ABSTRACT
Acceptance of the human papillomavirus (HPV) vaccination among parents and clinicians is high, but uptake remains low. Little is known about organizational and primary care team factors that influence the uptake of the HPV vaccine. Interviews with clinicians, clinic support staff, and parents of adolescent patients were conducted to better understand the interrelationships among the people and the organizational processes that influence HPV vaccine uptake at the point of care. Between July 2016 and February 2017, semi-structured interviews of 40 participants (18 clinicians, 12 clinic support staff, and 10 parents of adolescent patients) in a primary care network were conducted. Organizational structures and processes, such as electronic provider reminders, availability of “vaccination only” appointments, and knowledgeable primary care team members contributed to HPV vaccine uptake. Consistently high support of HPV vaccination was found among key informants; however, rather than refuse HPV vaccination, parents are opting to delay vaccination to a future visit. When parents express the desire to delay, clinicians and care team members described often recommending addressing HPV vaccination at a future visit, giving parents the impression that receiving the vaccine was not time-sensitive for their child. Discordance in HPV vaccination recommendations among providers and clinic support staff may contribute to delayed HPV vaccination. Strong, high-quality HPV vaccine recommendations are needed from all primary team members. Clinic interventions to accelerate HPV vaccine uptake may benefit from a team-based approach where every member of the primary care team is delivering the same consistent messaging about the importance of timely HPV vaccination.
Introduction
The human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. Approximately, 79 million Americans are currently infected and roughly 14 million Americans will acquire a new infection each year.Citation1 Spread through skin-to-skin contact and most commonly contracted through sexual contact, HPV impacts everyone, regardless of gender and sexual orientation. The Advisory Committee on Immunization Practices (ACIP) recommends routine HPV vaccination with the two-dose series at ages 11–12 years and recently updated their recommendation for catch up three-dose vaccination (for those who were not previously vaccinated) through age 26 for both males and females for the prevention of several HPV-associated diseases.Citation2 The prior HPV vaccine catch-up ages for males was 13 through 21Citation3 but is now aligned with the female recommendation to 26 years of age. The committee also recommended vaccination for individuals aged 27 through 45 years who have not been adequately vaccinated based on shared clinical decision-making between the patient and their provider.Citation2 HPV vaccination is the optimal primary prevention strategy against HPV-related diseases. The HPV vaccine can prevent about 92% of cancers caused by HPV and almost all cases of genital warts.Citation4
Despite these recommendations and the public health implications of full vaccination coverage, adolescent HPV vaccination rates remain low. In 2018, 51.1% of US adolescents aged 13–17 were up to date with the recommended HPV vaccination series.Citation5 Although this is an overall increase in uptake from previous years, it is still substantially lower than the coverage for the other two recommended vaccines at these ages; the tetanus, diphtheria, and acellular pertussis vaccine (Tdap) at 89%; and for the meningococcal conjugate vaccine (MenACWY) at 86.6%.Citation5
While there has been a wave of studies and systematic reviews that have examined the barriers and facilitators to HPV vaccination uptake,Citation6–Citation10 many of the findings from these studies have been inconsistent. These studies report high levels of vaccine acceptability among parents and clinicians; yet, nationally, HPV vaccine uptake remains far below the Healthy People 2020 goal of 80%.Citation11 The majority of studies have focused on one or two levels of influences (e.g., parents and/or clinicians); however, parents and clinicians have reported that their views on the HPV vaccine are influenced by each other as well as by factors related to the health care system.Citation6,Citation12,Citation13 Few studies have examined an integrated perspective that includes simultaneously elucidating the processes of care delivery and the role of primary care team members in facilitating the uptake of the HPV vaccine.Citation14–Citation16
The purpose of this study was to examine clinicians, clinic support staff, and parents of adolescent HPV vaccine delivery experiences at the point of care across an integrated primary care network. We sought to move beyond parent and individual clinician factors to include the perspective of other primary care team members, including nurses, medical assistants, clinic managers, and to clarify organizational factors, including patient care processes, decision support, clinic procedures and policies, and electronic health record systems in influencing HPV vaccine uptake. Exploring the relationships among individual, team, and organizational factors can help us better understand how these multiple levels of influences can contribute to the decision and follow-through of HPV vaccination. At each level, multiple converging and integrative processes determine whether vaccination occurs.
Materials and methods
Setting
This qualitative study was conducted within the University of California, Davis Health System (UCDHS) Primary Care Network (PCN). The PCN consists of 15 outpatient clinics located in Sacramento, CA, and the 9 surrounding communities. The majority of patients are privately insured. Interviews occurred between July 2016 and February 2017 at 9 participating clinics. The PCN provides care for about 8,300 adolescents aged 11–17 each year. The study protocol was approved by the University of California, Davis Institutional Review Board.
