ABSTRACT
The resurgence of whooping cough since the introduction of acellular (protein) vaccines has led to a renewed interest in the development of improved pertussis vaccines; Outer Membrane Vesicles (OMVs) carrying pertussis antigens have emerged as viable candidates. An in silico immunogenicity screen was carried out on 49 well-known Bordetella pertussis proteins in order to better understand their potential role toward the efficacy of pertussis OMVs for vaccine design; seven proteins were identified as being good candidates for including in optimized cellular and acellular pertussis vaccines. We then screened these antigens for putative tolerance-inducing sequences, as proteins with reduced tolerogenicity have improved vaccine potency in preclinical models. We used specialized homology tools (JanusMatrix) to identify peptides in the proteins that were cross-reactive with human sequences. Four of the 19 identified cross-reactive peptides were detolerized in silico using a separate tool, OptiMatrix, which disrupted the potential of these peptides to bind to human HLA and murine MHC. Four selected cross-reactive peptides and their detolerized variants were synthesized and their binding to a set of eight common HLA class II alleles was assessed in vitro. Reduced binding affinity to HLA class II was observed for the detolerized variants compared to the wild-type peptides, highlighting the potential of this approach for designing more efficacious pertussis vaccines.
Introduction
The causative agent of whooping cough or pertussis, the Gram-negative bacterium Bordetella pertussis (Bp), accounted for high mortality rates among children in the pre-vaccine era. The number of cases drastically decreased since the introduction of a pertussis vaccine in the 1950s. Whooping cough has reemerged in recent years despite relatively high vaccination rates and several decades of successful infant immunization programs.Citation1–Citation11 Several factors may be contributing to this increase, such as improved diagnoses, vaccination-induced pathogen adaptation, weaker memory responses and increased transmission due to the replacement of killed whole-cell pertussis vaccines (wPVs) with acellular vaccines (aPVs).
Development of aPVs was initiated due to public concerns with respect to the reactogenicity of the wPVs. The first aPV was introduced in Japan in 1981Citation12,Citation13 and was subsequently integrated into the vaccination programs of other developed countries.Citation14,Citation15 The aPVs currently in use contains one to five purified Bp proteins adjuvated with alum. The proteins included in the vaccines are: pertussis toxoid (Ptx: a protein complex of five different protein subunits), filamentous hemagglutinin (FhaB), pertactin (Prn), and fimbriae types 2 and 3 (Fim2 and Fim3). The amino acid sequence of FhaB encodes a preproprotein and its mature version is used as a component in several aPVs. A monovalent Ptx vaccine is used in Denmark whereas a trivalent aPV (Ptx, Prn, Fha) or pentavalent aPV (Ptx, Prn, Fha, Fim2, and Fim3) is used in most other high-income countries.
The aPVs are currently thought to induce an inferior immune response compared to wPVs. While aPVs do protect against severe disease and mortality in the first year of life, evidence suggests that the immune response is less broad, perhaps due to fewer antigens being present in the vaccine. In addition, wPV induces a mixed Th response with a Th1/Th17 bias, whereas aPV induces a Th2-dominated response. The latter was shown to result in more asymptomatic transmission and to provide a shorter duration of protection.Citation13,Citation16 Therefore, in 2015, the World Health Organization recommended that national vaccination programs that currently use wPV should continue to do so for the primary vaccination series.Citation13
Young infants are more vulnerable to pertussis and their morbidity and mortality risks are higher. Efforts to reduce transmission of pertussis to infants include the recommendation of additional booster vaccinations for teenagers, who act as a reservoir for transmission, maternal immunization or cocooning strategies.Citation17 However, all three approaches are difficult to implement on a large scale and are unlikely to control pertussis in the long-term.
Improved pertussis vaccines that provide broader immune responses, that stimulate long-term protection and that could prevent transmission may solve these problems. New types of vaccines currently under development include a live attenuated vaccine and Bp Outer Membrane Vesicle (OMV) vaccines (omvPV).Citation18 With respect to omvPV, it is hypothesized that these vaccines would provide the broad and long-term protective immune memory similar to the first-generation wPV, while also featuring a safety profile that is comparable to the second-generation and less reactogenic aPVs. Previous studies with omvPVs have shown that they confer protection in mice after both subcutaneous and mucosal immunization with a mixed Th1/Th17 response, similar to the response induced by infection.Citation19–Citation21 These results suggest that omvPVs have the potential to be a safe and effective next-generation pertussis vaccine.
Genetic engineering of Bp strains used in omvPV development allows for further reduction of reactogenicity and immunogenicity optimization. For example, genetic engineering of the LPS biosynthesis pathway has led to the identification of deletion mutants with reduced endotoxic activity.Citation22,Citation23 In addition, bacteria could be modified to express immunogenic proteins or peptides in their OMVs that are either not naturally present, or only present in very low amounts.Citation24–Citation27 Also, proteins that may downregulate immune responses, e.g. by activating regulatory T cell (Treg) pathways, can be removed and/or the regions of these proteins that induce Treg response can be altered.
Mouse studies have showcased differences in antibody responses and the type of T cell responses induced by aPV, omvPV, and infection. However, the poor correlation between serum antibody titers and effective protection from infection indicates that T cells may play an important role in protection against Bp. Published reports regarding Bp virulence factors have primarily focused on B cell epitopes, while only 14 HLA class II restricted T cell epitopes have been reported.Citation28 In the current study, a comprehensive in silico immunogenicity screen was performed to gain more insight in the potential contribution of well-known Bp proteins toward the efficacy and safety of omvPVs. In addition, in silico tools were used to screen these antigens for the presence of epitopes to which the immune system may be tolerant, due to high homology at the TCR interface with self-sequences.
