ABSTRACT
Background: Diphtheria-tetanus-pertussis (DTP) vaccine has already been involved in national vaccination program for several decades in China. The immunity against these diseases in the people of all ages is not well investigated.
Materials and methods: Serum samples were tested for IgG antibodies to diphtheria toxoid (DT), tetanus toxoid (TT) and pertussis toxin (PT) by using commercial ELISA kits.
Results: A total of 666 sera of patients from 1 day to 89 years of age was collected from 2018 to 2019. The protective rates of diphtheria, tetanus and pertussis were 45.5%, 54.4% and 4.7%, respectively. Only 4.7% of the study population had seropositivity against three of the diseases. Young infant (<3 m) and adult (>18y) were generally lack of protective antibody against diphtheria (81.7% and 58.3%) and tetanus (91.5% and 86.2%). An obvious increase in immunity level of diphtheria and tetanus was observed at 3 m-3y, but there was no significant increase of immunity to pertussis at any age group. All age groups showed low immunity to pertussis.
Conclusions: The present results revealed the susceptibility to diphtheria and tetanus in young infants and adults, and the susceptibility to pertussis over the ages, which highlight the need to improve the current vaccination program.
Introduction
Vaccination is the most important method to control and prevent childhood infections. A large part of the reduction in childhood mortality is attributed to the successful prevention of infectious diseases.Citation1Diphtheria, tetanus and pertussis are vaccine-preventable diseases. The main vaccines used in the prevention of diphtheria, tetanus and pertussis are diphtheria toxoid and tetanus toxoid combined with either whole-cell pertussis (DTwP) or acellular pertussis (DTaP).Citation1
In China, DTwP vaccine was introduced in 1978, and was replaced by DTaP in early 2007. Both DTaP and DTwP were used during 2007–2012, and only DTaP was administered since 2013. Primary vaccination of infants and young children consists of three doses of DTP (DTwP or DTaP) in the third, fourth and fifth months of life followed by a fourth dose at 18–24 months, with tetanus-diphtheria vaccine (Td) booster doses being recommended at 4–6 years.Citation2The first generation of children receiving DTP as their primary vaccination is now aged around 40 years. Additionally, there is neither maternal immunization nor booster vaccinations against diphtheria, tetanus and pertussis used in teenagers and adults in China. According to official estimates, since 2002 the vaccination coverage rate achieved with three doses of the DTP vaccination in childhood has been more than 90%. In 2011 the vaccination coverage of four doses was over 99%.Citation1 The incidence of whooping cough decreased to less than 1 per 100,000 since 1990. No case of diphtheria has been reported in China since 2006. The incidence of neonatal tetanus in China has also dramatically decreased from 1585 cases per 100,000 population in 2000 to 52 cases per 100,000 population in 2018. However, the number of pertussis cases has increased in recent years according to reports from the Chinese Center for Disease Control and Prevention (ChinaCDC), and some serological or molecular studies indicated that pertussis remains a serious disease in Chinese children and the disease burden is underestimated significantly.Citation3–6 Tetanus after trauma is the main type of non-neonatal tetanus in China and there are serious misdiagnosis and missed diagnosis of non-neonatal tetanus, leading to the underestimation of the incidence of non-neonatal tetanus.Citation7 Additionally, a recent series of scandals involving DTaP vaccines in China are affecting confidence in the country’s vaccination management system.Citation8
The serosurveillance, which measures immunity that results from vaccination or past infection, is a very useful investigation for the need for public health interventions.Citation1In recent years, serosurveillance of diseases prevented by DTP in some part of China has been published,Citation4,Citation9,Citation10 but there are few serological studies covering all age groups, and on the people living in undeveloped regions. The present cross-sectional study investigated antibodies specific for DTP vaccination of the people in all age groups and living in the Youyang county located in the southwestern mountain area of China, in order to gain an insight into the immunity level against these three diseases.
