ABSTRACT
CDC recommends that U.S. adults ≥50 years receive the herpes zoster (HZ) vaccine; but few are vaccinated at the recommended age. Little is known about how social determinants of health (SDH) influence timely vaccination. This retrospective observational study included U.S. adults aged ≥50 years who were vaccinated against HZ between 2014 and 2016 from IBM MarketScan commercial claims and Medicare supplemental databases. The cohort was classified into three groups based on age of vaccination: earlier (50–59 years), timely (60–64 years), and later (65+ years). Select SDH data from publicly-available sources were linked and included in multinomial logistic regression assessing the impact of SDH on timely vaccination. The final cohort comprised 549,544 individuals, 49.5% of whom were vaccinated at the age of 60–64. Odds of later HZ vaccination increased with higher poverty (OR: 1.035, 95% CI: 1.031–1.038), more democratic voters (OR: 1.011, 95% CI: 1.010–1.012), and lack of Internet access (OR: 1.028, 95% CI: 1.024–1.032), but decreased with higher health literacy (OR: 0.971, 95% CI: 0.970–0.973). Conversely, higher health literacy and lower poverty were associated with higher odds of earlier vaccination. Being male, not receiving a seasonal influenza vaccine, and higher healthcare utilization were associated with later vaccination. Individuals on an EPO/PPO vs. HMO plan, or who resided in regions other than the Northeast were more likely to receive the vaccine earlier. This study demonstrates the influence of SDH on time of HZ vaccination, but further research is needed to fully understand the impact of SDH on vaccination.
Introduction
Receipt of a herpes zoster vaccine helps reduce the risk of debilitating viral complications in adults, such as shingles and postherpetic neuralgia, particularly among those aged 50 years and older.Citation1 In 2008, the Advisory Committee on Immunization Practices (ACIP) of the US Centers for Disease Control and Prevention (CDC) provided an initial recommendation for adults aged 60 years and older to receive the herpes zoster (HZ) or shingles vaccine.Citation2 In conjunction with the availability of a recombinant zoster vaccine, ACIP updated its guidance in 2017, lowering the recommended age to 50 years and older.Citation3 However, despite the availability of two effective vaccines, rates of herpes zoster vaccination remain conspicuously low in the US. As of 2017, approximately one-third of adults 60 years and older had received the vaccine.Citation4 While this figure is above the established Healthy People 2020 goal for this vaccine, there remains a significant portion of the US population that is at-risk of being impacted by herpes zoster, a condition that is associated with approximately 2.4 billion USD in direct and indirect costs annually.Citation5
A key challenge in promoting vaccination against herpes zoster and other vaccines is perceived or actual hesitancy and resistance toward immunization. The rise of vaccine hesitancy has been particularly pronounced in recent years due to the increased skepticism perpetuated by misinformation spread through social media.Citation6 However, most of the attention studying the effects of this skepticism has been focused online at vaccination of children and adolescents, where the beliefs and attitudes of parents influence the extent to which younger Americans are vaccinated. Arguably, it is equally important to interpret vaccine-seeking behavior in adults, observations of which could help guide policymakers and providers in approaching efforts to encourage appropriate vaccination in older Americans. Initial investigations into predictors of herpes zoster vaccination in adults have suggested that the odds of vaccination are higher among females, adults with more education, those with higher incomes, rural areas residents, “dual-eligible” adults (i.e., having both Medicare and Medicaid coverage), and non-Hispanic Whites.Citation7–9
While these initial studies provided important guidance on the likelihood of certain adults to seek herpes zoster vaccination, elements beyond the healthcare system have seldom been the focus of investigations thus far. Such “social determinants of health” (SDH) are being increasingly recognized for their potentially important role in health-seeking behavior. The World Health Organization (WHO) defines social determinants of health as the “conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”Citation10 Arguably, multiple elements of this framework overlap with the vaccine hesitancy determinants matrix, also proposed by WHO. This matrix categorizes influencers on vaccine-seeking behavior by contextual, individual/group, and vaccine-specific factors that may contribute to whether an individual is vaccinated.Citation11 In supporting such a framework, WHO outlines for researchers a path forward in identifying the factors that may be at play when individuals are making vaccine-related decisions.