Participants
To be eligible for the study, participants had to be either a parent/guardian (hereby referred to as ‘parents’) of a patient aged 11–17 years; a clinician that provided primary care to patients aged 11–17 years; or a staff member who worked at a clinic that provided primary care to patients aged 11–17 years. Recruitment flyers were displayed at the clinics for parents and individual e-mails were sent to all clinicians and staff. Interested individuals called the number on the flyer and/or emailed the study coordinator directly to determine eligibility. Convenience (those who responded to the e-mail or flyer) and snowball (referral from participants) sampling was used to recruit the participants. All interviews were conducted in English. Parents and clinic staff received a $20 gift card as compensation for their participation and clinicians received a $40 gift card. Recruitment ended when data saturation was reached in each group with additional interviews yielding no new information (for parents this occurred after the eighth interview, or clinic support staff this occurred after the tenth interview and for clinicians this occurred after the fifteenth interview).
Interview and data analysis
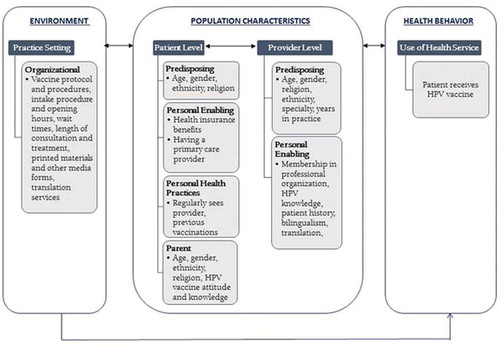
The Andersen Behavioral Model of Health Care Utilization,Citation17 one of the most well-established multilevel frameworks for investigating the use of health services guided the development of the interview guide. The model applies a systems perspective to integrate a range of domains associated with the decision to seek care. The Model posits that behaviors such as obtaining vaccinations are based upon the combination of patient predisposing characteristics (e.g., age, gender), enabling resources (e.g., patient–provider relationship, quality of communication), and need (e.g., individual perceived need and professional evaluated need). The Model also includes multiple feedback loops showing that outcome, in turn, affects population characteristics and health behavior. See for Adapted Anderson Model of Health Care Utilization.
Three separate interview guides, one for each category of informant (clinician, staff, and parent), were developed with probes for clarification to facilitate responses to the semi-structured and open-ended interview questions. The questions, grounded in the conceptual framework, were developed based on: (1) existing qualitative studies that explored factors that influence parental acceptance of the HPV vaccineCitation18,Citation19 and (2) patient,Citation20 provider,Citation21 and practice setting characteristicsCitation22 associated with vaccine uptake. Parent interviews assessed barriers and facilitators to accepting a recommendation from a clinician to get their child vaccinated; clinician interviews explored the barriers and facilitators to making a successful HPV vaccine recommendation for their patient; and staff interviews explored barriers and facilitators to carrying out that recommendation once a clinician has made it and a parent has accepted it. All three interview categories included individual (parent, clinician, and clinic staff), team and clinic/visit level questions and probes. Interview guides were also reviewed by clinical operations management and a parent whose adolescent was not receiving care at this academic medical center for appropriateness and comprehensiveness. Interviews were no longer than 30 min and began with a short survey to capture sociodemographics and clinic setting data. Questions focused on HPV vaccine knowledge, attitudes, and beliefs; barriers and facilitators to HPV vaccination; and recommendations to increase HPV vaccine uptake. See for domains of the framework that was included in the interview guide (some questions fit in multiple domains because of the probes following the initial question).Interviews were conducted by the research team, which consisted of the first author and three research assistants trained to conduct qualitative interviews. Clinician and staff interviews were conducted face to face while half of the parent interviews were conducted over the phone and the other half were conducted face to face. All interviews were digitally recorded, transcribed verbatim and uploaded into Dedoose, a software package for managing and analyzing qualitative research data.Citation23 Answers to open-ended questions were coded according to predefined categories based on the interview guide: (1) barriers; (2) facilitators; and (3) attitudes, knowledge, and beliefs about HPV vaccination and HPV-related disease. These categories were utilized to identify key points within the data (themes) with additional themes and subthemes created as they emerged. Three researchers independently coded the transcripts and then met to review codes and their meanings. Codes and themes were discussed to resolve initial differences and modifications of codes were made until agreement among all codes was achieved. Inter-rater agreement was 90% or greater for all codes and themes. Findings were then reconciled, summarized, and categorized.
Table 1. Components of the multilevel of influence framework included in the interview guide.
Results
Summary of survey
A total of 40 individuals participated in the interviews (10 parents/guardians, 12 clinic support staff, and 18 clinicians). All the parents interviewed were female and the majority were: between the ages of 40 and 49; have had some college experience; fluent in a second language; Christian; White; and born in the United States. All reported having insurance that would cover the cost of the HPV vaccine and 7 parents reported that their child has been vaccinated against HPV. Our parent sample is similar to the general PCN patient population in terms of race/ethnicity (majority being White) and having insurance that would cover the cost of the vaccine.
