ABSTRACT
Background: Lincang City in Yunnan Province on the China-Myanmar border, has reached the World Health Organization recommended coverage (95%) for measles-containing vaccine (MCV), but measles outbreaks still occur. We conducted a survey in Lincang City to determine the measles vaccination status of children on the China–Myanmar border.
Methods: We used multistage sampling among children aged 8–83 months. Information on measles vaccination status was obtained from the child’s vaccination certificate, and serum samples were tested using commercially available ELISA kits.
Results: A total of 938 children were surveyed. The vaccination coverage rate was 98.9% (95% CI: 98.2–99.6%) for measles–containing vaccine dose 1 (MCV1), and 95.8% (95% CI:94.9–96.7%) for measles–containing vaccine dose 2 (MCV2). The timely vaccination coverage rate was 52.0% (95% CI:48.8–55.2%) for MCV1, and 74.1% (95% CI: 82.9–89.0%) for MCV2. The timely-and–complete vaccination coverage rate was 41.0% (95% CI: 36.7–45.3%). The median delay period was 33 (95% CI: 27–39) days for MCV1, and 196 (95% CI: 146–246) days for MCV2. The seropositivity rate in children aged less than 7 years was 94.0% (95% CI: 92.5–95.5%) with a geometric mean titer of 1210.1 mIU/mL.
Conclusions: The MCV coverage was high, but timely and timely-and-complete vaccination coverage were low and insufficient to prevent measles outbreaks. It is necessary to add the timely and timely-and-complete vaccination coverage as indicators of vaccination to provide a more complete picture of measles immunization status.
Introduction
Measles is a highly pathogenic infectious disease and is a major cause of death in children.Citation1 In 1960, before measles–containing vaccine (MCV) became available, more than 2.6 million people worldwide died of measles every year. Between 2000–2018, measles deaths fell by 73% worldwide as a result of increased measles vaccine coverage.Citation2 By the end of 2019, measles-containing vaccine first dose (MCV1) immunization coverage among 1-year-olds was 85%; 178 countries had included a second dose as part of routine immunization and 71% of children received measles-containing vaccine second dose (MCV2) according to national immunization schedules.Citation3 Yet measles is still common in many developing countries, particularly in Africa and parts of Asia.Citation4,Citation5 In recent years, repeated measles outbreaks have continuously occurred in some European countries.Citation6,Citation7 In 2019, there were more than 870,000 cases of measles globally, five times as many as in 2017. Among World Health Organization (WHO) member states, only 42 countries reported no measles cases, and the top ten ranking countries in terms of the number of measles cases reported were Democratic Republic of the Congo, Madagascar, Ukraine, Philippines, Nigeria, Brazil, Vietnam, Kazakhstan, India and Niger, among which Madagascar and Brazil have not experienced large-scale measles outbreaks in the past 15 years. However, the number of measles cases in these countries began to increase exponentially in 2018. Although the annual number of measles cases in other countries remained high, the number of measles cases also increased rapidly in 2018.Citation8 More than 95% of those measles cases occurred in people who had not been vaccinated or had received just one dose of MCV. Furthermore, there were some cross–border imported cases.Citation9–11 The overwhelming majority (more than 95%) of measles deaths occur in countries with low per-capita incomes and weak health infrastructures.Citation12
COVID-19 is affecting routine immunization worldwide. Its impact is likely to be greater in low- and middle-income countries with limited and fragile health systems. In Africa, the number of unvaccinated children who die from measles far exceeds the number who die from COVID-19.Citation13 During the Embargo, more than half of all children missed immunization, and the number of unimmunized children increased rapidly, leaving them vulnerable to vaccine-preventable diseases.Citation14,Citation15 However, even in countries/states with high immunization coverage, there are still frequent large measles outbreaks year,Citation11,Citation16,Citation17 suggesting that high immunization coverage within countries/states can mask areas with low immunization coverage. Most of the areas with low immunization coverage are at national borders, where population mobility facilitates measles spread.Citation18,Citation19 Moreover, factors such as complicated immunization procedures, dated medical facilities, certain health conditions, and low educational level of parents in border areas, may affect the timely vaccination, resulting in a decrease in anti–measles antibody (IgG) levels among the population and a high risk of measles outbreaks.Citation20–22
