ABSTRACT
In the last two decades, outbreaks due to the foodborne hepatitis A virus (HAV) have been frequently reported in India, with adolescents and adults primarily affected. In India, most food handlers are adolescents and young adults who might be exposed to unsatisfactory environmental conditions and poor water quality. This increases the risk of HAV infection and consequently compounds the risk of HAV transmission from food handlers to susceptible populations. Given the shift in hepatitis A endemicity from high to intermediate levels in India, implementing the vaccination of food handlers has become important as it can also contribute to the elimination of hepatitis A in India. This narrative review makes a case for hepatitis A immunization of food handlers in India considering the growing food industry, evolving food culture, and the substantial burden caused by hepatitis A outbreaks.
PLAIN LANGUAGE SUMMARY
What is the context?
Hepatitis A disease is a common form of viral hepatitis and is transmitted through contaminated food and water or through close contact with an infected person. The virus with stands high temperature and can survive on surfaces for long periods of time.
In India, the burden of hepatitis A has shifted from children to adolescents and adults who are more culnerable to infection. They present a high risk of complications, often requiring hopitalization.
The prevention of the disease has often bee neglected, inadequate safety measures for the preparation of food (via food handlers) is a known risk factor for the transmission of hepatitis A.
What is new?
Our review highlights the relationship between food handling and hepatitis A infection among adolescents and adults in Inida.
The lack of knowledge of food safety regulations and hygiene measures among food handlers and the organizations that guide them may contribute to the spread of hepatitis A.
What is the impact?
Sanitation efforts, awareness and educational programs for food are needed to help reduce the transmission of hepatitis A virus and disease, yet these measures alone may not be sufficient.
Vaccination among high-risk populations such as food handlers can prevent hepatitis A infection and its complications as well as transmission.
Introduction
Hepatitis A virus (HAV) causes infection through the fecal-oral route. It is usually asymptomatic in children as compared to higher age groups in whom complications such as acute liver failure, autoimmune hepatitis, and others have been reported.Citation1 Typically, clinical illness resolves within two months, with approximately 10%–15% of persons showing prolonged or relapsing symptoms for up to 6 monthsCitation1,Citation2 and death in rare situations.Citation3
Hepatitis A is estimated to cause over 100 million cases and around 15,000–30,000 deaths per year worldwide.Citation4 It occurs intermittently and is known to cause outbreaks, with a trend of cyclic recurrences.Citation1 Globally, food contaminated with HAV accounts for 2–7% of all HAV outbreaks.Citation5 Infected individuals may require hospitalization which places a large strain on individual households expenses.Citation6 According to global estimates, approximately 600 million cases of foodborne illness related to 31 pathogens are reported annually, of which 14 million cases are due to HAV infection with 1,353,767 Disability-Adjusted Life-Years (DALYs),Citation7 which reflects the ability of the virus to persist in the environment and withstand food-production processes.Citation4 Food handlers play a major role in preparation of safe food, and they may transmit HAV to susceptible individuals, if infected themselves.Citation2,Citation8,Citation9 In India, lack of knowledge and awareness of preventing foodborne diseases and practice of proper hygiene among food handlers is a major concern as it may lead to a significant disease burden due to foodborne infections such as hepatitis A.Citation10
To date, there is no overview of the HAV disease burden in the context of food handling in the Indian setting. Thus, the objective of this review is to summarize evidence from published literature in order to create awareness among healthcare providers, the scientific community, and policymakers on the role of food handlers in HAV transmission and present strategies to prevent, control, and eliminate hepatitis A disease and related outbreaks in India (see ).
Hepatitis A in adolescents and adults: a shift in disease endemicity
In regions where sanitary conditions have improved rapidly, cases of HAV in adolescents and adults are accumulating as they do not have immunity resulting from exposure in early childhood.Citation11 In India, the burden of HAV infection has been on the rise with the disease being primarily reported in adolescents and adults.Citation12 In a community study of hepatitis A in India, it was observed that the attack rate was highest among the 15–24 years age group (4.6%) followed by 3.1% and 1.2% in 5–14 and <5 years age groups, respectively.Citation13 Attack rate for individuals >25 years of age was lower than 1%.Citation13 Although milder illness in children might not have been captured and no statistical analysis was conducted in the study, attack rates of this magnitude reflect the vulnerability of the adolescent and adult population to HAV.Citation13 According to recent census data, India has a population of roughly 1.38 billion people, of which approximately 63.7% are 15–59 years of age and economically active.Citation14 Given the attack rates in adolescents and adults, and the changing social and cultural behaviors in India,Citation15 it is a reasonable assumption that with the shifting HAV endemicity in India,Citation12 HAV infection could have a large impact on individual health, and families due to loss of income and productivity.