Materials and methods
Serum samples
The rest serum samples were collected randomly and continuously from patients in the clinical lab of Youyang Hospital from 2018 to 2019, after the clinical testing requirements finished. For this collection, 50 to 100 samples were required for each of the seven age groups: <3 months, 3-<18 months, 18 months-<3 years, 3-<6 years, 6-<18 years, 18-<40 years 40-<50 years 50-<60 years and 60≥ years. All serum samples were frozen at −60C for further test. Demographic information including age, sex, date of sampling, current residence (urban or rural) and clinical diagnosis was recorded. Cases with clinical diagnosis of pertussis, clinically suspected pertussis and immune-related diseases were not enrolled. The patients’ name, ID number, residential address and contact information were not collected for this study. The exemption from informed consent for study was approved by the ethics committee of Youyang Hospital.
Serological testing
Antibodies to diphtheria toxoid (DT), tetanus toxoid (TT) and pertussis toxin (PT) were determined by using commercially available ELISA kit (Serion, Germany). The antibody results were expressed in international units per milliliter (IU/ml).
Cutoff values
Results were evaluated with regard to protection levels, seropositivity and booster vaccine indication according to cutoff values, as recommended by the manufacturersCitation11 and previous studies:Citation3,Citation9,Citation12–14
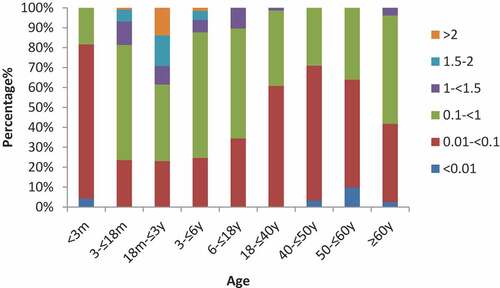
For diphtheria: <0.01 IU/ml (undetectable), 0.01–<0.1 IU/ml (no protection), 0.1–1.0 IU/ml (short term protection), >1.0–1.5 IU/ml (long term protection/booster after 5 years), >1.5–2.0 IU/ml (long term protection/booster after 7 years), >2.0 IU/ml (long term protection/booster after 10 years).
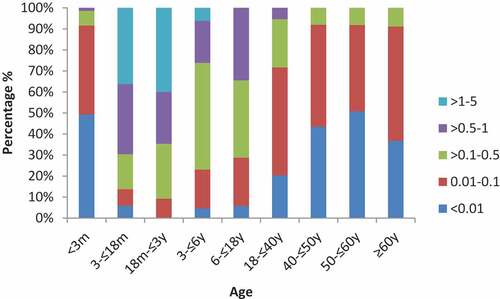
For tetanus: <0.01 IU/ml (undetectable), 0.01–0.1 IU/ml (no protection), >0.1–0.5 IU/ml (short-term protection), >0.5–1.0 IU/ml (long-term protection/booster after 3 years), >1.0–5.0 IU/ml (long-term protection/booster after5 years), >5.0 IU/ml (long-term protection/booster after 8 years)
For pertussis: <5 IU/ml (undetectable), 5–<40 IU/ml (seronegative), 40–<100 IU/ml (equivocal), >100 IU/ml (indicates an acute infection or recent vaccination/seropositive)
Data analysis
For statistical analysis, antibody concentrations below the lower limit for quantitation were assigned as half the lower limit of quantitation (0.005 IU/ml for DT and TT, and 2.5IU/ml for PT). Data were analyzed using the GraphPad Prism 5 and JMP 11. A chi-squared test (χ2) was used to compare proportions of subjects with protective antibody levels among different subgroups. A P value <.05 was considered statistically significant.
Results
Characteristics of study population
A total of 666 subjects were enrolled in the study with the age range of 1 day to 89 y. The males/females ratio was 1.32 (379/287). Vaccination history was known in 163 subjects aged 3 m-3y, and the rate of at least one dose of DTP vaccination was 98.8% (161/163). One hundred and five subjects within all age groups had diagnosed with respiratory infection, among them, 44 cases had a history of coughing ≥2 weeks.
