ABSTRACT
Introduction
The level of vaccination coverage with obligatory preparations in Poland reaches 98%. This is facilitated by the introduction of the Individual Vaccination Calendar (IVC) compliant with medical contraindications to vaccination.
Aim
The aim of the study was to assess whether the refusal of vaccinations after birth has an impact on the proper implementation of the vaccination calendar in the first year of life.
Methods
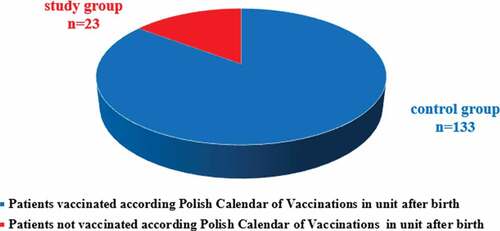
The study involved healthy, term newborns who were born in the Department of Neonatology in 2011–2015. There were 156 patients enrolled to the study. Among them, 133 were in the control group – vaccinated after birth, and 23 constituted the study group – not vaccinated after birth.
Results
Not all healthy newborns are vaccinated after birth, statistical significance was obtained between the study and control group (p < 0,00001).
Only 48% of patients not vaccinated after birth received TB-vaccine during the first year (p < 0,00053).
Parents of 26% of infants in the study and of 2% of infants in the control group declared using the IVC (p < 0,001).
Conclusions
Proper implementation of the vaccination schedule in the first year of life results from the initiation of vaccinations after birth.
Unreasonable introduction of the IVC promotes incorrect timing of mandatory vaccinations.
Introduction
The level of vaccination coverage with obligatory preparations in Poland reaches 96–98%Citation1. The high percentage of persons immunized against infectious diseases results from the proper implementation of the vaccination schedule (VS). Proper observance of indications and contraindications to vaccination is aimed at protecting the entire population: protection of the vaccinated person (individual immunity), as well as people who cannot receive all vaccinations (community resistance).Citation2 This is facilitated by the introduction of the Individual Vaccination Calendar (IVC) among chronically ill patients. Recent scientific reports show that improper implementation of the VS does not result from medical contraindications to vaccination but from parental decisions. Therefore, an attempt was made to assess the impact of parental decisions on vaccinations with regard to the implementation of the vaccination calendar.
Aim
The aim of the study was to assess whether the refusal of vaccinations after birth has an impact on the proper implementation of the vaccination calendar in the first year of life.
Material and method
The study included healthy, full-term newborns, born in the Neonatology Clinic of the University Hospital in Wrocław from January 2011 to December 2014.
A positive opinion of the Bioethical Committee at the Medical University in Wrocław for the conducted research (opinion no: KB-753/2012 of 25.10.2015) has been obtained.
Groups of patients were created based on the assessment of the general condition, clinical examination of newborns, the medical history obtained, vaccination qualifications according to the current communication of the Chief Sanitary Inspector regarding the Protective Vaccination Program () for a given year and the conducted questionnaire survey. The patient qualification process verified the socio-economic data concerning their parents, the course of pregnancy and delivery, the manner of termination of pregnancy as well as anthropometric data of newborns. On the basis of the sex-specific Fenton growth chartCitation3 for a given fetal age, eutrophic newborns were separated to be included in the study.
Table 1. Polish Calendar of Vaccinations in the first year of life (mandatory, refundable vaccinations)
The control group consists of randomly selected patients who meet the inclusion criteria () and are vaccinated with refunded vaccines in the first days of life. Parents provided their written consent to vaccinate the child in the neonatal unit. Refundable preparations are vaccines purchased from the state budget. There are two vaccines in the first day of life: vaccine against tuberculosis (BCG) and the first dose of hepatitis B vaccine (HBV). Nonrefundable preparation is vaccines purchased by parents, e.g., hepatitis B vaccine different firms or optional vaccines.
Table 2. Including and excluding criteria of patients for the study
The control group is composed of patients meeting the inclusion criteria, not vaccinated after birth at all, despite the lack of contraindications. The parents did not agree in writing to vaccinate the child in the neonatal unit. These newborns did not receive BCG or HBV in the unit after birth.
