?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Differences in obtaining a vaccine vary based on a multitude of factors including perceptions of vaccine safety, efficacy and willingness to pay (WTP). This study focuses on parent perceptions toward a vaccine for COVID-19 including their WTP decisions for their children and themselves. A mixed methods design using a cross-sectional survey was used to assess the perceptions of US parents, with children under 18, in response to the COVID-19 pandemic. The survey was administered online in November 2020 and 584 final responses were collected. The questionnaire consisted of approximately 37 closed and open-ended questions regarding personal background information; awareness, knowledge, and experience of the virus; perception toward vaccines and COVID-19; and the contingent valuation of a hypothetical COVID-19 vaccine. WTP was found to be higher for children and a direct relationship between the number of children and WTP was observed. Parents were willing to pay US$228–$291 for a vaccine for themselves and US$243–US$321 for their children. A positive impact on WTP was found with self-reported parent health status but not children. The findings of this study have important implications for policy programs which require detailed cost-benefit analyses. WTP for a COVID-19 vaccine is crucial to determine the partial benefits of vaccinating to reduce the risk of repetitive widespread outbreaks.
Introduction
The novel coronavirus COVID-19 is causing tremendous health consequences while creating economic havoc across the globe. Exactly 1 year after the first known COVID-19 patient in the United States (US), more than 113 million people around the world have contracted the disease with more than 29 million coming from the US.Citation1 This highly infectious disease has caused over 500,000 deaths in US in 1 year with 2.5 million deaths worldwide across 215 countries.Citation1 The medical community around the world has been working diligently to obtain the most effective COVID-19 vaccines to assist in ending this deadly pandemic.
The ability to stop the spread of this disease rests primarily on human behavior. Parents’ decisions whether to vaccinate their children against communicable diseases show great variability.Citation2,Citation3 Vaccine hesitancy for parents has surfaced over increases in autismCitation4 and timing of injections,Citation5 ingredients,Citation6 and anxiousnessCitation7 despite their being considered the most effective approach against an infectious disease outbreak.Citation2 Concerns, fears and misinformation can be seen as an indicator of declined confidence in vaccines.Citation8 Parents question their health-care providers to a higher degreeCitation9 and school exemptions to vaccinate have increasedCitation10 are indicators supporting vaccine hesitancy concerns.
While parental confidence, attitudes and perceptions toward vaccines have been investigated in the literature,Citation2,Citation9,Citation11 their WTP for a vaccine during a pandemic has yet to be adequately explored in the US. Little evidence is also available to compare risk-based health decisions taken on behalf of children. Gathering data about parents’ acceptance of and the WTP for a COVID-19 vaccine during the peak of this pandemic is essential to accurately assess vaccination decisions for their children and themselves when the health threats are not based on a hypothetical outbreak.
WTP values were assessed through a Contingent Valuation Model (CVM) which is a widely used non-market valuation technique to estimate the economic values of environmental goods and services that are not purchased and sold in markets. This survey-based approach has also been utilized in health care to estimate the values of various services such as of vaccines using stated preference information.Citation12–15 Estimates have been made for vaccines such as Dengue,Citation16 Ebola,Citation17 Hepatitis B,Citation18 Chikungunya fever,Citation19 Human Papillomavirus,Citation20,Citation21 and diseases caused by Meningococcus BCitation22 and COVID-19.Citation11,Citation13
This study focuses on parent perceptions toward a vaccine for COVID-19. Differences in obtaining a vaccine will vary based on a multitude of factors including perceptions of vaccine safety, efficacy and WTP. This study aimed to explore each of these areas among parents of children less than 18 years old. A cost-benefit analysis (CBA), comparison of the expected costs and benefits of a vaccine, may utilize the preference elicitation of willingness to improve health based on the stated WTP values.Citation23 Even though the US government announced that Americans would receive the vaccines for free during the pandemic, an accurate estimation of demand is a crucial step to assess the effectiveness of the current vaccination program.
Materials and methods
The university's Institutional Review Board provided approval for this study. Confidentiality and privacy rights of participants were observed throughout. Upon entry and prior to beginning the survey, participants were informed they were giving their voluntary consent to participate in the study. If participants chose to withdraw, they could do so at any time by exiting the survey.