Seroprevalence of anti-DT IgG
Of the 666 subjects tested, a total of 304 (45.6%) subjects lacked protection (<0.1 IU/ml), 297 (44.6%) subjects had short-term protection (0.1–1.0 IU/ml), and 65 (9.8%) of them showed long-term protection (>1.0 IU/ml). The overall protective rate of anti-DT IgG (≥0.1 IU/ml) was 54.4%. The lowest protective rates were observed in subjects <3 m(18.3%), and the highest protective rate of anti-DT IgG (76.9%) and proportion with long-term protection (38.5%) were observed in children aged 18 m- <3 y, and then the proportion of protective level declined with age to 29.0% among those aged 40–50 years. In subjects aged 40 years and over, protective rate increased slightly with age to 58.2% in > 60 years age group (). More than half (58.3%,161/276) of adults (>18y) were lack of protective antibody against There was significant difference in protective rates between the age groups or the gender groups, but not between the groups from different residence places ().
Table 1. Summarizes the proportion of protective antibody of pertussis, diphtheria and tetanus antibodies among subjects by age group, gender, and residence place group
Seroprevalence of anti-TT IgG
For anti-Ttx IgG, a total of 151 (22.7%) subjects had anti-Ttx IgG below the lower limit of detection (0.01 IU/ml), 212 (31.8%) subjects lacked protection (0.01–0.1 IU/ml), 138 (20.7%) subjects had short-term protection (>0.1–0.5 IU/ml), and 165 (24.8%) of them showed long-term protection (>0.5 IU/ml). There was significant difference in protective rates between age groups, while there was no difference between genders. Among <3 m age group, 49.3% (35/71) of them was below the detectable level, 91.5% (65/71) lacked protection. Compared with children without vaccinations (<3 m), the protective rates of anti-TT IgG in the 3 m- <3 y group (88.0% vs 8.5%, χ2 = 34.162, P < .0001) increased significantly, and the highest proportion with long-term protection (>0.5 IU/ml) were observed in the 18 m- <3 y group (90.8%). While the proportion of protective level (>0.1 IU/ml) declined progressively with increasing age from 90.8% at age 18 m − 3y to 28.4% at age 18–40y, and this proportion remained lower than 10% in all age groups aged >40 years (). Totally, 86.2% (238/276) of adults (>18y) were lack of protective antibody (<0.1 IU/ml) against tetanus.
Seroprevalence of anti-PT IgG
Only 4.7% of the study population were detected anti-PT IgG with protective antibody level, and all of whom had seropositivity against diphtheria and tetanus. The anti-PT IgG level in 440 subjects (66.1%) was below the detectable limitation (5 IU/ml). Even with detectable anti-PT IgG, the majority (86.3%,195/226) of them had antibody levels of 5- <40 IU/ml. A majority (95.3%,635/666) of the subjects have no immune protection (≤40 IU/ml). The highest protective rate was only 7.6%, observed in patients in the >60y group. There were no significant differences in the protective rate among different age groups, gender and resident places. The distribution of anti-PT IgG levels changed with age, as shown in , the proportion of anti-PT <5 IU/ml was above 70% in all age groups aged <18 years and reached its highest level at 84.6% in 3–6y, and then decreasing with age to 31.7% at >60y group. The proportion of anti-PT 5 − 40IU/ml increased from 12.3% in subjects aged 3–6 years to 60.8% in those aged >60 years.
Figure 3. The distribution of anti-PT IgG level in the sera of subjects among different age groups, different color bar represent different antibody level
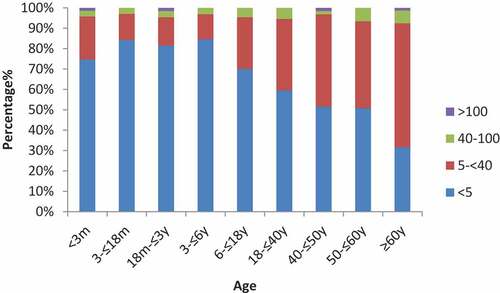
Three subjects had an anti-PT IgG≥100 IU/ml (3, 46 and 69 years respectively;≥1 years post pertussis vaccination), which was considered to be indicative of a recent pertussis infection, none of them had history of coughing ≥2 weeks. Another 20 subjects had anti-PT IgG 40- <100 IU/ml (6 in the 3 y- <18 y group and 14 in the ≥18 y group; ≥1 years post pertussis vaccination), indicative of a possible pertussis course, and four of whom had a history of coughing ≥2 weeks.