Forty-nine Bp proteins were selected for an in silico evaluation of their HLA class II restricted T cell-dependent immunogenic potential. Selection criteria for these proteins included their role in the virulence of Bp, their confirmed immunogenicity in mice, or their abundance in wild-type (WT) omvPVs, wPVs,Citation29 or aPVs. A homology screen against the human proteome was also performed to determine if these antigens contained T cell epitopes that had potential immune-modulating cross-reactivity with T cells trained to recognize human antigens.Citation30 Seven of these 49 proteins were subsequently studied in detail, particularly with regard to their immune-modulating potential. Two outer membrane proteins, Vag8 and BrkA, were selected for detailed evaluation because they are the two most abundant proteins in WT OMVs and rank among the top 10 most abundant proteins in wPV.Citation29 In addition, these proteins are present in Bp in its virulent phaseCitation31 and induce strong antibody responses in mice. Even though Ptx is not present in WT Bp OMVs, three subunits of Ptx (S1, S2, S3) were also selected as they are virulence factors generally thought to be important for protection, as showcased by the monovalent Ptx-based vaccine currently used in Denmark.
Finally, two virulence factors that are present in most aPVs but only present in low amounts in WT Bp OMVs, Prn and FhaB, were selected. This in-depth analysis focused on the characterization of epitopes associated with tolerance. Amino acid modifications were introduced in four of the identified putative Treg epitopes to remove the predicted tolerogenic signals. The predicted detolerized epitopes were confirmed to have reduced HLA binding affinity compared to their wild-type counterparts when tested in vitro.
Material & methods
In silico analysis
Amino acid sequences were retrieved for 49 Bp antigens (Tohama I/ATCC BAA-589/NCTC 13251) from the UniProt database and evaluated for HLA class II epitope content using the EpiMatrix algorithm.Citation32 This algorithm as well as the ClustiMer, JanusMatrix, and OptiMatrix algorithms discussed below are part of the proprietary iVAX toolkit developed by EpiVax, which is available for use under a commercial license or in grant-funded collaborations.
Each input sequence was parsed into overlapping 9-mer frames. In total, 180,323 frame-by-allele assessments were analyzed (Supplementary Table 1). Each 9-mer frame was evaluated for its likelihood to be presented by a panel of eight HLA class II supertype alleles: DRB1*0101, DRB1*0301, DRB1*0401, DRB1*0701, DRB1*0801, DRB1*1101, DRB1*1301, and DRB1*1501. Collectively, these alleles cover HLA variability of over 95% of the human population worldwide.Citation33 Input sequences were also evaluated for their potential to present epitopes via the I-Ad and I-Ed Balb/c MHC class II alleles. Each significant 9-mer/allele assessment is defined as an EpiMatrix hit and epitope density is summarized into an EpiMatrix Protein Score. Proteins with EpiMatrix Scores greater than 20 are considered to have an elevated immunogenic potential, while randomly generated sequences are expected to score around zero. A normalization process allows EpiMatrix Scores to be compared across antigens of different lengths or against a set of benchmark antigens on an EpiMatrix immunogenicity scale.
Regions of high epitope density were then identified in the protein sequences, using the ClustiMer algorithm, for selection of vaccine candidates with an increased breadth of reactivity.Citation32 ClustiMer searches for contiguous segments of 15–30 amino acids with elevated binding across common HLA-DR alleles. Epitope density within a cluster is estimated by EpiMatrix Cluster Scores, where scores of 10 and above are considered elevated. Peptide sequences with elevated EpiMatrix Cluster Scores contain multiple HLA class II binding motifs with scores reflecting the high likelihood of binding to most, if not all, HLA-DR supertype alleles.
Full-length antigens or clusters were subsequently evaluated with the JanusMatrix algorithm to identify epitopes that may be unlikely to stimulate effector T cell responses due to similarity (at the T cell receptor interface of the epitope) with epitopes contained in host antigens.Citation30 Each of the putative T cell epitopes identified by EpiMatrix was screened for T cell receptor (TCR)-face homology against epitopes derived from the human proteome (and restricted by the same HLA allele). A full description of the methodology has been published.Citation30 Full-length antigens and clusters with a JanusMatrix Homology Score greater than 3 and 2, respectively, are hypothesized to contain tolerated epitopes or epitopes that induce regulatory T cell (Treg) responses. Sequences with similar homology scores have been found to induce Tregs in several other studies.Citation34–Citation36 Clusters with a high potential for cross-reactivity with self-sequences were set aside for later evaluation.
A subset of these putative Treg sequences were further analyzed with the OptiMatrix algorithm to identify amino acid changes that could disrupt their regulatory potential. Mutations were identified such that they would (1) remove the binding motif of the putative Treg epitopes, or (2) modify the TCR-face of the putative Treg epitopes such that it decreases their homology with self-sequences and renders them more non-self.
Peptide synthesis
Selected HLA class II-restricted peptides were synthesized using standard solid-phase 9-fluoronylmethoxycarbonyl (Fmoc) chemistry (21st Century Biochemicals). The peptides were designed with N-terminal acetyl group and C-terminal amino group caps and delivered >85% pure as ascertained by HPLC, mass spectrometry and UV scan (ensuring purity, mass, and spectrum, respectively). Based on advice received from twenty-first Century Biochemicals, the BrkA_357 WT/OPT and Vag8_282 WT peptides were synthesized without an N-terminal acetyl group to facilitate synthesis and purification. In all cases, the amino acid content of each peptide was determined to enable reconstitution at highly accurate molarity.
