ABSTRACT
The influenza vaccine is not included in China’s national immunization program. Here, we assessed influenza vaccine coverage among Shanghai residents and estimated the impacts of the coronavirus disease 2019 (COVID-19) epidemic and a hypothetical free vaccine strategy on the willingness of participants to receive influenza vaccines. The coverage of influenza vaccines among Shanghai residents from 2015 to 2019 was 1.4% (range: 1%–2.4%). A total of 792 adult participants (aged 19–59 years) along with 821 children and 445 older individuals were included in the analysis. The willingness of participants to receive influenza vaccines reached 68.4% following the COVID-19 epidemic. Furthermore, if the vaccine was made available at no cost, 85.9% of participants were willing to be vaccinated. Our data indicated that influenza vaccine coverage is extremely low in Shanghai but that more than two-thirds of participants were willing to receive influenza vaccines following the COVID-19 epidemic. Making influenza vaccines available for free could further increase coverage.
Introduction
Coronavirus disease 2019 (COVID-19) has become a global pandemic. As the initial symptoms of influenza and COVID-19 are similar, interest in a safe and moderately effective influenza vaccine has increased dramatically in the absence of a COVID-19 vaccine.Citation1 It was reported that seasonal influenza vaccination among older individuals could prevent a proportion of COVID-19 morbidity and mortality.Citation2 The possibility of a simultaneous seasonal influenza epidemic during the COVID-19 epidemic has made widespread influenza vaccination more important than ever.Citation3
Most individuals are generally susceptible to influenza viruses.Citation4 The World Health Organization (WHO) recommends annual influenza vaccination because of the short period of vaccine-induced protective immunity and the need to adjust vaccine antigen composition each year.Citation4 Influenza vaccination is not included in the national immunization program in China and influenza vaccination coverage was extremely low (1.5–2.2%) from 2004 to 2014.Citation5 Many factors influence willingness to be vaccinated for influenza, such as knowledge of influenza and influenza vaccines, perceived seriousness of influenza, perceived benefits of vaccination, perceived susceptibility, costs of vaccination, and receipt of prior seasonal influenza vaccinations.Citation6–10 Changes in risk perception following the COVID-19 pandemic may also influence parents’ plans to vaccinate their children against influenza.Citation11 To our knowledge, there have been no studies of the effects of the COVID-19 epidemic and vaccine costs on the willingness of Chinese residents to receive influenza vaccination. Therefore, we conducted a survey in Shanghai, China, to assess adult participants’ willingness to accept influenza vaccines for themselves, as well as children or older individuals living with them, in the post-COVID-19 era.
Methods
From 1 July to 20 August 2020, adults (aged 19–59 years) who visited community health centers in Xuhui District, Shanghai to obtain vaccination services for themselves or for their children or older individuals in their households were asked to complete self-administered questionnaires by scanning quick response (QR) codes with their phones. As children and older individuals are at high risk for influenza,Citation4 participants responded for themselves and on behalf of any children (aged 0–18 years) or older individuals (aged ≥60 years) living with them. Participants with multiple children or older individuals living in their households responded once on behalf of all children and once on behalf of all older individuals. The survey included questions on influenza vaccination status during the 3 years prior to the COVID-19 epidemic and willingness to receive influenza vaccines during the influenza season following outbreak of the COVID-19 epidemic. When participants indicated their willingness to receive the influenza vaccine, they were informed that there was a fee for the vaccine. We also listed the prices of licensed trivalent and quadrivalent inactivated influenza vaccines in China (about 5.2 USD–10.1 USD and 18.6 USD–19.1 USD, respectively). We also investigated willingness to receive influenza vaccines if the vaccines were covered by the national immunization program (free of charge). Influenza vaccination coverage among Shanghai residents from 2015 to 2019 was estimated based on vaccination records in the Shanghai Immunization Information System. Differences among groups were compared using the chi-square test. Values of p < .05 were considered statistically significant. All statistical analyses were carried out using SPSS 18.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism 8 (GraphPad Inc., San Diego, CA, USA) was used to prepare histograms.