The study was carried out in 2011–2015. A total of 428 patients fulfilling the inclusion criteria took part, whilst. Finally, after one year, 156 patients qualified for the study.
The control group consisted of patients (133 newborns), who were vaccinated according to their Vaccination Calendar shortly after birth.
The study group consisted of patients (23 newborns), who were not vaccinated against tuberculosis or hepatitis B after birth.
The division of patients into groups is presented in .
Parental participation consisted in completing the questionnaire immediately after giving birth (Questionnaire regarding vaccinations of a healthy full-term newborn after birth – Annex 1) and a year after the birth of the child (Questionnaire regarding vaccinations after the child’s first year of life – Annex 2). The survey was conducted mainly with the mother during the hospitalization in the maternity unit. However, the survey after one year was carried out with the parents during their visit to the Neonatal Outpatient Clinic, after a telephone appointment or by telephone contact. The conversation with the parents was preceded by a physical examination of the patient.
The postnatal questionnaire (Annex 1) contained questions concerning the reasons for parents’ withdrawal from vaccination and sources of information on vaccination. In the survey after one year, the implementation of the vaccination calendar was analyzed (Annex 2) i.e., whether the vaccinations initiated during the hospitalization after birth were continued in accordance with the calendar, also in terms of timeliness, as well as whether and which vaccine was administered in those who did not receive post-natal vaccination. Lack of vaccination of the patient in the first year of life with obligatory vaccines was understood as the improper implementation of the vaccination calendar. Questions were asked regarding the child’s development and its clinical status, chronic diseases, which could constitute medical contraindications for vaccination, in the context of the withdrawal from vaccination. The timeliness of the vaccinations performed was analyzed along with the issue whether their possible postponement took place for medical reasons. If the Individual Vaccination Calendar was used, the reasons for its introduction were evaluated (the child’s condition), including the verification of their legitimacy in terms of medical reasons. The evaluation of obligatory and recommended vaccinations in the first year of life as well as the use of highly combined vaccines were assessed. The next questions concerned the sources of information on vaccination, as in the first questionnaire.
The results of the obtained tests were subjected to statistical analysis. In groups with heterogeneous variances, the nonparametric test of the Kruskal–Wallis rank sum was used, where the homogeneity of variance was checked using the Bartlett test. The χ2df test with Yates correction and the appropriate number of degrees of freedom were used to calculate the frequency of occurrences of discrete parameters in the studied groups. Statistical analysis was carried out using the package of computer statistical program EPIINFO version 7.1.1.14 (of July 2, 2013).
Results
Implementation of the vaccination calendar
The parents of healthy full-born infants refuse to start vaccinations at the neonatal unit, even in the absence of contraindications (p < 0,00001).
Not all healthy full-born newborns receive the vaccination against hepatitis B with reimbursed formulas in the neonatal unit (p < 0,00001).
On the basis of the data obtained after one year, the correct implementation of the calendar of protective vaccinations of the examined patients, as well as the timeliness of their performance and the legitimacy of postponing vaccinations in the first year of life were analyzed.
In the control group, the preventive vaccination schedule was implemented in all, i.e., 133, patients (100%) in comparison to the study group, where the vaccination schedule was correctly performed in 17 patients who accounted for 74% of this group (p < 0,00001). As a result, the vaccination calendar was not carried out in the first year of life in six patients, constituting 26% of the study group ().
Table 3. Complementation of the vaccination schedule in the study and control group, timing performance of vaccinations, and the validity of avoiding immunization
Of the 23 patients not vaccinated against tuberculosis after birth, 11 (48%) received vaccination (p < 0,00053) during the first year of life, which means that more than half of neonates who were not vaccinated against tuberculosis in the neonatal unit (12 patients, 52%) did not receive this vaccination in the first year of life! ().
Table 4. The implementation of vaccination in the first year of life in both groups in compared with the current Polish Calendar of Vaccination
The relative risk of not vaccinating an infant against tuberculosis in the first year of life is 2,09 if the child does not receive this vaccination in the neonatal unit (Rr2-23 = 0; Rr1-20 = 2,09 CI 1,36–3,20; Rr1-23 = 0,478 CI 0,312–0,733; Rr2-20 = 0).