HLA class II binding assay
In vitro HLA class II binding assays were performed as described previously.Citation37,Citation38 The binding assay yields an indirect measure of peptide-MHC affinity. In this assay, a fluorescently labeled, high binding control peptide, and soluble HLA molecules are loaded onto a 96-well plate along with unlabeled experimental peptides. The mixture is then allowed to stand overnight. Once the mixture has reached steady equilibrium (at 24 h), the HLA-peptide complexes are captured on an ELISA plate coated with anti-human HLA-DR antibody and labeled control peptides are detected with an Europium-linked probe. Time-resolved fluorescence measuring bound, labeled control peptide is assessed by a SpectraMax M5 unit. Binding of experimental peptides is expressed as the percent inhibition of the labeled control peptide (experimental fluorescence/control fluorescence multiplied by 100). The percent inhibition values for each experimental peptide (across a range of molar concentrations) are used to calculate the concentration at which it inhibits 50% of the labeled control peptide’s specific binding. This value is referred to as the peptide’s IC50.
The experimental peptides were initially solvated in DMSO. The reconstituted peptides were then mixed with binding reagents in aqueous buffering solution, yielding a range of final concentrations from 100,000 nM down to 100 nM. All peptides were then assayed against a panel of eight common HLA class II alleles: DRB1*0101, DRB1*0301, DRB1*0401, DRB1*0701, DRB1*0801, DRB1*1101, DRB1*1301, and DRB1*1501.
In this assay, the experimental peptides are considered to bind with very high affinity if they inhibit 50% of control peptide binding at a concentration of 100 nM or less, high affinity if they inhibit 50% of control peptide binding at a concentration between 100 nM and 1,000 nM, and moderate affinity if they inhibit 50% of control peptide binding at a concentration between 1,000 nM and 10,000 nM. Low-affinity peptides inhibit 50% of control peptide binding at concentrations between 10,000 nM and 100,000 nM. Peptides that fail to inhibit at least 50% of control peptide binding at any concentration below 100,000 nM or do not show a dose-dependent response pattern are considered to have a negligible affinity or to be non-binders, respectively.
Results
Overall immunogenicity and homology to the human proteome for 49 pertussis proteins
A selection of 49 proteins was made from thousands of potential vaccine targets present in pertussis (over 3,000) since immunogenicity screening of all potential vaccine targets would have been too time-consuming and costly. Twenty-three virulence factors were selected from a study by van de Waterbeemd and coworkers.Citation39 Twenty-six proteins were selected for their abundance in omvPVs and 22 proteins for their abundance in wPVs, based on LC-MS.Citation29 Furthermore, 8 proteins present in aPVs (pertussis toxin consists of 5 subunits) and 12 proteins with confirmed immunogenicity in miceCitation29 were selected (supplementary Table 2). Several proteins had multiple selection criteria (supplementary Figure 1) resulting in 49 unique proteins.
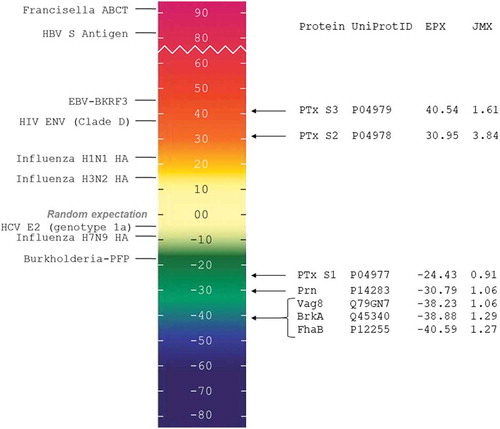
The 49 Bp antigens were screened with the iVAX platform to evaluate their overall immunogenic potential, calculated as EpiMatrix Protein Scores. Scores for these antigens ranged from 129.55 to −61.83 on the normalized immunogenicity scale (Supplementary Figure 2). Eight of the 49 proteins (16%) score in the upper range on the immunogenicity scale (i.e. their EpiMatrix Protein Scores exceed +20), indicating an elevated immunogenic potential. Sixteen out of 49 proteins (32%) score in the neutral range (EpiMatrix Protein Scores between −20 and +20), indicating an average immunogenic potential. Twenty-five out of 49 proteins (51%) score in the lower range on the EpiMatrix scale (EpiMatrix Protein Scores below −20), indicating a weak immunogenic potential.
Homology to the human proteome was then investigated with the JanusMatrix algorithm. Overall JanusMatrix Homology Scores for the 49 pertussis protein sequences ranged from 0.30 to 5.77, with an average JanusMatrix Homology Score of 1.71 (Supplementary Table 1). Six proteins had JanusMatrix Homology Scores ranging above 3, from 3.05 to 5.77. These proteins are expected to contain significant numbers of potentially cross-reactive peptides which may induce tolerance due to their homology with human sequences. This does not, however, mean that proteins with low JanusMatrix Homology Scores do not contain potentially cross-reactive peptides. Out of the eight proteins scoring highest on the immunogenicity scale (EpiMatrix Protein Score above 20), two were predicted to be potentially tolerated (EpiMatrix Protein Score above 20 and JanusMatrix Homology scores above 3). Four other proteins with a lower immunogenicity score also had high JanusMatrix Homology Scores and were also thought to be potentially tolerated.
