ABSTRACT
Background: Over the past few years, measles cases have increased worldwide, despite the availability of a safe and highly effective vaccine. Numerous countries have eliminated measles or have made substantial advancements toward elimination.
Materials and Methods: This study investigated the seroprevalence of anti-measles antibodies and vaccination status among 362 men and 81 women in Madinah. All participants were vaccinated or acquired immunity naturally due to infection. We aimed to examine the persistence of anti-measles IgG antibodies, which were qualitatively and quantitatively determined using ELISA.
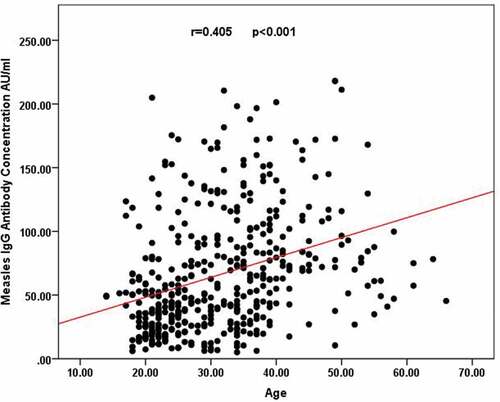
Results: We showed that measles seropositivity (92%, n = 408) was significantly more frequent than negative (5.4%, n = 14) and equivocal results (2.5%, n = 11). Among men, 92.8% were seropositive for the anti-measles IgG antibody, whereas 88.9% of women were seropositive. In addition, a significant relationship was observed between age and measles seropositivity, with a significant positive correlation between age and anti-measles antibody concentration as assessed by Spearman’s correlation analysis (r = 0.405, p < .001).
Conclusion: Based on these results, observing the serological status of the population 20–38 y after vaccination may be necessary to minimize the proportion of individuals who may be vulnerable to contracting measles. Despite the efficacy of the measles, mumps, and rubella vaccine and the positive global impact associated with the use of this vaccine, including a general decline in measles cases, attention must still be paid to the issue of measles risk, and seronegative individuals should be identified and advised to receive a booster dose of the vaccine.
Introduction
Measles virus (Morbillivirus) spreads from person to person through airborne transmission. Prior to vaccine development, greater than 90% of individuals experienced measles infections during childhood. Infants are protected by maternal antibodies that diffuse transplacentally during the first few months following delivery, after which individuals become vulnerable to the infection.Citation1
Measles is a highly transmissible viral disease characterized by fever, malaise, rash, cough, coryza, and conjunctivitis. Measles is best prevented by vaccination, and large reductions in measles incidence and mortality have focused attention on the potential for regional eradication and global abolition.Citation2 Transmission can also occur through person-to-person contact, in addition to airborne spread. The respiratory secretions from a measles patient, in the form of contagious droplets, can persist in airborne form for up to 2 hours. Consequently, the infection may also spread in public places.Citation3
Provisional records from the World Health Organization (WHO) have shown that during 2019, more measles cases were reported internationally than in any year since 2006. More than 500,000 positive measles cases were reported in more than 178 countries, some associated with widespread measles epidemics. The most recent data available, for 2018, suggested that more than 140,000 individuals died due to measles (https://www.cdc.gov/globalhealth/measles/globalmeaslesoutbreaks.htm accessed on 10–10-2020).
In 1974, the Expanded Program on Immunization (EPI) was unveiled by the WHO, which aimed to achieve the worldwide vaccination of children against several diseases, including tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, and measles. In 1990, approximately 80% of all children born worldwide were likely to have obtained vaccines that targeted these infectious diseases.Citation4 Concurrently with the introduction of the EPI program, a better standard of living and improved health care was reported throughout Saudi Arabia, and a Royal decree was enacted that all children were required to obtain vaccinations, which was a condition for obtaining their birth certificates.Citation5 Hence, in Saudi Arabia, every newborn is issued a birth certificate only at the age of 1 y or above, that is, after obtaining vaccinations.