In spite of WHO guidance, the role of SDH in adult vaccination has received limited research attention; importantly, recent results suggest the potential presence of localized factors as evidenced by geographic variation in adherence to age-appropriate herpes zoster vaccination.Citation7 Using a nationwide claims database, the objective of this study was to determine the extent to which select social determinants were related with age-appropriate herpes zoster vaccination across regions of the country. In doing so, analyses will provide initial guidance on whether certain environmental factors are related with herpes zoster vaccination at the recommended age in adults, providing guidance to a range of stakeholders involved with appropriately promoting immunizations in older adults.
Methods
Study design and data source
This retrospective observational study used data from 2013 to 2016 within two IBM MarketScan® databases: the Commercial Claims and Encounters database and Medicare Supplemental and Coordination of Benefits database. These databases include information on patient demographic, health plan, diagnosis, procedures, and healthcare utilization of a nationwide convenience sample of U.S. residents with private health insurance. The databases are de-identified and compliant with the Health Insurance Portability and Accountability Act of 1996. This study was determined to be non-human subjects research by the Institutional Review Board of the University of Tennessee Health Science Center.
Participant selection and measures
Eligible individuals included those aged 50 years or older in any of the years between 2014 and 2016 who had received the HZ vaccine anytime in that period. Despite the recommendation being for adults aged 60 years or older during the study period, 50 or above subjects were included as these population were found to benefit from the vaccine,Citation1 and to identify predictors of early vaccine-seeking behavior. Subjects were required to be continuously enrolled at least the year before and of vaccination. Those who resided outside a metropolitan statistical area (MSA) were excluded as SDH data were available for only those living in MSAs. Eligible patients were divided into three age groups: earlier vaccination (50–59 years), timely vaccination (60–64 years), and later vaccination (65 years and above) based on 2008 ACIP recommendation for HZ vaccination.Citation2
Vaccination was assessed for each participant by evaluating National Drug Codes from their pharmacy claims and Current Procedural Terminology codes from their inpatient and outpatient claims. If multiple HZ vaccination records existed for any patient, only the first vaccination record was retained. Standard demographic characteristics were extracted for comparison and included age, gender, region of residence, and health plan type. Other factors derived from claims included immunocompetency status (diagnosis codes listed in Appendix), influenza vaccine receipt in the year of HZ vaccination, and health resource utilization (e.g., number of inpatient admissions, emergency visits, outpatient visits, and pharmacy visits) in the year prior to the year the patient received the HZ vaccine. Multiple SDH factors were derived from several external sources and used as primary predictors for this study. Earlier research by WHO suggested that a matrix of factors influences vaccine-seeking behavior including contextual, individual/group, and vaccine-specific factors.Citation7 However, using the WHO matrix to predict individual behavior remains a challenge due to the lack of individual-level data on these factors; consequently, we identified suitable proxies for several factors within the matrix from external, publicly-available sources. The proxy factors included MSA-level estimates for health literacy, presidential election voting records (as a percent of democratic voters), the percent of residents living in poverty, the percent of computer owners, and the percent of residents who lack the Internet access. These SDH data were collected from the University of North Carolina (health literacy), county-level election data compiled by MIT for the 2012 presidential election (voting records by political party), and the American Community Survey (poverty, Internet, and computer ownership).Citation12–14 The values were originally at census tract or county levels and were averaged across the individual’s metropolitan statistical area (MSA) of residence. Such use of geographic proxies to identify the burden of SDH on health outcomes has been applied similarly elsewhere.Citation15
Statistical analysis
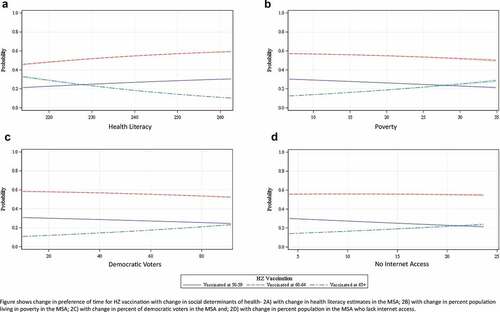
Descriptive statistics (frequencies and percentages for categorical variables and means and standard deviations for continuous variables) were provided on patient characteristics and three vaccinated groups were compared using t-tests and ANOVA. Multinomial logistic regression provided the odds of earlier and later HZ vaccination using SDH variables as primary predictors and controlling for other covariates. A p-value < 0.05 was set a priori as the threshold for statistical significance. The multinomial logistic regression model was used to determine and plot predicted probabilities of vaccination by age group against each SDH variable. Predicted probabilities provided the assessment of change in preference of age of vaccination with respect to change in the SDH factors keeping control variables fixed at the reference level or mean. All data analyses were conducted in 2020 using SAS, version 9.4 (Cary, NC).