Results
A total of 1,456 individuals accessed the questionnaire by scanning the QR code during the study period. Only 794 valid questionnaires were obtained, yielding an overall response rate of 54.5%. Two participants who had no knowledge of COVID-19 were excluded from the analysis. Of the remaining 792 participants, the average (± standard deviation) age was 33.3 ± 7.1 years and the majority were female (77.5%). In addition, 821 children and 445 older individuals living with the 792 participants were included in analyses of willingness to be vaccinated against influenza.
Sixty-three participants (8.0%) reported that they had been vaccinated at least once against seasonal influenza during the 3 years prior to the COVID-19 epidemic. Participants also reported that 64.8% of children and 31.2% of older individuals had received influenza vaccines in the last 3 years (). The estimated 5-year average influenza vaccination coverage among Shanghai residents from 2015 to 2019 was 1.4% (range: 1.0–2.4%). Coverage among children, older individuals, and adults was 5.5% (37,153/677,158), 1.3% (20,554/1,504,081), and 0.3% (6,684/2,424,458), respectively.
Figure 1. Comparison between self-reported influenza vaccination status before the coronavirus disease 2019 (COVID-19) epidemic and willingness to receive influenza vaccines after the COVID-19 epidemic or under a hypothetical free vaccine strategy among four groups of residents in Shanghai, China. Three asterisks (***) indicates a statistically significant difference between two groups (p < .001). † Influenza vaccination status before the COVID-19 epidemic and willingness to receive influenza vaccines were reported on the behalf of these groups by study participants
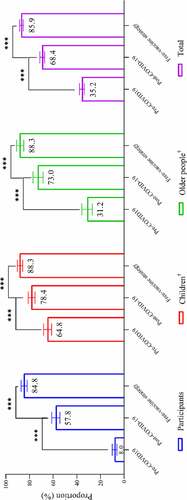
Following the COVID-19 epidemic, the willingness of participants to receive influenza vaccines during the coming influenza season reached 68.4%, higher than self-reported coverage before the COVID-19 epidemic (68.4% vs. 35.2%, chi-square = 467.9, p < .001). Compared with the pre-epidemic period, willingness to receive influenza vaccines increased significantly following the COVID-19 epidemic among participants (57.8% vs. 8.0%, chi-square = 446.3, p < .001), their children (78.4% vs. 64.8%, chi-square = 37.6, p < .001), and older individuals in their households (73.0% vs. 31.2%, chi-square = 155.8, p < .001) (). Furthermore, if influenza vaccines were made available at no cost, the willingness of participants, their children and older adults living with them, to become vaccinated further increased to 85.9%. This represented a significant increase compared with vaccination in the absence of such a strategy (85.9% vs. 68.4%, chi-square = 187.5, p < .001).
Discussion
COVID-19 is still a global pandemic, but the local epidemic in Shanghai has been brought under control by strong preventive and control measures in China.Citation12 Perhaps because no COVID-19 vaccine is yet available, 68.4% of participants were willing to receive an influenza vaccine in the season following the COVID-19 epidemic in Shanghai, China. Willingness to receive influenza vaccination increased further to 85.9% if the vaccine was included in the national immunization program.