Of the 22 patients not vaccinated against Hepatitis B at birth, 59% (p < 0,00349) received the vaccination in the first year of life, meaning that as many as 41% of patients not vaccinated in the neonatal unit did not receive this vaccination in their first year of life. The relative risk of not vaccinating an infant against hepatitis B in the first year of life is 0.591 times greater if the child does not receive this vaccination in the neonatal unit (Rr1-22 = 0,591 CI 0,417–0,837).
The vaccination of patients from the study group against diphtheria, pertussis, tetanus, polio, and Haemophilus influenza type b was performed in the first year of life in 61% of cases. Among the members of this group, 39% were not immune to the above-mentioned diseases (p < 0,00001). The implementation of vaccination in the first year in both groups is shown in .
Table 5. Sources of information about vaccinations in both groups
Timeliness of vaccination ()
Avoiding immunization concerned situations in which patients did not receive vaccinations according to the current vaccination calendar (). It was analyzed whether postponement in vaccination occurred on medical reasons (justified) or not (unjustified).
Postponement of vaccination in the first year of life in the control group took place in 14% of patients, only 4% of which were justified (p < 0,00001) .
Postponement of vaccination in the first year of life in the study group took place in 100% of patients, only 4% of which were justified (p = 0,892).
Unjustified postponement of vaccination took place in 14% of the population surveyed.
Parents of 26% of infants in the study group declared using the Individual Vaccination Calendar.
Parents of 2% of infants in the control group declared using the Individual Vaccination Calendar.
For these data, statistical significance was obtained: p < 0,001; OR = 0,04 (CI 95,0% 0,01–0,23).
The comparison of results obtained after one year in both groups is presented in .
In the control group, 5% of patients are chronically ill. In the study group, there are no chronically ill patients and 4,5% of patients have an Individual Vaccination Calendar. It was statistically significant that the possible siblings of the patient from the control group would be vaccinated less often in the future in comparison to the siblings of the patient in the control group ().
Patients from the control and study group live in the environment of vaccinated people, where both parents and relatives were vaccinated in the past (p < 0,001).
There is a statistically significant difference between the study and control groups in the distribution of information about vaccinations from the doctor (p = 0,002) and from the media (p < 0,001) in the child’s first year of life ().
Medical staff are the main source of information on vaccination in the control group in the first year of life (p = 0,002).
Parents of vaccinated children more often used information from the doctor than parents of unvaccinated children (72% vs. 39%).
The psychomotor development of all patients was normal. The clinical condition of the patients was good. One of the examined patients from the control group had congenital immunodeficiency, autism, VSD, and WPW.
Due to the lack of response from all respondents, the question concerning infections was excluded.
Discussion
Anti-vaccine attitudes
In the study at the Department of Neonatology in 2011–2015, it was shown that not all healthy, full-term newborns receive vaccinations in the neonatal unit after birth (p < 0,00001). Unjustified postponement of vaccinations results from parental decision. In English-language literature, the term “vaccine hesitancy” is used to characterize people who accept vaccination but have significant concerns about it.Citation4 The concept of “vaccine-hesitant parents” (VHPs) was coined in a similar way, describing a diverse group of parents presenting different attitudes to vaccination, beliefs, preferences regarding the immunization schedule, and its implementation.Citation5
The authors categorized VHPs in various ways. The criterion for the division is based on the degree of implementation of the current vaccination program of the child: full implementation of the vaccination program, selective implementation, delayed vaccination schedule, lack of implementation of the vaccination schedule. Guts et al.Citation6 divided the population of undecided parents into five subgroups: proponents of vaccination, willing to communicate, health advocates, concerned caregivers, the worried. Keane et al.Citation7 proposed the division into the believers in vaccination, the doubtful, the indifferent, and unconvinced. The four-group division was also adopted by Benin et al.Citation8 acceptors, those undecided, delaying, refusing. In turn, Gowda et al.Citation9 carried out a questionnaire, verifying the parents’ levels of indecisiveness in the context of the implementation of future vaccinations. Leask et al.Citation10 proposed a division including a group of parents as follows: absolute acceptors, careful acceptors, undecided, selective or delaying vaccinations, and refusing. It is worth emphasizing that VHPs include parents who have doubts about vaccination but still use it.Citation4 After the analysis of the divisions, a similar trend of the variant with similar terminology was found.