Lincang City in Yunnan Province, is the most important transportation center in southwest Yunnan.Citation23 From 2010 to 2018, MCV immunization coverage (two doses) in Lincang City ranged from 98.74–99.70%, and immunization coverage in each county ranged from 95.96–100.00% (Lincang City Measles Vaccination Questionnaire, 2016–2020). Although the immunization level of Lincang City has reached the WHO recommended level (95%), there are still measles cases. Imported cases are an important source of infection in countries where measles has been eliminated. The vaccination coverage rate and seropositivity rate of children in Myanmar are lower than those in Lincang City, that is, children in Myanmar are more susceptible to measles. The large population flow along the China-Myanmar border is more likely to result in imported cases.Citation24,Citation25 In addition, children in Lincang City may have delayed or incomplete vaccination,Citation19 which may lead to subtherapeutic IgG levels insufficient to provide resistance to the measles virus.
Therefore, a sample survey was conducted in Lincang City, to assess the MCV vaccination status in children, determine the effect of immunization status on seropositivity and the influence of vaccination status on IgG level, and provide a scientific basis for the vaccination program in Yunnan Province.Citation26
Methods
Study setting and population
We conducted a cross–sectional survey using multistage sampling among children aged 8–83 months in Lincang City. Lincang City has an area of 24,000 km2 with eight counties, 2.536 million population, and 23 ethnic groups, sharing a 290.79 km-long border with Myanmar in the southwest. MCV refers to vaccines containing measles vaccine components, including leprosy vaccine, measles-mumps-rubella vaccine and measles-mumps vaccine. Routine vaccination consists of MCV1 and MCV2, administered at the age of 8 months old 18–24 months, respectively. In order to more comprehensively and scientifically evaluate the vaccination status and measles serum antibody level of children in Lincang City, a sample survey was conducted among children aged 8–83 months.
The inclusion criteria were: (1) age 8–83 months; (2) vaccination certificate available; (3) no contraindications for immunization; (4) blood samples can be provided; and (5) have resided in the local area for at least 6 months.
Informed consent was obtained from the children’s guardians.
Sampling and sample size
Lincang City has a total of eight counties. Three towns were randomly selected from each county; three villages were randomly selected from each town; and 13 households were randomly selected from each village. If the family had more than one child, the youngest child was chosen. If the household did not have any children meeting the inclusion criteria, a neighboring household was selected.
Data collection
The survey began on October 1, 2019, and lasted for two months. Vaccination information and basic information, including date of birth, sex, and ethnicity were obtained from the vaccination certificate. Serum samples were collected by medical professionals and sent to the Center for Disease Control and Prevention (CDC) in Lincang City for antibody titer level testing. EpiData 3.1 was used to establish the database and double entry of data was carried out by two researchers.
Technical indicators
The measles vaccination status of each child was determined according to the schedule of national immunization procedures. The vaccination status of children was divided into early vaccination, timely vaccination, delayed vaccination, unvaccinated, complete vaccination and timely-complete vaccination. Children who were vaccinated with MCV1 at aged 8 months (244–273 days), and vaccinated with MCV2 at aged 18–24 months (548–730 days), were defined as having received timely vaccination. Receipt of vaccination before and after the window for timely vaccination, were classified as early and delayed vaccination, respectively. Children who had received two doses of MCV in a timely manner, were classified as having received timely-complete vaccination. Children who had received two doses of MCV, with one or both given outside the recommended time-frame, were classified as having complete vaccination. Unvaccinated was defined as having not been vaccinated with MCV before the survey.