Discussion
The present study has shown that 81.7%, 91.5% and 95.8% of infants aged <3 months had no protection against diphtheria, tetanus and pertussis, respectively, placing them vulnerable to these three vaccine-preventable diseases. This is of particular concern, since this age group is more likely to have disease-related complications and even death.Citation15 In the United States, women receive a DTaP vaccine during the 27th through 36th week of each pregnancy and it turns out to be infants of immunized women had significantly higher concentrations of antibodies to all vaccine antigens from birth until age of 2 months and did not substantially alter infant responses to DTaP.Citation16In the present study, most of women of child-bearing age (18–40y) who lack protective antibodies, our findings emphasize the importance of maternal vaccination in China.
After the implementation of basic vaccination at the third, fourth and fifth months of age, and a dose of booster vaccination at 18–24 months, the protective proportion of diphtheria and tetanus increased significantly in the 3 m – <3y age group. According to the current schedule, a second booster dose of Td vaccine is recommended for Chinese children at 6 y old, but no significant increase of protective rate to diphtheria and tetanus was observed after 6 y, the actual rate of vaccination with Td recommended for 6 y old was unknown, which made it difficult to analyze the potential reasons why there is no obvious increase in the immunity against these two diseases.
Our study also shows the waning immunity with increasing age, the proportion of protective level of diphtheria and tetanus declined progressively with age from 18 m-3y age group to those aged 18–40 years. Protection from the vaccine lasts only 10 years, so it is important for adults to get a booster vaccine every 10 years.Citation15 In Some European and American countries, Td boosters are recommended every 10 years starting at age 19, to assure ongoing protection against tetanus and diphtheria for full life.Citation15 In China, Td booster is not recommended for inoculation in adults regularly unless they are wounded. The present data were an important evidence for adults to get a booster vaccine in China.
As for the protective cut off value for diphtheria, both 0.1 IU/ml and 0.01 IU/ml were used in different studies.Citation17,Citation18 With the long-term implementation of childhood vaccination program in China. There have been no diphtheria cases ever reported in the past 28 years in Chongqing and no cases reported in recent 14 years in China, there are few opportunities for people to get naturally infected with diphtheria. Thus, for safety reasons, the higher cut off value (0.1 IU/ml) was adopted in our study. According to the WHO, the global diphtheria cases are mainly concentrated in India and South-East Asia Region around China. The overall positivity rate of anti-DT IgG in our study was 54.4%, which means that a majority of population are susceptible to diphtheria. The results are consistent with previous studies carried out in BeijingCitation10and JinanCitation4 in China. Due to the waning diphtheria immunity and easy susceptibility, China may at high risk of diphtheria imports and local outbreaks,Citation7suggesting that booster doses are critical to maintain high antibody levels, and diphtheria surveillance needs to be strengthened in China.
Tetanus is almost completely prevented by active immunization.Citation19 Subjects older than 40 years of age in our study showed low tetanus protection, possibly because this population were born before 1978, most of them never received DTP vaccination in childhood or have waning immunity if they never received subsequent booster doses. In developing countries, tetanus is a major cause of death in newborn babies, whereas in developed countries, the risk for both tetanus disease and mortality was higher among persons aged ≥65 years.Citation20Moreover, adults with tetanus can present with unusual clinical forms and diagnosis of it can be difficult.Citation20 A recent article in China reported that adult tetanus can be misdiagnosed, of the 30 patients, eight were misdiagnosed with mental diseases,Citation21 suggesting that booster doses are critical to protect against tetanus infection in the elderly.
