citation39 and Danchin et al.Citation42 found that pregnant women who already had other children were less concerned about the risks associated with vaccination and were less hesitant to vaccinate their children than primiparae, while Heyman et al. found an association between acceptance of HPV vaccination and educational level, with most women who accepted this vaccine holding a professional degree.Citation30
Both Rosso et al.Citation43 and Corben et al.Citation39 found an association between trust in the health system and a positive attitude toward vaccination. Corben et al. found that respondents who strongly supported childhood vaccination and were “not at all hesitant” toward vaccination showed higher levels of trust in their child’s doctor.Citation39 In a multivariate analysis, Rosso et al. found a significant association between positive attitudes and a good perception of the quality of the Country’s healthcare system.Citation43 Their study also found positive attitudes to be associated with high levels of knowledge of the safety and efficacy of vaccines, while having had indirect experience of the side effects of vaccination and having received information about vaccination through the media (TV, radio, newspapers, etc.) were not likely to result in a positive attitude.Citation43
Of all the attitudinal dimensions assessed in their study, both at baseline and in the control group, Saitoh et al. found higher scores relating to perceived severity and social norms (influencing the decision to vaccinate). Average scores for the perceived benefits of vaccination were slightly higher than those for the perceived barriers to vaccination.Citation32
Dubé et al. also found an association between the type of health professional who delivered information on vaccines and attitudes toward immunization. In their qualitative study, all but one of the unfavorable mothers were under the care of a midwife.Citation34
Finally, Betsch et al. assessed changes in attitudes during the period from pregnancy to 3, 6 and 14 months after childbirth, finding that, during all follow-up interviews, the women had higher risk perceptions and worried more about vaccine-preventable diseases than about potentially adverse events associated with vaccination.Citation41
Intention to vaccinate/vaccination uptake and its determinants
Eleven studies assessed their sample’s intention to vaccinateCitation29-Citation35,Citation37,Citation40,Citation43,Citation44 and four assessed vaccination uptake after birth, either based on official registriesCitation35,Citation40,Citation41 or on the responses to follow-up interviews.Citation41
In Wroe et al., 67% of participants stated they would immunize their child, while only 5% stated they definitely would not. There was a strong association between an individual’s antenatal ratings of likelihood to immunize and their actual immunization decision (0.87).Citation29 Seventy-five percent of expectant mothers included in the study by Weiner et al. planned to have their child receive all the vaccinations recommended, approximately 15% planned to personalize their vaccination schedule, delaying or not receiving some of the recommended vaccines, while 4% had not yet decided.Citation33 Saitoh et al. found higher rates of women intending only to accept specific vaccines (50.0%) rather than all vaccines (33.3%) in their control group, while the proportion of women intending full immunization was higher in the pre-intervention group (53%% versus 26.5% of women intending to accept only some vaccines). Both groups had high rates of non-respondents.Citation32 Timely immunization was intended by 81% of women in the study by Grant et al., and this actually occurred in 70% of the infants surveyed.Citation35 In the study by Corben et al., 92.2% of women wanted their new baby to receive all the recommended vaccinations, 83.2% of infants were fully vaccinated within 30 days of the recommended date for each vaccine, and a further 12.1% were immunized after a minor delay (< 10% of follow-up days). There was a significant association between intention and actual immunization, with infants of pregnant women who decided upon full immunization more likely to be immunized on time (OR = 7.65, 95% CI: 4.87 − 12.18).Citation39 Danchin et al. found “unquestioning acceptors” and “cautious acceptors” (defined as people willing to accept all vaccines with no concerns or just minor concerns) accounting for 64.2% and 29.1% of the sample respectively, while refusers of all vaccine were only 1.2%. In their study, immunization was taken up in 89% of children with available records.Citation42 In their qualitative study, Dubé et al. found that 35 women out of 54 accepted all vaccinations, while 12 selected only some of them or chose to delay immunization.Citation34 Betsch et al. found that 14 months after birth, on average, children had received 79% of the recommended vaccines.Citation42 In Gualano et al., 98.1% of the sample intended to vaccinate their children.Citation38