The serum samples of children were tested by Lincang CDC, according to the Diagnostic Criteria for Measles (WS296–2008).Citation27 The antibody titer was divided into three categories: negative, positive and equivocal. Titers of >200 mIU/mL, 150–200 mIU/mL, and <150 mIU/mL were defined as positive, equivocal, and negative, respectively.
Statistical analysis
EpiData 3.1 (EpiData Association, Odense, Denmark) and R 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria) were used for data collection and collation, respectively. The vaccination coverage and 95% confidence interval (CI) of MCV1 and MCV2 were calculated. Kaplan-Meier analysis was used to calculate the median delay and 95% CI of MCV1 and MCV2. The calculation of vaccination coverage of MCV2 and timely-complete vaccination coverage did not include children under 24 months of age. Children under 8 months of age were not included in the calculation of the complete vaccination coverage rate. The seropositivity rate and 95% CI were calculated for each group. The chi–square test was used to compare the seropositivity rate between groups. P values <.05 were regarded as statistically significant.
Ethical considerations
The Ethics Committee of the Dali University Faculty of Public Health approved the study in advance (Reference number: 20181206–6).
Results
Demographic characteristics
A total of 938 children participated in the survey, and all children provided blood samples. Their characteristics are shown in . The number of participants in each county ranged from 117–118, with children aged 8–24 months accounting for 43.6–53.4%. The ratio of boys to girls was 50.3:49.7. Of the children, the Han, Yi, and other ethnicities were 52.1%, 18.1%, and 29.7%, respectively.
Table 1. Demographic characteristics of children
Vaccination status
shows the vaccination coverage rate. The coverage rate of MCV1 was 11.7% for early vaccination, 52.0% for timely vaccination, and 35.2% for delayed vaccination; 1.1% were unvaccinated. For MCV2, the coverage rate of early, timely, and delayed, vaccination was 8.2%, 74.1%, 13.5%, respectively, and 4.2% were unvaccinated. The complete vaccination coverage and timely-complete vaccination coverage were 57.9% and 41.0%, respectively, while 42.4% of children had received only one dose of MCV or were unvaccinated.
Table 2. Number and coverage of vaccination for MCV1 and MCV2 by county
Median delay in vaccination
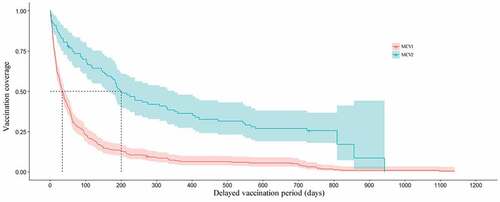
The median delay in MCV1 and MCV2 was 33 and 196 days, respectively (). shows the Kaplan–Meier curves of delayed MCV vaccination.
Table 3. Median delay vaccination period for MCV1 and MCV2
Figure 1. Kaplan-Meier curves of delayed vaccination for measles-containing vaccination 1 (MCV1, red) and measles-containing vaccination 2 (MCV2, blue) among children in Lincang City, Yunnan Province, China. The shaded areas represent the 95% confidence intervals. The dashed lines indicate that the median delay in vaccination is 33 days for MCV1, and 196 days for MCV2
Seroepidemiological profiles
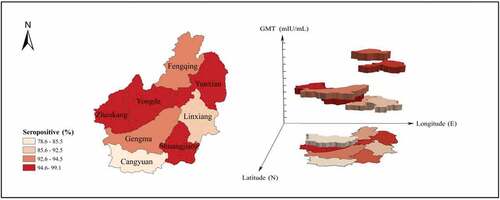
shows the seroepidemiological profiles. The seropositivity rate for each age group was 92.1–96.0% with geometric mean titers (GMT) of 1124.1–1231.6 mIU/mL. Boys had a seropositivity rate of 92.6% with a GMT of 1228.3 mIU/mL, and girls had a seropositivity rate of 97.6% with a GMT of 1229.3 mIU/mL. Cangyuan County had a seropositivity rate of 78.6% with a GMT of 478.7 mIU/mL, and other counties had seropositivity rates between 92.3% and 99.1% with a GMT ranging between 843.8 and 2298.2 mIU/mL. The seropositivity rate among complete, timely-complete and one-dose and unvaccinated children ranged between 80.0% and 95.1% with a GMT ranging between 1225.3 and1230.9 mIU/mL. There were no statistically significant differences in the seropositivity rate according to vaccination status and age, while there were statistically significant differences according to the sex, ethnicity, and county. In , the seropositivity rate and the GMT of each county is shown in two and three dimensions, respectively.