Survey instrument description
An online questionnaire composed of multiple parts was constructed. The facial validity was established by trained survey researchers and pilot data was collected among a sample of 50 to ensure the questionnaire was performing appropriately and to validate the initial WTP bids. The questionnaire consisted of approximately 37 closed and open-ended questions regarding 1) personal background information; 2) awareness and knowledge of COVID-19; 3) perceptions toward COVID-19 and vaccines; 4) experience of COVID-19 and 5) contingent valuation of a hypothetical COVID-19 vaccine. Survey respondents, on average, answered 33 questions with a mean completion time of 14 minutes.
Target population, recruitment & procedure
This study targeted self-identifying parents in the US. A parent was defined as having a child under 18 years of age. Survey administration occurred online across November 2020. Qualtrics, a survey technology solution, provided an online representative sample and data collection for this project. Participants were recruited from various sources, including website intercept recruitment, member referrals, targeted e-mail lists, gaming sites, customer loyalty web portals, permission-based networks, and social media to provide a few examples. A mixed methods design using a cross-sectional survey strategy to assess the perceptions of parents in response to the COVID-19 pandemic was utilized. Socio-demographic and health-based quotas were implemented to ensure that the dataset would represent the characteristics of the US population.
Contingent valuation approach
The CVM is a non-market valuation technique that relies heavily on stated preferences to estimate the value of a product or an amenity. One of the common fields of application is the health care where private demands of various products such as drugs and vaccines can be estimated. As a part of CVM, respondents are directly asked to state their WTP for the product in question after they are given a full description of a scenario. Double bounded dichotomous choice (DBDC) with an open-ended max WTP question was the preferred method in this study due to its ability to produce a more accurate set of WTP values and participants’ familiarity with the yes or no pricing questions.Citation24,Citation25
According to Hanemann,Citation26 incorporating the dichotomous questions to extract WTP values can be explained by a random utility model where consumers make choices from a set of alternatives to maximize their utility (U):
Where represents the set of choices.
To assess preferences regarding a hypothetical COVID-19 vaccine, the participants of the survey who agreed to pay out of pocket were asked the following questions for themselves and their children:
Would you be willing to pay $X per dose for COVID-19 Vaccine for yourself (children)?
The initial bid amount () was randomly distributed from a range of prices (US$25, US$50, US$80, US$112.5, US$174) which was determined based on the pre-survey testing responses and the average prices of similar vaccines in the US.Citation27 If the answer to the first bid (
) was a yes (no), a follow-up question with the second bid (SBn) value was directed to each respondent where
= 2
=
. Another set of dichotomous questions were not included as the added complexity of a third lag was not found to improve the accuracy or the depth of the DBDC model.Citation28 Regardless of the answer to the
, the respondent was asked to state his or her maximum WTP (MWPTn) for the vaccine.
For the participants who answered the first and second bidding questions Yes/Yes or No/No, their stated MWPTn was considered as their final bids. If a participant accepted (rejected) the first bid but rejected (accepted) the second one, the midpoint of the first and second bids instead of the answer to the open-ended question (
) was considered as the respondent’s WTP.
Some of the responses were marked as “protest answers” if the respondents rejected all bids and answered 0 to the open-ended questions. These observations along with the contradictory responses to the WTP and open-ended questions were censored. After eliminating the outliers using the boxplot method, the final sample size consisted of 584 responses. This is well above the threshold of a minimum sample size of 385 needed to have an accurate representation of a population with at least 1 million people with 95% confidence interval.Citation29
Statistical model
A multivariate linear regression was performed to investigate how various independent variables would impact the WTP for a COVID-19 vaccine. The WTP values were transformed using a natural logarithm function (ln) to reduce the skewness in data. The initial bid (FBn) and the age of the child were randomly distributed to minimize the occurrence of anchoring effect bias. The empirical model can be presented as follows:
Where WTP = willingness to pay; α = intercept; β = coefficient of each independent variable; X = each independent variable. presents the independent variables considered in this study.
Table 1. Variable definitions and descriptive statistics (N = 584)
To test for heteroskedasticity in residuals, the Bresich-Pagan test was performed. The results confirmed the models for parents and their children were both homoscedastic. While the Shapiro-Wilk normality tests confirmed that the data was normally distributed, the presence of multicollinearity was checked by computing the Variation Inflation Factor (VIF)s. Because the highest VIF value was 1.87, which was lower than the threshold of 10, we ruled out multicollinearity between independent variables.Citation30
Results and discussion
Demographic and background characteristics
Surveyed parents were predominately female (56%) with a college education (64%) and an annual income between US$40,000–US$80,000 with almost an average of 2 children (µ = 1.985 SD = 1.127). The majority of parents self-indicated good or very good health and very good or excellent health for their children. Less than 5% of the parents and children survey had contracted COVID-19 at the time of the survey. also shows that most parents (56%) know children infected with COVID-19 are less likely to develop severe illness compared with adults. A majority of parents indicated beliefs that the complications of COVID-19 are serious (83%) and a public health threat (81%) while being worried their child(ren) would get infected (74%) and were afraid of their child(ren) experiencing symptoms (69%). Nearly 72% of parents indicated vaccines being important in preventing disease.