The intermittent outbreak of measles among immunized older children has been reported in diverse nations, and the causes of some of these cases have been identified to clarify the reasons for vaccine failure. In 1991, a similar outbreak of measles was reported in the Al-Qassim region of Saudi Arabia.Citation6
Epidemiological studies have shown that measles outbreaks continue to occur globally, and measles remains a prominent cause for mortality, particularly among children younger than 5 y of age.Citation7 Accurate global prevalence assessments are difficult to acquire due to differences in surveillance methods and the likely under-reporting of measles incidence.Citation8
Natural measles infection is generally believed to result in permanent immunity. Immunity associated with the receipt of the measles vaccination is also thought to be highly protective against infection. For example, during an outbreak in the Netherlands, unvaccinated individuals were several times more likely to develop infections compared with vaccinated individuals.Citation9
Sporadic measles infections within Saudi Arabia have been reported by several studies, including outbreaks in Tabuk,Citation10 Al-Qassim,Citation11 and, more recently, in Jeddah in 2018 among a Myanmar resident population.Citation12
The measles vaccination recommendations in Saudi Arabia have undergone several adjustments since the 1970s. A mono dose injection was recommended in the 1970s and 1980s, which was revised to a 2-dose program, in the 1990s, with a mono dose recommended at 6 months, and the measles, mumps, and rubella (MMR) vaccine recommended at 12 months. From 1998–2000, a national MMR campaign was directed at school-aged children.Citation13 Starting in 1982, the administration of the measles vaccination became prerequisite to obtain a child’s birth certificate. As a result, vaccination coverage increased dramatically, from 8% to 80% and then to more than 90% in 1980,1984, and 1990, respectively.Citation14 This increase in measles vaccination has also had a key positive influence on other infant vaccination programs and has decreased the occurrence of measles from 46,115 cases per year to fewer than 1,000 cases per year by 2001.Citation15
The shift from immunity acquired through natural exposure to the measles virus to that induced as a result of vaccination needs to be continuously monitored.Citation16 There is dearth of studies on the seroprevalence of measles antibodies in the holy city of Madinah, a hub to pilgrims from across the globe. The objective of this study was to determine the current seroprevalence of antibodies against measles virus in a population of Madinah, Saudi Arabia. Further, to evaluate the efficacy of measles vaccination programs, the population immunity was assessed, prior to and post introduction of measles vaccine by monitoring the serological status in people of different age groups. Our results may have important implications for the health-care policymakers of Saudi Arabia in lowering the proportion of individuals at possible risk of infection in the future in order to successfully achieve measles elimination.
Materials and methods
Study population
This cross-sectional study was conducted from August 2019 to March 2020. A total of 443 healthy Saudi adult participants, including 362 men and 81 women were recruited among blood donors at the central blood bank, Madinah, Saudi Arabia. On average, nearly 90 individuals donate their blood to the central blood bank every day. During the recruitment process, every fifth person from the donor list was invited to participate in the study. The men outnumbered the women who were not as keen to participate in the serological survey as men. Participants were categorized into age groups according to the history of the measles and MMR vaccination recommendations in Saudi Arabia, as follows:1) Individuals born before 1982 (before mandatory measles vaccination); 2) individuals born between 1982–1990 (received mandatory measles vaccination but not MMR vaccination); 3) individuals born between 1991–2000 (1 dose of MMR vaccination); and 4) individuals born after 2001 (2 doses of MMR vaccination). Using G power, version 3.1, the sample size was determined and at least 322 participants were estimated to be sufficient to achieve a power of 0.8, an alpha of 0.05, and a medium effect size. After informed consent was obtained from each subject, blood samples were collected and stored in 5-ml vacutainer serum tubes. Blood samples collected from participants at the Regional Blood Bank, Madinah were immediately transported to the Virology Research Laboratory of the College of Applied Medical Sciences, Taibah University, for further processing. Samples were centrifuged for 15 minutes at 2,500 RPM within 1 hour of collection using a regular routine centrifuge. Sera was then quickly transferred to plastic screw-cap vials and frozen at −20°C until analysis.
Ethical approval
This study was conducted in compliance with relevant national regulations, institutional policies, and the tenets of the Helsinki Declaration. The study was approved by the Research Ethical Committee of Taibah University.
Enzyme-linked immunosorbent assay (ELISA)
Indirect ELISA for the concurrent qualitative and quantitative detection of measles IgG antibodies was performed using the commercial Human ELISA Kits (Human, Wiesbaden, Germany), according to the manufacturer’s instructions. On each plate, the blanks, negative, and positive controls provided with the kits were included for assay quality control. All washing steps were performed using a semi-automated ELISA washer and reader (Biotek, Winooski, US), according to the manufacturer’s instructions.
