ABSTRACT
Background
In the absence of definitive treatment, vaccination against COVID-19 emerged as an effective solution to the spread of the pandemic. This study aimed to investigate the factors impacting the rates of COVID-19 vaccine acceptance in Jordan, in addition to examining the relationship between COVID-19 risk perception and vaccine acceptance among the Jordanian population.
Methods
This cross-sectional study was conducted among a sample of adults (aged ≥18) residing in Jordan. Data were collected using an online questionnaire disseminated using social media platforms between December 2nd and December 29th, 2020.
Results
A total of 2,268 (72.3%) participants demonstrated willingness to receive the COVID-19 vaccine. The mean COVID-19 risk perception score among the participants was 4.65 out of 10 (median 5; IQR 3–6). Higher risk perception scores were significantly associated with being female (p = .001), young (p < .001), or a smoker (p = .005). A significant positive correlation was identified between COVID-19 vaccine acceptance and risk perception scores (OR = 1.319, 95%, CI = 1.261–1.380, p < .001). Moreover, male participants (75%, OR = 1.220, 95% CI = 1.007–1.479, p = .043), participants aged 18–24 years (78.1%, OR = 1.635, 95% CI = 1.189–2.246, p = .002), and participants with children aged under 18 years (73.9%, OR = 1.210, 95% CI = 1.010–1.450, p = .039) were more willing than their counterparts to get vaccinated.
Conclusion
COVID-19 risk perception and certain sociodemographic characteristics (i.e., being male, being young, and having children aged under 18 years) were found to be significantly associated with vaccine acceptance. Policymakers are recommended to develop public educational campaigns to enhance people’s trust in and willingness to take the COVID-19 vaccine.
Introduction
The emergence and spread of the coronavirus disease 2019 (COVID-19) came with negative impacts and unprecedented challenges that affected the physical and mental well-being of people worldwide.Citation1 Although COVID-19 was announced a global pandemic over a year ago, survivors of the disease are still healing from its devastating effects, whilst others are battling active infective episodes of circulating variants of severe acute respiratory syndrome coronavirus 2 (SARS-COV2).Citation2,Citation3
In the absence of definitive treatment, vaccination against COVID-19 emerged as an effective solution to the spread of the pandemic.Citation4 In Jordan, rollout of COVID-19 vaccines began in December 2020 following the Jordan Food and Drug Administration’s (JFDA) approval of both BNT162b2 (Comirnaty, Pfizer-BioNtech) and BBIBP-CorV (Sinopharm, Beijing CNBG) for emergency use.Citation5 By March 2021, three more vaccines had been approved by the JFDA for emergency use (AZD1222, Oxford-AstraZeneca; JNJ-78436735, Johnson & Johnson; and Gam-COVID-Vac, Sputnik V). Although the approval of multiple COVID-19 vaccines has provided hope for controlling the pandemic, other multi-dimensional factors may impact COVID-19 vaccine uptake among the Jordanian population.Citation4,Citation5
Risk perception is an estimate of person’s future probability of contracting certain diseases in light of behavioral and temporal factors.Citation6 In terms related to COVID-19, a person with lower perceived risk of getting infected with COVID-19 is expected to be reluctant to undertake any precautionary measures leading, ultimately, to lower odds of vaccine uptake compared to counterparts.Citation6,Citation7 With risk perception considered a major driver of behaviors, COVID-19 risk perception may be a core factor in the low level of vaccine acceptance (i.e., vaccine hesitancy) among the Jordanian population despite the availability of the vaccine.Citation6,Citation7 Unfortunately, vaccine hesitancy can be pervasive, misguided, and contagious.Citation8,Citation9 Moreover, vaccine hesitancy has been suggested to impede herd immunity against COVID-19, which has been defined as immunity that is achieved when around 70% of the population have been vaccinated against COVID-19 and developed protective antibodies against future infection.Citation10 It is worth noting that with the development of the Delta variant of Coronavirus, experts have suggested that 90% of the population should be vaccinated to achieve herd immunity.Citation11
Understanding the factors that influence people’s acceptance toward taking the COVID-19 vaccine is critical, especially given the vaccine-related rumors and conspiracy theories that have been spreading on social media and other online platforms.Citation12 The spread of misinformation can negatively impact people’s confidence in taking the vaccine, hence disrupting national and international efforts to control the spread of the disease.Citation13 Moreover, the active involvement of healthcare providers, including pharmacists, in leading public awareness campaigns and their involvement in administrating the COVID-19 vaccine have been proposed as potential strategies for promoting vaccine acceptance.Citation14 Therefore, the current study aimed to investigate the factors impacting the rates of COVID-19 vaccine acceptance in Jordan, in addition to examining the relationship between COVID-19 risk perception and vaccine acceptance among the Jordanian population.