Clinicians included 10 pediatricians, an internal medicine specialist, 6 family practice physicians, and a physician assistant. The majority of clinicians were female; between the ages of 30 to 39; not fluent in a second language; Christian; employed by the health system for over 10 years; and born in the United States. All clinicians reported being a member of a professional medical association. Clinicians also reported that they recommended the HPV vaccine to all their patients between the ages of 11–17 all the time and that it is very important that their patients aged 11–17 be vaccinated against HPV. Additionally, clinicians stated they usually recommended the vaccine during routine visits and during physicals and the majority saw an average of 3–5 patients between the ages of 11–17 per a typical 8-h workday.
Clinic support staff included eight medical assistants (MAs), one licensed vocational nurse (LVN), and three clinic managers. The majority of clinic support staff were: female; between the ages of 30 to 39; Christian; not fluent in a second language; born in the United States; and were employed by the health system for over 10 years. All staff were familiar with the HPV vaccine, and all thought it was either very important or somewhat important that their patients aged 11–17 years be vaccinated against HPV. Characteristics of interview participants are summarized in .
Clinic staff reported a range of 10–50 adolescent patients seen at their clinic per day and in terms of clinic atmosphere the majority reported that their clinic was busy, but reasonable. Staff also reported that interpreters were readily available through the health system; however, the use of interpreters varied by clinic. Characteristics of clinics are summarized in .
Table 2. Characteristics of interview participants.
Major themes and the barriers, facilitators, and recommendations to improve HPV vaccinations are summarized in .
Table 3. Characteristics of clinics.
Table 4. Summary of key findings of practice, clinician, staff, and parent factors associated with HPV vaccine uptake and recommendations to accelerate HPV vaccine uptake.
Qualitative results by theme
Practice level
HPV vaccination at point of care
When asked how HPV vaccines are administered, clinic support staff and clinicians stated that once a parent consented to vaccination, the clinician placed an HPV vaccine order in the patient’s electronic medical record and after the clinician completed the visit, a clinic staff (e.g., MA, LVN, etc.) came into the exam room and administered the vaccine. Prior to administering the vaccine, the clinic staff asked the family if they had any questions concerning the vaccination process and/or the vaccine and if the family did, the clinic staff gave them the HPV Vaccine Information Sheet (VIS). Many of the clinic staff who administered the vaccine stated that parents usually had additional questions regarding the vaccine, even after agreeing with the clinician to vaccinate. When families had additional questions the MA/LVN “referred them back to their provider” and went “back to the doctor to tell them they changed their minds.” As explained by the LVN, “when they (parents) get the handout (VIS) and they look at it and the first thing that they see is sexually. So I think the way it is presented to them kind of pushes them off … and then they change their minds, they are like, I don’t want to get this.”
Infrastructure
All participants agreed that having a strong organizational infrastructure that was conducive to HPV vaccination aided in the administration of the vaccine. When asked what has helped with recommending the vaccine, one clinician stated, “I get a little warning in their medical records saying they’re due for it, so it makes it easy for me to remember to ask them.” Another clinician mentioned, “I have a great shot clinic that people can just walk in and go to and I think the availability of that is pretty open.” Parents also agreed that it was “super easy to schedule an (HPV vaccination) appointment” and as one parent exclaimed, “you don’t necessarily have to see the doctors, you just show up to the immunization nurses and they handle it really quickly. I just go in, there is no co-pay for the immunization.”
Parent primer (recommendation)
All participants felt that the health system could support HPV vaccination efforts by providing HPV vaccine education to parents prior to their child’s medical visit. As one clinician described, “we are a big health system, at some point we should have a health campaign or something that you know talks about getting the vaccine for your kid.” Another clinician suggested having the health system send out educational mailers to parents of 9- and 10-year-olds “so we can refer back to that, rather than hitting the parents with the information during visit.” Another clinician remarked, “It would be nice if people heard about the vaccine from places other than their doctor’s office, because then when they come in here, I just need to reinforce something that they already heard about. It’s always hard when they hear something completely new and then they are all nervous about it, and then they say well, I haven’t heard much about the vaccine, I wish I had more information.” Parents agreed that, “some parents want to be informed before the appointment, then they can send a brochure out through the mail and say hey this is coming up, just kind of a FYI.”