Serum samples were initially diluted 1:100 with dilution buffer and mixed thoroughly. The cutoff values for anti-measles IgG antibodies were calculated, and the results were evaluated qualitatively as either positive, negative, or equivocal. According to the manufacturer’s instructions, samples with optical densities greater than or equal to 15% above the cutoff value were considered to be positive, samples with optical densities less than 15% below the cutoff value were considered negative, and samples within 15% above or below the cutoff value were considered equivocal. The IgG antibody concentration values for measles were calculated according to the optical density values and were expressed in human units per liter (AU/ml).
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (IBM SPSS Statistics version 25; Armonk, NY, USA) with a significance level set at p ≤ 0.05, using 95% confidence intervals (CIs). Descriptive statistics (mean ± standard deviation (SD)) were calculated to describe quantitative variables. The Kruskal–Wallis test was used to detect significant differences among more than two groups of non-normally distributed quantitative data, whereas the Mann–Whitney U test was used to detect significant differences between two independent groups. Participants were divided into four age groups (younger than 20 y, 20–29 y, 30–38 y, and older than 38 y). Qualitative variables were described using frequency and percentage. Cross tabulation and Chi-square analysis or Fisher’s exact test were used, where appropriate, to test independence among qualitative variables. Spearman’s rank correlation coefficient and scatter plots were used to detect and illustrate the correlations between age and IgG antibody concentrations. Logistic regression analysis was conducted to examine the effect of the age grouping and sex on the status of measles immunization.
Results
Demographic characteristics of the study subjects
In this study, 443 Saudi participants who presented at the Regional Blood Bank, Madinah and gave their consent to participate in the serological survey were recruited, including 362 (81.7%) men and 81 (18.3%) women. The mean age of the study participants was 31.8 ± 9.9 y (mean ± SD), and men were slightly older than women, with mean ages of 32.5 ± 10.2 and 28.5 ± 7.1, respectively. According to measles vaccination history, the participants were stratified into four age groups: older than 38 y (22.6%, n = 100), 30–38 y (31.6%, n = 140), 20–29 y (39.1%, n = 173), and younger than 20 y (6.8%, n = 30, ).
Table 1. Demographic characteristics of study participants (n = 443)
Analysis of specific anti-measles IgG antibody detection and sex
The anti-measles IgG antibody analysis showed that participants were significantly more likely to be categorized as seropositive (92.1%, n = 408, p < .001) than as categorized as seronegative (5.4%, n = 24) or equivocal (2.5%, n = 11).
Among men, 92.8% were seropositive for the anti-measles IgG antibody, whereas 88.9% of females were seropositive. No significant difference was observed between sex for anti-measles IgG antibody concentrations (p = .384, ).
Table 2. Distribution of measles serological status by gender (n = 443)
Distribution of anti-measles IgG antibodies among age groups
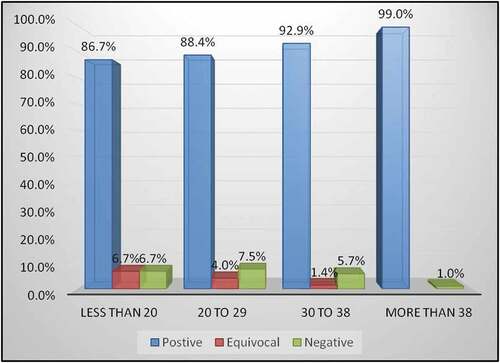
The distribution of seropositivity for the measles IgG antibodies in each age group is presented in . The highest seropositivity for IgG antibodies, 99%, was observed for the older than 38 y group (95% confidence interval (95% CI): 97%–100%). Among the participants in the 30–38 y group, 92.9% (95% CI: 88.6%–97.2%) were seropositive. In the 20–29 y group and the younger than 20 y group, 88.4% (95% CI: 83.6%–93.2%) and 86.7% (95% CI: 74.5%–98.9%), respectively, were seropositive for anti-measles IgG antibody. In addition, a significant (p = .019) directional relationship was observed between age and measles seropositivity, which indicated that the frequency of seropositivity for the anti-measles IgG antibody among our participants increased with age, resulting in the observed age-dependent pattern ().