Quite different from diphtheria and tetanus, the antibody levels of pertussis maintained low level throughout all age groups, and even no immune responses were observed after the basic vaccination and booster. This is consistent with previous study carried out in China.Citation4,Citation9The different patterns of antibody level observed for diphtheria, tetanus and pertussis in one combined vaccine indicated that vaccination has limited contribution to the immunity level of pertussis in the population, perhaps some of the vaccines used in China are unable to induce long-lasting immune responses, and the quality of vaccines used should be tested. Additionally, only anti-PT IgG was evaluated in our study, which was not complete indicator of missing immunity. In China, whole cell vaccine (wP) was used during 1978–2007 and partly (together with acellular component vaccines (aP)) used during 2007–2012. wP induces an immune response against many components other than PT and some of these antigens (e.g., filamentous hemagglutinin, pertactin, and fimbriae) may confer protection.Citation22 Thus, a low level of antibody to PT might not reflect poor protection against pertussis for persons born before 2012. Meanwhile, as has been demonstrated in some studies, memory B-cells and T-cells in addition to antibodies may contribute to protection against pertussis.Citation23,Citation24Thus,it would make the study better that some cell-mediated immunity could be involved.Citation24
In this study, according to clinical diagnosis, cases diagnosed with pertussis and suspected pertussis were not included. However, among the 666 subjects, 3 subjects had anti-PT IgG ≥100IU/ml (≥1 years post pertussis vaccination), indicative of a recent pertussis course. Another nine subjects had anti-PT IgG 40- <100 IU/ml (≥1 years post pertussis vaccination), indicative of a possible pertussis course, indicated the general lack of understanding of pertussis in current clinical practice. Moreover, the proportion of anti-PT 5–40IU/ml increased with age from 12.3% in subjects aged 3–6 years to 60.8% in those aged >60 years. In China, the final DTP vaccination is given at age 18 − 24 months, and no booster doses were used to protect adolescents and adults against pertussis.Citation2The proportion of anti-PT 5–40 IU/ml increased in the 18–40y age group most likely represents recent infection with B. pertussis. Meanwhile, it has been reported that DTaP induce a weaker immune response than DTwP,Citation25thus,the rise may be attributable in part to the lower immunity from DTaP vaccine replaced DTwP vaccine in recent years. For subjects aged 40 years and over, it can be interpreted as more chance of pertussis natural infection, because this population does not have the opportunity to be vaccinated in childhood according to the vaccination policy. Additionally, adults with pertussis may present atypical symptoms,Citation26they do not usually seek treatment, the missed pertussis cases are the source of the infection to the vulnerable population. This makes pertussis difficult to monitor and control. Taken together, these findings indicated the existing surveillance system in China may underestimate the true incidence of pertussis. Thus, surveillance should be strengthened to better understand the real burden of pertussis in China.
There were certain limitations to this study. First, we only have information on the vaccination status of patients aged 3 m-3y, most of the information on the vaccination status of patients could not be obtained. Second, there are no exact standards for the cutoff of antibody level of pertussis infection, various cutoffs for recent infection used in different studies.Citation27,Citation28 According to the previous study,Citation3 anti-PT IgG≥100 IU/ml (≥1 years post pertussis vaccination) was used in our study. However, we don’t know whether the definition is suitable for Chinese population, further efforts should be made to develop the local definition for serum antibody of pertussis in China.
In conclusion, the present results revealed the susceptibility to diphtheria and tetanus in young infants and adults, and the susceptibility to pertussis over the ages. These findings highlight the need to improve the current vaccination program to afford protection for full life. Additionally, the existing surveillance system in China may underestimate the true incidence of pertussis.
Author contributors
Kaihu Yao, Changhui Chen conceived and designed the study. Dandan Liu, Xiaoping Cheng, Shi Wei, Lin Yuan did the clinical samples collection and performed the experiments. Dandan Liu, Kaihu Yao analyzed the data. Dandan Liu wrote the first draft of the manuscript and Kaihu Yao and Changhui Chen revised the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We thank all patients and their parents who made this work possible, and all study clinical staff at Youyang County People’s Hospital, Chongqing, China.
Additional information
Funding
References
- Peck M, Gacic-Dobo M, Diallo MS, Nedelec Y, Sodha SV, Wallace AS. Global routine vaccination coverage, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(42):937–42. doi:10.15585/mmwr.mm6842a1. PMID:31647786.