Clinician and staff level
Dealing with HPV vaccine-hesitant parents
When parents expressed a desire to delay getting the vaccine, staff, and clinicians did not push for same-day vaccination. Clinicians described the vaccine as “optional,” “not required for school,” and “not urgent.” For example, when asked how he dealt with parents who wanted to wait, one clinician stated he told families, “we have until you turn 26 to do this. It’s not an urgent vaccine and the next time you come in we can discuss it again.” Another clinician stated that he, “prints out the HPV vaccination sheet information, hand it to them (the family) and tell them whenever they are ready, I say call me and I can get it done.” One MA added, “maybe we will revisit it the next time they come in because there is a wide range of ages … they might refuse and say well can we do it next year or the year after.” Another MA responded, “I tell them they don’t have to do it today, the order is valid for two years depending on how the doctor ordered it and that they can come back once they do the research for it.”
Effective strategies
Clinicians and staff agreed that emphasizing the message of cancer prevention and normalizing the vaccine are the two most effective strategies to improve HPV vaccination rates. When asked why she chose to vaccinate her daughter, one mother exclaimed, “I don’t want my daughter or kids to have cervical cancer or anything. I would want my daughter to be prevented from any form of disease that will keep her from living her life.” Agreeing, the LVN stated, “they have to know the purpose of the vaccination is that it prevents diseases such as cervical cancer.” When describing his strategy, one clinician explained, “I usually start off talking that it’s to help prevent cancer. I talk about the importance of cancer prevention.”
Clinicians also presented the vaccine as they would any other vaccine by “listing it (the HPV vaccine) as a package expected at this age,” and stating that “the American Academy of Pediatrics recommends the following shots: HPV, Tdap, Meningococcal vaccine”. As described by one clinician, “Once I defined my approach of just packaging the HPV as part of a normal package deal for an 11-year-old, things started to become easier.” To normalize the vaccine, one clinician stated that she also made the following analogy to parents, “I just kind of reassure them that when they (their child) was first born, we gave them the Hepatitis B vaccine and that is also a sexually transmitted disease, and you (the parent) were okay with giving them that right at birth.”
Clinician and staff education (recommendation)
Clinicians and clinic support staff agreed that everyone (e.g., clinicians, administrative staff, MAs, nurses, etc.) at the clinic would benefit from “more HPV education” and that “the more people who mention it throughout the clinic visit, then the more receptive the parents are to have it done.” As one MA explained, “It doesn’t make any sense for you (staff) to go in a room and give somebody injections that you are not educated on. Oh, you (the parent) have a question, give me one moment to go back and ask the doctor, that is not efficient work at all.” Additionally, staff reported being asked by parents about their opinion on the HPV vaccine. For example, one MA said, “I would just discuss with them where I come from, I would let them know a little bit of my religious background, how my parents wouldn’t vaccinate me and how I felt as an adult now as vulnerable as a child.” Another MA added that when parents asked her about the vaccine she would respond with, “I have 2 kids, and when they are old enough, they will be vaccinated as well.”
When asked what would make the greatest impact on increasing the HPV vaccine uptake rate, a clinician stated, “If we were to focus on what would make the biggest difference, it would be having a continuity of people bringing it up so when the MA’s in the room with the patients them saying, hey has anyone asked you about the HPV vaccine or it looks like you’re due for your HPV vaccine, let’s talk about it … on the clinic side its getting hit at least once or preferably more than once so people realize this seems to be important because they keep bringing it up.” Agreeing, one mother shared her HPV vaccine experience, “He (the doctor) put in the order, and then his LVN came in. She is very good, she explained what she was going to do and it was very quick.”
Parent level
Sexual debut
All participants cited that a major challenge to vaccination is the fact that because the virus is sexually transmitted, parents are worried that receiving the HPV vaccine would encourage their children to become sexually active. While the parents interviewed did not cite sexual activity as a barrier to vaccinating their own children, they stated that it is a barrier for many parents including for their friends and family members with children. As one parent explained, “ … like I said a lot of parents think that if you get the vaccine it’s because you’re going to have sex.” A MA added, “You get it through being sexually active … They (parents) are going to say, not my child, they don’t need to be vaccinated because my child wouldn’t do that, and my child is not sexually active.” Clinicians agreed that there is “this misconception that somehow giving the vaccine is condoning sexual activities, sort of as if we are putting their kids on birth control or something … that we are expecting them to become sexually active.”
Delaying HPV vaccination
When asked if her daughter’s clinician discussed the vaccine during the visit, a mother said, “In all truthfulness, the doctor went over this with me, and as she was explaining, I was up to do it, but just not yet.” Clinicians and clinic support staff agreed that parents “usually don’t outright refuse, they will say we will not at this time,” and would request to “wait until their child is older.” As described by one clinician, “Parents feel that (the HPV vaccine) it isn’t necessary. They don’t feel like their kids need to have it … they think it’s too early, and they want to do it later.”