In-depth analysis of seven pertussis proteins
Seven of the 49 Bp protein sequences were selected to be studied in detail using the iVAX platform: Vag8, BrkA, Ptx subunits S1, S2, and S3, Prn and FhaB ( and ). Selection of these proteins was not solely based on their immunogenicity and JanusMatrix scores from the initial screening, but also on their expected relevance for OMV vaccine design and presence in aPVs.
Table 1. Seven pertussis proteins ranked by JanusMatrix homology scores.
Figure 1. EpiMatrix Protein Immunogenicity Scale. EpiMatrix Protein Immunogenicity Scores (EPX) higher than 20 are considered to be potentially immunogenic. On the left of the scale we have included some well-known proteins for comparison. Note that the low-scoring proteins near the bottom of the scale are known to engender little to no immunogenicity while the higher scoring proteins near the top of the scale are all known immunogens. JanusMatrix Homology Scores (JMX) indicates the level of homology between epitopes present in the source antigen and with epitopes derived from the human proteome.
The eight proteins with overall immunogenicity scores above 20 and the six proteins with high Janus scores, were detected in very low amount in LC-MS analyses of omvPVs (<0.40% and <1.06% of total protein, respectively) or not detected at all and therefore considered less relevant for OMV vaccine design. Of note, engineering in antigens with the highest immunogenic potential and limited predicted similarity with self-antigens into OMVs may offer a way to increase their antigenicity while mitigating risks of inducing tolerance. Currently, however, these proteins can be considered to be less than ideal candidates for removing potential tolerance inducing epitopes because of their absence or low abundance in OMVs and their limited homology with human sequences.
Three of the eight immunogenic proteins are present in acellular vaccines: Ptx S2, S3 and S5, as components of Pertussis toxin. The subunits with the highest scores, S2 and S3, were therefore selected for detailed analyses. In addition, Ptx S2 also showed regions with a high JanusMatrix homology score.
Five additional proteins were selected for detailed analyses despite having low-predicted immunogenicity and JanusMatrix scores. Ptx S1, FhaB, and Prn were selected because they are important components of aPVs. Vag8 and BrkA were selected because they are highly abundant in omvPVsCitation29 (33.98% and 24.10% of total protein, respectively).
The in-depth immunogenicity analysis identified 113 epitope clusters containing potential T effector (Teff) or T regulatory (Treg) epitopes (data not shown). Eight epitopes were excluded since they are located in the signal peptides of their source antigen and are thus absent from the mature protein. Of the 105 remaining epitopes, 86 were identified as putative Teff epitopes and 19 displayed a high degree of homology with the human proteome and were therefore designated as putative Treg epitopes, following similar approaches used when identifying and validating tolerogenic sequences in our other vaccine work.Citation34–Citation36 The iVAX platform identified three putative Treg epitope sequences in both Vag8 and BrkA, 11 in FhaB, and one in both Ptx subunit S2 and Prn. These sequences have similar homology scores to previously identified Treg epitopes.Citation34–Citation36 No putative Treg epitope sequences were found in Ptx subunits S1 and S3.
Design of detolerized variants of four putative T regulatory epitopes
Out of the 19 putative Treg epitopes with elevated human cross-conservation, four putative Treg peptide epitopes (designated WT for wild-type) were selected based on their elevated cross-conservation with the Balb/c proteome (), rendering them relevant in humans as well as in murine models which are currently used in vaccine development. Two of these four putative Treg epitopes were derived from Vag8 (Vag8_282; 15-mer sequence and Vag8_385; 16-mer sequence), one was derived from BrkA (BrkA_357; 17-mer sequence), and one was derived from FhaB (FhaB_531; 17-mer sequence). Detolerized variants (designated OPT for optimized; ) were designed with iVAX for each peptide by disrupting the binding anchors of the predicted human HLA and murine MHC binding motifs. Limiting the binding affinity effectively abrogates the ability of the peptide to induce a T cell response, whether regulatory or effector. Detolerized and wild-type sequences had identical lengths.
Table 2. Candidate T regulatory peptides derived from Bp with elevated cross-conservation to human and Balb/c mice (WT) and their detolerized variants (OPT).
The binding affinity of these eight peptides (4 WT and 4 OPT peptides) was tested and validated in in vitro HLA class II binding assays for eight supertype HLA-DRB1 alleles.
HLA class II binding assays
shows the binding results for the putative T regulatory peptides and their detolerized variants (see also Supplementary Table 3). In the case of BrkA_357, the WT peptide bound to all eight alleles, as predicted. Disruption of the predicted binding anchors in OPT-BrkA_357 reduced the binding affinity of the peptide for HLA-DR in all cases. For DRB1*0101, OPT-BrkA_357 bound at a lower affinity but within the same affinity category. For DRB1*0401, DRB1*1101, and DRB1*1501, OPT-BrkA_357 bound at a lower affinity category. For DRB1*0801, the OPT peptide bound with a negligible affinity, and for DRB1*0301, DRB1*0701, and DRB1*1301, the OPT-BrkA was a non-binder. In addition, modifications to the OPT peptide affect TCR facing residues in all three 9-mer framesCitation30 that remain predicted to bind to HLA-DR, reducing the likelihood of cross-conserved T cell responses.
Figure 2. Measured IC50 of the candidate T regulatory peptides and their detolerized variants across HLA-DR alleles. Each line connects the IC50 measured for the wild-type (WT) and detolerized (optimized, OPT) sequences for HLA-DR1, HLA-DR3, HLA-DR4, HLA-DR7, HLA-DR8, HLA-DR11, HLA-DR13, and HLA-DR15. Binding affinity categories: very high affinity, IC50 ≤ 100 nM, high affinity, 100 nM < IC50 ≤ 1,000 nM, moderate affinity, 1,000 nM < IC50 ≤ 10,000 nM, low affinity, 10,000 nM < IC50 ≤ 100,000 nM, negligible affinity, 100,000 nM < IC50. Peptides with no dose-dependent response (no IC50) are considered non-binders.