- Guo B, Page A, Wang H, Taylor R, McIntyre P. Systematic review of reporting rates of adverse events following immunization: an international comparison of post-marketing surveillance programs with reference to China. Vaccine. 2013;31(4):603–17. doi:10.1016/j.vaccine.2012.11.051. PMID: 23200940.
- Chen Z, Zhang J, Cao L, Zhang N, Zhu J, Ping G, Zhao J, Li S, He Q. Seroprevalence of pertussis among adults in China where whole cell vaccines have been used for 50 years. J Infect. 2016;73(1):38–44. doi:10.1016/j.jinf.2016.04.004. PMID: 27063282.
- Meng Q, Li L, Shi W, Wang Q, Ding M, Liu Y, Ma X, Yao K. Seroprevalence of diphtheria and pertussis immunoglobulin G among children with pneumonia in Jinan, China. BMC Pediatr. 2018;18(1):383. doi:10.1186/s12887-018-1337-y. PMID: 30518371.
- Xu Y, Wang L, Xu J, Wang X, Wei C, Luo P, Ma X, Hou Q, Wang J. Seroprevalence of pertussis in China: need to improve vaccination strategies. Hum Vaccin Immunother. 2014;10(1):192–98. doi:10.4161/hv.26335. PMID: 24018405.
- Wang Z, Han R, Liu Y, Du Q, Liu J, Ma C, Li H, He Q, Yan Y. Direct detection of erythromycin-resistant bordetella pertussis in clinical specimens by PCR. J Clin Microbiol. 2015;53(11):3418–22. doi:10.1128/JCM.01499-15. PMID: 26224847.
- Ning G, Gao Y, Xia W, Wu D, Li J, Li Y, Shao Z, Yin Z. Epidemiology of neonatal tetanus in China during 2010–2017. Chin J Vaccines Immunization. 2018;24:379–82.
- Yuan X. China’s vaccine production scare. Lancet. 2018;392(10145):371. doi:10.1016/S0140-6736(18)31725-2. PMID: 30152367.
- Meng QH, Liu Y, Yu JQ, Li LJ, Shi W, Shen YJ, Li L, Zhan SN, Yang F, Wang YJ, Yao KH. Seroprevalence of maternal and cord antibodies specific for diphtheria, tetanus, pertussis, measles, mumps and rubella in Shunyi, Beijing. Sci Rep. 2018;8(1):13021. doi:10.1038/s41598-018-31283-y. PMID: 30158679.
- Li X, Chen M, Zhang T, Li J, Zeng Y, Lu L. Seroepidemiology of diphtheria and pertussis in Beijing, China: a cross-sectional study. Hum Vaccin Immunother. 2015;11(10):2434–39. doi:10.1080/21645515.2015.1062954. PMID:26177302.
- Broad portfolio of IVD assays | SERION Diagnostics; 2018 Nov 20 [accessed 2020 Sep 18]. https://www.serion-diagnostics.de/en/products/product-finder/?tx_vsproducts_products%5BproductFilter%5D%5Bfilterword%5D=&tx_vsproducts_products%5BproductFilter%5D%5Bproductgroup%5D%5B0%5D=1&cHash=8ceba9fc2fb9b605dabb503d6e95d4ad.
- Naumann P. Diphtherie–Immunität und ihre epidemiologische Bedeutung. Dtsch Med Wschr. 1983;108:1090.
- Pietsch M, Pietsch R. Einsatz der ELISA-Technik zur Messung antitoxischer Tetanus-Antikörper. Wehrmed Mschr. 1989;6:258–62.
- Kelso JM, Greenhawt MJ, Li JT, Nicklas RA, Bernstein DI, Blessing-Moore J, Cox L, Khan D, Lang DM, Oppenheimer J, et al. Adverse reactions to vaccines practice parameter 2012 update. J Allergy Clin Immunol. 2012;130(1):25–43. doi:10.1016/j.jaci.2012.04.003.PMID:. 22608573.
- Liang JL, Tiwari T, Moro P, Messonnier NE, Reingold A, Sawyer M, Clark TA. Prevention of pertussis, tetanus, and diphtheria with vaccines in the United States: recommendations of the Advisory Committee on Immunization Practices(ACIP). MMWR Recomm Rep. 2018;67(2):1–44. doi:10.15585/mmwr.rr6702a1.PMID:. 29702631.