Table 3. Age group distribution of serological status for measles IgG antibodies (N = 443)
Figure 1. Prevalence of anti-measles IgG seropositivity by age group. In the absence of access to vaccination records, the individuals were stratified into vaccinated and un-vaccinated groups depending on their age and probable vaccination history. A significant directional relationship was observed between age groups and seropositivity for anti-measles IgG antibody (p = .019). Age group frequencies: > 38 (n = 100), 30–38 (n = 140), 20–29 (n = 173), and < 20 (n = 30)
Differences between vaccinated and non-vaccinated individuals
Another relationship was observed between measles seropositivity and vaccination status. Seropositivity for measles was 90.1% (309/343) among vaccinated individuals and 99% (99/100) among unvaccinated individuals (p = .010, ). The levels of anti-measles IgG antibodies were also quantitatively evaluated. shows the comparison between anti-measles IgG antibody concentrations in vaccinated and non-vaccinated individuals. These results indicated that the highest anti-measles IgG antibody concentrations were associated with natural infection, rather than with vaccination. Interestingly, we found that the median anti-measles IgG antibody concentration among the vaccinated older than 38 y group was 82.19 AU/ml, which was significantly higher (p < .001) than the concentrations observed for the unvaccinated groups younger than 20 y (49.09 AU/ml), 20–29 y (37.50 AU/ml), and 30–38 y (62.75 AU/ml). The 30–38 y group had an antibody concentration that was significantly higher than those for the younger than 20 y and 20–29 y groups (p = .019 and p = .001, respectively). However, no significant difference was observed between the younger than 20 y and 20–29 y groups (p = .715).
Figure 2. Prevalence of anti-measles IgG seropositivity by vaccination history. A significant relationship was detected between vaccination status and seropositivity for anti-measles IgG antibody (p = .010 by Fisher’s exact). Born before 1982 (n = 100), Born after 1982 (n = 343)
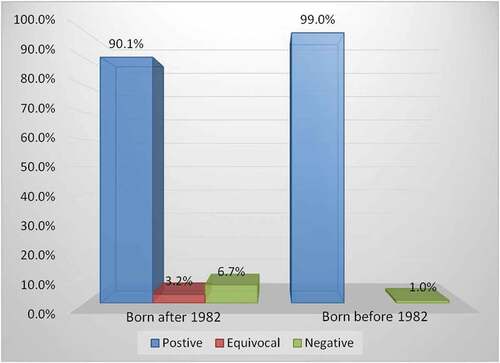
Figure 3. Concentrations of anti-measles IgG antibodies for each age group among vaccinated and non-vaccinated individuals. The median for each age group is indicated by the horizontal line inside the box, which represents the 50% percentile. The 25% and 75% percentiles are indicated by the lower and the upper ends of each box, respectively, and the distance between the two percentiles represents the interquartile range (IQR), which is a measure of the dispersion of values. The ends of the whiskers represent 1.5 times the IQR. Extreme values that occur outside the box and whiskers are considered to be outliers and are indicated by small dots. Age group frequencies: > 38 (n = 100), 30–38 (n = 140), 20–29 (n = 173), and < 20 (n = 30)
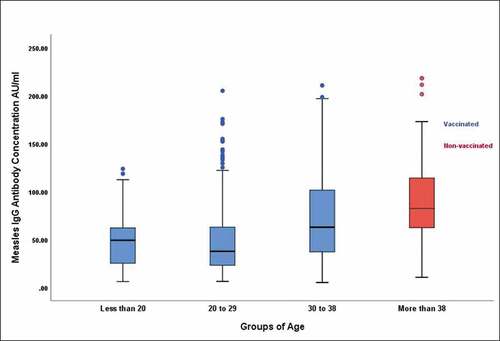
Overall, the median IgG antibody concentration among unvaccinated individuals was significantly higher than the median IgG antibody concentration among vaccinated individuals (82.19 vs. 45.13 AU/ml, p = .001). In addition, the highest values for anti-measles IgG antibody concentration were most likely to be observed in the vaccinated 20–29 y group, compared with the other vaccinated age groups.