Current status of the burgeoning food industry in India
In recent years, India has undergone rapid socioeconomic growth resulting from increasing trade and industry, increasing degree of modernization, and access to better education, health services, housing, nutrition, and technology. This has led to an increase in disposable income which is leading to an unprecedented change in consumer behavior. Coupled with favorable demographics, this has led to a rapid growth in the food sector. The Indian food industry is projected to grow at a compounded annual growth rate of approximately 10% per year (2020–2025)Citation16 with multinational fast food corporations being the major segments.Citation17 Furthermore, according to a statistical report, the number of street food stalls in India are also steadily growing with an increase from 920,000 in 2008 to 1.2 million in 2013.Citation18 These data are indicative of the increasing numbers of people opting to eat out at food establishments.
Evolution of food culture in India
Given the socioeconomic progress in India, there has been a transition in population behavior, attributable mainly to the steadily rising income levels of the Indian population. The spending capacity of the Indian working population between 25 and 49 years of age is amongst the top three in the world.Citation17 Given that the majority of the population is active in the workforce, this has led to an increase in overall spending and consequently to a change in eating out habits. shows that among individuals below 50 years of age, about 70% would dine outside 1–3 times per week, and 15% would eat out 4–6 times per week; among individuals of 20–30 and 31–40 years of age, up to 10% would eat out more than 16 times in one week. Notably, 89% of individuals who ate outside of their home indicated that cleanliness was important or extremely important.Citation19 Reasons for eating outside of home are related to time constraints of individuals which are driven by both men and women increased focus on their career.Citation17 Adolescents and adults in India have a culture of eating and socializing at street food stalls, attending weddings and other social events which are found ubiquitously across the country. Also, the number of educational institutes according to the All India Survey on Higher Education (AISHE) in 2018–19, were approximately 993 universities, 39,931 colleges and 10,725 stand-alone institutions in India with cafeterias available in 87%, 57% and 61% of these institutions, respectively.Citation20 A large proportion of the Indian population is also known to travel long distances for work or other reasons; between 2010 and 2019, the Indian railway network transported over 23 million passengers every day.Citation21 Given the duration of these long journeys, passengers are compelled to obtain food provided by catering facilities or independent food retailers who operate on the trains.
Figure 1. Habits of eating outside in India (number of times per week) per age group. Source: Adapted from Srividhya, 2014.Citation19yrs, years
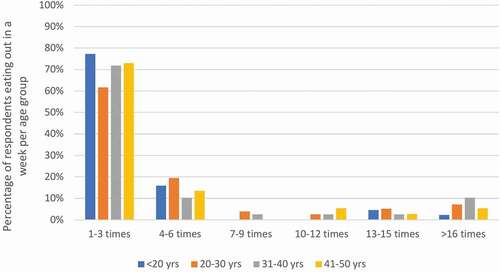
Collectively, these data reflect that a large population in India is potentially at risk of being exposed to foodborne HAV infection.
Role of food handling in HAV outbreaks in India
According to the National Center for Disease Control (NCDC), an outbreak due to a foodborne disease is declared when two or more cases of a similar illness occur after the consumption of a common food or the observed number of cases of a specific disease exceeds the anticipated number.Citation22 In India, incidence data for hepatitis A are limited or generally lacking, but despite the lack of surveillance system, few information on HAV incidence is nevertheless available, as reported through the Integrated Disease Surveillance Programme (IDSP) at NCDC.Citation23 According to the NCDC, there were a total of 315 outbreaks of viral hepatitis between 2010 and 2013, and HAV was responsible for 10%–30% of acute viral hepatitis cases and 5%–15% of acute liver failure cases in India.Citation23
provides a summary of publications describing HAV outbreaks reported across India among adolescents and adults covering the time period 2004–2020.Citation13,Citation24–35 A majority of the studies documented the source of the outbreaks as unsafe food handling, unhealthy personal hygiene, or unsafe sanitation practices.Citation24,Citation25,Citation27,Citation29,Citation30,Citation32–35 Outbreaks were also linked to the utilization of contaminated water or food by hotels and restaurants.Citation13,Citation26,Citation28 For example, one study reported that an outbreak occurred due to the use of unclean water in a welcome drink at a wedding ceremony.Citation31 Across studies, the adolescent and adult groups were reported to have the highest number of cases (). This observation is clearly noticeable in regions with better sanitation, hygiene, and higher standards of living.Citation13,Citation26,Citation28–32,Citation34 While there were a few reports of cases in children,Citation25,Citation33,Citation35 most cases in other states were also reported in adolescents and adults ().