Methods
Study design
The current study used a cross-sectional design among a sample of adults (aged ≥18) residing in Jordan. An online questionnaire via SurveyMonkey® was disseminated using social media platforms, including Facebook, Twitter, and WhatsApp, and the enrollment of participants lasted between December 2nd and December 29th, 2020. Data collection was initiated after the authorization of the BNT162b2 (Comirnaty, Pfizer-BioNtech) and BBIBP-CorV (Sinopharm, Beijing CNBG) COVID-19 vaccines for emergency use by the JFDA and prior to the beginning of the COVID-19 vaccination campaign in Jordan (i.e., January 13, 2021). Approval to conduct this study was obtained from the Institutional Review Board at King Abdullah University Hospital (IRB number: 3/137/2020).
Survey instrument
The study questionnaire was adapted (with permission) from previous workCitation15,Citation16 and translated into Arabic following ISPOR’s Principles of Good Practice for Translation and Cultural Adaptation.Citation17 The adapted questionnaire consisted of four parts. The first part aimed to collect the participants’ basic sociodemographic information (i.e., age, gender, education, and employment status). The second part was a COVID-19 risk perception scale that comprised 10 items scored on a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. The third part of the questionnaire aimed to assess participants’ views on COVID-19 vaccine administration and enforcement, whilst the fourth part aimed to assess the factors related to COVID-19 vaccine hesitancy. The questionnaire also included a question about whether the participants had received the influenza vaccine in the preceding five years.
Sample size
The online sample size calculator Rao Soft® was used to calculate the minimum sample size. The number of adults (i.e., aged 18 years or over) in Jordan is approximately 3,500,000. The sample size generated by the software was 601 adults using a margin of error of 4% and a confidence interval of 95%.
Statistical analysis
Responses to the online questionnaire were exported to the Statistical Package for the Social Sciences (IBM SPSS) version 25 (IBM Corporation, Armonk, NY, USA), with incomplete responses excluded from the final analyses. Descriptive statistics (i.e., percentages and frequencies) were used to analyze the demographic characteristics of the participants. Responses to the risk perception scale were dichotomized (0 = strongly disagree/disagree/neutral; 1 = agree/strongly agree), and the risk perception score was calculated by summing the participants’ dichotomized responses. The total possible risk perception score ranged from 0 to 10, with higher scores indicating higher COVID-19 risk perception. Chi-square analysis and one-way ANOVA were performed to compare the mean risk perception, COVID-19 vaccine acceptance, and previous influenza vaccine uptake scores based on the different sociodemographic variables. Moreover, binary logistic regression with a stepwise backward model was used to assess the association of participants’ intention (i.e., binary variable) to take COVID-19 vaccine (i.e.,dependent variable) with the sociodemographic variables and risk perception scores (i.e., independent variables).
Results
A total of 3,121 participants completed the questionnaire, of whom 2,304 (73.8%) were female and 1,521 (48.7%) aged between 18–24 years (). The majority of the participants were unemployed (n = 1,846; 59.1%), and 77% (n = 2,404) had completed post-secondary education (). The mean COVID-19 risk perception score was 4.65 SD 1.9: median 5; IQR 3–6). Risk perception scores were significantly higher (p < .001) among participants who had COVID-19 vaccine acceptance (median 5; IQR 4–6) than among participants who did not have COVID-19 vaccine acceptance (median 4; IQR 3–5). Further, younger participants, female participants, and smokers had significantly higher risk perception scores than did older participants (p < .001), male participants (p = .001), and nonsmokers (p = .005), respectively ().