Table 4. Seroepidemiological profiles by sex, ethnicity, age, county and vaccination status
Discussion
This study found that the vaccination coverage rates of MCV1 (98.9%) and MCV2 (95.8%) among children in Lincang City were high, which is consistent with the annual statistical results of the Lincang CDC; however, the timely vaccination coverage rates of MCV1 (52.0%) and MCV2 (74.1%) were low, and the complete vaccination coverage rate (57.9%) and the timely-complete vaccination coverage rate (41.0%) of MCV were even lower, and the median delay in the administration of MCV1 (33 days) and MCV2 (196 days)is a cause for concern. A substantial proportion of children were not vaccinated within the recommended time-frame.
Indicators of timely vaccination coverage and timely-complete vaccination coverage are rarely used to assess vaccination status, in China or elsewhere but, rather, the simple overall coverage is generally reported, regardless of whether the children were vaccinated within the nationally recommended time-frame. This greatly overestimates the vaccination coverage rate and obscures the timeliness, effectiveness, and authenticity of childhood vaccination.
Other countries have similar problems with ensuring timely vaccination with MCV. A study conducted in India found a timely vaccination coverage rate for MCV1 of 49.98%, with a median delay period of 368 days.Citation28 A study conducted in Switzerland found a timely vaccination coverage rate for MCV1 of 46.20%, with a median delay of 78 days, and a timely-complete vaccination coverage rate of only 10.00%.Citation29 A study conducted in Ethiopia found early, timely, and delayed vaccination coverage rates of 51.3%, 26.4%, and 22.3%, respectively;Citation30 and a study conducted in Lebanon found timely vaccination coverage rates for MCV1 and MCV2 of 44.3% and 63.5%, respectively.Citation31
Differences in timely vaccination coverage and the median delay period for MCV across countries are to be expected because of differences in the timing of measles vaccination in different countries. If these indicators are calculated on the basis of national vaccination programs, all countries have low timely vaccination rates and children are subject to delayed vaccination.
Thar et al.Citation32 analyzed the measles vaccination status in Myanmar and found that the vaccination coverage rate of MCV2 was lower than that of MCV1, contrary to the results of our study, which found a higher vaccination coverage rate of MCV2 than that of MCV1. When a child receives MCV1, the health workers should make an appointment with the child’s guardian for the child to receive MCV2. In addition, medical institutions should advise the guardian to register relevant information when MCV1 is given, so that the system can send a message reminding the guardian to bring the child for MCV2. In China, the MCV1 vaccination window is 1 month, and the MCV2 vaccination window is 6 months, so children are more likely to be vaccinated with MCV2 within the specified time window. If a relationship of trust can be established between health workers and guardians, this may increase the timely vaccination rate of children born in hospitals, even in countries with low vaccination coverage.Citation33
Rybak et al.Citation34 studied delayed vaccination of French children and found that delayed MCV1 vaccination increased the risk of delayed vaccination with MCV2, contrary to the findings of this study. This study found that if the MCV1 is delayed, the delay in receiving MCV2 was reduced significantly. Delayed in the administration of MCV2 may be reduced by health workers providing vaccine education to the guardian when the child receives MCV1, to provide the guardian with an awareness of the importance of vaccination, thereby reducing the risk of delayed MCV2 vaccination. The government plays an active role in immunization. In 2008, China began to implement the Expanded Program on Immunization,Citation35 and the implementation plan provides detailed explanations on the specific issues of children’s immunization. Vaccine literacy of the population has been popularized. In addition, a series of education programs formulated by the government played a contributory role in training and promoting of a sense of responsibility and professional quality among immunization workers, ensuring smooth implementation of the program.