It should be noted that although 35.2% of participants self-reported having received at least one dose of influenza vaccination within the last 3 years, the estimated 5-year average coverage of influenza vaccination among Shanghai residents was only 1.4%. This discrepancy may have at least three explanations. First, because influenza vaccines need to be formulated annually, self-reported coverage included any individual who received even one dose during the 3-year period. Second, recall bias may act to inflate vaccine coverage. Third, the high influenza vaccination coverage self-reported among participants may have reflected a biased sample; our study was not population-based, and only included individuals who visited community health centers as well as children and older adults living with them. Influenza vaccination coverage among Shanghai residents was similar to the national level,Citation5 but significantly lower than coverage in Beijing (20.6%) where influenza vaccines are included in local immunization procedures.Citation10 Influenza vaccine coverage in our study was lower than that in countries of two WHO regions (EURO and AMRO: 112–271 doses distributed per 1000 population in 2015).Citation13 It was reported that only 5% of influenza vaccine doses were distributed to 50% of the world’s population, including China.Citation13 However, following the COVID-19 epidemic, willingness to receive influenza vaccines among participants in our study was only slightly lower than in Australia (68.4% vs. 76.5%), where the influenza vaccine is included in the national immunization program.Citation14 Therefore, rapidly increasing willingness to receive influenza vaccines may pose challenges for influenza vaccine manufacturers, vaccine cold-chain transportation, and vaccinators. Fortunately, China has experience of working to vaccinate large numbers of people in a short period. Examples include the H1N1 vaccination campaign in 2009Citation15 and the measles vaccination campaign in 2010.Citation16
In China, the effectiveness of inactivated influenza vaccines against influenza-like illness was about 42–47%.Citation4 Therefore, the benefit of influenza vaccination during the COVID-19 epidemic is to enable a proportion of individuals to avoid influenza infection, thereby reducing risk of contracting COVID-19 in hospitals by decreasing the number of medical visits. In addition, vaccination may reduce the psychological burden associated with development of nonspecific febrile symptoms during the COVID-19 epidemic. With increased vaccine coverage, hospitals could also significantly reduce the numbers of patients with influenza-like illnesses that need to be screened for COVID-19, improving the specificity of COVID-19 surveillance. Therefore, it is recommended that the influenza vaccine be made available to residents free of charge to increase coverage, especially among older individuals who are at high risk for both influenza and COVID-19.Citation2,Citation4 Fortunately, our study found that although older people were slightly less likely to be vaccinated against influenza following the COVID-19 epidemic than children (73.0% vs. 78.4%), they were significantly more likely to be vaccinated than adults (73.0% vs. 57.8%). This finding is in line with trends in influenza vaccine coverage among children, older individuals and adults in Shanghai: children have the highest coverage (5.5%), followed by the elderly (1.3%) and then by adults (0.3%). The results of our study will help guide government departments in making influenza vaccination decisions, especially in three WHO regions (EMRO, AFRO and SEARO) where the supply of influenza vaccines only accounted for about 5% of global distribution.Citation13
Our study had several limitations. First, the participants sampled here may have represented a biased subset of Shanghai residents. Analysis of vaccination coverage and vaccination strategy suggested that our observations might be difficult to generalize to other countries or regions, especially WHO regions with much higher vaccine distribution and uptake (AMRO, EURO and WPRO).13 Second, participants responded on their willingness to receive influenza vaccines for their children or older individuals living in their households, which may not provide a true reflection of the willingness of children and older adults to be vaccinated. Third, participants’ self-reported coverage was significantly higher than the estimated 5-year average coverage among Shanghai residents in this study, and thus our results may have overestimated willingness to be vaccinated. Fourth, our study only evaluated the impact of the COVID-19 epidemic and vaccine costs on willingness to receive influenza vaccines and did not consider other factors. However, our data contribute novel and timely evidence of the need for influenza vaccination following the COVID-19 epidemic. There are very limited data on this topic.
In conclusion, nearly two-thirds of participants in our study were willing to receive influenza vaccines following the COVID-19 epidemic. If this finding is representative of Shanghai as a whole, demand for influenza vaccines will pose a significant challenge for manufacturers, vaccine cold-chain transportation, and vaccinators owing to the currently low coverage of influenza vaccination among Shanghai residents. It is recommended that a free vaccination strategy should be implemented among residents, especially older individuals and children, which would also significantly increase influenza vaccine coverage.
Disclosure of potential conflicts of interest
All of the authors declared no conflict of interests.
Additional information
Funding
References
- Paguio JA, Yao JS, Dee EC. Silver lining of COVID-19: heightened global interest in pneumococcal and influenza vaccines, an infodemiology study. Vaccine. 2020;38(34):5430–35. doi:10.1016/j.vaccine.2020.06.069.
- Thindwa D, Garcia Quesada M, Liu Y, Bennett J, Cohen C, Knoll MD, von Gottberg A, Hayford K, Flasche S. Use of seasonal influenza and pneumococcal polysaccharide vaccines in older adults to reduce COVID-19 mortality. Vaccine. 2020;38:5398–401. doi:10.1016/j.vaccine.2020.06.047.