Attempts to characterize a group of parents questioning the legitimacy of vaccination of children are aimed at defining a specific group of people, with regard to whom specific actions should be undertaken to convince them to vaccinate their children. The authors distinguish data on the immune system, communication, and information (socio-economic) family characteristics as well as parents’ attitudes and the level of their knowledge. Factors affecting the attitudes of improper implementation of the vaccination schedule are higher education, lower socioeconomic status, limited knowledge of health workers.Citation11
The character of the group of undecided parents is reflected in the search for knowledge about vaccination. Because VHPs want to be co-deciding about the health of the child, they reach for the available sources of information about vaccinations. In co-deciding on the use of vaccine in their child, parents want to maintain some control over their child’s health.
The success of the prevention of infectious diseases is based on:
The development of effective immunization.
Relevant vaccination schedules and their distribution to the public.
Monitoring of the safety of vaccinations by reporting vaccine injury (VI)
Public acceptance of the proposed VS.Citation12
A disturbance in any of the elements interferes with the process of effective infection prevention.
Conclusions
Proper implementation of the vaccination calendar in the first year of life results from the initiation of vaccination administration after birth
Unjustified introduction of the Individual Vaccination Calendar promotes the incorrect implementation of mandatory vaccinations and delay of immunization.
Disclosure of potential conflict of interest
We declare no conflict of interest. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
We would like to thank Robin and Barbara ROYLE for their help in the language correction of the text.
Additional information
Funding
References
- Jaroszewska K, Marciniak A, Gałwak M, Życińska K, Wardyn K, Nitsch-Osuch A. Perception of anti-vaccination movements by parents of young children. Post N Med. 2014;27:617–21.
- Bernatowska E. Immune system diseases and protective vaccinations. In: Kawalec W, Grenda H, Ziółkowska H editors. Pediatrics. Vol. 2. Warsow (PL): PZLW; 2011. p. 1048–79.
- Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013 Apr 20;13:59. doi:10.1186/1471-2431-13-59. PMID: 23601190.
- Bernatowska EA, Wolsk-Kuśnierz B, Kurenko-Deptuch M, Zwolska Z, Casanova J-L, Piatosa B, Dongen J, Roszkowski K, Mikoluc B, et al. Disseminated bacillus calmette-guerin infection and immunodeficiency. Emerg Infect Dis. 2007;5:179–801. PMID: 18044052. doi:10.3201/eid1305.060865.
- Gowda C, Dempsey A. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013;9:1755–62. PMID: 23744504. doi:10.4161/hv.25085.
- Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization attitudes and beliefs among parents: beyond a dichotomous perspective. Am J Health Behav. 2005;29(1):81–92. doi:10.5993/ajhb.29.1.7. PMID: 15604052
- Keane MT, Walter MV, Patel BI, Moorthy S, Stevens RB, Bradley KM, Buford JF, Anderson EL, Anderson LP, Tibbals K, et al. Confidence in vaccination: a parental model. Vaccine. 2005;23:2486–93. [online]. doi: 10.1016/j.vaccine.2004.10.026. PMID: 15752835. doi:. .
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–41. doi:10.1542/peds.2005-1728. PMID: 16651306
- Gowda C, Schaffer SE, Kopec K, Markel A, Dempsey AF. Dose the relative importance of MMR vaccine concerns differ by degree of parental vaccine hesitancy?: an exploratory study. Hum Vaccin Immunother. 2013;9:430–36. PMID: 23032161. doi:10.4161/hv.22065.
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communication with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012;12:154–61. PMID: 22998654. doi:10.1186/1471-2431-12-154.