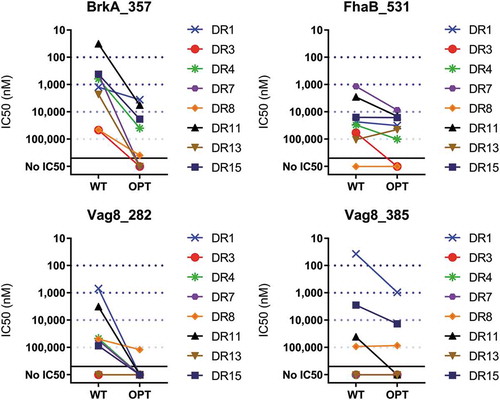
In the case of FhaB_531, the WT peptide bound to six of the eight alleles. Disruption of binding anchors in OPT-FhaB_531 reduced the binding affinity in all six cases. For DRB1*0101, DRB1*0401, DRB1*0701, and DRB1*1501, OPT-FhaB_531 bound at a lower affinity but within the same affinity category as the WT peptide. For DRB1*1101, WT-FhaB_531 bound at moderate affinity while the OPT peptide registered an IC50 in the low-affinity category. Conversely, for DRB1*1301, the WT peptide had a negligible affinity, but the OPT peptide bound at a low affinity. For DRB1*0301, OPT-FhaB_531 was a non-binder. Lastly, for DRB1*0801, neither the WT nor the OPT sequences bound, as predicted. In addition, modifications to the OPT peptide affect TCR facing residues in two of the four 9-mer frames that remain predicted to bind to HLA-DR, reducing the likelihood of cross-recognition by tolerogenic T cells.
The WT version of Vag8_282 bound to six alleles. For all six of these alleles, the OPT version bound at a reduced affinity. For DRB1*0101, DRB1*0401, DRB1*0701, DRB1*1101, and DRB1*1501, the OPT peptide was a non-binder, while for DRB1*0801 the OPT peptide had a negligible affinity.
Lastly, the WT version Vag8_385 bound to four alleles. For three of these alleles, the OPT version bound at a reduced affinity. For DRB1*0101 and DRB1*1501, the OPT peptide bound within a lower affinity category, while for DRB1*1101 OPT Vag8_385 was a non-binder. For DRB1*0801, there was no change in the binding category and for DRB1*0301, DRB1*0401, DRB1*0701, and DRB1*1301 neither the WT nor the OPT versions showed any binding. In addition, modifications to the OPT Vag8_385 affect TCR facing residues of all three 9-mer frames that remain predicted to bind to HLA-DR.
Discussion
Epitope-engineering is a well-established technique that has been used widely in protein therapeutics,Citation40–Citation42 and has also been used to modify potential cross-reactive epitopes that could contribute to undesirable auto-immune responses. For example, the approach was used to reduce the potential for cross-reactivity with self in the context of a Lyme disease vaccine.Citation43 Recent studies have demonstrated that engineering epitopes may also improve the antigenicity and efficacy of vaccines.
Here we performed a first high-level screen of 49 candidate Bp vaccine antigens that showed that these proteins covered the whole range of immunogenic potential, from elevated to negligible (Supplementary Figure 2). It is notable that few Bp proteins (16%) were identified as potentially highly immunogenic based on their predicted T cell epitope content, while the majority of proteins were predicted to have a low or neutral immunogenicity potential. In this regard, some proteins were classified very differently from what was expected. For example, Ptx S1 is a protein against which a very strong antibody response is raised and for which putative T cell epitopes have been reported, whereas no putative T cell epitopes have been reported in the literature for Ptx S2.Citation28 In our MHC II-restricted T cell screen, however, Ptx S1 was the only Ptx subunit with an overall low predicted immunogenic potential, whereas Ptx S2 showed an elevated predicted immunogenic potential.
Discrepancies between observed and predicted immunogenicity might be explained in several ways. First, B cell and helper T cell epitopes do not necessarily co-localize, on the same protein. Alternatively, proteins with several immunogenic regions, but also long stretches of low T cell epitope content, have lower scores than shorter proteins with more concentrated T cell epitopes per unit protein. The immunogenic regions of these low-scoring proteins may, however, drive effective immune response. Indeed, Ptx S1 is not devoid of T cell epitopes and contains six predicted effector T cell epitope clusters with an immunogenicity score above 10 (data not shown). These may induce an immune response despite the overall immunogenic potential of the protein. The normalization of the immunogenicity scores based on protein length also tends to disfavor shorter protein sequences, such as Ptx S1.
In addition, it is important to identify signal peptides when evaluating the immunogenicity of antigens. These regions usually contain many putative T cell epitopes, which can artificially distort the predicted immunogenic potential of mature antigens in which signal sequences are absent. Due to the highly homologous nature of signal peptides across proteins and species, putative T cell epitopes present within these regions tend to share a high degree of similarity with other self-sequences containing these motifs, which may also artificially increase predicted homology with human sequences.
Altogether, this initial screening of candidate epitopes gave a high-level overview of the overall immunogenic potential of Bp antigens. We, however, believe that a detailed screening is essential in order to better select and optimize antigens for vaccine design.