- Munoz FM, Bond NH, Maccato M, Pinell P, Hammill HA, Swamy GK, Walter EB, Jackson LA, Englund JA, Edwards MS, et al. Safety and immunogenicity of tetanus diphtheria and acellular pertussis (Tdap) immunization during pregnancy in mothers and infants: a randomized clinical trial. JAMA. 2014;311(17):1760–69. doi:10.1001/jama.2014.3633. PMID: 24794369.
- Theeten H, Hutse V, Hens N, Yavuz Y, Hoppenbrouwers K, Beutels P, Vranckx R, Van Damme P. Are we hitting immunity targets? The 2006 age-specific seroprevalence of measles, mumps, rubella, diphtheria and tetanus in Belgium. Epidemiol Infect. 2011;139(4):494–504. doi:10.1017/S0950268810001536. PMID: 20587123.
- Yao N, Zeng Q, Wang Q. Seroepidemiology of diphtheria and pertussis in Chongqing, China: serology-based evidence of Bordetella pertussis infection. Public Health. 2018;156:60–66. doi:10.1016/j.puhe.2017.12.009. PMID: 29408190.
- Rhinesmith E, Fu L. Tetanus disease, treatment, management. Pediatr Rev. 2018;39(8):430–32. doi:10.1542/pir.2017-0238. PMID: 30068747.
- Ergonul O, Egeli D, Kahyaoglu B, Bahar M, Etienne M, Bleck T. An unexpected tetanus case. Lancet Infect Dis. 2016;16(6):746–52. doi:10.1016/S1473-3099(16)00075-X.Review. PMID: 27301930.
- Wei JG, Wang SX, Qin H. Clinical diagnosis and treatment of adult tetanus. Sci Technol. 2019;31(25):191. (in Chinese)
- Scheller EV, Cotter PA. Bordetella filamentous hemagglutinin and fimbriae: critical adhesins with unrealized vaccine potential. Pathog Dis. 2015;73(8):ftv079. doi:10.1093/femspd/ftv079. PMID: 26416077.
- Hendrikx LH, Oztürk K, de Rond LG, Veenhoven RH, Sanders EA, Berbers GA, Buisman AM. Identifying long-term memory B-cells in vaccinated children despite waning antibody levels specific for Bordetella pertussis proteins. Vaccine. 2011;29(7):1431–37. doi:10.1016/j.vaccine.2010.12.033. PMID: 21187178.
- Brummelman J, Wilk MM, Han WG, van Els CA, Mills KH. Roads to the development of improved pertussis vaccines paved by immunology. Pathog Dis. 2015;73(8):ftv067. doi:10.1093/femspd/ftv067. PMID: 26347400.
- Brummelman J, Wilk MM, Han WG, van Els CA, Mills KH. Waning vaccine immunity in teenagers primed with whole cell and acellular pertussis vaccine: recent epidemiology. Expert Rev Vaccines. 2014;13(9):1081–106. doi:10.1093/femspd/ftv067. PMID: 26347400.
- Cherry JD. Adult pertussis in the pre- and post-vaccine eras: lifelong vaccine-induced immunity? Expert Rev Vaccines. 2014;13(9):1073–80. doi:10.1586/14760584.2014.935765. PMID: 24985069.
- Sakakibara Y, Ohtani Y, Jinta T, Fujie T, Miyazaki Y, Inase N, Saito R, Akaza M, Sasano T, Sumi Y. Concentrations of immunoglobulin G antibodies against pertussis toxin does not decrease over a long period of time in Japan. Intern Med. 2016;55(22):3257–63. doi:10.2169/internalmedicine.55.6973. PMID: 27853066.
- Rønn PF, Dalby T, Simonsen J, Jørgensen CS, Linneberg A, Krogfelt KA. Seroepidemiology of pertussis in a cross-sectional study of an adult general population in Denmark. Epidemiol Infect. 2014;142(4):729–37. doi:10.1017/S0950268813002446. PMID: 24103353.