Rosso et al. and Bechini et al. assessed the intention of pregnant women to vaccinate against specific infectious diseases: in Rosso et al., an intention to vaccinate with the hexavalent vaccine was expressed by the highest proportion of respondents (76.8%), followed by the anti-MMR vaccine (64.3%),Citation43 while Bechini et al. found the highest intention rates for tetanus (78%), meningitis B and C (74 and 77%, respectively), pertussis and measles (both 70%).Citation44 At the other end of the scale, high rates of respondents (26.5% and 11.3% of women, respectively) indicated that they did not intend to vaccinate their children with the anti-varicella and the anti-HPV vaccines in Rosso et al.,Citation43 with 7% of pregnant women giving the same indication for both varicella and rotavirus vaccines in Bechini et al.Citation44 Rosso et al. found high levels of uncertainty about the anti-rotavirus (66.2%) and anti-pneumococcal vaccines (55.4%).Citation43 In the study by Heyman et al., intention to vaccinate against HPV depended on the sex of the fetus, being 27.7% in the case of male and 40.0% for a female,Citation30 while a study on rotavirus vaccine found the intention to vaccinate among respondents who had already heard about this vaccine was 74%.Citation31
Seven studies also conducted an inferential analysis to assess the determinants of vaccination choices. Factors most frequently associated with vaccination uptake across studies were the perceived benefits/value of vaccination for the individual and the communityCitation29,Citation33,Citation43 and confidence in vaccine safety.Citation29,Citation33,Citation39,Citation43 Wroe et al. found two main types of factor to be associated with immunization: perception of risk and benefit of vaccination (immunizers had higher ratings of perceived personal and community benefit of immunization, and lower ratings of perceived risk) and emotional factors (anticipated regret if harm should occur after inaction was the strongest predictor of likelihood to immunize the child, along with feelings of responsibility if harm should occur after inaction and a lower level of regret/feeling of responsibility if harm should occur after action).Citation29 Betsch et al. assessed attitudes toward vaccination both during pregnancy and after birth, together with the impact of these attitudes on vaccine uptake; they found that attitude at 14 months was the only significant predictor of complete vaccine uptake at 14 months. A change in attitudes toward vaccination after birth was found to be associated with changes in concerns about disease.Citation42
Rosso et al. found that higher levels of knowledge were also associated with the intention to vaccinate with particular vaccines (anti-pnemuococcal, anti-meningococcal B and anti-HPV vaccines).Citation43 The source of information on vaccines also showed an association with vaccination intentions and uptake: Rosso et al. found an association between receiving information from a health professional and intention to vaccinate with anti-MMR, anti-meningococcal B and anti-varicella.Citation44 Morin et al. found that having already heard about the rotavirus vaccine in the media was negatively associated with uptake of rotavirus vaccination.Citation31 In the qualitative study by Dubé et al., some differences were observed in decision-making on vaccination among vaccine-hesitant mothers under the care of physicians versus midwives, with midwives strengthening the intention of vaccine-hesitant mothers to delay vaccination.Citation34
Results on the association between parity and acceptance of vaccination were inconsistent across studies: while some found that first-time mothers were more negative about vaccinating their children (particularly for some specific vaccines, as recorded by Mohd Azizi et al. for the rotavirus vaccine,Citation36 and by Rosso et al. for the anti-pneumococcal and anti-meningococcal C vaccines,Citation43 others found that primiparae were more likely to intend to vaccinate.Citation31,Citation35 Dubé et al. found that vaccine-hesitant primipara mothers were more likely to accept all vaccines than vaccine-hesitant multipara mothers.Citation30
Both Corben et al.Citation39 and Danchin et al.Citation42 also assessed maternal immunization (influenza and pertussis vaccines) during pregnancy as a possible determinant of childhood vaccination choices, finding no association with children’s vaccination uptake”.
Socio-demographic factors were not associated with the intention to vaccinate in most studies, with some exceptions. Both Grant et al. and Rosso et al. found an association between lower educational levels and intention to vaccinate (in Rosso et al., this was statistically significant for the anti-rotavirus vaccine).Citation35,Citation43 Grant et al. also found an association between ethnicity and intention to vaccinate, with women of Pacific or Asian ethnicity being more likely to accept vaccinations.Citation35
Discussion
This systematic review provides a synthesis of the available evidence on the knowledge of and attitudes toward pediatric vaccination, the sources of information most frequently consulted, the frequency of vaccine hesitancy and/or denial, and factors influencing vaccination choices in pregnant women.