A detailed immunogenicity screening may be relatively easy to perform for viruses. The limited number of antigens present in their genomes usually allows the screening of all proteins within a short timeframe. Thousands of potential vaccine targets are however present in bacteria (over 3,000 in the case of pertussis). Therefore, the selection of a smaller subset of proteins is recommended to reduce analysis time and cost. Our in-depth analysis was restricted to seven Bp proteins known to be virulence factors. Other criteria for selection were their abundance in OMV (Vag8, BrkA), their presence in aPV (Ptx S1, S2, S3, Prn, FhaB) and high immunogenicity and homology scores in the previous high-level immunogenicity analysis (Ptx S2, S3).
Using the ClustiMer tool, we found 113 high-density T cell epitope clusters in the seven proteins under study, of which 19 were predicted to contain putative tolerance inducing epitopes. Identification of putative Treg epitopes using similar in silico methodologies and their subsequent functional validation has been previously reported by EpiVax.Citation34–Citation36 Since loss of immune memory is a problem associated with existing vaccines, removing these epitopes might increase the efficacy of vaccine antigens and could lead to increased longevity of memory responses. As a first step to test this hypothesis, putative Treg epitopes were carefully assessed, potential amino acid modifications were identified, and detolerized variants were designed to reduce their immunomodulating potential. Modifications that would reduce the HLA-DR binding of tolerizing epitopes were prioritized for testing in HLA binding assays.
The detolerized (or optimized) variants showed decreased binding affinities in in vitro HLA binding assays ( and Supplementary Figure 3), suggesting that putative tolerizing epitopes are less likely to be presented to circulating T cells, including Tregs, when detolerized. The modifications introduced here also took into consideration the removal of putative murine Treg epitopes, allowing the testing of concept vaccines lacking these immunomodulatory epitopes in mice and maximizing their relevance for translation to humans (binding to murine MHC was not tested but in vivo studies are anticipated).
While we have confirmed decreased binding affinity to HLA for the detolerized pertussis sequences, we have not validated in the current study the regulatory nature of the wild-type putative Treg epitopes using functional T cell assays. Although our approach has been validated in other studies,Citation34–Citation36 it is possible that some of the sequences selected for detolerization would not induce Tregs in their native form.
These results highlight that removing Treg epitopes from omvPVs via targeted mutagenesis to improve their efficacy is a potential method of improving vaccine efficacy. Such an approach was effectively applied to H7N9 influenza: a Treg epitope in the HA protein was identified in silico, modifications were introduced, and improved immunogenicity of the H7 hemagglutinin antigen was observed in vivo in humanized mice.Citation36 Additional influenza-related immune-engineering studies are ongoing.Citation44
Several aspects of this study are important for designing the next generation of Bp vaccines. First, lessons were learnt from broadly studied differences between the efficacy of wPV and aPV and between vaccines and natural infections. In this regard, omvPV were found to induce broad antibody responses and a mixed Th1/Th17-dominated T cell response in mice, resembling responses induced by wPVCitation21 and infection.Citation45 However, though responses to infection often serve as a reference, we know from past studies that natural infections confer improved protection compared to current vaccines, but do not promote life-long immunity to Bp.Citation46 Next-generation vaccines should ideally alleviate this issue, which could be achieved by removing immunomodulatory factors such as Treg epitopes.
This study has some potential limitations. In silico predictions are based on contiguous linear epitopes and spliced epitopes will not be found. With respect to modifying the sequence of putative Treg epitopes, it is possible that the amino acid changes that were introduced will affect the conformation of the antigen. Further investigation is needed to determine if these changes will disrupt existing B cell epitopes or the stability of proteins within the omvPV. In addition, the detailed immunogenicity screening and Treg epitope identification analyses performed here can be expanded to other Bp proteins to gain a more comprehensive understanding of pertussis antigens which could be important for the development of improved vaccines.
In conclusion, current pertussis vaccines are effectively preventing severe disease in young children, but new approaches are needed to reverse its resurgence. It is currently thought that increasing the longevity of memory responses and the prevention of asymptomatic transmission will be important characteristics of a truly improved vaccine. Removal of Treg epitopes present in natural Bp antigens could possibly contribute to this achievement. We detail here a method for the identification and modification putative Treg epitopes in pertussis antigens that are contained in current vaccines. We demonstrate that targeted modifications to a few key amino acids can reduce binding to HLA. Overall, the concept of removing or altering Treg epitopes from antigens used in current vaccines is possible and incorporation of these detolerized variants might be an important next step in vaccine optimization.
Disclosure of potential conflicts of interest
ADG and WM are senior officers and majority shareholders, and GR and PH were employees, at the time this research was conducted, of EpiVax, Inc., a company specializing in the immunoinformatic analysis. These authors recognize the presence of a potential conflict of interest and affirm that the information represented in this paper is original and based on unbiased observations.
Supplemental Material
Download Zip (4.1 MB)Acknowledgments
The collaboration project is co-funded by the PPP Allowance made available by Health~Holland, Top Sector Life Sciences & Health, to stimulate public–private partnerships. We would like to acknowledge Sundos Khan for her help in reviewing this manuscript, and the EpiVax laboratory team for performing the HLA Binding assays.
Supplementary Material
Supplemental data for this article can be accessed online at http://dx.doi.org/10.1080/21645515.2019.1703453.
Additional information
Funding
References
- Rumbo M, Hozbor D. Development of improved pertussis vaccine. Hum Vaccin Immunother. 2014;10:2450–53.
- Halperin SA. The control of pertussis–2007 and beyond. N Engl J Med. 2007;356:110–13.
- Libster R, Edwards KM. Re-emergence of pertussis: what are the solutions? Expert Rev Vaccines. 2012;11:1331–46.