Since 1978, when China added measles vaccination to the immunization schedule, and 1986, when it added a second doses, the incidence of measles has greatly decreased. In 2019, there were 2,974 cases of measles reported, in incidence rate of 0.213%.Citation36 There is still a risk of measles transmission. Domestic studies have shown that anti-measles IgG antibody seropositivity in children aged over 24 months increases with age and with additional vaccine doses.Citation37 The results of the serological study showed no statistically significant differences by age. There was also no statistically significant difference in the seropositivity among these children whether or not they had been vaccinated and whether or not they had been vaccinated with MCV on time or completely. These findings were contrary to our expectations and are difficult to explain. In general, children vaccinated with MCV have significantly higher antibody levels. Vaccinated children who are exposed to measles and becomes infected, tend to develop atypical symptoms, and so their infection may remain undiagnosed. The measles antibody level of children with mild infection increases during convalescence, which is why some children who had not been vaccinated had high measles antibody titers. Higher vaccination coverage may be associated with a higher hidden infection rate in the corresponding population. There are few reports on the proportion of children who acquire natural immunity due to undiagnosed infection, and this requires further study. In this study, there were 388 children who had been immunized only once, of whom 344 (88.7%) were <18 months old. Another study conducted using the Chinese measles detection information management system, found that the GMT levels, seropositivity and that the measles incidence rate was the highest, with infants under 12 months, accounting for 23.81% of all cases.Citation38 Therefore, the age-specific incidence rate of measles may affect the seropositivity rate, especially in the younger children and in one-dose vaccine recipients.
There were significant differences in seropositivity by county. Cangyuan County had the lowest seropositivity rate, which was significantly lower than the seropositivity rate in the other counties, but there was no significant difference between other seven counties. The immunization coverage in Cangyuan County was high and did not differ significantly from the other counties, because after a measles outbreak in Lincang, a supplementary immunization programs and catch-up immunization activities were implemented, which targeted the susceptible population in the whole city. this resulted in an increased immunization coverage of children. However, it is worth noting that the early vaccination rate in Cangyuan County with its low seropositivity rate, was much higher than that in other counties. However, many children were vaccinated with MCV1 early, before the recommended age of 8 months. In children vaccinated with MCV1 early, the interval between MCV1 and MCV2 is prolonged. During this time, it is difficult to maintain the antibody level at a level sufficient to prevent measles. In addition, we also found that most of the children in Cangyuan County were being raised by their grandparents. The parents of these children go out to work,leaving the children with their grandparents and these children become left-behind children (LBC). Because grandparents’ awareness of immunization tend to be low, these LBC may not be vaccinated within the recommended time-frame. Therefore, when publicizing the immunization policy, publicity should be directed toward the guardians of LBC. Children’s guardians should take their children to the hospital for vaccination in strict accordance with the immunization schedule. Health workers have a responsibility to explain the immunization schedule to children’s dependents and to vaccinate children in strict accordance with the schedule.
In summary, children’s immunization requires more attention, especially with respect to ensuring timely vaccination, complete vaccination, and timely-complete vaccination. In addition, the monitoring of immunization of LBC should be strengthened.
Highlights of the study: A survey of a random sample of children was conducted in the villages of eight counties in Lincang City, so the survey is representative of the vaccination status of children in Lincang City. In addition, the study results included indicators such as timely vaccination, complete vaccination and timely-complete vaccination. These results provide a scientific explanation of why measles outbreaks continue to occur in areas with high measles vaccine coverage.