- Belongia EA, Osterholm MT. COVID-19 and flu, a perfect storm. Science. 2020;368:1163. doi:10.1126/science.abd2220.
- National Immunization Advisory Committee (NIAC) Technical Working Group (TWG), Influenza Vaccination TWG. Technical guidelines for seasonal influenza vaccination in China, 2019–2020. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(11):1333–49. doi:10.3760/cma.j.issn.0254-6450.2019.11.002. PMID: 31838802.
- Yang J, Atkins KE, Feng L, Pang M, Zheng Y, Liu X, Cowling BJ, Yu H. Seasonal influenza vaccination in China: landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine. 2016;34:5724–35. doi:10.1016/j.vaccine.2016.10.013.
- Brien S, Kwong JC, Buckeridge DL. The determinants of 2009 pandemic A/H1N1 influenza vaccination: a systematic review. Vaccine. 2012;30:1255–64. doi:10.1016/j.vaccine.2011.12.089.
- Shahrabani S, Benzion U, Yom Din G. Factors affecting nurses’ decision to get the flu vaccine. Eur J Health Econ. 2009;10:227–31. doi:10.1007/s10198-008-0124-3.
- Teitler-Regev S, Shahrabani S, Benzion U. Factors affecting intention among students to be vaccinated against A/H1N1 influenza: a health belief model approach. Advances in Preventive Medicine. 2011;2011:353207. doi:10.4061/2011/353207.
- Tsutsui Y, Benzion U, Shahrabani S, Din GY. A policy to promote influenza vaccination: a behavioral economic approach. Health Policy. 2010;97:238–49. doi:10.1016/j.healthpol.2010.05.008.
- Wu S, Su J, Yang P, Zhang H, Li H, Chu Y, Hua W, Li C, Tang Y, Wang Q. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: a large, population-based survey in Beijing, China. BMJ Open. 2017;7(9):e017459. doi:10.1136/bmjopen-2017-017459.
- Goldman RD, McGregor S, Marneni SR, Katsuta T, Griffiths MA, Hall JE, Seiler M, Klein EJ, Cotanda CP, Gelernter R, et al. Willingness to Vaccinate Children against Influenza after the Coronavirus Disease 2019 Pandemic. The Journal of Pediatrics. 2021;228:87–93. doi:10.1016/j.jpeds.2020.08.005.
- Tu H, Tu S, Gao S, Shao A, Sheng J. Current epidemiological and clinical features of COVID-19; a global perspective from China. J Infect. 2020;80:1–9. doi:10.1016/j.jinf.2020.04.011.
- Palache A, Abelin A, Hollingsworth R, Cracknell W, Jacobs C, Tsai T, Barbosa P. force IIVSt. Survey of distribution of seasonal influenza vaccine doses in 201 countries (2004-2015): the 2003 World Health Assembly resolution on seasonal influenza vaccination coverage and the 2009 influenza pandemic have had very little impact on improving influenza control and pandemic preparedness. Vaccine. 2017;35:4681–86. doi:10.1016/j.vaccine.2017.07.053.
- Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ, Ayre J, Batcup C, Copp T, Cornell S, Dakin T. Sydney Health Literacy Lab C-g. Willingness to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases. 2020. doi:10.1016/S1473-3099(20)30559-4.
- Liang XF, Li L, Liu DW, Li KL, Wu WD, Zhu BP, Wang HQ, Luo HM, Cao LS, Zheng JS, et al. Safety of influenza A (H1N1) vaccine in postmarketing surveillance in China. The New England Journal of Medicine. 2011;364:638–47. doi:10.1056/NEJMoa1008553.
- Ma C, Gregory CJ, Hao L, Wannemuehler KA, Su Q, An Z, Quick L, Rodewald L, Ma F, Yan R, et al. Risk factors for measles infection in 0-7 month old children in China after the 2010 nationwide measles campaign: A multi-site case-control study, 2012-2013. Vaccine. 2016;34:6553–60. doi:10.1016/j.vaccine.2016.02.002.