Estimations of willingness to pay
Two multivariate linear regression models were executed to assess the impact of independent variables on WTP for the vaccine for parents (Model-1) and their children (Model-2). The results are presented in . While a set of socioeconomic variables were included in each model, the factors associated with health, knowledge, perceived risk, and experience with the virus were tailored for each model based on their relevance and importance.
Table 2. Variables associated with willingness to pay (WTP as natural log form) for Covid-19 vaccine from linear regression models
The regression results indicated that income was positively associated with adults’ WTP for a COVID-19 vaccine for themselves and their children. This is especially important for model validation as the positive relationship between income and WTP is highly anticipated in contingent valuation studies.Citation31
The statistical relationship between the set of perceived risk variables, complications, threat, and prevention, and parents’ WTP for a hypothetical COVID-19 vaccine was consistent with the previous studiesCitation32–34 that determined if individuals were aware of the potential risks of a virus or disease, they would be willing to pay more for a potential solution. These variables did not show any variation in terms of statistical significance or how they impact the WTP when they were added to the second model.
Self-reported health status of parents was found to have a positive impact on WTP but a statistically significant impact of children’s health status on WTP in the second model was not observed. The existing literature has mixed findings about the effects of respondents’ perceived health ratings on the value of a vaccine. Wong et al.Citation21 conducted a study using the health belief model to assess the roles of various predictors of WTP for a COVID-19 vaccine, including health status, in Malaysia and found no statistically significant relationship. Even though Garcia and CerdaCitation13 did not evaluate the impact on health status, they found that respondents with chronic diseases were more likely to pay a price premium for a COVID-19 vaccine. The relationship between improved health status and higher WTP may be evaluated within the context of the positive correlation between self-reported health and income suggested by Larrimore;Citation35 Hildebrand and Van Kerm.Citation36
While the knowledge of the virus had positive impact on the WTP for children, it had no statistically significant effect on WTP for parents themselves. A similar scoring system for virus knowledge was incorporated into CVM models in some of the first studies that examined the WTP for a hypothetical COVID-19 vaccine.Citation13,Citation37 While the knowledge contributed positively to higher WTP in Chile, it was found to have no impact in Ecuador. The increasing significance and importance of knowledge when children are involved may be due to parental altruism toward children. For instance, Dickie and GerkingCitation38 found that parents’ WTP for skin cancer reduction risk was higher for their children than themselves.
Male, African-American and Black respondents were the only demographics who were willing to pay more for a COVID-19 vaccine for their children. Males’ higher WTP for a vaccine was observed in a similar study that investigated the value of a hypothetical COVID-19 vaccine in Ecuador,Citation37 though the respondents were not asked to state their pricing preferences for their children. Brown et al.Citation39 examined how mothers’ preferences would impact WTP for human papillomavirus vaccine for their daughters in the US. Black population were found to be more likely to choose a vaccine for protection of their daughters.
One interesting and unique finding of Model-2 is that as the number of children increased in a household, the WTP for child vaccination increased. When parents make decisions about vaccinations for their children, the budgetary limitations may be important especially if the parents are self-paying and the household size is larger. However, this income and price effect may be dominated by health concerns that having more unvaccinated children may increase the possibility of spreading the virus in the household. This finding was echoed in research conducted by Sourborn et al.Citation40 where number of children in the household significantly and positively influenced the WTP for hypothetical childhood malaria vaccine in rural Burkina Faso.
Mean and median willingness to pay
The mean and median WTP for a hypothetical COVID-19 vaccine for parents and their children are presented in . To compare the WTP values, parametric and non-parametric values were also computed. The estimated mean values are consistent with parametric and non-parametric values which validates the estimates of linear regression. Parents are willing to pay significantly more for a COVID-19 vaccine for their children than themselves, confirming the parental altruism outlined throughout the study. In summary, each parent, on average, would be willing to pay approximately US$228–US$291 for a vaccine for themselves and US$243–US$321 for their children.