Results
A total of 549,544 individuals met all the inclusion-exclusion criteria and had complete data (). Nearly half of the population (49.5%) belonged to the timely vaccination group (i.e., 60–64 years) (). A majority of the population across all three groups were female (52–58%) and immunocompetent (75–84%). Approximately half of the earlier and timely vaccination groups received the influenza vaccine in the year of HZ vaccination, but less than one-fourth of those among the later vaccination group had done so over the same time period (). Compared to the earlier and timely groups, the later vaccination group had higher average pharmacy visits (18.9 vs. 14.1 and 14.1, respectively, p < .0001), outpatient visits (16.1 vs. 12.7 and 12.3, respectively, p < .0001), inpatient admissions (0.15 vs. 0.06 and 0.07, respectively, p < .0001), and emergency visits (0.25 vs. 0.15 and 0.15, respectively, p < .0001) ().
Table 1. Patient population
Multinomial logistic regression determined that the odds of later HZ vaccination increased with higher poverty rates (OR: 1.035, 95% CI: 1.031–1.038) and in communities with more democratic voters (OR: 1.011, 95% CI: 1.010–1.012) but decreased with higher estimates of health literacy (OR: 0.971, 95% CI: 0.970–0.973) in the MSA (). People with access to technology were less prone to later vaccination as computer ownership had lower odds (OR: 0.986, 95% CI: 0.982–0.989) and lack of internet access had higher odds (OR: 1.028, 95% CI: 1.024–1.032) of later vaccination. Males, those identified as immunocompromised, and adults with no record of influenza vaccination in the year of HZ vaccination were associated with higher odds of later vaccination (). Higher utilization of any health resource was associated with higher odds of later vaccination.
Table 2. Odds of earlier and later herpes zoster vaccination
The odds of earlier HZ vaccination slightly increased with increases in heath literacy (OR: 1.002, 95% CI: 1.000–1.004) but decreased slightly with increases in poverty (OR: 0.992, 95% CI: 0.989–0.995), the proportion of democratic voters (OR: 0.999, 95% CI: 0.998–0.999), and lower proportion of internet access (OR: 0.983, 95% CI: 0.980–0.987) in the MSA. Factors associated with lower odds of earlier vaccination were not being vaccinated against seasonal influenza in the same year (OR: 0.871, 95% CI: 0.859–0.882), and having more inpatient admissions (OR: 0.870, 95% CI: 0.850–0.890) and pharmacy visits (OR: 0.998, 95% CI: 0.997–0.998) ().
Predicted probabilities were obtained to assess the change in preference of time for HZ vaccination with change in SDH values. These probabilities were estimated keeping covariates constant at the reference level (for categorical variables) or at the mean (for continuous variables), i.e. the findings in are for a female living in the Northeast who is on an HMO health plan, is immunocompetent, had received the influenza vaccine in the baseline year, and had average number of pharmacy, outpatient, inpatient, and emergency visits. From , 60–64 years was the most preferred age group for HZ vaccination at any health literacy level and the preference increased with increases in health literacy in the MSA. Age 65 and above was the preferred group over 50–59 years age group until health literacy level of approximately 228, after which the preference flipped. A health literacy level of 228 can be translated to an intermediate health literacy skill as per the National Assessment of Adult Literacy (NAAL),Citation16 indicating that those with at least intermediate health literacy skills were more likely to vaccinate earlier. The most preferred age group for vaccination was 60–64 at any poverty level although the preference declined as percentage of poverty increased (). In MSAs with up to 28% population living in poverty, earlier vaccination was preferred over later vaccination, but beyond that percent of poverty, later vaccination becomes more preferable. A similar relationship was seen between earlier and later vaccination preference with change in percent population living with lack of Internet access. In MSAs where more than 21% of the population lived with no internet access, later vaccination was more preferable than earlier vaccination, and 60–64 years remained the overall preferred age for vaccination (). Regardless of political view, 60–64 years was the most preferred group for vaccination (). However, the preference for 60–64 and 50–59 groups declined and 65+ group increased with an increase in the percent of the democratic vote in the MSA.