Table 1. HAV outbreaks among adolescents and adults in India
Lessons learned from foodborne HAV outbreaks
Given India’s socioeconomic diversity, there is a significant variation in the occurrence of HAV outbreaks within India; importantly, several lessons can be learned. While it is important that the risk of outbreaks in different regions should be closely monitored and proactively mitigated, strategies to prevent HAV infection and transmission are urgently needed in the country. In this context, the phrase “From farm to plate, make food safe”Citation36 for food safety might be useful, as it could help in developing a preventive strategy composed of different complementary measures such as improving sanitation and access to clean drinking water, maintaining healthy food and water hygiene practices, and immunization.Citation4
Barriers and challenges for food handlers
It is essential to understand the barriers and challenges faced by food handlers to ensure the successful implementation of an intervention strategy to control, and ideally contribute to the elimination of hepatitis A in India. The main barrier that food handlers face whilst realizing the importance of food safety, is the lack of time to collect relevant regulatory information for their establishment,Citation37 and assimilate the guidelines put in place by several bodies in India,Citation38 like the Food Safety and Standards Authority of India (FSSAI).Citation39 This is in part due to the complex regulatory framework that oversees the implementation of food safety principles.Citation9,Citation38 Furthermore, the dissemination practices related to updates on changes in regulations and guidelines of food safety adopted by these bodies are inadequate.Citation38 Regarding small- and medium-scale food industries, Food Business Operators (FBO) have stated that they find it difficult to stay updated on relevant procedural and compliance changes and do not have the capacity to track regulatory changes.Citation38 Even if food safety principles are implemented, relevant institutional and human resources to monitor food safety coupled with satisfactory laboratory and testing-capacity are generally unavailable in India.Citation38
Knowledge, attitudes, and practices among food handlers in India
The complexities related to food regulations, poor knowledge, general awareness about hygiene, and the improper safety practices of food handlers are known to impede the prevention of foodborne illnesses such as hepatitis A. Importantly, the lack of education or training influences the attitude of food handlers toward implementing food safety principles.Citation40–43 A cross-sectional study among street food vendors revealed that a majority of them were familiar with the terms “food hygiene” and “foodborne illness.” However, less than one-third of these street food vendors had acceptable food preparation practices.Citation43 An indifferent attitude toward implementing and maintaining food hygiene was significantly associated with age, gender, education, marital status and type of food vendor.Citation43 Singh et al. showed that basic hygiene and sanitation practices were documented as less than satisfactory among food vendors due to a lack of adequate infrastructure and training related to food hygiene.Citation44 Other studies have found similar associations.Citation40–42 Collectively, this evidence suggests a high prevalence of general awareness about hygiene and food safety principles among food handlers, yet these principles were seldom implemented, mainly attributable to an indifferent attitude toward food safety.
Strategies for the control and elimination of foodborne hepatitis A
In terms of strategies to minimize the risk of HAV outbreaks, several non-pharmaceutical and pharmaceutical interventions should be utilized to tackle HAV transmission due to food handling. First, in terms of non-pharmaceutical interventions, water quality should be improved and monitored regularly to ensure the provision of clean and safe drinking water for food handling and preparation. Second, chlorination of wells and the use of boiled water should be implemented for food, drink, and ice preparations. Finally, within the context of food preparation, food safety principles should be implemented in food establishments such as street food stalls, cafeterias, restaurants, and hotels. The importance of proper handwashing should also be stressed. In addition to these interventions, the spread of hepatitis A may be controlled and prevented through hepatitis A vaccination.
The World Health Organization (WHO) states that vaccination against hepatitis A should be part of a comprehensive plan for the prevention and control of viral hepatitis, including measures to improve hygiene and sanitation and measures for outbreak control. The WHO recommends implementation of HAV vaccination of children ≥1 years of age in universal vaccination programs of countries where a shift in endemicity has been documented, following epidemiology and cost-effectiveness considerations.Citation3,Citation4,Citation45 Moreover, the WHO considers food handlers as a risk group.Citation4
In India, to date, no universal vaccination recommendations are made for groups most susceptible to HAV, such as adolescents and adults or food handlers.Citation46 However, the Indian Medical Association (IMA) and the Association of Physicians of India (API) recommend hepatitis A vaccination in special or high-risk individuals such as adolescents and adults,Citation47 and food handlers.Citation48 While vaccination of food handlers does not address the situation wherein food itself may be contaminated with hepatitis A, this strategy would be an important step in preventing the transmission of HAV to susceptible individuals.