Table 3. Parametric and non-parametric estimates of the mean and median WTP for Covid-19 vaccines
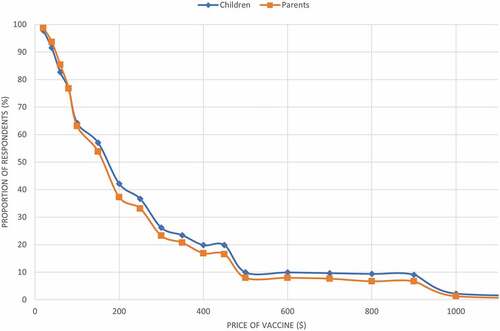
shows the parents’ demand curves for the hypothetical COVID-19 vaccine for themselves and their children based on the cumulative distribution of WTP values. When the price of the vaccine is above US$100, parents are willing to pay more for their children than themselves. As the vaccine becomes more expensive, their altruistic intuition may be the driving force of the difference in WTP for themselves and their children. If the COVID-19 vaccine was not fully subsidized by the Federal government, at the price of US$80 for two doses, 76% of Americans would be willing to vaccinate themselves and their children which would help achieving herd immunity.
Results help assess parents’ valuation of risk for themselves and their children when the health crisis is not based on a hypothetical outbreak but a real-life pandemic situation. The analysis of data collected during this outbreak reveals important clues about the factors associated with parents’ acceptance of a vaccine given differences in income, age, perceived risk, and personal attitude toward vaccines.
Several potential limitations may apply to this study that can impact internal and external validity. Not all useful information may have been captured, leading to an internal validity threat with mostly closed-format questions.Citation41 Since respondents are self-reporting data, socially desirable answers and recall errors merit consideration. Response rate could affect external validity, although due to quota sampling, this study is not expected to be at any greater threats to external validity than the typical survey.Citation42 Of course, due to the cross-sectional design of the study no relationship between cause and effect can be implied. Another limitation to note is that expectations of a fully subsidized vaccine may have impacted the respondents’ stated preferences.
Conclusions
This study provides an insight into the differences between parents’ WTP for a COVID-19 vaccine for themselves and their children. Our results highlight that parents, on average, are willing to pay more (US$287) for a vaccine for their children than themselves (US$260). The results of this study will have important implications for policy makers as an incredible amount of effort has already been given to fight this outbreak. Public policy programs require detailed cost-benefit analyses and WTP for a COVID-19 vaccine would be crucial to determine the partial benefits of finding the right treatment or vaccine to reduce the risk of contraction and repetitive widespread outbreaks.
Authors’ contributions
Serkan Catma and Diana Reindl contributed equally to this research manuscript. The survey preparation and data organization was led by Diana Reindl. Statistical modeling and interpretation of the results were performed by Serkan Catma. The first draft of the manuscript was written by Diana Reindl and Serkan Catma. After incorporating the comments from both authors, the final draft was organized and approved.
Consent to participate
Participants in the survey were informed that their involvement was completely voluntary, and the survey could be stopped anytime. They were assured that their responses were anonymous and confidential. All respondents provided informed consent.
Consent for publication
Both authors provided consent for submitting the final manuscript to the journal, and if accepted, for the publication of the manuscript.
Disclosure of potential conflicts of interest
There are no conflicts of interest or competing interest to declare.
Data availability material
The datasets and other study materials are available upon request.
Additional information
Funding
References
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf Dis. 2020;20(5):534–534. doi:10/1016/S1473-3099(20)30120-1.
- Kennedy A, LaVail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff. 2011;30(6):1151–59. doi:10.1377/hlthaff.2011.0396.
- Low MSF, Tan H, Hartman M, Tam CC, Hoo C, Lim J, Chiow S, Lee S, Thng R, Cai M, et al. Parental perceptions of childhood seasonal influenza vaccination in Singapore: a cross-sectional survey. Vaccine. 2017;35(45):6096–102. doi:10.1016/j.vaccine.2017.09.060.
- Offit P. Vaccines and autism revisited: the Hannah Poling case. N Engl J Med. 2008;358(20):2089–91. doi:10.1056/NEJMp0802904.
- Offit PA, Quarles J, Gerber MA, Hackett CJ, Marcuse EK, Kollman TR, Gellin BG, Landry S. Addressing parents’ concerns: do multiple vaccines overwhelm or weaken the immune system? Pediatrics. 2002;109(1):124–29. doi:10.1542/peds.109.1.124.