Our literature search showed that pregnant women have recently been recognized as a key population in which to study vaccine hesitancy: eight out of the 15 studies included in this review were published in 2018 and 2019. As expected, most of the available data on this topic were produced by research groups based in western countries, where hesitancy has increased the most, leading to a decrease in vaccination uptake. However, little evidence has been produced so far at the European level: one study was conducted in Germany and three in Italy. More evidence may also be needed from other European countries, especially from those facing challenges in maintaining high immunization rates.
All studies found that most women are positive about the importance of vaccination in protecting individuals and the community against infectious disease. This is also reflected in the high rate of women reporting their intention to vaccinate their children, from a 50.0% intention for specific vaccines found by Satoh et al.Citation32 to 92.2% reported for childhood vaccination in general reported by Corben et al.Citation39 However, the studies we surveyed also found high rates of women expressing concerns about the safety of vaccines and expressing a lack of trust in the quality and impartiality of information provided by healthcare professionals. The percentages of hesitant women, when specifically assessed through the PACV questionnaire, ranged from 8% reported by Cunningham et al.Citation37 to 25.5% by Mohd Azizi et al.Citation36 Rates of women declining to vaccinate their children with all vaccines ranged from 1.2% in Danchin et al.Citation42 to 5% in Wroe et al.Citation29 We found that attitudes relating to the importance of vaccines and the intention to vaccinate may depend on the infectious disease in question,Citation36,Citation43,Citation44 suggesting that the categorization of women as “for” or “against” vaccination as a whole may not always be appropriate, and that vaccine-specific factors, peculiar to each vaccination, need to be considered among the determinants of acceptance.Citation34,Citation43 This was also suggested by the WHO SAGE WG, which grouped the factors influencing the decision to accept, delay or reject some or all vaccines into three categories: contextual, individual and group, and vaccine/vaccination-specific influences.Citation15
The inferential analyses conducted in some of the studies confirmed that acceptance of pediatric vaccination in this specific population appears to be mainly driven by issues of complacency (perceived benefits of vaccinations) and confidence (trust in the efficacy and safety of vaccines and in the healthcare system). As previously suggested,Citation43 an effort should be made to improve the availability of data on the safety and efficacy of vaccines, including by non-industry sponsored and unbiased sources,Citation47,Citation48 and to strengthen reporting and pharmacovigilance systems.Citation49 Convenience has not found to be a determinant of the intention to vaccinate nor of vaccination uptake in any of the studies. Similarly, socio-demographic factors, such as education or income, do not seem to play a role in influencing hesitancy or decline of vaccinations in western countries. These data suggest that vaccine hesitancy is a widespread phenomenon in different population strata, and that there might be a need to target messages according to different educational and literacy levels. In several studies,Citation34,Citation36,Citation40 first-time mothers showed higher levels of hesitancy and concerns about vaccination than women who already had children, suggesting they should be a priority target for interventions aimed at increasing confidence in immunization practices. In fact, the first pregnancy represents a particularly propitious moment, since attitudes and beliefs about vaccinations are often not yet fully structured.Citation9
Only a few studies assessed how much expectant mothers know about vaccination, producing inconsistent results.Citation33,Citation44 However, all studies surveyed suggest that misinformation about the risks associated with vaccines, including the risk of developing autism and other serious side effects, is still widespread. Knowledge and awareness issues are among the most frequently cited reasons for vaccine hesitancy globally and it has been suggested that addressing the gaps in knowledge may help decrease vaccine hesitancy.Citation50 In this regard, when developing interventions aimed at increasing vaccine acceptance, an assessment of the most common knowledge gaps and misbeliefs in the target population may be useful for tailoring educational messages.