Discussion
Vaccine hesitancy is a growing worldwide concern.Citation11 While much of the focus has been toward the outcomes and consequences of hesitancy related to pediatric vaccination, less attention has been paid to vaccine hesitancy in adults.Citation17,Citation18 This study examined the impact of select social determinants of health on shingles vaccination across age groups and areas of the country as a means to help in developing effective means to counter adult vaccine hesitancy.
This study adds to only a handful of others which explored herpes zoster vaccine-seeking behavior and hesitancy in the U.S. and abroad. A 2009 survey in the Netherlands found that determinants of vaccine hesitancy included the lack of a formal recommendation by a provider and a patient’s perception of a low risk of contracting shingles.Citation19 Similarly, a 2014 survey in U.S. community pharmacies found that patients were unaware that they needed the vaccine, although the perceived risk of shingles occurrence was only seen in a small minority as opposed to the Netherlands survey.Citation20 Lastly, in a 2019 survey in the United Kingdom, quality provider recommendation and a perceived risk of shingles were found to be positively associated with zoster vaccination.Citation21 Of note, the survey sample in the Netherlands perceived disease risk among the eligible population as low and consequently it was a major determinant of vaccine hesitancy, whereas the 2019 U.K. survey found that higher perceived risk was associated with vaccination and highlights the importance of this factor. This may explain in part why differences in vaccine-seeking behaviors across genders became less profound as age increased. Men had a higher probability of becoming vaccinated “later” while women were more likely to be vaccinated “earlier.” However, this effect waned as men approached the age of 65. In general, men are less likely to accept preventative care recommendations and vaccine recommendations in particular.Citation22–25 The waning effect seen here may be related to the increasing incidence of shingles occurrence with age, and it stands to reason that as one ages the chances of first-hand knowledge of someone diagnosed with shingles may also increase.Citation26
The importance of provider recommendations is further emphasized in the present study. Vaccination was associated with more frequent visits to the pharmacy and medical offices, most likely due to a higher likelihood of vaccine recommendations being made. Given that pharmacy visits are more frequent than other provider settings, the role of the pharmacist in making quality zoster recommendations on a routine basis may have a large impact on overall zoster vaccination rates.Citation20,Citation27 ACIP and other professional organizations recommend combining vaccine recommendations to improve vaccine hesitancy (e.g., seasonal influenza vaccination and pneumococcal vaccinations concomitantly administered).Citation28 Results from the present study support this practice as it leads to earlier vaccination.
Social determinants of health were also found to be significantly linked to vaccination. This is an important finding as limited research has been done linking SDH to vaccinations. The work that has been done has demonstrated that SDH factors such as education, income, and location (underserved areas) negatively impact vaccine status.Citation29 The present study adds to this, as it was found that poverty, health literacy, living in an area with a majority democrat voter affiliation, computer ownership, and internet access were significant predictors of zoster vaccination. The current study shed light on the cutoff values for each SDH variable where individual’s vaccine-seeking behavior alters and helps identify social parameters to consider when designing vaccination policies. For instance, those with health literacy below the intermediate level, or who live in areas where over 28% of the population live below the poverty level or over 21% do not have Internet access are more likely to delay vaccination and may need additional assistance or convincing to seek vaccination in time. These findings also help target and drive vaccination interventions for public health efforts and health plan quality improvements. This is similar to SDH impact on pneumococcal and influenza vaccination. In a recent observational study, individuals residing in high health literacy or democratic voter-rich areas were found to be more likely to receive pneumococcal vaccination.Citation30 In a recent systematic review of quantitative and qualitative studies on seasonal influenza vaccination, factors including age, gender, sources of information, and social influence were found to be determinants of vaccination status.Citation31 Interestingly in the current study, internet access was positively correlated with earlier vaccination and negatively correlated with later vaccination. Computer access did not impact earlier vaccination, but negatively impacted later vaccination. This phenomenon calls for further exploration in future studies, especially in light of the established impact of perceived risk on zoster vaccination, and the current era of social media and post-truth politics.