Hepatitis A vaccination of food handlers
Worldwide, there are several hepatitis A vaccines available for use in adolescents and adults; clinical trials have reported that hepatitis A vaccination is safe and efficacious in these populations.Citation3,Citation4 The remarkable immunogenicity of hepatitis A vaccines in adolescents and adults is reflected in rapid seroconversion rates, enabling both preexposure and postexposure prophylaxis.Citation3,Citation4,Citation49 The efficacy and safety of hepatitis A vaccination have been established in children, adolescents, and adults.Citation3,Citation4
The value of immunization of food handlers has also been demonstrated in the real-world setting, as in the United States (US). Despite a low HAV endemicity, several hepatitis A outbreaks in St. Louis (two restaurants and one cafeteria) led to the implementation of mandatory hepatitis A vaccination of food handlers. Consequently, the case rate of hepatitis A dropped from 3 per 100,000 population during the pre-hepatitis A vaccination period to 1 per 100,000 population, thereby lowering the morbidity and economic burden.Citation50 Recently (2019), The Alabama Department of Public Health, Immunization Division, recommended hepatitis A vaccination for all food workers across the state, given that there were 132 confirmed outbreak-related cases in at least 25 Alabama counties.Citation51 Such initiatives testify to the value of vaccination of food handlers in the prevention of hepatitis A and underscores the importance of local outbreak data in vaccine-policy decision-making. This is in line with recommendations from US Advisory Committee on Immunization Practices (ACIP) to vaccinate food handlers with hepatitis A vaccine based only on local epidemiological data.Citation52 It is worth noting that mandatory hepatitis A vaccination for food handlers is not recommended by the US ACIP, probably because investigation reports of HAV infected food handlers transmitting infections in restaurants are not directly reported to the US Centers for Disease Control and Prevention (CDC) but reported in local newspapers.Citation53 However, the ACIP recommendation state that contamination of food with HAV can occur from the time of harvest, processing, handling, or after cooking the food; and also in imported food items.Citation52 In this context, the ACIP does recommend HAV vaccination for individuals requesting protection without acknowledgment of a risk factor.Citation52 Few countries that have intermediate HAV endemicity in the Asia-Pacific region (e.g. Sri LankaCitation54) recommend the vaccination of high-risk groups such as food handlers. In Ireland, a country with low endemicity, recent guidelines stipulate that hepatitis A vaccination is recommended for food handlers who are not immune.Citation55 Yet, to our knowledge, there is no experience of this strategy from countries that are experiencing a shift in HAV endemicity, like India.
In the Indian setting, HAV immunization of adults is often neglected or there is a lack of drive among policymakers, HCPs and other stakeholders. Moreover, low perception or access to vaccination and cost issues may also play an important role.Citation56,Citation57 A recent review on economic evaluations of hepatitis A vaccination strategies suggests that hepatitis A vaccination has favorable cost-effectiveness in middle-income countries if they are of high and intermediate endemicity.Citation58 Given the shift from high to intermediate endemicity and the substantial cost of treating one HAV case (USD 346) in India,Citation6 vaccination of food handlers to prevent the spread of HAV across the country could potentially be cost-effective, and even cost-saving when both direct and indirect costs of disease are taken into account. These reports should be a wake-up call for the policymakers to make hepatitis A vaccination mandatory for food handlers and not merely to rely on standard interventions such as investigation, education, proper sanitation, and hygiene.
Discussion
This review article makes a case for the immunization of food handlers in India considering the growing food industry, evolving food culture, and hepatitis A outbreaks. We identified several outbreaks that occurred between 2004 and 2020 across several states in India which resulted from improper food handling practices and the use of inadequate water supply.Citation13,Citation24–35 Observations from outbreaks support a shifting endemicity in India with adolescents and adults being primarily affected by HAV infection.Citation13,Citation24–35 This finding is consistent with reports from other countries that have also seen improvements in socioeconomic indicators; with increasing incomes and improvements in access to clean water and adequate sanitation.Citation59,Citation60
In line with the 2030 WHO elimination targets for viral hepatitis,Citation61 the Government of India initiated the National Viral Hepatitis Control Programme, the Swachh Bharat Mission campaign and the National Rural Drinking Water Programme (NRDWP) with an overall objective to raise awareness, reduce morbidity and mortality and provide safe, potable water for all.Citation62–64 Moreover, regulations by the FSSAICitation39 and the Bureau of Indian Standards are available and are continually updated.Citation65 It has become important to ensure that awareness and training programs about regulations related to procedural changes are optimized and communicated to food handlers in a timely manner. Within this context, identifying potential gaps in the knowledge, attitudes, and self-reported practices of food handlers is imperative to refine interventional strategies to promote food safety.
Using the recently published review on the changing HAV epidemiology in IndiaCitation12 with our findings, the evidence could be useful for healthcare providers and policymakers in India to help define hepatitis A prevention strategies, including targeted immunization of risk groups, such as food handlers. For middle-income nations, like India, resource constraints pose an important barrier to provision of and access to medical services such as immunization. Data on the levels of morbidity, comorbidity, and mortality due to hepatitis A are also needed to assess the size of the burden to healthcare systems and society.