Media misinformation
When asked about challenges to vaccination, all participants commented that media coverage of the HPV vaccine resulted in parents receiving inaccurate or incomplete information regarding the vaccine. As explained by one parent, “I think that there was so much damage that has been done in the past with the study that correlated autism with immunization. I have to say that out of the people I have spoken with (that have children), that is the reason; because they strongly believe that there is a correlation between the two.” Another mother echoed the same sentiment, “There were a couple of articles that I read and a couple of them seem to be like severe cases … you know those things are out there so just making sure that those are being addressed so people who aren’t misinformed about it.” One clinician remarked that “when they (parents) go on the Internet, they get the wrong information. They might hear about, you know, adverse thing that may have happened, and they are scared about it … ”
Discussion
Interventions to improve HPV vaccine uptake usually focus on patients/parents or healthcare clinicians, without addressing the role of other primary care team members and organizational resources and infrastructure.Citation14,Citation16,Citation24 We conducted this study with clinicians, clinic support staff, and parents to better understand how HPV vaccination occurs at point of care. We found that there are interdependencies among people and processes that make HPV vaccination completion challenging. First, clinicians must recommend the vaccine to the patient/parent, secondly, the patient/parent needs to accept that recommendation, and lastly the clinic staff has to carry out the recommendation. Our findings show that beyond the clinician and patient/parent, organizational factors such as EMR-linked clinical decision support systems, flexible appointment times, clinic workflows and knowledgeable clinic support staff affected HPV vaccine uptake. See for a diagram of the factors and barriers related to the HPV vaccine decision-making process at the point of care. Future interventions to accelerate the uptake of the HPV vaccine should include individual, interpersonal, and organizational strategies to address these multiple levels of influences.
We found that despite the overall acceptance and support for the HPV vaccine, participants reported delayed vaccination. Consistent with other research, our study revealed that parents were not refusing vaccination, but rather wanted to delay vaccination until their child was older, and when parents voiced this desire to wait, clinicians and clinic staff did not push for same-day vaccination. In one study, providers described on time HPV vaccination as a broad spectrum, ranging from ages 12–26.Citation25 Another study found that when parents wanted to delay vaccination, clinicians agreed to wait because they did not think the adolescent was at risk for developing HPV.Citation26 Mahoney et al. reported that clinicians may be prioritizing other adolescent vaccines over the HPV vaccine because of misconceptions regarding the risk and severity of HPV infections.Citation27 Similarly, in our study, the main reason cited for delaying vaccination was that parents did not feel that their child needed to be protected against a sexually transmitted disease at their current age because they believed their child is not sexually active nor will they be sexually active soon. However, according to the 2015 Youth Risk Behavior Surveillance Survey, 41.2% of high school students reported having sexual intercourse and 30.1% reported that they were currently sexually active; thus, there may be an underestimation of teen sexual activity among parents and clinicians.Citation28 This lack of regard for timely HPV vaccination coupled with not pushing for same-day vaccination is alarming for several reasons. Older adolescents have less preventative care visits compared to younger adolescents,Citation29 thus opportunities to vaccinate them become more limited, leaving them more vulnerable to HPV infections. Additionally, not only have studies shown that younger adolescents respond better to the HPV vaccine than older adolescents and young adults,Citation30,Citation31 but they are also more cost-effective to vaccinate younger adolescents because the number of doses increases from two to three when administered at 15 years of age and older. Additionally, it appears that there is lack of knowledge among parents, clinicians, and clinic support staff on the importance of timely HPV vaccinations, hence the nonchalant attitudes toward postponing vaccination. Future research is needed to develop communication strategies that negate parental desires to delay vaccination. Educational interventions should also highlight the importance of timely HPV vaccinations. We also found a disconnect between clinician recommendation of the HPV vaccine and clinic follow-through of vaccine delivery. Clinicians reported recommending the vaccine to their patients and parents expressed high acceptance of the vaccine; however, when staff came to administer the vaccine, in some cases, the vaccine was not given. We found several explanations for this pattern. While clinic staff supported HPV vaccination, they expressed varying knowledge of HPV vaccination. Most staff indicated that they knew HPV was a virus and that the vaccine can prevent cervical cancer but were unable to go into great depth or breadth regarding other aspects of HPV and/or the vaccine (e.g., staff did not mention other cancers associated with the virus nor did they know the dosing schedules). When the staff encountered families that had follow-up HPV questions, staff were not confident in their ability to answer the families follow-up questions. Staff referred families back to their clinician and suggested vaccination at a future appointment. Staff also reported being asked about their opinion on the vaccine and many shared with parents and patients their own personal vaccination experience. This is consistent with findings from Chuang et al.,Citation16 which found uptake of the HPV vaccine to be related to multiple factors at the health care team level. Prior studies have focused on the importance of a clinician’s strong HPV vaccination recommendationCitation32,Citation33; however, clinic support staff are usually the first point of contact for families during a patient visit and they are also usually the ones who administered the HPV vaccine and as such their recommendation can reinforce or hinder that of the clinicians. Consistent with other studies, our findings also provide evidence that having a pro HPV vaccine clinic culture, where all clinic staff and clinicians are on the same page regarding vaccination, could accelerate the HPV vaccine uptake rate.Citation15,Citation16 Future interventions should consider a team-based training approach on how to offer a strong clinic HPV vaccine recommendation because staff knowledge, attitudes, and beliefs toward vaccination play major factors in whether or not vaccination occurs.
