ABSTRACT
During the COVID-19 pandemic, antivaccination social media accounts are proliferating online, threatening to further escalate vaccine hesitancy related to the COVID-19 vaccine. This commentary seeks to alert and encourage the health care provider community, including health care professionals and academic organizations, to engage in social media to counter the mounting vaccine-related infodemic. To validate our recommendation for engagement, the authors describe preliminary findings using a mixed methods approach of quantitative Twitter-based ranking algorithms of networks and users with qualitative content analysis of 1 million tweets related to COVID-19 vaccine conversations. Results show highly polarized and active antivaccine conversations that were primarily influenced by political and nonmedical Twitter users. In contrast, less than 10% of the tweets stemmed from the medical community, demonstrating a lack of active health care professional connectivity in addressing COVID-19 misinformation. The authors introduce the concept of Health Care Provider Social Media Hesitancy to refer to the public health threat of health care providers’ nonaction in providing pro-vaccine and scientific information about the vaccine on social media. The authors conclude by describing multilevel strategies for encouraging health care providers and the medical community to effectively “Tweet up” to combat the mounting threat of vaccine misinformation and hesitancy.
Recent studies report that over 85,000 new anti-SARS CoV-2 vaccine (hereto referred to as COVID-19 vaccine) Facebook accounts have been developed in the past year alone and are continuously proliferating across various platforms (e.g., YouTube, Twitter) resulting in the total number of anti-COVID-19 vaccine followers nearing 60 million. Alarmingly, efforts including newly launched social media policies are expected to make little impact on the exponential growth of vaccine-related misinformation.Citation1,Citation2 President Biden’s most recent executive order to deliver 100 million vaccines within the next 100 days of his administration strengthens several important vaccine delivery strategies, including implementing a national vaccine public education plan,Citation3 yet it does not explicitly target the ubiquitous anti-COVID-19 vaccine sentiments observed across all social media platforms. Similarly, although medical and public health professions have heightened awareness of the public-health messaging challenges ahead,Citation4,Citation5 a failure to centrally target what has been contextualized as the COVID-19 social-media infodemic may continue to plague the mass-vaccination plans now in place in the US.
As a collective, health care professionals, health care organizations, and academic organizations (collectively referred to as HCPs herein) are historically and uniformly the most important drivers of vaccine uptake.Citation6 Moreover, HCP-led messaging using social media platforms has had positive impact on recent public health crisesCitation7 and vaccine campaigns.Citation8 Thus, as fervently as HCPs have fought on the clinical frontlines of the COVID-19 pandemic, we, as HCPs, must consider redoubling our efforts toward countering the digital frontlines of the infodemic. Yet, past trends related to HCP engagement in social media-based public health messaging reflect that fewer than 60% of HCPs use social media for professional purposes,Citation9 and that most are passive users – colloquially defined as those who “scroll past” controversial topics, merely “liking” content without commenting, or simply “retweeting” content they may support.
Our intercollaborative HCP team’s preliminary analysis of over 1 million tweets in July 2020 of COVID-19 vaccine influencers and sentiments () evidenced these alarming gaps in HCP-led public health messaging related to the COVID-19 vaccine. By using Twitter API (Application Programming Interface) using predefined keyword queries to extract relevant tweets, we found that only 10% of the most influential profiles engaging in the COVID-19 vaccine conversation were HCPs. In contrast, influential profiles opposing the vaccine tended to be non-HCPs who are extremely vocal and highly visible due to their active engagement with this conversation. Moreover, the limited number of HCPs who are actively engaging with the vaccine conversation did not represent frontline fields with vaccine expertises like infectious disease, immunology, pediatrics, family medicine, internal medicine, or nursing professionals.