Table 1. COVID-19 vaccine acceptance and risk perception mean scores across sociodemographic characteristics
Most of the participants reported a willingness to take the COVID-19 vaccine (n = 2,268, 72.3%), among whom 94.1% (n = 2,134) reported that they would accept to take the vaccine if it was recommended by a physician and 28.2% (n = 639) if recommended by a pharmacist. Moreover, 2,658 participants (85.2%) reported that they believed that physicians should administer the vaccines, whilst 945 reported (30.3%) that pharmacists should also be authorized to administer the vaccines (). Over two-thirds of the participants did not agree that governments and employers should enforce COVID-19 vaccination on citizens and employees, and this disagreement was significantly higher among participants who were unwilling to take the vaccine (p = .001).
Table 2. Participants’ views on COVID-19 administration and enforcement
Upon exploring the differences in attitudes toward the COVID-19 vaccine (), there were statistically significant differences in responses to the items within all domains (p < .001) except for the domain related to the cost of the vaccine (p = .784). As compared to participants who were willing to take the vaccine, participants who refused to take the vaccine had higher mean scores for the items related to the potential of side effects precipitation (3.0 (0.92) vs. 2.5 (0.78)) and liability to getting sick following vaccination (2.9 (0.91) vs. 2.3 (0.80)). Interestingly, participants who were willing to take the vaccine had higher mean scores for the item related to the possible death causality of the COVID-19 vaccines (2.9 (0.85) vs. 2.5 (0.99)). Moreover, participants who were willing to be vaccinated were more likely than participants who were unwilling to be vaccinated to believe that the vaccines would help in controlling the spread of COVID-19 infection, recovering the economy, and minimizing the burden on healthcare systems (mean scores 3.6 (0.81) vs. 2.8 (0.91), 3.7 (0.82) vs. 2.9 (0.97), and 3.1 (0.94) vs. 3.9 (0.76), respectively).
Table 3. Factors related to COVID-19 vaccine hesitancy
The binary logistic regression assessed the association between risk perception and vaccine acceptance adjusting for gender, age, and living with children (less than 18 years) (). Males a had a greater odds ratio (OR) for vaccines acceptance than did females (95% CI = 1.007–1.479, p = .043). Besides, younger participants’ (i.e., 18–24 years) also had 1.635 greater odds for vaccine acceptance in comparison to older age groups(≥55 years) (95% CI = 1.189–2.246, p = .002). In addition, participants who had children aged under 18 years were more likely than their counterparts to report vaccine acceptance (OR = 1.210, 95% CI = 1.010–1.450, p = .039). Moreover, COVID-19 risk perception was found to predict vaccine acceptance (OR = 1.319, 95%, CI = 1.261–1.380, p < .001) indpendent from other factos.
Table 4. Binary logistic regression for COVID-19 vaccine acceptance by sociodemographic variables
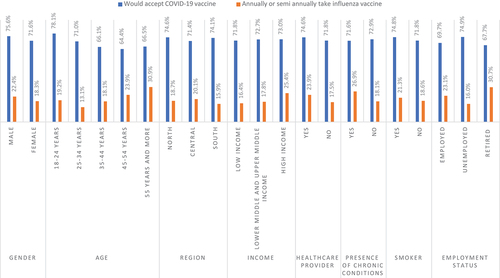
Reported influenza vaccine uptake was compared to reported COVID-19 vaccine acceptance in light of the sociodemographic characteristics of the participants in order to identify whether having received the seasonal influenza vaccine predicted COVID-19 vaccine acceptance (). Firstly, although participants with higher income level were more willing than low-income participants to take the COVID-19 vaccine (73% vs 71.8%; ), only a quarter of participants with high income had received the seasonal influenza vaccine (25.4%; ). Further, 78.1% of participants aged 18–24 years reported COVID-19 vaccine acceptance, though only 19.2% reported seasonal influenza vaccine uptake. Lastly, although two thirds of chronic disease sufferers reported high vaccine acceptance, the influenza vaccine uptake percentage among the same group was lower than expected (71.6% vs. 26.9%, respectively).