Healthcare professionals were shown to play a secondary role in informing pregnant women about the risks and benefits of immunization in nearly all studies, where the media and internet (also including non-institutional websites) were reported as the main sources of information on vaccines. This finding suggests both the need to strengthen the role of healthcare professionals in discussions around vaccine safety and efficacy and in promoting the positive involvement of various media, while carefully monitoring the content of the information provided.Citation51 Among healthcare professionals, midwives would be ideally placed to support expectant mothers in making informed decisions about maternal and infant vaccination. However, some of the included studies also reported pediatricians and GPs as a source of information on vaccinations in this populationCitation42-Citation44; the importance of these professionals will become more relevant after childbirth, with the transition from maternity to health and child services, in a time where decisions about vaccinations take their final shape. However, the available evidence suggests that while most healthcare professionals are favorable to vaccinations in general, there are a wide range of beliefs and concerns in this group, including doubts regarding the safety and usefulness of vaccines and mistrust especially of pharmaceutical companies.Citation19,Citation52-Citation55 Some studies also reported the feeling of not being sufficiently informed to address parental concerns.Citation19,Citation52 Specific training strategies would be needed to provide different healthcare providers with the ability to deliver effective communication regarding vaccines safety and efficacy to parents, but also with the aim of counteracting hesitant behavior within health workers themselves.Citation53
This systematic review has some limitations. The first is strictly linked with the nature of vaccine hesitancy itself, which, as clearly defined by the SAGE WG, is a context-specific phenomenonCitation15: the results obtained by the studies in this survey may therefore not be generalizable to the whole population of pregnant women. More research would be needed, mainly in non-western, middle and low income countries, where different cultural and social factors may play a role in the acceptance of vaccination.Citation2,Citation56,Citation57 Generalizability is also limited by the fact that different tools were used across studies to assess hesitancy, knowledge and attitudes, few of which were validated prior to their useCitation45,Citation46,Citation58: the same concepts may therefore have been measured by different items, making the results not fully comparable across studies and consequently not allowing the combination results in a quantitative synthesis. In this regard, Larson et al. have stressed that many vaccine studies assess trust in vaccinations mainly through single-item measures, leaving an implicit definition of trust, indicating that a thorough understanding of trust as it relates to vaccine acceptance is currently under-researched.Citation59
Conclusions
We provide an overview of the available evidence on factors affecting the vaccination choices of pregnant women in different settings, confirming that pregnancy is a time when ideas around pediatric immunization begin to take shape. Therefore, pregnant women represent an ideal target population for which strategies aimed at increasing trust in vaccinations could be developed. These strategies should focus on strengthening the role of healthcare professionals, particularly midwives, in delivering information on vaccines, increasing their capacity to effectively manage vaccine hesitancy in parents, but also counteracting hesitant behaviors within health workers themselves, and on the involvement of different media tools, which continue to represent the main source of information for most women. Interventions should be tailored based on a context-specific analysis of the determinants of vaccine hesitancy and should also take into account specific vaccine-related factors. Further evidence from non-western and low- or middle-income countries may be needed.
Disclosure of potential conflicts of interest
The authors declare no potential conflicts of interest.
Additional information
Funding
References
- Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff TA, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–46. doi:10.2471/blt.07.040089.
- Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi:10.1016/j.ebiom.2016.08.042.
- Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378(9790):526–35. doi:10.1016/S0140-6736(11)60678-8.
- Dempsey AF, Schaffer S, Singer D, Butchart A, Davis M, Freed GL. Alternative vaccination schedule preferences among parents of young children. Pediatrics. 2011;128(5):848–56. doi:10.1542/peds.2011-0400.
- Robison SG, Groom H, Young C. Frequency of alternative immunization schedule use in a metropolitan area. Pediatrics. 2012;130(1):32–38. doi:10.1542/peds.2011-0400.
- Raude J, Fressard L, Gautier A, Pulcini C, Peretti-Watel P, Verger P. Opening the “Vaccine Hesitancy” black box: how trust in institutions affects French GPs’ vaccination practices. Expert Rev Vaccine. 2016;15:937–48. doi:10.1080/14760584.2016.1184092.
- Liu F, Enanoria WTA, Zipprich J, Blumberg S, Harriman K, Ackley SF, Wheaton WD, Allpress JL, Porco TC. The role of vaccination coverage, individual behaviors, and the public health response in the control of measles epidemics: an agent-based simulation for California. BMC Public Health. 2015;15:447. doi:10.1186/s12889-015-1766-6.
- Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016;315:1149–58. doi:10.1001/jama.2016.1353.
- European Centre for Disease Prevention and Control. Measles and Rubella surveillance-2017. Stockholm: ECDC; 2018 [accessed 2019 Nov 11]. https://ecdc.europa.eu/sites/portal/files/documents/Measles-and-Rubella-Surveillance-2017-final_0.pdf>.
- Adamo G, Sturabotti G, De Soccio P, Prencipe GP, Sciarra I, Baccolini V, Massimi A, Marzuillo C, Iannazzo S, Villari P, et al. The elimination of measles and rubella in Italy. Ig Sanita Pubbl. 2017;73:429–42.
- Adamo G, Baccolini V, Marzuillo C, Sturabotti G, Villari P. Slow progress in measles and rubella elimination in Italy. Epidemiol Biostat Public. 2016;13:e120751–52. doi:10.2427/12075.
- Dascalu S. Measles epidemics in Romania: lessons for public health and future policy. Front Public Health. 2019;7:98. doi:10.3389/fpubh.2019.00098.
- Centers for Disease Control and Prevention (CDC). Measles cases and outbreaks. [accessed 2019 Dec 15]. https://www.cdc.gov/measles/cases-outbreaks.html.
- WHO. SAGE working group dealing with vaccine hesitancy (March 2012 to November 2014). World Health Organization; 2015 [accessed 2019 Nov 11]. http://www.who.int/immunization/sage/sage_wg_vLccine_hesitancy_apr12/en/.
- MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dubé E, Gellin B, Goldstein S, Larson H, MacDonald N, Manzo ML, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- Karthigesu SP, Chisholm JS, Coall DA. Do grandparents influence parents’ decision to vaccinate their children? A systematic review. Vaccine. 2018 Nov 26;36(50):7456–62. doi:10.1016/j.vaccine.2018.10.017.
- Bocquier A, Ward J, Raude J, Peretti-Watel P, Verger P. Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines. 2017;16(11):1107–18. doi:10.1080/14760584.2017.1381020.
- Collange F, Verger P, Launay O, Pulcini C. Knowledge, attitudes, beliefs and behaviors of general practitioners/family physicians toward their own vaccination: A systematic review. Hum Vaccin Immunother. 2016;12(5):1282–92. doi:10.1080/21645515.2015.1138024.
- Attwell K, Wiley KE, Waddington C, Leask J, Snelling T. Midwives’ attitudes, beliefs and concerns about childhood vaccination: a review of the global literature. Vaccine. 2018;36(44):6531–39. doi:10.1016/j.vaccine.2018.02.028.
- Wilson RJ, Paterson P, Jarrett C, Larson HJ. Understanding factors influencing vaccination acceptance during pregnancy globally: A literature review. Vaccine. 2015;33(48):6420–29. doi:10.1016/j.vaccine.2015.08.046.
- Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Am J Prev Med. 2015;49:S391–8. doi:10.1016/j.vaccine.2015.09.035.
- Olander EK, Darwin ZJ, Atkinson L, Smith DM, Gardner B. teachable moment’ – a conceptual analysis of women’s perinatal behaviour change. Women Birth. 2016;29:e67–71. doi:10.1016/j.wombi.2015.11.005.
- Atkinson L, Shaw RL, French DP. Is pregnancy a teachable moment for diet and physical activity behaviour change? An interpretative phenomenological analysis of the experiences of women during their first pregnancy. Br J Health Psychol. 2016;21:842–58. doi:10.1111/bjhp.12200.
- Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202:135.e1–8. doi:10.1016/j.ajog.2009.06.008.
- Shemilt I, Mugford M, Byford S, et al. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions, version 5.1.0. The Cochrane Collaboration; 2011 [accessed 2019 Dec 15]. http://www.handbook.cochrane.org.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi:10.1016/j.jclinepi.2009.06.006.
- Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013 Feb 19;13:154. doi:10.1186/1471-2458-13-154.
- Critical Appraisal Skills Programme. CASP qualitative checklist [ online]; 2018 [accessed 2019 Nov 11]. http://www.phru.nhs.uk/Doc_Links/Qualitative%20Appraisal%20Tool.pdf.