Figure 1. Network Graph of COVID-19 vaccine conversation on Twitter. Each node is a Twitter account. An edge is a retweet relations between two nodes. Labels are all the “verified” health care provider (HCP) Twitter accounts (n = 9) among the 107 most influential accounts. The size of node reflects the level of influentialness using PageRank algorithm (the bigger the node, it is more influential). Data and methods: COVID-19 and vaccine relevant Twitter data is collected between July 1st-31st of 2020 using Twitter API (Application Programming Interface). From the initial 751,691 nodes, we filtered in giant components with degree range over 7, which gave us a total of 1,992 nodes for the network analyses. Louvain algorithm is used to create the clusters, and manual coding of sample tweets from each of the major clusters was conducted to understand attitudes toward vaccine (far-left dust colored cluster: supporters of SARS CoV-2 vaccines including political leaders, media channels with HCPs accounts labeled; middle purple cluster: political leaders and other individual accounts with mixed with positive and opposing attitudes on vaccine; far-right green cluster: SARS CoV-2 opposition accounts)
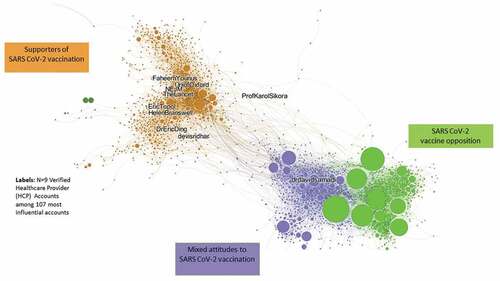
Our data analysis additionally revealed that antivaccine communities are highly active on Twitter (demonstrated by large nodes in and reflecting the generation of hourly content at times), and more densely connected than pro-vaccine groups, suggesting a high reliance on these inner networks for generating and disseminating vaccine hesitant sentiments. This interactivity pattern was in direct contrast to the level of engagement of COVID-19 vaccine supportive groups, including HCPs and major news media, which showed significantly lower levels of engagement (evidenced by smaller nodes of network activity in ) and interconnectivity (evidenced by distance between clusters), around supportive COVID-19 vaccine conversations.
This type of HCP social-media hesitancy can no longer be accepted in light of the greater awareness of antivaccine social media patterns that demonstrate relentless and “24–7 day per week misinformation dosing regimens.” Long-standing hesitancy by HCPs has allowed antivaccine activists and political activists the greatest chance to effectively “dose” the public with misinformation at a critical time point in the pandemic where vaccine access is improving and vaccine uptake is critically needed. Overcoming the alarming paucity of accurate and valid COVID-19 vaccine public health messaging will require that HCPs deliver the much-needed missed doses of vaccine truths by engaging in COVID-19 vaccine campaigns that harness both traditional messaging and online social media strategies, with a particular focus on involving social media influencers that can target misinformation.Citation4 As Shafer et al. proposed, “frontline health care workers should be taught how to make strong recommendations for SARS CoV-2 vaccination, including … sharing their personal experiences with COVID-19 and the vaccine.” Yet, a call to action to deliver these recommendations and share our stories across platforms and embrace our role as social media influencers remains a notable gap in our collective efforts.
Although many have previously made cases for the importance of HCPs to broadly “Tweetup” professionally,Citation9 our data clearly demonstrate that HCPs remain significantly hesitant to: 1) be active on social media; 2) be interconnected with other users and networks; and 3) generate new COVID-19 vaccine focused content. Prior work suggests that concern for damage to professional image, potential breaches of patient privacy, violation of personal–professional boundaries,Citation10 perpetuating personal biases, and data-security issuesCitation5 are notable barriers reported by HCPs. Fortunately, many health care institutions and professional organizations have issued pragmatic policies and guidelines (i.e., creating separate personal and professional accounts, social media training, optimizing privacy settings) to mitigate individual and organizational social-media-based risks.Citation11 Our early data, as well as other recent social-media patterns, validate that sustained HCP social media hesitancy in the wake of a growing infodemic should be considered a public health threat where the benefits of HCP engagement now outweigh the potential risks. Whereas in the past, public health messaging may have relied on traditional channels, such as high impact journals, visually appealing television and media campaigns, or broad phone-based algorithms to deliver public health messages, HCP voices must embrace the era of social media public health messaging and confront the COVID-19 vaccine infodemic where it exists.