This study has a few limitations. First, it consisted of only privately insured populations who are either working or have worked and, therefore, the findings may not be generalizable to beneficiaries who are not working or have other or no insurance. Furthermore, rural residents could not be studied as SDH data were not available for them. Also, other social determinants including but not limited to race, employment status, availability of transportation, physical environment etc. could influence HZ vaccination but could not be studied due to unavailability. Cost-sharing components were not controlled which may have influenced vaccine-seeking behavior. Moreover, the SDH factors incorporated are generalized at the MSA level but, the impact of these factors at the patient level may vary. This study aimed to demonstrate a high-level signal first that can be further studied with a deeper level analysis using more granular data. Finally, being an observational study, the current study cannot establish causal relationships between SDH and HZ vaccination. As the recommendation for receiving the vaccine has changed to 50 years of age, the magnitude of the impact of SDH factors may change; although, the direction should not alter.
In conclusion, many Americans receive the HZ vaccine at an older age than recommended or do not receive it at all. Policies focused at improving care for individuals with substandard social determinants of health such as low health literacy, high poverty, and poor access to internet have potential to be effective in mitigating vaccine hesitancy and encouraging early vaccine-seeking behavior. Patients with high healthcare utilization suffer delay in receiving the HZ vaccine, indicating strong advocacy from physicians and pharmacists at every opportunity can significantly improve vaccination. Combining recommendation for HZ vaccine with more widely used vaccines e.g. influenza can greatly improve the timely use of HZ vaccination. Further research is needed for more comprehensive understanding of the impact of social determinants on vaccination.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Supplemental Material
Download MS Word (43.9 KB)Acknowledgments
The research and recommendations presented in this paper are that of the authors and do not reflect the official policy of CDC. This article contents have not been previously presented or submitted anywhere else. This study was not funded by any sponsor.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
References
- Food and Drug Administration. Zostavax (herpes zoster vaccine) questions and answers; Oct 2018. [accessed 2020 Sep]. https://www.fda.gov/vaccines-blood-biologics/vaccines/zostavax-herpes-zoster-vaccine-questions-and-answers
- Centers for Disease Control and Prevention, Prevention of herpes zoster: recommendations of the advisory committee on immunization practices (ACIP). MMWR Early Release. 2008;57(6June):1–30.
- Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, Harpaz R. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103–08. doi:10.15585/mmwr.mm6703a5.
- Healthy people 2020 [Internet]. Immunization and Infectious Diseases. Washington (DC): U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. [ accessed 27 Jan 2020]. https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4673.
- Harvey M, Prosser LA, Rose AM, Ortega-Sanchez IR, Harpaz R. Aggregate health and economic burden of herpes zoster in the United States: illustrative example of a pain condition. Pain. 2020;161:361–68.
- Benecke O, DeYoung SE. Anti-vaccine decision-making and measles resurgence in the United States. Glob Pediatr Health. 2019;6:2333794X19862949.
- La EM, Trantham L, Kurosky SK, Odom D, Aris E, Hogea C. An analysis of factors associated with influenza, pneumoccocal, Tdap, and herpes zoster vaccine uptake in the US adult population and corresponding inter-state variability. Hum Vaccin Immunother. 2018;14(2):430–41. doi:10.1080/21645515.2017.1403697.
- Hechter RC, Tartof SY, Jacobsen SJ, Smith N, Tseng HF. Trends and disparity in zoster vaccine uptake in a managed care population. Vaccine. 2013;31(41):4564–68. doi:10.1016/j.vaccine.2013.07.053.
- Shen AK, Warnock R, Selna W, MaCurdy TE, Chu S, Kelman JA. Vaccination among Medicare-fee-for service beneficiaries: characteristics and predictors of vaccine receipt, 2014-2017. Vaccine. 2019;37(9):1194–201. doi:10.1016/j.vaccine.2019.01.010.
- World Health Organization [Internet]. Social determinants of health. Geneva (Switzerland): World Health Organization. [ accessed 2020 Jan 27]. https://www.who.int/social_determinants/sdh_definition/en/.
- MacDonald NE; The SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- National Health Literacy Mapping to Inform Health Care Policy. Health literacy data map. University of North Carolina at Chapel Hill. [accessed 2018 Jul 2]. http://healthliteracymap.unc.edu/#
- MIT Election Data and Science Lab, 2018, “County presidential election returns 2000-2016”. [accessed 27 Jan 2020]. https://doi.org/10.7910/DVN/VOQCHQ,HarvardDataverse,V6,UNF:6:ZZe1xuZ5H2l4NUiSRcRf8Q==[fileUNF].