The findings of this review must be interpreted with caution due to several limitations. First, reports of outbreaks from different regions are characterized by sociocultural and economic diversity. Second, epidemiological data from the outbreaks were not analyzed to assess whether hygiene and sanitation were indeed the reasons influencing the shift in average age of individuals infected with HAV in the different regions of the country. Despite these limitations, it is noteworthy to mention that most HAV outbreaks in India demonstrate that adolescents and adults were the most common population segment affected by the disease, which testifies to the shifting endemicity in India. This underscores the importance of vaccinating food handlers in India, the majority of whom are themselves adolescents and young adults.
Conclusion
The burden of HAV outbreaks due to improper food handling procedures is substantial and growing in India, with food handlers being primarily exposed to the disease, and transmitting the disease to susceptible individuals. While the current paper focuses on the Indian setting, the principles may be relevant to other countries globally that showcase similar dynamics such as a shifting HAV endemicity (from high to intermediate), improving socio-economic conditions and an increase in overall disposable income to eat outside of the home. In this context, guidelines on the prevention and management of hepatitis A may need to be revised to be more comprehensive in their inclusion of risk groups. Governments of countries should view vaccination as an investment into their preventive health care programs, which would ultimately save on health care spend. Additionally, HCPs need to enhance the standard of care of adults and routinely offer vaccination to eligible individuals.
Contributorship
All authors participated in the design of this review, interpretation of the results; and the development of this manuscript. All authors had full access to the data and gave final approval before submission.
Clinical Trial Registration
NCT Number (www.clinicaltrials.gov) and NA to come.
Declaration of interest
Jaydeep Mazumdar, Ashish Agrawal, Shafi Kolhapure and Anar Andani are employees of the GSK group of companies. Anar Andani holds shares in the GSK group of companies. Jaydeep Mazumdar, Ashish Agrawal, Shafi Kolhapure and Anar Andani and declare no other financial and non-financial relationships and activities. Bhaskar Shenoy declares no financial and non-financial relationships and activities and no conflicts of interest.
Acknowledgments
The authors thank the Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK. Amandine Radziejwoski coordinated the manuscript development and editorial support. Amrita Ostawal (Arete Communication UG) provided medical writing support.
Additional information
Funding
References
- Centers for Disease Control and Prevention. Epidemiology and prevention of vaccine-preventable diseases. Washington (DC): Public Health Foundation. 2015 [accessed 2020 Jul 03]. https://www.cdc.gov/vaccines/pubs/pinkbook/index.html.
- Sinha A, Dutta S. Waterborne & foodborne viral hepatitis: a public health perspective. Indian J Med Res. 2019;150(5):432–8. doi:10.4103/ijmr.IJMR_1430_18.
- World Health Organization. Position paper on hepatitis A vaccines: june 2012. Wkly Epidemiol Rec. 2012. 28-29: 285-286. [accessed 2020 Jan 02]. https://apps.who.int/iris/bitstream/handle/10665/241938/WER8728_29_261-276.PDF;jsessionid=1846D0A5AEEA44B43DA222ADFA369FF1?sequence=1.
- World Health Organization. The immunological basis for immunization series: module 18: hepatitis A. Geneva: World Health Organization; 2019. [accessed 2020 Oct 15]. https://apps.who.int/iris/bitstream/handle/10665/326501/97892516327-eng.pdf?sequence=1&isAllowed=y.
- Randazzo W, Sánchez G. Hepatitis A infections from food. J Appl Microbiol. 2020 [accessed 2020 Jul 03];129:1120–32. doi:10.1111/jam.14727.
- Rakesh PS, Retheesh R, Chandran R, Sadiq A, Ranjitha S. Out-of-pocket expenditure due to hepatitis A disease: a study from Kollam district, Kerala, India. Indian J Med Res. 2017;146(3):426–29. doi:10.4103/ijmr.IJMR_275_16.
- World Health Organization. Estimates of the global burden of foodborne diseases. Geneva (Switzerland): WHO; 2015. [accessed 2020 Apr 15]. https://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf?sequence=1.
- Morey RJ, Collier MG, Nelson NP. The financial burden of public health responses to hepatitis A cases among food handlers, 2012-2014. Public Health Rep. 2017;132(4):443–47. doi:10.1177/0033354917710947.
- Shukla S, Singh SP, Shankar R. Food safety regulatory model in India. Food Control. 2014;37:401–13. doi:10.1016/j.foodcont.2013.08.015.
- Bhattacharya S, Talati S, Gupta A, Malhotra S, Singh A. Implementing a skill development program among food handlers in tertiary care hospital to improve their personal hygiene: a pilot study. J Educ Health Promot. 2019;8:129. doi:10.4103/jehp.jehp_452_18.
- Gripenberg M, Aloysia D’Cor N, L’Azou M, Marsh G, Druelles S, Nealon J. Changing sero-epidemiology of hepatitis A in Asia Pacific countries: a systematic review. Int J Infect Dis. 2018;68:13–17. doi:10.1016/j.ijid.2017.12.021.