In addition to the widely cited strategies of emphasizing the message that HPV is cancer preventionCitation34,Citation35 and normalizing the vaccineCitation36,Citation37 clinicians also attributed having a strong organizational vaccine infrastructure (e.g., clinician alert, flexible clinic hours, tracking systems, etc.) as a factor that contributed to vaccination. This finding is consistent with the literature that indicates that vaccine protocols and proceduresCitation38 and practice attitudes toward vaccinationCitation39,Citation40 are clinic level factors that influence HPV vaccine uptake.
Lastly, our study findings indicate that while most parents have heard of the HPV vaccine, parents were not sufficiently primed for vaccination prior to office visits. Like the clinic support staff, all parents in our study knew the HPV vaccine prevented cervical cancer but were unaware of the other cancers associated with the virus, particularly the cancers that affected boys. Most thought that the reason boys were vaccinated was to ensure that they would not infect girls with the virus (and while this is true), many were surprised to learn about HPV-related oral, penile, and anal cancers. One mother was not aware that the vaccine was available for boys. Time constraints have been cited as a major barrier to vaccination by cliniciansCitation7 and a recommendation to abate time constraints suggested by clinicians and clinic staff was to provide education to the parents before the office visit. Clinicians can then focus their time on answering any lingering questions parents may have. However, presenting the HPV vaccine as a standard bundle for adolescent immunizations has been widely cited as an effective strategy to increase uptake of the HPV vaccine,Citation41,Citation42 thus providing parents with an educational primer that emphasized the HPV vaccine may contradict efforts to normalize the vaccine. Additionally, while there is an abundance of HPV vaccination educational materials available online to parents, there are few educational materials that introduce the vaccine as a standard bundle with other routinely recommended vaccines for adolescents. Future research should examine the effects of educational materials that bundle all recommended vaccines for adolescents, rather than having a standalone HPV educational primer.
Limitations
This study has some limitations to consider. While all the parent participants were mothers, existing literature report that mothers are the primary decision-makers when it comes to vaccinating their child against HPV.43,Citation44 Additionally, our parent participants did not include any vaccine-resistant parents; thus, the opinions and views expressed by the parents reflect those that have either had their child vaccinated against HPV or have yet to vaccinate their child (but were not opposed to vaccination). We also interviewed a small number of participants that were all recruited from a single health system; thus, results may not be generalizable to all groups and healthcare settings. However, while there is limited variation in organizational infrastructure in the network, the primary care clinics serve a diverse population including patients with varying health insurance plans (e.g., Medi-Cal-California’s Medicaid Program, Cover California-California’s health insurance marketplace, major health plans); has a broad geographic scope (three counties); and the clinics vary in terms of their number of adolescent patients served. As such we were able to elicit broad and diverse responses from participants on the mechanisms involved in a clinician’s HPV vaccine recommendation, parental acceptance of that recommendation and clinic follow-up to ensure that the vaccination occurs.
Conclusion
HPV vaccine uptake is a complex process that is interdependent on multiple levels of influences. By examining the HPV vaccine uptake process at the point of care, several factors that can help explain low HPV vaccination rates and strategies to accelerate HPV vaccine uptake were identified. Our results underscore the interrelationships among the various stakeholders as well as the processes involved in the decision and follow-through of HPV vaccination. Study findings confirm that in addition to clinician recommendation and communication with parents, organizational and primary team factors can also affect HPV vaccine uptake. Clinic support staffs’ HPV vaccine knowledge, attitudes, and beliefs can hinder or strengthen the recommendation of the clinician. Clinic-wide HPV vaccination training may help align interests so that clinic support staff and clinicians are giving the same consistent timely message around HPV vaccination to all families. Interventions to accelerate HPV vaccine uptake should include integrative methods and strategies at the parent, primary care team (e.g., clinician, clinic support staff), and practice setting levels.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We thank-you to Drs. Joan R. Bloom and Mahasin S. Mujahid for their review of drafts of this article. We would also like to thank the University of California Davis Health Primary Care Network staff, clinicians, and parents for their participation in the study and Duke LeTran, Kim Nguyen, and Catrina Franco for assisting with conducting the interviews, transcriptions, and for coding.
Additional information
Funding
References
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, Su J, Xu F, Weinstock H. Sexually transmitted infections among US women and men. Sex Transm Dis. 2013;40(3):187–93. doi:10.1097/olq.0b013e318286bb53.