- Rainey JA, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999-2009. Vaccine. 2011;29(46):8215–21. doi:10.1016/j.vaccine.2011.08.096. PMID: 21893149
- Velan B. Acceptance on the move: public reaction to shifting vaccination realities. Human Vaccines. 2011;7(12):1261–70. doi:10.4161/hv.7.12.17980. PMID: 22108039
Annex 1.
QUESTIONNAIRE REGARDING VACCINATIONS OF A HEALTHY FULL-TERM NEWBORN AFTER BIRTH
1. Do you agree to carry out a questionnaire regarding vaccinations of a healthy full-term newborn after birth YES □ NO □
2. Do you agree to vaccinate your child in the first day of life according to the current vaccination schedule against tuberculosis? YES □ NO □
3. Do you agree to vaccinate your child in the first day of life according to the current vaccination calendar against hepatitis B vaccine available in the hospital? YES □ NO □
4. Do you agree to vaccinate your child in the first day of life according to the current hepatitis B vaccination calendar with your own vaccine? YES □ NO □
5. Do you agree to vaccinate your child with your own vaccine because of the composition (e.g., thimerosal) of the vaccine proposed in the hospital? YES □ NO □
6. Have you decided not to vaccinate your child due to fear of compromising your child’s immune system? YES □ NO □
7. Have you decided not to vaccinate your child because of fear of side effects of the vaccine’s additional ingredients? YES □ NO □
8. Have you decided not to vaccinate your child because of fear that your child will have autism? YES □ NO □
9. Will you agree to vaccinate your child according to the current vaccination calendar over 6 months old?YES □ NO □
10. Will you never consent to vaccinate your child? YES □ NO □
11. Did you get information about vaccinations from the internet? YES □ NO □
12. Did you get information about vaccinations from another patient?YES □ NO □
13. Did you get information about vaccinations from your doctor?YES □ NO □
14. Will you agree to carry out a similar survey in 12 months regarding your child’s vaccination in the first year of life?YES □ NO □
Medical history number: Mother’s age:
Gestational age: Apgar score:
Birth weight: Mother’s education:
Annex 2:
QUESTIONNAIRE REGARDING VACCINATIONS AFTER THE CHILD’S FIRST YEAR OF LIFE
1. Do you agree to the questionnaire regarding your child’s vaccinations in the first year of life? YES □ NO □
2. Has your child been vaccinated against tuberculosis? YES □ NO □
3. Has your child been vaccinated against hepatitis B? YES □ NO □
4. Was your child vaccinated with whole-cell vaccine against diphtheria, tetanus, and pertussis at 2 months of life? YES □ NO □
5. Was your child vaccinated with an acellular vaccine against diphtheria, tetanus, and pertussis at 2 months of life? YES □ NO □
6. Was your child vaccinated against Haemophilus influenzae type b invasive infection at 2 months of life? YES □ NO □
7. Was your child vaccinated against poliomyelitis at 3 months of life? YES □ NO □
8. Has your child received combined/booster vaccinations (which one)? YES □ NO □
9. Will your child receive the next compulsory vaccinations according to the current vaccination schedule? YES □ NO □
10. Did you decide to vaccinate your child due to information obtained from the media? YES □ NO □
11. Did you decide to vaccinate your child because of information from friends? YES □ NO □
12. Did you decide to vaccinate your child because of information obtained from medical staff? YES □ NO □
13. Has your child ever had any side effects as a result of the vaccinations? YES □ NO □
14. Have vaccinations been postponed due to your child’s clinical condition? YES □ NO □
15. Will you never consent to vaccinate your child? YES □ NO □
16. In the first half of life, did your child often get sick due to an infection (≥4 times a year)? YES □ NO □
17. Have you had any allergies in your child’s first half of life? YES □ NO □
18. Does the child live in the environment of people vaccinated against the above-mentioned diseases? YES □ NO □
19. Will any future offspring be vaccinated in the future? YES □ NO □
20. Is the baby breastfed? YES □ NO □
21. Is the baby fed artificial milk? YES □ NO □