- Agrawal A, Singh S, Kolhapure S, Hoet B, Arankalle V, Mitra M. Increasing burden of hepatitis A in adolescents and adults and the need for long-term protection: a review from the Indian subcontinent. Infect Dis Ther. 2019;8(4):483–97. doi:10.1007/s40121-019-00270-9.
- Rakesh PS, Mainu TTCR, Raj A, Babu D, Rajiv M, Mohandas KS, Das A, Balasubramanian A. Investigating a community wide outbreak of hepatitis A in Kerala, India. J Family Med Prim Care. 2018;7(6):1537–41. doi:10.4103/jfmpc.jfmpc_127_18.
- Ministry of Statistics and Programme Implementation - Government of India, UN - World population prospects 2019. Population of India. Internet: statisticTimes.Com; 2020. [accessed 2020 Apr 15]. http://statisticstimes.com/demographics/population-of-india.php.
- Vashishtha VM. Adolescent immunization schedule: need for a relook. Indian Pediatr. 2019;56(2):101–04. doi:10.1007/s13312-019-1479-5.
- Mordor Intelligence. India foodservice market - Growth, trends, and forecast (2020-2025). Hyderabad (India): Mordor Intelligence; [accessed 2020 May 31]. https://www.mordorintelligence.com/industry-reports/india-foodservice-market.
- Chitnis SP. A study on scenario of fast-food industry in India. Int J Trend Sci Res Dev. 2019;Special Issue:88–90. doi:10.31142/ijtsrd23071.
- Statista. Total number of street food stalls/kiosks across India from 2008 to 2013. New York (NY): Statista; 2016. [accessed 2020 Apr 16]. https://www.statista.com/statistics/676715/number-of-street-food-stalls-in-india/.
- Srividhya N. Eating out habit of individuals – an analytical study (with special reference to Puducherry city). IJBMI. 2014;3(6):38–44.
- Ministry of Human Resource Development - Department of Higher Education. All India Survey on Higher Education (2015-16). New Delhi (India): Government of India; 2016. [accessed 2020 Jun 09]. https://mhrd.gov.in/sites/upload_files/mhrd/files/statistics-new/AISHE2015-16.pdf.
- Statista. Passenger traffic in railways across India from financial year 2010 to 2019. New York (NY): Statista; 2019. [accessed 2020 May 31]; Available from: https://www.statista.com/statistics/726386/india-railway-passenger-traffic/.
- National Centre for Disease Control. Food-borne diseases and food safety in India. New Delhi (India): Government of India; 2017. [accessed 2020 Apr 18]. https://ncdc.gov.in/WriteReadData/linkimages/CD%20Alert4053017156.pdf.
- National Centre for Disease Control. Viral hepatitis: the silent disease - Prevention, control and treatment guidelines. New Delhi (India): Government of India; 2016. [accessed 2020 Jun 01]. https://ncdc.gov.in/WriteReadData/l892s/File614.pdf.
- Arora D, Jindal N, Shukla RK, Bansal R. Water borne hepatitis a and hepatitis e in malwa region of punjab, India. J Clin Diagn Res. 2013;7(10):2163–66. doi:10.7860/jcdr/2013/5966.3459.
- Chobe L, Arankalle VA. Investigation of a hepatitis A outbreak from Shimla Himachal Pradesh. Indian J Med Res. 2009;130:179–84.
- Gurav YK, Retheesh Babu G, Vinu KP, Lole KS. Suspected spread of hepatitis A virus from a restaurant among adults in rural area of the Kerala state, India. Epidemiol Infect. 2019;147:e210. doi:10.1017/S0950268819000967.
- Kadri SM, Rehman SU, Rehana K, Benetou DR, Ahmad DF, Abdullah A, Chattu VK. Hepatitis A and E outbreak surveillance during 2015-2017 in Kashmir, India: is the water to blame? J Epidemiol Glob Health. 2018;8(3–4):203–07. doi:10.2991/j.jegh.2018.04.101.
- Kurup K, Ponnaiah M, Gurav YK. Infected food handlers led to an outbreak of hepatitis A in Ernakulam district, Kerala, Southern India, 2016. Clin Epidemiol Glob Health. 2019;8(1):308–12. doi:10.1016/j.cegh.2019.08.001.
- Rakesh P, Sherin D, Sankar H, Shaji M, Subhagan S, Salila S. Investigating a community-wide outbreak of hepatitis a in India. J Glob Infect Dis. 2014;6(2):59–64. doi:10.4103/0974-777X.132040.
- Raveendran S, Rakesh PS, Dev S, Vijayakumar N, Prasannakumar P. Investigation of an outbreak of hepatitis A in a coastal area, Kerala, Southern India. J Prim Care Community Health. 2016;7(4):288–90. doi:10.1177/2150131916647007.