Discussion
In the present study, 72.3% of the participants demonstrated willingness to receive COVID-19 vaccination, and COVID-19 risk perception was significantly associated with vaccine acceptance. Moreover, male participants, participants aged 18–24 years, and participants who had children aged under 18 years were more willing than their counterparts to get vaccinated.
The majority of the participants (72.3%) reported willingness to be vaccinated against COVID-19 if this was recommended by a healthcare professional (e.g., physician or pharmacist) and proven to be safe and effective. Similar results have been reported in Germany (70%), the Netherlands (73%), Italy (74%), France (75%), and Portugal (75%).Citation18,Citation19 On the other hand, lower acceptance rates have been reported by other studies in Jordan (28.4%-37.4%)Citation20,Citation21 and other countries such as Kuwait (23.6%-53.1%), Poland (57%), and Russia (55%).Citation20,Citation22,Citation23 The present study findings suggest that willingness to take the COVID-19 vaccine should be sufficient for achieving COVID-19 herd immunity, based on the previous herd immunity threshold of 70%. However, a sharp increase in the herd immunity threshold to around 90% or more has been proposed in light of the development of the Delta variant of Coronavirus.Citation24 Moreover, the rate of acceptance toward taking COVID-19 vaccines was at least three times higher than the rate of influenza annual or semiannual vaccine uptake (n = 605, 19.4%). One logical explanation for this difference is that 66.2% of the participants believed COVID-19 to be more severe than influenza.
Our study results indicated that male participants had a significantly lower mean COVID-19 risk perception score (4.9, SD 1.91) than did females (4.6 SD 1.87), although vaccine acceptance among male participants (75.6%) was significantly higher than among female participants (71.6%). Similar findings have been reported by other studies around the world.Citation15,Citation19,Citation23 According to Sallam et al., females in Jordan rely on social media platforms as a source of information regarding the COVID-19 outbreak and vaccination, and therefore, they are more likely than males to believe vaccine-related conspiracies.Citation20,Citation25,Citation26 Moreover, in the present study, rates of COVID-19 vaccine acceptance were higher among participants who had children than among participants who did not have children (73.9% vs. 69.9%). At the time of data collection for this study, there were no data to suggest the safety of COVID-19 vaccination for children. However, there was no significant difference in the mean COVID-19 risk perception scores between the two groups. A previous study in Turkey reported that 63.7% of the participating parents were unwilling to have their children vaccinated against COVID-19, although 59.9% were willing to get vaccinated themselves.Citation27 Therefore, it is possible that participants who had children had higher acceptance toward getting vaccinated as an indirect measure to protect their children from becoming infected with COVID-19, since children were unable to receive the vaccine at the time this study was conducted.
In this study, nearly one third of the participants believed that pharmacists should be authorized to administer COVID-19 vaccines. This is an interesting finding considering the fact that pharmacists in Jordan were granted authorization to administer the influenza vaccine in August 2020 (i.e., only four months prior to data collection for this study). In a previous study in Jordan, pharmacists reported that administering COVID-19 vaccines in community pharmacies would expedite the vaccination process, encourage more people to get vaccinated, and increase vaccine accessibility.Citation14,Citation28,Citation29
Moreover, in the present study, participants who were unwilling to get vaccinated against COVID-19 had greater concerns regarding vaccine safety and were more skeptical toward the effectiveness of the vaccines, as compared to their counterparts. This finding comes consistent with findings reported by previous studies.Citation13,Citation19 Furthermore, nearly 30% of the participants believed that the government and employers should mandate getting vaccinated against COVID-19. A study conducted in the United States found that 40.9% of the participants accepted their state government mandating COVID-19 vaccination for adults, while 47.7% of the participants accepted employers mandating the vaccination of their employees.Citation30 However, mandatory vaccination can reduce public support by overriding personal autonomy, ultimately reducing vaccine uptake.Citation31
The current study highlights the need to involve healthcare professionals (e.g., physicians and pharmacists) to positively influence the population’s acceptance for COVID-19 vaccine.Citation15 In addition, policymakers are encouraged to grant trained pharmacists the authority to offer and administer COVID-19 vaccine in community pharmacies or as part of mass vaccination campaigns.Citation14 Moreover, authorities can employ social media to encourage anti-vaccine and undecided people to ensure global immunity, hence slowing the emergence of new variants of the virus.