- Cagney M, MacIntyre CR, McIntyre P, Puech M, Giammanco A. The seroepidemiology of pertussis in Australia during an epidemic period. Epidemiol Infect. 2006;134:1208–16.
- Celentano LP, Massari M, Paramatti D, Salmaso S, Tozzi AE, Group E-N. Resurgence of pertussis in Europe. Pediatr Infect Dis J. 2005;24:761–65.
- Clark TA. Changing pertussis epidemiology: everything old is new again. J Infect Dis. 2014;209:978–81.
- Fisman DN, Tang P, Hauck T, Richardson S, Drews SJ, Low DE, Jamieson F. Pertussis resurgence in Toronto, Canada: a population-based study including test-incidence feedback modeling. BMC Public Health. 2011;11:694.
- Rodgers L, Martin SW, Cohn A, Budd J, Marcon M, Terranella A, Mandal S, Salamon D, Leber A, Tondella ML, et al. Epidemiologic and laboratory features of a large outbreak of pertussis-like illnesses associated with cocirculating Bordetella holmesii and Bordetella pertussis–Ohio, 2010-2011. Clin Infect Dis. 2013;56:322–31.
- McCarthy M. Acellular vaccines provided less protection during California pertussis outbreak. BMJ. 2013;346:f3325.
- Hozbor D, Mooi F, Flores D, Weltman G, Bottero D, Fossati S, Lara C, Gaillard ME, Pianciola L, Zurita E, et al. Pertussis epidemiology in Argentina: trends over 2004-2007. J Infect. 2009;59:225–31.
- Cherry JD. Epidemic pertussis in 2012–the resurgence of a vaccine-preventable disease. N Engl J Med. 2012;367:785–87.
- Sato Y, Kimura M, Fukumi H. Development of a pertussis component vaccine in Japan. Lancet. 1984;1:122–26.
- WHO. Pertussis vaccines: WHO position paper, August 2015–recommendations. Vaccine 2016;34:1423–25.
- Greco D, Salmaso S, Mastrantonio P, Giuliano M, Tozzi AE, Anemona A, Ciofi Degli Atti ML, Giammanco A, Panei P, Blackwelder WC, et al. A controlled trial of two acellular vaccines and one whole-cell vaccine against pertussis. Progetto pertosse working group. N Engl J Med. 1996;334:341–48.
- Olin P, Rasmussen F, Gustafsson L, Hallander HO, Heijbel H. Randomised controlled trial of two-component, three-component, and five-component acellular pertussis vaccines compared with whole-cell pertussis vaccine. Ad Hoc group for the study of pertussis vaccines. Lancet. 1997;350:1569–77.
- Kapil P, Merkel TJ. Pertussis vaccines and protective immunity. Curr Opin Immunol. 2019;59:72–78.
- de Greeff SC, Teunis P, de Melker HE, Mooi FR, Notermans DW, Elvers B, Schellekens JF. Two-component cluster analysis of a large serodiagnostic database for specificity of increases of IgG antibodies against pertussis toxin in paired serum samples and of absolute values in single serum samples. Clin Vaccine Immunol. 2012;19:1452–56.
- Locht C. Will we have new pertussis vaccines? Vaccine. 2018;36:5460–69.
- Roberts R, Moreno G, Bottero D, Gaillard ME, Fingermann M, Graieb A, Rumbo M, Hozbor D. Outer membrane vesicles as acellular vaccine against pertussis. Vaccine. 2008;26:4639–46.
- Gaillard ME, Bottero D, Errea A, Ormazabal M, Zurita ME, Moreno G, Rumbo M, Castuma C, Bartel E, Flores D, et al. Acellular pertussis vaccine based on outer membrane vesicles capable of conferring both long-lasting immunity and protection against different strain genotypes. Vaccine. 2014;32:931–37.
- Raeven RH, Brummelman J, Pennings JL, van der Maas L, Tilstra W, Helm K, Van Riet E, Jiskoot W, Van Els CA, Han WG, et al. Bordetella pertussis outer membrane vesicle vaccine confers equal efficacy in mice with milder inflammatory responses compared to a whole-cell vaccine. Sci Rep. 2016;6:38240.
- Geurtsen J, Dzieciatkowska M, Steeghs L, Hamstra HJ, Boleij J, Broen K, Akkerman G, El Hassan H, Li J, Richards JC, et al. Identification of a novel lipopolysaccharide core biosynthesis gene cluster in Bordetella pertussis, and influence of core structure and lipid A glucosamine substitution on endotoxic activity. Infect Immun. 2009;77:2602–11.
- Geurtsen J, Steeghs L, Hamstra HJ, Ten Hove J, de Haan A, Kuipers B, Tommassen J, van der Ley P. Expression of the lipopolysaccharide-modifying enzymes PagP and PagL modulates the endotoxic activity of Bordetella pertussis. Infect Immun. 2006;74:5574–85.
- van de Waterbeemd B, Streefland M, van der Ley P, Zomer B, van Dijken H, Martens D, Wijffels R, Van der Pol L. Improved OMV vaccine against Neisseria meningitidis using genetically engineered strains and a detergent-free purification process. Vaccine. 2010;28:4810–16.
- van der Ley P, van der Biezen J, Poolman JT. Construction of Neisseria meningitidis strains carrying multiple chromosomal copies of the porA gene for use in the production of a multivalent outer membrane vesicle vaccine. Vaccine. 1995;13:401–07.