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68:698–702. doi:10.15585/mmwr.mm6832a3externalicon.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination — updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2016;65(49):1405–08. doi:10.15585/mmwr.mm6549a5.
- Senkomago V, Henley SJ, ThomTias CC, Mix JM, Markowitz LE, Saraiya M. Human papillomavirus–attributable cancers — United States, 2012–2016. MMWR Morb Mortal Wkly Rep. 2019;68:724–28. doi:10.15585/mmwr.mm6833a3.
- Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Fredua B, Singleton JA, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68:718–23. doi:10.15585/mmwr.mm6833a2.
- Bratic JS, Seyferth ER, Bocchini JA. Update on barriers to human papillomavirus vaccination and effective strategies to promote vaccine acceptance. Curr Opin Pediatr. 2016;28(3):407–12. doi:10.1097/mop.0000000000000353.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents. JAMA Pediatr. 2014;168(1):76. doi:10.1001/jamapediatrics.2013.2752.
- Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine. 2012;30(24):3546–56. doi:10.1016/j.vaccine.2012.03.063.
- Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Prev Med. 2017;95:26–37. doi:10.1016/j.ypmed.2016.11.019.
- Loke AY, Kwan ML, Wong Y, Wong AK. The uptake of human Papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8(4):349–62. doi:10.1177/2150131917742299.
- U.S. Department of health and human services. Healthy people 2020. Immunization and infectious diseases. [accessed 2019 Jul 24]. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
- Garbutt JM, Dodd S, Walling E, Lee AA, Kulka K, Lobb R. Barriers and facilitators to HPV vaccination in primary care practices: a mixed methods study using the consolidated framework for implementation research. BMC Fam Pract. 2018;19:1. doi:10.1186/s12875-018-0750-5.
- Lake PW, Kasting ML, Christy SM, Vadaparampil ST. Provider perspectives on multilevel barriers to HPV vaccination. Hum Vaccin Immunother. 2019:1–10. doi:10.1080/21645515.2019.1581554.
- Fernández ME, Allen JD, Mistry R, Kahn JA. Integrating clinical, community, and policy perspectives on human papillomavirus vaccination. Annu Rev Public Health. 2010;31(1):235–52. doi:10.1146/annurev.publhealth.012809.103609.
- Hudson SM, Rondinelli J, Glenn BA, Preciado M, Chao C. Human papillomavirus vaccine series completion: qualitative information from providers within an integrated healthcare organization. Vaccine. 2016;34(30):3515–21. doi:10.1016/j.vaccine.2016.02.066.
- Chuang E, Cabrera C, Mak S, Glenn B, Hochman M, Bastani R. Primary care team- and clinic level factors affecting HPV vaccine uptake. Vaccine. 2017;35(35):4540–47. doi:10.1016/j.vaccine.2017.07.028.
- Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998–2011. GMS Psycho Social Med. 2012;9:Doc11. doi:10.3205/psm000089.
- Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics. 2006;117(5):1486–93. doi:10.1542/peds.2005-1381.
- Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr. 2011;11(1):74. doi:10.1186/1471-2431-11-74.
- Kessels SJM, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine. 2012;30:3546–56. doi:10.1016/j.vaccine.2012.03.063.
- Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Babbel C, Kempe A, Dunne EF, Stokley S, Dickinson LM. A national survey of pediatrician knowledge and attitudes regarding human papillomavirus vaccination. Pediatrics. 2006;118(6):2280–89. doi:10.1542/peds.2006-1946.
- Tiro JA, Pruitt SL, Bruce CM, Persaud D, Lau M, Vernon SW, Skinner CS. Multilevel correlates for human papillomavirus vaccination of adolescent girls attending safety net clinics. Vaccine. 2012;30(13):2368–75. doi:10.1016/j.vaccine.2011.11.031.
- Dedoose Version 8.0.35. web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles (CA): SocioCultural Research Consultants, LLC; 2018.
- Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Hum Vaccin Immunother. 2016;12(6):1566–88. doi:10.1080/21645515.2015.1125055.
- Henrikson NB, Tuzzio L, Gilkey MB, McRee A. “You’re never really off time”: healthcare providers’ interpretations of optimal timing for HPV vaccination. Preventive Med Rep. 2016;4:94–97. doi:10.1016/j.pmedr.2016.05.002.
- Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr. 2011;11:1. doi:10.1186/1471-2431-11-74.
- Mahoney MC, Saad-Harfouche FG, Widman CA, Twarozek AM, Erwin DO, Rodriguez EM. Clinician misperceptions about the importance of adolescent HPV vaccination. World J Vaccines. 2016;6:1. doi:10.4236/wjv.2016.61002.