Limitations
Although the large number of retrieved responses adds to the reliability and generalizability of the study findings, there are a few limitations to the present study. Firstly, the sample may not be representative for some demographic groups (i.e., insufficient representation of the south region, and the majority of respondents were female and from a young age group). Secondly, data were collected online through social media networks using a self-report tool, which may have led to selection bias. However, the use of a large study sample is expected to have counteracted potential selection bias. Furthermore, the present study explored vaccine acceptance among Jordanians prior to the development of currently identified variants of coronavirus (e.g., the Delta variant), which may have affected the way people envision the protective and harmful effects of available vaccines. Thus, it is highly recommended to conduct a series of follow-up studies with change detection analysis as we progress through the COVID-19 pandemic in order to obtain an accurate and up-to-date reflection of vaccine acceptance among the Jordanian population.
Conclusion
In conclusion, the majority of our study participants demonstrated willingness to receive COVID-19 vaccination. COVID-19 risk perception and certain sociodemographic characteristics (i.e., being male, being young, and having children aged under 18 years) were found to be significantly associated with vaccine acceptance. The results of the present study underpin the importance of collaborative multidisciplinary campaigns to enhance public trust in COVID-19 vaccination. In this regard, healthcare providers (including physicians and pharmacists among others) can play an active role as leaders of mass public evidence-based campaigns to enhance people’s trust in COVID-19 vaccination. Furthermore, attitudinal surveillance is encouraged to get better insights regarding stems of vaccination hesitancy among general population.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, Tran BX, Hussain S, Hoang MT, Le XT, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PloS One. 2021;16(2):e0246824. doi:10.1371/journal.pone.0246824.
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta bio-medica: Atenei Parmensis. 2020;91(1):157–7. doi:10.23750/abm.v91i1.9397.
- Centers for Disease Control and Prevention (CDC). SARS-CoV-2 variant classifications and definitions. 2021 [accessed 2021 Nov 9]. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html .
- Edwards B, Biddle N, Gray M, Sollis K. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PloS One. 2021;16(3):e0248892. doi:10.1371/journal.pone.0248892.
- Jordan–COVID19 vaccine tracker [accessed 2021 Nov 9]. https://covid19.trackvaccines.org/country/jordan/ .
- Brewer NT, Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behavior. Ann Behav Med. 2004;27(2):125–30. doi:10.1207/s15324796abm2702_7.
- World Health Organization. Report of the Sage working group on vaccine hesitancy. Published 2014 [accessed 2021 Nov 9]. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf .
- Wiyeh AB, Cooper S, Nnaji CA, Wiysonge CS. Vaccine hesitancy ‘outbreaks’: using epidemiological modeling of the spread of ideas to understand the effects of vaccine related events on vaccine hesitancy. Expert Rev Vaccines. 2018;17(12):1063–70. doi:10.1080/14760584.2018.1549994.
- Wiysonge CS, Ndwandwe D, Ryan J, Jaca A, Batouré O, Anya BPM, Cooper S. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Hum Vaccin Immunother. Published online 2021 March 8;1–3. doi:10.1080/21645515.2021.1893062.
- John TJ, Samuel R. Herd immunity and herd effect: new insights and definitions. Eur J Epidemiol. 2000;16(7):601–06. doi:10.1023/A:1007626510002.