- Wroe AL, Turner N, Salkovskis PM. Understanding and predicting parental decisions about early childhood immunizations. Health Psychol. 2004;23(1):33–41. doi:10.1037/0278-6133.23.1.33.
- Heyman KP, Worley MJ Jr, Frey MK, Kessler RT, Bodurka DC, Slomovitz BM. Willingness of pregnant women to vaccinate themselves and their newborns with the HPV vaccine. Vaccine. 2011;29(28):4618–22. doi:10.1016/j.vaccine.2011.04.062.
- Morin A, Lemaître T, Farrands A, Carrier N, Gagneur A. Maternal knowledge, attitudes and beliefs regarding gastroenteritis and rotavirus vaccine before implementing vaccination program: which key messages in light of a new immunization program? Vaccine. 2012;30(41):5921–27. doi:10.1016/j.vaccine.2012.07.050.
- Saitoh A, Nagata S, Saitoh A, Tsukahara Y, Vaida F, Sonobe T, Kamiya H, Naruse T, Murashima S. Perinatal immunization education improves immunization rates and knowledge: a randomized controlled trial. Prev Med. 2013;56(6):398–405. doi:10.1016/j.ypmed.2013.03.003.
- Weiner JL, Fisher AM, Nowak GJ, Basket MM, Gellin BG. Childhood immunizations: first-time expectant mothers’ knowledge, beliefs, intentions, and behaviors. Vaccine. 2015;33(Suppl 4):D92–98. doi:10.1016/j.vaccine.2015.09.037.
- Dubé E, Vivion M, Sauvageau C, Gagneur A, Gagnon R, Guay M. “Nature does things well, why should we interfere?”: vaccine hesitancy among mothers. Qual Health Res. 2016;26(3):411–25. doi:10.1177/1049732315573207.
- Grant CC, Chen MH, Bandara DK, Marks EJ, Gilchrist CA, Lewycka S, Carr PE, Robinson EM, Pryor JE, Camargo CA, Morton SM. Antenatal immunisation intentions of expectant parents: relationship to immunisation timeliness during infancy. Vaccine. 2016;34(11):1379–88. doi:10.1016/j.vaccine.2016.01.048.
- Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. doi:10.1016/j.vaccine.2017.04.010.
- Cunningham RM, Minard CG, Guffey D, Swaim LS, Opel DJ, Boom JA. Prevalence of vaccine hesitancy among expectant mothers in Houston, Texas. Acad Pediatr. 2017:1–7. doi:10.1016/j.acap.2017.08.003.
- Gualano MR, Bert F, Voglino G, Buttinelli E, D’Errico MM, De Waure C, Di Giovanni P, Fantini MP, Giuliani AR, Marranzano M, et al. Attitudes towards compulsory vaccination in Italy: results from the NAVIDAD multicentre study. Vaccine. 2018;36:3368–7334. doi:10.1016/j.vaccine.2018.04.029.
- Corben P, Leask J. Vaccination hesitancy in the antenatal period: a cross-sectional survey. BMC Public Health. 2018;18(1):566. doi:10.1186/s12889-018-5389-6.
- Daley MF, Narwaney KJ, Shoup JA, Wagner NM, Glanz JM. Addressing parents’ vaccine concerns: a randomized trial of a social media intervention. Am J Prev Med. 2018;55(1):44–54. doi:10.1016/j.amepre.2018.04.010.
- Betsch C, Bödeker B, Schmid P, Wichmann O. How baby’s first shot determines the development of maternal attitudes towards vaccination. Vaccine. 2018;36(21):3018–26. doi:10.1016/j.vaccine.2018.04.023.
- Danchin MH, Costa-Pinto J, Attwell K, Willaby H, Wiley K, Hoq M, Leask J, Perrett KP, O’Keefe J, Giles ML, et al. Vaccine decision-making begins in pregnancy: correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine. 2018;36(44):6473–79. doi:10.1016/j.vaccine.2017.08.003.
- Rosso A, Massimi A, De Vito C, Adamo G, Baccolini V, Marzuillo C, Vacchio MR, Villari P. Knowledge and attitudes on pediatric vaccinations and intention to vaccinate in a sample of pregnant women from the City of Rome. Vaccine. 2019;37(14):1954–63. doi:10.1016/j.vaccine.2019.02.049.