Interestingly, we observed a significant positive correlation between age and anti-measles IgG antibody concentrations using Spearman’s rank correlation (r = 0.405, p < .001, ).
Multiple logistic regression analysis
The logistic regression was performed to test the effect of age groups and sex on seropositivity of measles. The positive status was stated as reference, females compared to males, and age groups were compared to the age group (more than 38). presents logistic regression derived odd ratios (OR) and related 95% confidence intervals (CI). The model showed that the younger than 20 y group had a higher probability of being equivocal than other age groups (OR = 7.89; 95% CI: 0.68–91.74), while the probability of being seronegative is lower in the 30–38 y group than other age groups (OR = 5.71; 95% CI: 0.70–46.58). Females had a lower probability of being equivocal than males (OR = 0.78; 95% CI: 0.16–3.70) and a higher probability of being seronegative than males (OR = 1.68; 95% CI: 0.66–4.23).
Table 4. Multivariate logistic regression: effect of the age grouping and sex on measles immunization status
Discussion
Measles morbidity and mortality have been declining due to the implementation of several official global initiatives, such as the EPI, as an enhanced vaccination approach,Citation8 and in several countries, the disruption of local measles transmission has been reported (https://www.euro.who.int/en/media-centre/sections/press-releases/2019/measles-in-europe-record-number-of-both-sick-and-immunized accessed on 10–10-2020). Additionally, the eradication of measles remains a high priority worldwide. Fortunately, the Saudi government has initiated and supported legislative actions to achieve a better standard of living and improved health care throughout the country. One very crucial law was the implementation of the Royal decree, which states all children are required to receive their vaccinations as a condition for obtaining their birth certificates.Citation5 As a result, a noticeable decline in measles cases has been documented in this country.
Several countries globally have suffered from recent measles outbreaks. As of 5 November 2019, 413,308 definite cases of measles have been reported to the WHO, which exceeds the formal monthly record reported by all 187 Fellow States in 2019 (https://www.who.int/csr/don/26-november-2019-measles-global_situation/en/accessed on 10–10-2020). Unfortunately, measles case numbers are likely to be underreported; therefore, the reported number of definite cases globally might not reveal the true extent of measles cases throughout the world. Based on information relayed by official databases, such as those maintained by the WHO and CDC, not all the countries report the cumulative cases or outbreaks that occur within their borders. And hence, it will not give a conclusive theme about the actual affliction on governments. In addition, no data is currently available regarding the vaccine coverage for a considerable number of Asian and African countries.Citation17
In addition to insufficient vaccination, even in some high-income European countries, studies have verified that some vaccinated individuals remain seronegative, even after receiving the vaccine.Citation18 Consequently, a growing number of individuals are vulnerable to measles infection.Citation19 Therefore, we aimed to investigate the persistence of the memory humoral immune response among the population in Madinah, Saudi Arabia. Our findings have suggested that the laboratory verification of response to measles virus infection represents a crucial element of surveillance that is essential for supporting measles control and eradication plans. Moreover, an approach involving rigid control measures and routine vaccination programs should be adopted to minimize the possibility of national epidemics.
Our results revealed a high seroprevalence of anti-measles antibodies among adult Saudi participants, which serves as an indicator of the continued effectiveness of the vaccine among this population; however, the percentage of seronegative individuals identified is a matter of concern. As has been reported for mumps vaccine, whether the decline in the humoral immunity was due to an initial lack of response to the vaccine (identified as primary vaccine failure) or due to a declining immune response over time, referred to as waning immunity (identified as secondary vaccine failure) has not yet been investigated thoroughly.Citation20,Citation21 Moreover, the low-avidity of the measles IgG antibody has resulted in the reinfection of several individuals in the United States.