As a first step in turning the tide of HCP social media hesitancy, we propose a formal reframing of social media as an academically and medically valuable resource, with HCP authors and social media content considered eligible as “high impact” in parallel to traditional scholarly content. Furthermore, it will be vital for health care and academic organizations to implement multitiered strategies to begin addressing the infodemic that may include but are not limited to: 1) developing and implementing internal methods to detect prevalent health misinformation (health care’s version of Politifact); 2) requiring and expanding conversations with social media executives to identify safeguards against health-care-related misinformation; 3) delegating socio-culturally diverse frontline staff and HCPs with roles specific to pro-vaccination to counter COVID-19 misinformation by sharing their stories and perspectives; 4) incentivizing and supporting HCPs within organizations to be active on social media; and 5) providing coaching by nonmedical influencers to HCPs focused on social media strategies that generate impact.
In addition to the reframing of social media as a valuable vaccine truth delivery tool for HCPs, we propose other individual strategies for empowering HCPs to overcome social-media hesitancy. These include but are not limited to: 1) if not already a user, create a professional user account with the goal of communicating and advocating about health-related issues; 2) follow all peer-reviewed medical journals and organizations that align with your specialty and cause; 3) follow other colleagues, users who you work with or may know on social media platforms; 4) follow highly influential HCP accounts (i.e., @DrTomFrieden, @EricTopol on Twitter); 5) connect journal articles and other evidence-based information with your commentary (content with a reference); 6) engage and inquire about your organization’s social media channels and presence; 7) be actively involved in social media conversations specific to COVID-19 and COVID-19 vaccine with the goal of correcting misinformation; 8) respond as able to individuals who like, retweet, or comment on your posts; and 9) consider use of free, online media schedulers to generate regular and strategically timed tweets (e.g., Hootsuite, Tweetdeck) or other content.
Strategies focused on meaningfully and safely engaging HCPs on social media, promoting interconnectivity across the medical and public health communities on COVID-19 vaccine truths, and sustaining these messaging efforts across vaccine implementation stages will be our best hope of preventing any more missed doses and promoting “misinformation immunity” for all.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- Rutschman SA. Facebook’s latest attempt to address vaccine misinformation—and why it’s not enough. Health Affairs Blog; St. Louis U. Legal Studies; 2020. Research paper no. 2020-35.
- Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digit Health. 2020;2(10):e504–e505. doi:10.1016/S2589-7500(20)30227-2. PMID: 32984795.
- Biden JR. National strategy for the COVID-19 response and pandemic preparedness. In: Office E, editor. The White House; 2021, p. 36–38. [accessed 2021 Apr 9]. https://www.whitehouse.gov/wp-content/uploads/2021/01/National-Strategy-for-the-COVID-19-Response-and-Pandemic-Preparedness.pdf .
- Schaffer Deroo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. 2020;323(24):2458–59. doi:10.1001/jama.2020.8711. PMID: 32421155.
- Merchant RM, South EC, Lurie N. Public health messaging in an era of social media. JAMA. 2021;325(3):223. doi:10.1001/jama.2020.24514. PMID: 33393964.
- Sturm L, Donahue K, Kasting M, Kulkarni A, Brewer NT, Zimet GD. Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health. 2017;61(2):246–51. doi:10.1016/j.jadohealth.2017.02.006. PMID: 28455129.
- Hagen L, Keller T, Neely S, DePaula N, Robert-Cooperman C. Crisis communications in the age of social media: a network analysis of Zika-related tweets. Soc Sci Comput Rev. 2018;36(5):523–41. doi:10.1177/0894439317721985.
- Keim-Malpass J, Mitchell EM, Sun E, Kennedy C. Using Twitter to understand public perceptions regarding the #HPV vaccine: opportunities for public health nurses to engage in social marketing. Public Health Nurs. 2017;34(4):316–23. doi:10.1111/phn.12318. PMID: 28261846.
- Fuller MY, Allen TC. Let’s have a Tweetup. The case for using Twitter professionally. Arch Pathol Lab Med. 2016;140(9):956–57. doi:10.5858/arpa.2016-0172-SA. PMID: 28261846.
- Parsi K. Why can’t we be friends? A case-based analysis of ethical issues with social media in health are. AMA J Ethics. 2015;17(11):1009–18. doi:10.1001/journalofethics.2015.17.11.peer1-1511.
- Ventola CL. Social media and health care professionals: benefits, risks, and best practices. Pharm Ther. 2014;39(7):491–520. PMID: 25083128