- Zachariah SM, Sreedevi C, Aswathy S, Kokkayil P, Mathews AA. Investigation of hepatitis A outbreak in Palakkad district. Int J Community Med Public Health. 2017;4(11):4125–30. doi:10.18203/2394-6040.ijcmph20174630.
- Arankalle VA, Sarada Devi KL, Lole KS, Shenoy KT, Verma V, Haneephabi M. Molecular characterization of hepatitis A virus from a large outbreak from Kerala, India. Indian J Med Res. 2006;123(6):760–69.
- Chadha MS, Lole KS, Bora MH, Arankalle VA. Outbreaks of hepatitis A among children in Western India. Trans R Soc Trop Med Hyg. 2009;103(9):911–16. doi:10.1016/j.trstmh.2008.11.014.
- Rakesh PS, Mohandas S. 84 outbreaks of Hepatitis A in last five years in Kerala State – are we resigning to fate? Nat J Res Com Med. 2017;6(3):267–70.
- Srinivasan M, Sindhu KN, Kumar SJ, Abraham P, Anandan S, Balaji V, Mohan VR, Kang G, John J. Hepatitis. A outbreak with the concurrence of Salmonella typhi and Salmonella poona infection in children of Urban Vellore, South India. Am J Trop Med Hyg. 2020;102(6):1249–52. doi:10.4269/ajtmh.19-0742.
- World Health Organization. World Health Day 2015: from farm to plate, make food safe. Geneva (Switzerland): WHO; 2015. [accessed 2020 Apr 15]. https://www.who.int/mediacentre/news/releases/2015/food-safety/en/.
- Kumari V, Kapur D. Understanding barriers to compliance to food safety standards in the catering establishments using a qualitative research method: focus group discussion. Int J Sci Res Sci Technol. 2018;4(10):423–40. doi:10.32628/IJSRST18401135.
- Yang H. Food Safety in India: status and Challenges. New Delhi (India): Tata Cornell Institute for Agriculture and Nutrition; 2017. TCI-TARINA Policy Brief No. 5. [accessed 2020 Jul 04]. https://tarina.tci.cornell.edu/wp-content/uploads/2017/11/TCI-TARINA-Policy-Brief-No.5.pdf.
- Food Safety and Standards Authority of India. Food safety and standards regulations. New Delhi (India): Government of India; 2020. [accessed 2020 Jul 05]. https://www.fssai.gov.in/cms/food-safety-and-standards-regulations.php.
- Dudeja P, Singh A, Sahni N, Kaur S, Goel S. Effectiveness of an intervention package on knowledge, attitude, and practices of food handlers in a tertiary care hospital of north India: a before and after comparison study. Med J Armed Forces India. 2017;73(1):49–53. doi:10.1016/j.mjafi.2016.10.002.
- Prabhu PM, Shah RS. A study of food handlers in public food establishments in Maharashtra, India. Int J Sci Res. 2014;3(7):1485–89.
- Manes MR, Kuganantham P, Jagadeesan M, Laxmidevi M, Dworkin MS. A step towards improving food safety in India: determining baseline knowledge and behaviors among restaurant food handlers in Chennai. J Environ Health. 2016;78(6):18–25. quiz 117
- Mukherjee S, Mondal TK, De A, Misra R, Pal A. Knowledge, attitude and practice of food hygiene among street food vendors near a tertiary care hospital in Kolkata, India. Int J Community Med Public Health. 2018;5(3):1206-11. doi:10.18203/2394-6040.ijcmph20180786.
- Singh AK, Dudeja P, Kaushal N, Mukherji S. Impact of health education intervention on food safety and hygiene of street vendors: a pilot study. Med J Armed Forces India. 2016;72(3):265–69. doi:10.1016/j.mjafi.2016.02.008.
- Stuurman AL, Marano C, Bunge EM, De Moerlooze L, Shouval D. Impact of universal mass vaccination with monovalent inactivated hepatitis A vaccines - A systematic review. Hum Vaccin Immunother. 2017;13(3):724–36. doi:10.1080/21645515.2016.1242539.
- Indian Academy of Pediatrics. IAP Guidebook on Immunization 2018-19. New Delhi (India): Jaypee Brothers Medical Publishers; 2020. [accessed 2020 May 30]. https://iapindia.org/pdf/124587-IAP-GUIDE-BOOK-ON-IMMUNIZATION-18-19.pdf.
- Indian Medical Association. Lifecourse immunization: pediatric to geriatric vaccines. Indian Medical Association. [accessed 2020 Jun 10]. http://www.ima-india.org/ima/pdfdata/IMA_LifeCourse_Immunization_Guide_2018_DEC21.pdf
- Expert Group of the Association of Physicians of India on Adult Immunization in India. The Association of Physicians of India evidence-based clinical practice guidelines on adult immunization. J Assoc Physicians India. 2009;57:345–56.