- Chatterjee A, O’Keefe C. Current controversies in the USA regarding vaccine safety. Expert Rev Vaccines. 2010;9(5):497–502. doi:10.1586/erv.10.36.
- Stern AM, Markel H. The history of vaccines and immunization: familiar patterns, new challenges. Health Aff (Millwood). 2005;24(3):611–21. doi:10.1377/hlthaff.24.3.611.
- Black S, Rappuoli R. A crisis of public confidence in vaccines. Sci Transl Med. 2010;2(61):61–68. doi:10.1126/scitranslmed.3001738.
- Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 Health Styles survey. Pediatrics. 2011;127(Suppl 1):S92–9. doi:10.1542/peds.2010-1722N.
- Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360(19):1981–88. doi:10.1056/NEJMsa0806477.
- Wong LP, Alias H, Wong PF, Lee HY, Sazaly A. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. doi:10.1080/21645515.2020.1790279.
- Asgary A. Assessing households’ willingness to pay for an immediate pandemic influenza vaccination programme. Scand J Public Health. 2012;40:412–17. doi:10.1177/1403494812453884.
- Garcia LY, Cerda AA. Contingent assessment of the COVID-19 vaccine. Vaccine. 2020;38(34):5424–29. doi:10.1016/j.vaccine.2020.06.068.
- Goldman RD, McGregor S, Marneni SR, Katsuta T, Griffiths MA, Hall JE, Seiler M, Klein EJ, Cotanda CP, Gelernter R, et al. Willingness to vaccinate children against influenza after the coronavirus disease 2019 pandemic. J Pediatr. 2020;1–7. doi:10.1016/j.jpeds.2020.08.005.
- Harapan H, Mudatsir M, Yufika A, Nawawi Y, Wahyuniati N, Anwar S, Yusri F, Haryanti N, Wijayanti NP, Rizal R, et al. Community acceptance and willingness-to-pay for a hypothetical Zika vaccine: a cross-sectional study in Indonesia. Vaccine. 2019;37(11):1398–406. doi:10.1016/j.vaccine.2019.01.062.
- Yeo HY, Shafie AA. The acceptance and willingness to pay (WTP) for hypothetical dengue vaccine in Penang, Malaysia: a contingent valuation study. Cost Eff Resour Alloc. 2018;16(60):1–10. doi:10.1186/s12962-018-0163-2.
- Mudatsir M, Anwar S, Fajar JK, Yufika A, Ferdian MN, Salwiyadi S, Imanda AS, Azhars R, Ilham D, Timur AU, et al. Willingness-to-pay for a hypothetical Ebola vaccine in Indonesia: a cross-sectional study in Aceh. F1000Res. 2019;8(1441):1441. doi:10.12688/f1000research.20144.1.
- Rajamoorthy Y, Radam A, Taib NM, Rahim KA, Munusamy S, Wagner AL, Mudatsir M, Bazrbachi A, Harapan H. Willingness to pay for hepatitis B vaccination in Selangor, Malaysia: a cross-sectional household survey. PLoS ONE. 2019;14(4):e0215125. doi:10.1371/journal.pone.0215125.
- Sarmento TTR, Godói IP, Reis EA, Godman B, Ruas CM. Consumer Willingness to pay for a hypothetical chikungunya vaccine in Brazil and the implications. Expert Rev Pharmacoecon Outcomes Res. 2019:1–8. doi:10.1080/14737167.2020.1703181.
- Cerda AA, García LY, Albornoz DV. Parents willingness to pay for a humanpapillomavirus vaccine to protect their adolescent daughters. Maule Region, Chile. Salud publica de Mexico. 2014;56:48–55.
- Wong CK, Man KKC, Ip P, Kwan M, McGhee SM. Mothers’ preferences and willingness to pay for humanpapillomavirus vaccination for their daughters: a discrete choice experiment in Hong Kong. Value Health. 2018;21(5):622–29. doi:10.1016/j.jval.2017.10.012.
- Marshall H, Chen G, Clarke M, Ratcliffe J. Adolescent, parent and societal preferences and willingness to pay for meningococcal B vaccine: a discrete choice experiment. Vaccine. 2016;34(5):671–77. doi:10.1016/j.vaccine.2015.11.075.