- US Census Bureau. American community survey; 2014. [Accessed 2018 Jul 2]. https://factfinder.census.gov/
- Comer KF, Grannis S, Dixon BE, Bodenhamer DJ, Wiehe SE. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep. 2011;126(Suppl3):54–61. doi:10.1177/00333549111260S310.
- Kutner M, Greenberg E, Jin Y, Paulsen C, White S. The health literacy of america’s adults: results from the 2003 national assessment of adult literacy. U.S. Department of Education, Institute of Education Sciences, and National Center for Education Statistics. Sep 2006. [2020 accessed Jun 25]. https://nces.ed.gov/pubs2006/2006483.pdf
- Lo NC, Hotez PJ. Public health and economic consequences of vaccine hesitancy for measles in the United States. JAMA Pediatrics. 2017 Sep 1;171(9):887–92. doi:10.1001/jamapediatrics.2017.1695.
- Edwards KM, Hackell JM. Countering Vaccine Hesitancy. Pediatrics. 2016;138(3):e20162146. doi:10.1542/peds.2016-2146
- Opstelten W, van Essen GA, Hak E. Determinants of non-compliance with herpes zoster vaccination in the community-dwelling elderly. Vaccine. 2009;27(2):192–96. doi:10.1016/j.vaccine.2008.10.047.
- Teeter BS, Garza KB, Stevenson TL, Williamson MA, Zeek ML, Westrick SC. Factors associated with herpes zoster vaccination status and acceptance of vaccine recommendation in community pharmacies. Vaccine. 2014 Sep 29;32(43):5749–54. doi:10.1016/j.vaccine.2014.08.040.
- Bricout H, Torcel-Pagnon L, Lecomte C, Almas MF, Matthews I, Lu X, Wheelock A, Sevdalis N. Determinants of shingles vaccine acceptance in the United Kingdom. PLoS One. 2019;14(8):e0220230. doi:10.1371/journal.pone.0220230. Published 2019 Aug 1
- Hernandez EM, Margolis R, Hummer RA. Educational and gender differences in health behavior changes after a gateway diagnosis. Journal of Aging and Health. 2018 Mar;30(3):342–64. doi:10.1177/0898264316678756.
- Saint Onge JM, Krueger PM. Health lifestyle behaviors among US adults. SSM-Population Health. 2017 Dec;1(3):89–98. doi:10.1016/j.ssmph.2016.12.009.
- Buchan SA, Kwong JC. Trends in influenza vaccine coverage and vaccine hesitancy in Canada, 2006/07 to 2013/14: results from cross-sectional survey data. CMAJ Open. 2016;4(3):E455–62. doi:10.9778/cmajo.20160050.
- Centers for Disease Control and Prevention. Flu vaccination coverge, United States, 2016–17 influenza season. [accessed 2018 May 3]. https://www.cdc.gov/flu/fluvaxview/coverage-1617estimates.htm.
- Schmader K. Herpes zoster and postherpetic neuralgia in older adults. Clin Geriatr Med. 2007;23(3):615–32, vii–viii. doi:10.1016/j.cger.2007.03.003.
- Hohmann LA, Hastings TJ, Ha DR, Garza KB, Huston SA, Chen L, Westrick SC. Impact of a mulit-component immunization intervention on pneumococcal and herpes zoster vaccinations: A randomized controlled trial of community pharmacies in 2 states. RSAP. 2019;15:1453–63.
- Centers for Disease Control and Prevention. Timing and Spacing of Immunobiologics. General best practice guidelines for immunization: best practice guidance of the Advisory Committee on Immunization Practices (ACIP). [accessed 2020 May 13]. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/timing.html.
- Jain A, van Hoek AJ, Boccia D, Thomas SL. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine. 2017 Apr 25;35(18):2315–28. doi:10.1016/j.vaccine.2017.03.013.
- Gatwood J, Shuvo S, Hohmeier KC, Hagemann T, Chiu C, Tong R, Ramachandran S. Pneumococcal vaccination in older adults: an initial analysis of social determinants of health and vaccine uptake. Vaccine. 2020 July;31(38):5607–17. doi:10.1016/j.vaccine.2020.06.077.
- Nagata JM, Hernández-Ramos I, Kurup AS, Albrecht D, Vivas-Torrealba C, Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults≥ 65 years: a systematic review of qualitative and quantitative data. BMC Public Health. 2013 Dec;13(1):388. doi:10.1186/1471-2458-13-388.