Limitations: Children whose caretaker could not provide a vaccination certificate were excluded from the study. These children are more likely to be unvaccinated or not vaccinated in time, thus leading to overestimation of the vaccination coverage rates and timely vaccination rates. Immunization, as a basic medical health service, is affected by multiple factors. This study does not provide a comprehensive scientific explanation for the failure of childhood immunization.
Author contributions
SYY and TTT conceptualized the study, outlined the design and supervised data analysis, as well as worked out details and led field study. XTY and TZ analysis of the data, manuscript preparation and manuscript writing. ZKY and LL directly coordinated the research and fieldwork. All authors have read and approved the final manuscript.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Disclosure of potential conflicts of interest
The authors declare that they have no competing interests.
Acknowledgments
We would like to thank all the participants who took part in this study. We are grateful to the leaders of Lincang City and the village committees in the survey villages for their assistance with the fieldwork. We also thank Editage for English language editing.
Additional information
Funding
References
- World Health Organization. Strategic plan 2012–2020; [accessed 2020 Oct 21]. https://www.who.int/immunization/diseases/measles/zh.
- World Health Organization. Immunization, vaccines and biologicals; 2020 Jul 15 [accessed 2020 Oct 21]. https://www.who.int/immunization/diseases/measles/en/dan.
- World Health Organization. Immunization coverage; [accessed 2020 Oct 21]. https://www.who.int/en/news-room/fact-sheets/detail/immunization-coverage.
- Gao Y, Kc A, Chen C, Huang Y, Wang Y, Zou S, Zhou H. Inequality in measles vaccination coverage in the “big six” countries of the WHO South-East Asia region. Hum Vaccin Immunother 2020;16(7):1485–97. PMID: 32271649. doi:10.1080/21645515.2020.1736450.
- Debie A, Lakew AM. Factors associated with the access and continuum of vaccination services among children aged 12–23 months in the emerging regions of Ethiopia: evidence from the 2016 Ethiopian demography and health survey. Ital J Pediatr 2020;46(1):28. PMID: 32131868. doi:10.1186/s13052-020-0793-9.
- Fabiani M, Fano V, Spadea T, Piovesan C, Bianconi E, Rusciani R, Salamina G, Greco G, Ramigni M, Declich S, et al. Comparison of early childhood vaccination coverage and timeliness between children born to Italian women and those born to foreign women residing in Italy: a multi-centre retrospective cohort study. Vaccine. 2019;37(16):2179–87. PMID: 30902479. doi:10.1016/j.vaccine.2019.03.023.
- Plans-Rubió P. Low percentages of measles vaccination coverage with two doses of vaccine and low herd immunity levels explain measles incidence and persistence of measles in the European Union in 2017–2018. Eur J Clin Microbiol Infect Dis. 2019;38(9):1719–29. PMID: 31289949. doi:10.1007/s10096-019-03604-0.
- World Health Organization. Measles and rubella surveillance data; [accessed 2020 Oct 21]. https://www.who.int/immunization/monitoring_surveillance/data/incidence_series.xls.
- Sodjinou VD, Douba A, Nimpa MM, Masembe YV, Randria M, Ndiaye CF. Madagascar 2018–2019 measles outbreak response: main strategic areas. Pan Afr Med J. 2020;37(20). PMID: 33062122. doi:10.11604/pamj.2020.37.20.24530.
- Zhou RR, Li LQ, Yuan SY, Yu W, Li QF, Gong QY, Li JR, Zhao ZX. Effectiveness of measles-containing vaccine during a measles outbreak in the China-Myanmar border area. Int J Epidemiol Infect Dis. 2020;47(2):111–15. doi:10.3760/cam.j.cn.331340-20191011-00174.