- Park M, Jit M, Wu JT. Cost-benefit analysis of vaccination: a comparative analysis of eight approaches for valuing changes to mortality and morbidity risks. BMC Med. 2018 Sep 5;16(1):139. PMID: 30180901; PMCID: PMC6123970. doi:10.1186/s12916-018-1130-7.
- Bateman IJ, Carson RT, Day B, Hanemann M, Hanleys N, Hett T, Jones-Lee M, Loomes G, Mourato S, Ozdemiroglu E, et al. Economic valuation with stated preference techniques: a manual. Cheltenham (UK): Edward Elgar; 2002. ISBN 1840649194.
- Boyle KJ. Contingent valuation in practice. In: Champ, Patricia A., Boyle, Kevin J., Brown, Thomas C editors., A primer on nonmarket valuation. Dordrecht, The Netherlands: Springer; 2017. p. 104.
- Hanemann M. Welfare evaluations in contingent valuation experiments with discrete responses. Am J Agric Econ. 1984;66(3):332–41. doi:10.2307/1240800.
- Centers for Disease Control and Prevention. CDC vaccine price list. National Center for Immunization and Respiratory Diseases; 2021 [accessed 2021 Feb 1]. https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html.
- Cooper JC, Hanemann M Referendum contingent valuation: how many bounds are enough? Paper Presented at the American Agricultural Economics Association Convention in San Diego, CA, USA; Economic Research Service: Washington, DC; 1995.
- Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–10. doi:10.1177/001316447003000308.
- Lin FJ. Solving multicollinearity in the process of fitting regression model using the nested estimate procedure. Qual Quant. 2008;42(3):417–26. doi:10.1007/s11135-006-9055-1.
- Palanca-Tan R. The demand for a dengue vaccine: a contingent valuation survey in Metro Manila. Vaccine. 2008 Feb 13;26(7):914–23. doi:10.1016/j.vaccine.2007.12.011.
- Rajamoorthy Y, Radam A, Taib NM, Rahim KA, Wagner AL, Mudatsir M, Munusamy S, Harapan H. The relationship between perceptions and self-paid hepatitis B vaccination: a structural equation modeling approach. PLoS ONE. 2018;13:e0208402. doi:10.1371/journal.pone.0208402.
- Basu R. Willingness-to-pay to prevent Alzheimer’s disease: a contingent valuation approach. Int J Health Care Finance Econ. 2013 Dec;13(3–4):233–45. PMID: 23996130. doi:10.1007/s10754-013-9129-2.
- Liu JT, Hammitt JK, Wang JD, Tsou MW. Valuation of the risk of SARS in Taiwan. Health Econ. 2005 Jan;14(1):83–91. PMID: 15386665. doi:10.1002/hec.911.
- Larrimore J. Does a higher income have positive health effects? Using the earned income tax credit to explore the income-health gradient. Milbank Q. 2011 Dec;89(4):694–727. PMID: 22188352; PMCID: PMC3250638. doi:10.1111/j.1468-0009.2011.00647.x.
- Hildebrand V, Van Kerm P. Income inequality and self-rated health status: evidence from the European community household panel. Demography. 2009;46(4):805–25. doi:10.1353/dem.0.0071.
- Sarasty O, Carpio CE, Hudson D, Guerrero-Ochoa PA, Borja I. The demand for a COVID-19 vaccine in Ecuador. Vaccine. 2020 Dec;38(51):8090–98. doi:10.1016/j.vaccine.2020.11.013.
- Dickie M, Gerking S. Genetic risk factors and offsetting behavior: the case of skin cancer. J Risk Uncertain. 1997;15(1):81–97. doi:10.1023/A:1007789921003.
- Brown DS, Johnson FR, Poulos C, Messonnier ML. Mothers’ preferences and willingness to pay for vaccinating daughters against human papillomavirus. Vaccine. 2010;28(7):1702–08. ISSN 0264-410X. doi:10.1016/j.vaccine.2009.12.024.
- Sauerborn R, Gbangou A, Dong H, Przyborski JM, Lanzer M. Willingness to pay for hypothetical malaria vaccines in rural Burkina Faso. Scand J Public Health. 2005;33(2):146–50. PMID: 15823976. doi:10.1080/14034940510005743.
- Price J, Murnan J. Research limitations and the necessity of reporting them. Am J Health Educ. 2004;35(2):66–67. doi:10.1080/19325037.2004.10603611.
- Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–06. doi:10.1001/jama.2012.3532.