- Bechini A, Moscadelli A, Pieralli F, Sartor G, Seravalli V, Panatto D, Amicizia D, Bonanni P, Boccalini S. Impact assessment of an education course on vaccinations in a population of pregnant women: a pilot study. J Prev Med Hyg. 2019;60(1):E5–11. doi:10.15167/2421-4248/jpmh2019.60.1.1093.
- Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–605. doi:10.1016/j.vaccine.2011.06.115.
- Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013;167(11):1065–71. doi:10.1001/jamapediatrics.2013.2483.47.
- Manzoli L, Flacco ME, D’Addario M, Capasso L, De Vito C, Marzuillo C, Villari P, Ioannidis JPA. Non-publication and delayed publication of randomized trials on vaccines: survey. BMJ. 2014;348:g3058. doi:10.1136/bmj.g3058.
- De Vito C, Manzoli L, Marzuillo C, Anastasi D, Boccia A, Villari P. A systematic review evaluating the potential for bias and the methodological quality of meta-analyses in vaccinology. Vaccine. 2007;25:8794–806. doi:10.1016/j.vaccine.2007.10.034.
- Adamo G, Sturabotti G, Baccolini V, de Soccio P, Prencipe GP, Bella A, Magurano F, Iannazzo S, Villari P, Marzuillo C, et al. Regional reports for the subnational monitoring of measles elimination in Italy and the identification of local barriers to the attainment of the elimination goal. PLoS One. 2018;13(10):e0205147. doi:10.1371/journal.pone.0205147.
- Marti M, de Cola M, MacDonald NE, Dumolard L, Duclos P. Assessments of global drivers of vaccine hesitancy in 2014—looking beyond safety concerns. PLoS One. 2017;12(3):e0172310. doi:10.1371/journal.pone.0172310.
- Goldstein S, MacDonald NE, Guirguis S, SAGE Working Group on Vaccine Hesitancy Collaborators. Health communication and vaccine hesitancy. Vaccine. 2015;33(34):4212–14. doi:10.1016/j.vaccine.2015.04.042.
- Filia A, Bella A, D’Ancona F, Fabiani M, Giambi C, Rizzo C, Ferrara L, Pascucci MG, Rota MC. Childhood vaccinations: knowledge, attitudes and practices of paediatricians and factors associated with their confidence in addressing parental concerns, Italy, 2016. Euro Surveill. 2019;24:6. doi:10.2807/1560-7917.ES.2019.24.6.1800275.
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–06. doi:10.1016/j.vaccine.2016.10.042.
- Verger P, Fressard L, Collange F, Gautier A, Jestin C, Launay O, Raude J, Pulcini C, Peretti-Watel P. Vaccine hesitancy among general practitioners and its determinants during controversies: A national cross-sectional survey in France. EBioMedicine. 2015;2(8):891–97. doi:10.1016/j.ebiom.2015.06.018.
- Verger P, Collange F, Fressard L, Bocquier A, Gautier A, Pulcini C, Raude J, Peretti-Watel P. Prevalence and correlates of vaccine hesitancy among general practitioners: a cross-sectional telephone survey in France, April to July 2014. Euro Surveill. 2016;21(47):30406. doi:10.2807/1560-7917.ES.2016.21.47.30406.
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–59. doi:10.1016/j.vaccine.2014.01.081.
- Larson Williams A, Mitrovich R, Mwananyanda L, Gill C. Maternal vaccine knowledge in low- and middle-income countries—and why it matters. Hum Vaccin Immunother. 2019;15(2):283–86. doi:10.1080/21645515.2018.1526589.
- Massimi A, Rosso A, Marzuillo C, Prencipe GP, De Soccio P, Adamo G, Sturabotti G, Vacchio MR, De Vito C, Villari P. Childhood vaccinations: a pilot study on knowledge, attitudes and vaccine hesitancy in pregnant women. Epidemiol Biostat Public Health. 2017;14:e126251–55. doi:10.2427/12625.
- Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, Paterson P. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother. 2018;14(7):1599–609. doi:10.1080/21645515.2018.1459252.