- Delaporte E, Jeannot E, Sudre P, Wyler Lazarevic C, Richard J, Chastonay P. Measles in Geneva between 2003 and 2010: persistence of measles outbreaks despite high immunisation coverage. Euro Surveill. 2011;16(39):19980. PMID: 21968424. doi:10.2807/ese.16.39.19980-en.
- World Health Organization. Immunization, vaccines and biologicals; 2020 Jan [accessed 2020 Oct 21]. https://www.who.int/immunization/diseases/measles/en/.
- Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, Soundardjee R, Dharma VK, Shah MT, Abdullah S, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 2020;38(45):7146–55. PMID: 32943265. doi:10.1016/j.vaccine.2020.08.019.
- Jamal D, Zaidi S, Husain S, Orr DW, Riaz A, Farrukhi AA, Najmi R. Low vaccination in rural Sindh, Pakistan: a case of refusal, ignorance or access? Vaccine. 2020;38(30):4747–54. PMID: 32467011. doi:10.1016/j.vaccine.2020.05.018.
- Omoleke SA, Getachew B, Igoh CS, Yusuf TA, Lukman SA, Loveday N. The potential contribution of supplementary immunization activities to routine immunization in Kebbi State, Nigeria. J Prim Care Community Health. 2020;11:2150132720932698. PMID: 32508212. doi:10.1177/2150132720932698.
- Agopian A, Young H, Quinlan S, Rice MM. Timeliness of childhood vaccinations in Armenia, 2015–2016. Vaccine. 2020;38(30):4671–78. PMID: 32448619. doi:10.1016/j.vaccine.2020.05.032.
- Zhou R, Li L, Yuan S, Yin J, Li Q, Guo L, Li M, Zhao Z, Song Z. Health and economic costs of an import-initiated measles outbreak in an international border area of Yunnan Province. Hum Vaccin Immunother. 2020:1–6. PMID: 32991225. doi:10.1080/21645515.2020.1815488.
- Zhang WY, Xiong P, Liu SN, Zeng Z, Xu Q, Luan GJ, Xu AQ, Zhang YJ. Age-specific coverage of childhood routine immunization based on the immunization information system in Shandong province. Chin J Vaccine Immun. 2019;25:193–97.
- Hu Y, Chen Y, Wang Y, Liang H, Lv H. Age-appropriate vaccination coverage and its determinants for the polio containing vaccine 1–3 and measles-containing vaccine doses in Zhejiang province, China: a community-based cross-sectional study. Hum Vaccin Immunother. 2020;16(9):2257–64. PMID: 32048897. doi:10.1080/21645515.2020.1718439.
- Degarege A, Krupp K, Srinivas V, Ibrahimou B, Madhivanan P. Structural equation modeling to detect correlates of childhood vaccination: a moderated mediation analysis. Plos One. 2020;15(10):e240749. PMID: 33057426. doi:10.1371/journal.pone.0240749.
- He Z, You FF, Zhou Z. Risk factors for measles in adults: a meta-analysis of case-control study. Mod Prev Med. 2019;46:1171–75.
- People’s Government of Yunnan Province. Yunnan yearbook 2019; [accessed 2020 Oct 21]. http://stats.yn.gov.cn/tjsj/tjnj/201912/P020191202608100339128.zip.
- Zhou R, Yuan S, Yu W, Li L, Li Q, Guo L, Zhao Z, Song Z. Measles immunity in the China-Myanmar border region, Lincang city, Yunnan province, 2017. Hum Vaccin Immunother. 2020;16(4):881–85. PMID: 31662039. doi:10.1080/21645515.2019.1673641.
- Tang XY, Geater A, McNeil E, Zhou HX, Deng QY, Dong AH. Timeliness and completeness of measles vaccination among children in rural areas of Guangxi, China: a stratified three-stage cluster survey. J. Epidemiol. 2017;27(7):317–24. PMID: 28187960. doi:10.1016/j.je.2016.08.006.