- Kann L, Olsen EO, McManus T, Harris WA, Shanklin SL, Flint KH, Lowry R, Chyen D, Whittle L, Thornton J, et al. Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12 — United States and selected sites, 2015. MMWR Surveillance Summaries. 2016;65(9):1–202. doi:10.15585/mmwr.ss6509a1.
- Rand CM, Shone LP, Albertin C, Auinger P, Klein JD, Szilagyi PG. National health care visit patterns of adolescents. Arch Pediatr Adolesc Med. 2007;161(3):252. doi:10.1001/archpedi.161.3.252.
- Block SL, Nolan T, Sattler C, Barr E, Giacoletti KE, Marchant CD, Castellsague X, Rusche SA, Lukac S, Bryan JT. Comparison of the immunogenicity and reactogenicity of a prophylactic quadrivalent human papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in male and female adolescents and young adult women. Pediatrics. 2006;118(5):2135–45. doi:10.1542/peds.2006-0461.
- Reisinger KS, Block SL, Lazcano-Ponce E, Samakoses R, Esser MT, Erick J, Puchalski D, Giacoletti KED, Sings HL, Lukac S, et al. Safety and persistent immunogenicity of a quadrivalent human papillomavirus types 6, 11, 16, 18 L1 virus-like particle vaccine in preadolescents and adolescents. Pediatr Infect Dis J. 2007;26(3):201–09. doi:10.1097/01.inf.0000253970.29190.5a.
- Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–92. doi:10.1016/j.vaccine.2016.01.023.
- Gilkey MB, McRee A. Provider communication about HPV vaccination: A systematic review. Hum Vaccin Immunother. 2016;12(6):1454–68. doi:10.1080/21645515.2015.1129090.
- Malo TL, Gilkey MB, Hall ME, Shah PD, Brewer NT. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol Biomarker Prev. 2016;25(10):1383–91. doi:10.1158/1055-9965.epi-16-0224.
- Krantz L, Ollberding NJ, Beck AF, Carol Burkhardt M. Increasing HPV vaccination coverage through provider-based interventions. Clin Pediatr (Phila). 2017;57(3):319–26. doi:10.1177/0009922817722014.
- Farmar AM, Love-Osborne K, Chichester K, Breslin K, Bronkan K, Hambidge SJ. Achieving high adolescent HPV vaccination coverage. Pediatrics. 2016;138(5):e20152653. doi:10.1542/peds.2015-2653.
- Shay LA, Street RL, Baldwin AS, Marks EG, Lee SC, Higashi RT, Skinner CS, Fuller S, Persaud D, Tiro JA; Shay LA, Street RL, Baldwin AS, Marks EG, Lee SC, Higashi RT, et al. Characterizing safety-net providers’ HPV vaccine recommendations to undecided parents: A pilot study. Patient Educ Couns. 2016;99(9):1452–60. doi:10.1016/j.pec.2016.06.027.
- Szilagyi PG, Rand CM, McLaurin J, Tan L, Britto M, Francis A, Dunne E, Rickert D. Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 2008;121(Supplement 1):S15–S24. doi:10.1542/peds.2007-1115c.
- Tiro JA, Sanders JM, Pruitt SL, Stevens CF, Skinner CS, Bishop WP, Persaud D, Persaud D. Promoting HPV vaccination in safety-net clinics: a randomized trial. Pediatrics. 2015;136(5):850–59. doi:10.1542/peds.2015-1563.
- Farmar AL, Love-Osborne K, Chichester K, Breslin K, Bronkan K, Hambidge SJ. Achieving high adolescent HPV vaccination coverage. Pediatrics. 2016 Nov 1;138(5):e20152653. doi:10.1542/peds.2015-2653.
- Bailey HH, Chuang LT, DuPont NC, Eng C, Foxhall LE, Merrill JK, Wollins DS, Blanke CD. American society of clinical oncology statement: human papillomavirus vaccination for cancer prevention. J Clin Oncol. 2016 Apr 11;34(15):1803–12. doi:10.1200/JCO.2016.67.2014.
- Conroy K, Rosenthal SL, Zimet GD, Jin Y, Bernstein DI, Glynn S, Kahn JA. Human papillomavirus vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination. J Women Health. 2009;18(10):1679–86. doi:10.1089/jwh.2008.1329.
- Allen JD, De Jesus M, Mars D, Tom L, Cloutier L, Shelton RC. Decision-making about the HPV vaccine among ethnically diverse parents: implications for health communications. J Oncol. 2012;(2012:1–5. doi:10.1155/2012/401979.
- Berenson AB, Laz TH, Hirth JM, McGrath CJ, Rahman M. Effect of the decision-making process in the family on HPV vaccination rates among adolescents 9–17 years of age. Hum Vaccin Immunother. 2014;10(7):1807–11. doi:10.4161/hv.28779.