- Liu Y, Rocklöv J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J Travel Med. 2021;28(7). doi:10.1093/JTM/TAAB124.
- Islam MS, Kamal AHM, Kabir A, Southern DL, Khan SH, Hasan SMM, Sarkar T, Sharmin S, Das S, Roy T, et al. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PloS One. 2021;16(5):e0251605. doi:10.1371/journal.pone.0251605.
- Larson HJ, Smith DMD, Paterson P, Cumming M, Eckersberger E, Freifeld CC, Ghinai I, Jarrett C, Paushter L, Brownstein JS, et al. Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect Dis. 2013;13(7):606–13. doi:10.1016/S1473-3099(13)70108-7.
- Mukattash TL, Jarab AS, Abu Farha RK, Nusair MB, Al Muqatash S. Pharmacists’ perspectives on providing the COVID-19 vaccine in community pharmacies. J Pharm Health Serv Res. 2021;12(2):313–16. doi:10.1093/jphsr/rmab008.
- Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi:10.1016/j.eclinm.2020.100495.
- McFadden SM, Malik AA, Aguolu OG, Willebrand KS, Omer SB. Perceptions of the adult US population regarding the novel coronavirus outbreak. PloS One. 2020;15(4):e0231808. doi:10.1371/journal.pone.0231808.
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P. Principles of good practice for the translation and cultural adaptation process for patient‐reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8(2):94–104. doi:10.1111/j.1524-4733.2005.04054.x.
- Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–06. doi:10.1016/j.vaccine.2020.09.041.
- Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. The European Journal of Health Economics. Published online 2020;21(7):977–82. doi:10.1007/s10198-020-01208-6.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. doi:10.3390/vaccines9010042.
- El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;16(4):e0250555. doi:10.1371/journal.pone.0250555.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi:10.1038/s41591-020-1124-9.
- Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, Almansouri W, Alzalzalah S, Ziyab AH. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Principles Pract. 2021;30(3):262–71. doi:10.1159/000514636.
- Dyer O. Covid-19: delta infections threaten herd immunity vaccine strategy. Published online 2021.
- Sallam M, Dababseh D, Yaseen A, Al-Haidar A, Taim D, Eid H, Ababneh NA, Bakri FG, Mahafzah A . COVID-19 misinformation: mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PloS One. 2020;15(12):e0243264. doi:10.1371/journal.pone.0243264.
- Sallam M, Dababseh D, Yaseen A, Al-Haidar A, Ababneh NA, Bakri FG, Mahafzah A. Conspiracy beliefs are associated with lower knowledge and higher anxiety levels regarding COVID-19 among students at the University of Jordan. Int J Environ Res Public Health. 2020;17(14):4915. doi:10.3390/ijerph17144915.
- Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID‐19 vaccine: a cross sectional study. Int J Clin Pract. Published online 2021;75(9):e14364. doi:10.1111/ijcp.14364.
- Nusair MB, Arabyat R, Mukattash TL, Alhamad H, Ghaida MTA, Momani MY. Pharmacists’ perspectives on providing the influenza vaccine in community pharmacies: a qualitative study. Risk Manag Healthc Policy. 2020;13:2179. doi:10.2147/RMHP.S265133.
- Alhamad H, Abu-Farha R, Albahar F, Jaber D. Public perceptions about pharmacists’ role in prescribing, providing education and delivering medications during COVID-19 pandemic era. Int J Clin Pract. 2021;75(4):e13890. doi:10.1111/IJCP.13890.
- Largent EA, Persad G, Sangenito S, Glickman A, Boyle C, Emanuel EJ. US public attitudes toward COVID-19 vaccine mandates. JAMA Network Open. 2020;3(12):e2033324–e2033324. doi:10.1001/jamanetworkopen.2020.33324.
- Gostin LO, Salmon DA, Larson HJ. Mandating COVID-19 vaccines. Jama. 2021;325(6):532–33. doi:10.1001/jama.2020.26553.