- Tang XY, Geater A, McNeil E, Zhou HX, Deng QY, Dong AH, Li Q. Parental migration and children’s timely measles vaccination in rural China: a cross-sectional study. Trop Med Int Health. 2016;21(7):886–94. PMID: 27137758. doi:10.1111/tmi.12719.
- World Health Organization. Immunization agenda; [accessed 2020 Oct]. https://www.who.int/zh/news-room/fact-sheets/detail/immunization-coverage.
- Standardization administration. Diagnostic criteria for measles; 2008 Dec 11 [accessed 2020 Oct 31]. http://hbba.sacinfo.org.cn/stdDetail/b591a9707ed1da765dfd6ffe4a79092f.
- Wagner AL, Shenton LM, Gillespie BW, Mathew JL, Boulton ML. Assessing the timeliness of vaccine administration in children under five years in India, 2013. Vaccine. 2019;37(4):558–64. PMID: 30595345. doi:10.1016/j.vaccine.2018.12.035.
- Schneider R, Reinau D, Schur N, Blozik E, Früh M, Signorell A, Heininger U, Schwenkglenks M, Meier CR. Coverage rates and timeliness of nationally recommended vaccinations in Swiss preschool children: a descriptive analysis using claims data. Vaccine. 2020;38(6):1551–58. PMID: 31791812. doi:10.1016/j.vaccine.2019.11.057.
- Marefiaw TA, Yenesew MA, Mihirete KM. Age-appropriate vaccination coverage and its associated factors for pentavalent 1–3 and measles vaccine doses, in northeast Ethiopia: a community-based cross-sectional study. PLOS One. 2019;14(8):e218470. PMID: 31419230. doi:10.1371/journal.pone.0218470.
- Rauniyar SK, Munkhbat E, Ueda P, Yoneoka D, Shibuya K, Nomura S. Timeliness of routine vaccination among children and determinants associated with age-appropriate vaccination in Mongolia. Heliyon. 2020;6(9):e4898. PMID: 30734029. doi:10.12688/gatesopenres.12898.1.
- Thar AMC, Wai KT, Harries AD, Show KL, Mon LL, Lin HH. Reported measles cases, measles-related deaths and measles vaccination coverage in Myanmar from 2014 to 2018. Trop Med Health. 2020;48:4. PMID: 32047360. doi:10.1186/s41182-020-0191-4.
- Nakatudde I, Rujumba J, Namiiro F, Sam A, Mugalu J, Musoke P. Vaccination timeliness and associated factors among preterm infants at a tertiary hospital in Uganda. PLOS One. 2019;14(9):e221902. PMID: 31490987. doi:10.1371/journal.pone.0221902.
- Rybak A, Vié Le Sage F, Béchet S, Werner A, Thiebault G, Bakhache P, Virey B, Caulin E, Cohen R, Levy C. Timeliness of routine immunization in non-preterm children less than 2 years old using electronic data capture in an ambulatory setting in France in the context of vaccine hesitancy. Arch Pediatr 2019;26(2):56–64. PMID: 30638762. doi:10.1016/j.arcped.2018.11.011.
- The Central People’s Government of the People’s Republic of China. Expand the implementation plan of national immunization program; [accessed 2021 Feb 14]. http://www.gov.cn/gzdt/2008-02/19/content_893572.htm.
- National Bureau of Statistics. China statistical yearbook 2020; [accessed 2021 Feb 14]. http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm.
- Qiu JJ, Chen PQ, Wang JM. A sero-epidemiological study on measles, rubella and mumps among the community–based populations aged 0 to 40 years in Yangzhong City, Jiangsu of China. Chin J Dis Control Prev. 2017;21(11):1178–80. doi:10.16462/j.cnki.zhjbkz.2017.11.024.
- Liu YJ, Zhao HM, Xu R, Guan F. Analysis on level of measles antibody among healthy population in Dali Prefecture in 2018. Infect Dis Inf. 2020;33:444–47.