- Salverda ML, Meinderts SM, Hamstra HJ, Wagemakers A, Hovius JW, van der Ark A, Stork M, van der Ley P. Surface display of a borrelial lipoprotein on meningococcal outer membrane vesicles. Vaccine. 2016;34:1025–33.
- Rouppe van der Voort E, Schuller M, Holst J, de Vries P, van der Ley P, van den Dobbelsteen G, Poolman J. Immunogenicity studies with a genetically engineered hexavalent PorA and a wild-type meningococcal group B outer membrane vesicle vaccine in infant cynomolgus monkeys. Vaccine. 2000;18:1334–43.
- Vaughan K, Seymour E, Peters B, Sette A. Substantial gaps in knowledge of Bordetella pertussis antibody and T cell epitopes relevant for natural immunity and vaccine efficacy. Hum Immunol. 2014;75:440–51.
- Raeven RH, van der Maas L, Tilstra W, Uittenbogaard JP, Bindels TH, Kuipers B, van der Ark A, Pennings JL, van Riet E, Jiskoot W, et al. Immunoproteomic profiling of bordetella pertussis outer membrane vesicle vaccine reveals broad and balanced humoral immunogenicity. J Proteome Res. 2015;14:2929–42.
- Moise L, Gutierrez AH, Bailey-Kellogg C, Terry F, Leng Q, Abdel Hady KM, VerBerkmoes NC, Sztein MB, Losikoff PT, Martin WD, et al. The two-faced T cell epitope: examining the host-microbe interface with JanusMatrix. Hum Vaccin Immunother. 2013;9:1577–86.
- Cummings CA, Bootsma HJ, Relman DA, Miller JF. Species- and strain-specific control of a complex, flexible regulon by Bordetella BvgAS. J Bacteriol. 2006;188:1775–85.
- Moise L, Gutierrez A, Kibria F, Martin R, Tassone R, Liu R, Terry F, Martin B, De Groot AS. iVAX: an integrated toolkit for the selection and optimization of antigens and the design of epitope-driven vaccines. Hum Vaccin Immunother. 2015;11:2312–21.
- Southwood S, Sidney J, Kondo A, Del Guercio MF, Appella E, Hoffman S, Kubo RT, Chesnut RW, Grey HM, Sette A. Several common HLA-DR types share largely overlapping peptide binding repertoires. J Immunol. 1998;160:3363–73.
- Liu R, Moise L, Tassone R, Gutierrez AH, Terry FE, Sangare K, Ardito MT, Martin WD, De Groot AS. H7N9 T-cell epitopes that mimic human sequences are less immunogenic and may induce Treg-mediated tolerance. Hum Vaccin Immunother. 2015;11:2241–52.
- Losikoff PT, Mishra S, Terry F, Gutierrez A, Ardito MT, Fast L, Nevola M, Martin WD, Bailey-Kellogg C, De Groot AS, et al. HCV epitope, homologous to multiple human protein sequences, induces a regulatory T cell response in infected patients. J Hepatol. 2015;62:48–55.
- Wada Y, Nithichanon A, Nobusawa E, Moise L, Martin WD, Yamamoto N, Terahara K, Hagiwara H, Odagiri T, Tashiro M, et al. A humanized mouse model identifies key amino acids for low immunogenicity of H7N9 vaccines. Sci Rep. 2017;7:1283.
- Moise L, McMurry JA, Buus S, Frey S, Martin WD, De Groot AS. In silico-accelerated identification of conserved and immunogenic variola/vaccinia T-cell epitopes. Vaccine. 2009;27:6471–79.
- Steere AC, Klitz W, Drouin EE, Falk BA, Kwok WW, Nepom GT, Baxter-Lowe LA. Antibiotic-refractory Lyme arthritis is associated with HLA-DR molecules that bind a Borrelia burgdorferi peptide. J Exp Med. 2006;203:961–71.
- van de Waterbeemd B, Streefland M, Pennings J, van der Pol L, Beuvery C, Tramper J, Martens D. Gene-expression-based quality scores indicate optimal harvest point in Bordetella pertussis cultivation for vaccine production. Biotechnol Bioeng. 2009;103:900–08.
- Michalska M, Schultze-Seemann S, Kuckuck I, Wolf P. In vitro evaluation of humanized/de-immunized anti-PSMA immunotoxins for the treatment of prostate cancer. Anticancer Res. 2018;38:61–69.
- Cantor JR, Yoo TH, Dixit A, Iverson BL, Forsthuber TG, Georgiou G. Therapeutic enzyme deimmunization by combinatorial T-cell epitope removal using neutral drift. Proc Natl Acad Sci U S A. 2011;108:1272–77.
- King C, EN G, Mazor R, JL L, Pastan I, Pepper M, Baker D. Removing T-cell epitopes with computational protein design. Proc Natl Acad Sci U S A. 2014;111:8577–82.
- Federizon J, Lin YP, Lovell JF. Antigen engineering approaches for Lyme disease vaccines. Bioconjug Chem. 2019;30:1259–72.
- Moise LM, Biron B, Boyle CM, Kurt Yilmaz N, Jang H, Schiffer C, Ross T, Martin WD, De Groot AS. T cell epitope engineering: an avian H7N9 influenza vaccine strategy for pandemic preparedness and response. Hum Vaccin Immunother. 2018;14:2203–07.
- Raeven RH, Brummelman J, Pennings JLA, van der Maas L, Helm K, Tilstra W, Van Der Ark A, Sloots A, Van Der Ley P, Van Eden W, et al. Molecular and cellular signatures underlying superior immunity against Bordetella pertussis upon pulmonary vaccination. Mucosal Immunol. 2018;11:979–93.
- Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24:S58–61.