The assessment of measles-specific humoral immunity several years after vaccination and the impact of demographic variables, such as race, ethnicity, sex, and age, on antibody concentrations are of significant consequence for measles vaccine-related investigations. We used the logistic regression to test the effect of age groups and sex on seropositivity of measles.Citation22 We found no significant difference between anti-measles IgG antibody concentrations according to sex, which agrees with the results of a previous study that showed no significant correlation between antibody titers and demographic variables, including sex and ethnicity.Citation23
Compulsory measles vaccinations, comprising of one dose of the Schwartz vaccine, were announced in Saudi Arabia in 1982 by the Royal decree and became a prerequisite for obtaining a birth certificate. Consequently, vaccination coverage increased from 8% in 1980 to 80% in 1984 and to more than 90% in 1990.Citation24
Our results showed that seroprevalence was the highest among individuals older than 38 y who were born during the pre-vaccination period, prior to the routine vaccination against measles. Most likely, nearly everyone in this age group had acquired measles during childhood and, consequently, were expected to have developed immunity due to natural infection. People aged 30–38 y were much more likely to have received the routine single-dose measles vaccination. The 20–29 y group was most likely to have received a single dose of MMR, whereas those younger than 20 y were most likely to have received two doses of the MMR vaccine. The latter group showed the lowest rates of anti-measles antibody positivity.
Our data is consistent with a similar study conducted in China, with a slight difference in the age groups examined (the oldest group was older than 40 y, whereas ours were older than 38 y). The study in China found that people across three age groups demonstrated reduced levels of anti-measles antibody positivity compared with those aged older than 40 y, who most likely acquired immunity from natural infection.Citation25 Our results were also consistent with those obtained by Coppeta et al., who found that the highest proportion of seropositivity and the highest anti-measles IgG antibody concentrations were found in a group of health workers born before 1982.Citation26
Similar to reports by other researchers, our data showed that the equivocal frequency was high among all vaccinated age groups, and in individuals aged younger than 20 and 20–29 y, seroprevalence fell with age, accompanied by a rise in the proportion of individuals with equivocal titers. These findings indicate that lower antibody levels are produced after vaccination (or a rapid antibody loss occurs) compared with exposure to the virus through natural infection. Consequently, fading vaccine-induced immunity is likely to result in reduced measles control.Citation25,Citation27,Citation28 This assumption could be supported incidentally by the increase in measles outbreaks and epidemics that continue to occur, even in populations with advanced measles vaccine coverage.
The measles seroprevalence rate (92%) demonstrated in our study is slightly lower than that required to maintain herd immunity (95%), as has also been reported by others.Citation29 However, the seronegative rate (5.4%), is suggestive of very high immunity levels to measles in the sample population of Madinah, considering the model which proposed that the percentage of susceptible individuals should get over the threshold of 7.5% of the population for elimination.Citation30 When stratified by age, the age group of 20–29 y seem to be at risk, as it shows that the seronegative rate could be >7.5% (95% CI = 6.9–8.1), also given the higher prevalence of equivocal cases (4%). Our results may have implications for the health-care policymakers to reinforce the measles vaccination programs so as to mitigate the residual susceptibility among newborn as well as in individuals who have escaped both routine vaccination programs and natural infection in the past.
Our study is the first in Saudi Arabia to have investigated participants based on the history of measles vaccine implementation. Therefore, these data offer important insights to the authorities in the country, indicating that such seroepidemiological extended studies are necessary to fully understand vaccine effectiveness and the durability of the anti-measles antibody in other regions of the country. Additionally, this study will provide the Ministry of Health expert vaccine committee guidance regarding appropriate vaccine doses and recommendations for possible additional booster doses of the MMR vaccine to be administered to seronegative individuals so as to reduce the proportion of individuals at probable risk of infection in the future. Moreover, the evaluation of immune status against measles is critical among health-care workers, which should be considered as a recommendation.
The main limitation of this study was the convenient use of samples of adult healthy volunteers in Madinah with predominantly men (81.7%) compared to women. The women were not keen to participate in the survey unlike men. Thus, the demographics by sex or age are only for the participants who showed willingness to participate in the study. Hence, sex difference in the seroprevalence study does not represent the entire population of Madinah. In the absence of random sampling of Madinah population, extrapolation of the study findings to the population of Saudi Arabia requires careful consideration.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- Smetana J, Chlibek R, Hanovcova I, Sosovickova R, Smetanova L, Gal P, Dite P. Decreasing seroprevalence of measles antibodies after vaccination - possible gap in measles protection in adults in the Czech Republic. PLoS One. 2017;12(1):e0170257. Epub 2017/ 01/14. doi:10.1371/journal.pone.0170257.