- Nelson NP, Link-Gelles R, Hofmeister MG, Romero JR, Moore KL, Ward JW, Schillie SF. Update: recommendations of the Advisory Committee on Immunization Practices for Use of Hepatitis A Vaccine for Postexposure Prophylaxis and for Preexposure Prophylaxis for International Travel. MMWR Morb Mortal Wkly Rep. 2018;67:1216–20. doi:10.15585/mmwr.mm6743a5.
- Rebmann T, Wilson KD, Loux T, Iqbal AZ, Peters EB, Peavler O. Outcomes, approaches, and challenges to developing and passing a countywide mandatory vaccination policy: St. Louis County’s experience with hepatitis A vaccine for food service personnel. AIMS Public Health. 2016;3(1):116–30. doi:10.3934/publichealth.2016.1.116.
- Alabama Department of Public Health. ADPH recommends hepatitis A vaccine for all food workers. 2019 [accessed 2020 Oct 7]. https://www.alabamapublichealth.gov/news/2019/08/27a.html.
- Nelson NP, Weng MK, Hofmeister MG, Moore KL, Doshani M, Kamili S, Koneru A, Haber P, Hagan L, Romero JR, et al. Prevention of Hepatitis A Virus Infection in the United States: recommendations of the Advisory Committee on Immunization Practices, 2020. MMWR Recomm Rep. 2020;69(RR–5):1–38. doi:10.15585/mmwr.rr6905a1.
- Sharapov UM, Kentenyants K, Groeger J, Roberts H, Holmberg SD, Collier MG. Hepatitis A Infections among Food Handlers in the United States, 1993–2011. Public Health Rep. 2016;131(1):26–29. doi:10.1177/003335491613100107.
- Sri Lanka Medical Association. SLMA Guidelines and Information on Vaccines. Sixth Edition. 2017 [accessed 2020 Oct 5]. https://slma.lk/wp-content/uploads/2017/12/GSK-SLMA-Guidelines-Information-on-Vaccines.pdf.
- Health Service Executive. Immunisation Guidelines. 2020. [Accessed: 2020 Oct 15]. https://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/.
- Dash R, Agrawal A, Nagvekar V, Lele J, Di Pasquale A, Kolhapure S, Parikh R. Towards adult vaccination in India: a narrative literature review. Hum Vaccin Immunother. 2020;16(4):991–1001. doi:10.1080/21645515.2019.1682842.
- Koul P, Swaminathan S, Rajgopal T, Ramsubramanian V, Joseph B, Shanbhag S, Mishra A, Raut S. Adult immunization in occupational settings: A consensus of Indian experts. Indian J Occup Environ Med. 2020;24(1):3–15. doi:10.4103/ijoem.IJOEM_50_20.
- Suwantika AA, Yegenoglu S, Riewpaiboon A, Tu HA, Postma MJ. Economic evaluations of hepatitis A vaccination in middle-income countries. Expert Rev Vaccines. 2013;12(12):1479–94. doi:10.1586/14760584.2013.851008.
- Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine. 2010;28(41):6653–57. doi:10.1016/j.vaccine.2010.08.037.
- Patterson J, Abdullahi L, Hussey GD, Muloiwa R, Kagina BM. A systematic review of the epidemiology of hepatitis A in Africa. BMC Infect Dis. 2019;19(1):651. doi:10.1186/s12879-019-4235-5.
- Waheed Y, Siddiq M, Jamil Z, Najmi MH. Hepatitis elimination by 2030: progress and challenges. World J Gastroenterol. 2018;24(44):4959–61. doi:10.3748/wjg.v24.i44.4959.
- Ministry of Health and Family Welfare. National Viral Hepatitis Control Program. Government of India; 2018. [accessed 2020 Jul 04]. https://www.nhp.gov.in/national-viral-hepatitis-control-program-(nvhcp)_pg.
- Ministry of Drinking Water and Sanitation. Guidelines for Swachh Bharat Mission (Gramin). New Delhi (India): Government of India; 2017. [accessed 2020 Jul 04]. http://swachhbharatmission.gov.in/sbmcms/writereaddata/images/pdf/Guidelines/Complete-set-guidelines.pdf.
- Ministry of Drinking Water and Sanitation. National rural drinking water programme. New Delhi (India): Government of India; 2013. [accessed 2020 Jul 04]. https://pib.gov.in/newsite/mbErel.aspx?relid=100016.
- Bureau of Indian Standards. The National Standards Body of India. Government of India; 2019. [ccessed 2020 Jul 04]. https://bis.gov.in/index.php/the-bureau/about-bis/.