- Moss WJ, Griffin DE. Measles. Lancet. 2012;379(9811):153–64. Epub 2011/ 08/23. doi:10.1016/S0140-6736(10)62352-5.
- Coleman KP, Markey PG. Measles transmission in immunized and partially immunized air travellers. Epidemiol Infect. 2010;138(7):1012–15. Epub 2009/ 11/03. doi:10.1017/S0950268809991129.
- The State of the World’s Children 1998: a UNICEF report. Malnutrition: causes, consequences, and solutions. Nutr Rev. 1998;56(4 Pt 1):115–23. Epub 1998/ 05/19. doi:10.1111/j.1753-4887.1998.tb01723.x.
- Tufenkeji H, Kattan H. Childhood immunization in the Kingdom of Saudi Arabia. Ann Saudi Med. 1994;14(2):91–93. Epub 1994/ 03/01. doi:10.5144/0256-4947.1994.91.
- Hegazy IS, Al-Beyari TH, Al-Amri AH, Noeman SA, Qureshi NA, Abdelgadir MH. A seroepidemiological study of measles: some practical implications for measles immunization program, Kingdom of Saudi Arabia. Ann Saudi Med. 1994;14(5):399–404. Epub 1994/ 09/01. doi:10.5144/0256-4947.1994.399.
- Stein CE, Birmingham M, Kurian M, Duclos P, Strebel P. The global burden of measles in the year 2000–a model that uses country-specific indicators. J Infect Dis. 2003;187(Suppl 1):S8–14. Epub 2003/ 05/02. doi:10.1086/368114.
- Patel MK, Dumolard L, Nedelec Y, Sodha SV, Steulet C, Gacic-Dobo M, Kretsinger K, McFarland J, Rota PA, Goodson JL, et al. Progress toward regional measles elimination - worldwide, 2000-2018. MMWR Morb Mortal Wkly Rep. 2019;68(48):1105–11. Epub 2019/ 12/06. doi:10.15585/mmwr.mm6848a1.
- van den Hof S, Conyn-van Spaendonck MA, van Steenbergen JE. Measles epidemic in the Netherlands, 1999-2000. J Infect Dis. 2002;186(10):1483–86. Epub 2002/ 10/31. doi:10.1086/344894.
- Al-Arabi Al-Ghamdi AM, Al-Faraj MH, Ibrahim HM, Al Mamun M. Epidemiological analysis of notified measles cases and review of surveillance system during an outbreak in Tabuk, Saudi Arabia. Ann Epidemiol. 2011;21(4):262–71. Epub 2011/ 03/08. doi:10.1016/j.annepidem.2010.12.004.
- Jahan S, Al Saigul AM, Abu Baker MA, Alataya AO, Hamed SA. Measles outbreak in Qassim, Saudi Arabia 2007: epidemiology and evaluation of outbreak response. J Public Health (Oxf). 2008;30(4):384–90. Epub 2008/ 08/22. doi:10.1093/pubmed/fdn070.
- Al-Abdullah N. A measles outbreak in a refugee community in Jeddah City, Saudi Arabia. J Hosp Infect. 2018;100(4):e264–e5. Epub 2018/ 06/03. doi:10.1016/j.jhin.2018.05.018.
- Khalil MK, Nadrah HM, Al Yahia OA, ElGhazali G. Seroresponse to the second measles vaccine dose at school entry in Qassim province, Saudi Arabia. East Mediterr Health J. 2011;17(3):191–95. Epub 2011/ 07/09. doi:10.26719/2011.17.3.191.
- Khalil MK, Al-Mazrou YY, Al-Jeffri M, Al-Ghamdy YS. Measles immunization in Saudi Arabia: the need for change. East Mediterr Health J. 2001;7(4–5):829–34. Epub 2004/ 08/31.
- Poi KM. Measles: the epidemiology and control of an outbreak. J Am Coll Health. 1983;31(4):158–61. Epub 1983/ 02/01. doi:10.1080/07448481.1983.9940433.
- Khalil MK, Al-Mazrou YY, AlHowasi MN, Al-Jeffri M. Measles in Saudi Arabia: from control to elimination. Ann Saudi Med. 2005;25(4):324–28. Epub 2005/ 10/11. doi:10.5144/0256-4947.2005.324.
- Greenwood B. The contribution of vaccination to global health: past, present and future. Philosophical Transactions of the Royal Society B: Biological Sciences. 2014;369(1645):20130433. doi:10.1098/rstb.2013.0433.
- Poethko-Müller C, Mankertz A. Seroprevalence of measles-, mumps- and rubella-specific IgG antibodies in German children and adolescents and predictors for seronegativity. PLoS One. 2012;7(8):e42867. Epub 2012/ 08/11. doi:10.1371/journal.pone.0042867.
- Kang HJ, Han YW, Kim SJ, Kim YJ, Kim AR, Kim JA, et al. An increasing, potentially measles-susceptible population over time after vaccination in Korea. Vaccine. 2017;35(33):4126–32
- Hanna-Wakim R, Yasukawa LL, Sung P, Arvin AM, Gans HA. Immune responses to mumps vaccine in adults who were vaccinated in childhood. J Infect Dis. 2008;197(12):1669–75. Epub 2008/ 04/19. doi:10.1086/588195.
- Briss PA, Fehrs LJ, Parker RA, Wright PF, Sannella EC, Hutcheson RH, Schaffner W. Sustained transmission of mumps in a highly vaccinated population: assessment of primary vaccine failure and waning vaccine-induced immunity. J Infect Dis. 1994;169(1):77–82. Epub 1994/ 01/01. doi:10.1093/infdis/169.1.77.
- Held L, Hens N, O’Neill P, & Wallinga J, editors. Handbook of Infectious Disease Data Analysis. 1st ed. CRC Press; 2019. doi:10.1201/9781315222912.
- Haralambieva IH, Ovsyannikova IG, O’Byrne M, Pankratz VS, Jacobson RM, Poland GA. A large observational study to concurrently assess persistence of measles specific B-cell and T-cell immunity in individuals following two doses of MMR vaccine. Vaccine. 2011;29(27):4485–91. Epub 2011/ 05/05. doi:10.1016/j.vaccine.2011.04.037.
- Al-Mazrou YY, al-Jeffri M, Ahmed OM, Aziz KM, Mishkas AH. Measles immunization: early two-doses policy experience. J Trop Pediatr. 1999;45(2):98–104. Epub 1999/ 05/26. doi:10.1093/tropej/45.2.98.
- Xiong Y, Wang D, Lin W, Tang H, Chen S, Ni J. Age-related changes in serological susceptibility patterns to measles: results from a seroepidemiological study in Dongguan, China. Hum Vaccine Immunother. 2014;10(4):1097–03. Epub 2014/ 01/23. doi:10.4161/hv.27734.
- Coppeta L, Pietroiusti A, Lieto P, Ferraro M, Grelli S, Stillo M, Magrini A. Measles immunity in an Italian teaching hospital. Occup Med (Chic Ill). 2018;69(2):143–45. doi:10.1093/occmed/kqy132.
- Chen CJ, Lee PI, Hsieh YC, Chen PY, Ho YH, Chang CJ, Liu D-P, Chang F-Y, Chiu C-H, Huang Y-C, et al. Waning population immunity to measles in Taiwan. Vaccine. 2012;30(47):6721–27. Epub 2012/ 05/29. doi:10.1016/j.vaccine.2012.05.019.
- de Melker H, Pebody RG, Edmunds WJ, Levy-Bruhl D, Valle M, Rota MC, SALMASO S, van den HOF S, BERBERS G, SALIOU P, et al. The seroepidemiology of measles in Western Europe. Epidemiol Infect. 2001;126(2):249–59. Epub 2001/ 05/15. doi:10.1017/S0950268801005234.
- Rearigh L, O’Neill J, Kubat M, Sayles H, Swindells S, Bares SH. Surprisingly low levels of measles immunity in persons with HIV: a seroprevalence survey in a United States HIV clinic. Open Forum Infect Dis. 2020;7(10):ofaa428. Epub 2020/ 10/20. doi:10.1093/ofid/ofaa428.
- Trentini F, Poletti P, Melegaro A, Merler S. The introduction of ‘No jab, No school’ policy and the refinement of measles immunisation strategies in high-income countries. BMC Med. 2019;17(1):86. Epub 2019/ 05/18. doi:10.1186/s12916-019-1318-5.