ABSTRACT
Objective: To determine the knowledge and attitude on infant vaccination among a couple of Universiti Putra Malaysia (UPM) staffs in Serdang, Selangor. Methods: A cross-sectional study was carried out involving 97 respondents. A cluster sampling technique for the categorization of the faculty in UPM to science-based and non-science-based is used. Then, fishbowl technique was adopted in selecting the faculty from the two categorizations, which consists of 1) science-based: Faculty Biotechnology and Science Biomolecule and Faculty of Science; 2) non-science-based: Faculty of Economics and Management and Faculty of Language and Communication. Consequently, a simple random method was used to choose the respondent based on the inclusion and exclusion criteria. Data on socio-demographic characteristic, knowledge and attitude regarding infant vaccination were collected using a modified and pretested questionnaire. The data then were analyzed using SPSS version 22. Results: Of 97 respondents, 78 (80.4%) had high knowledge, and 49 (50.5%) have moderate attitude regarding infant vaccination. Overall, science-based faculty and non-science-based faculty prevalence of refuse infant vaccination was 2.1%, 6.5%, respectively. There was a significant association between educational level and the knowledge (p < .05, p = .019). However, there was no significant association between socio-demographic and attitude. Other than that,, there was no association between knowledge and attitude among these two different types of faculty (P > .05, p = .256, p = .597). Conclusion: Effort are needed for focusing on health education campaign with collaboration between health-care professionals, social media and community to improve their awareness for immunization.
Introduction
A vaccine is one of the most extraordinary findings in the medical field. Instead, Lim et al.Citation1 stated that it is the most effective and cheapest method to prevent or reduce the burden of vaccine-preventable disease; it is a biological preparation that increases body immune system toward targeted disease.Citation2 The vaccine is made from weakened or killed microbes. Toxins or surface protein from this microorganism will stimulate the body immune system to destroy and memorize it so that the immune system can easily detect and destroy any of the microorganism in the next encounter.Citation3 World Health Organization has estimated that immunization has averted between 2 and 3 million deaths each year.Citation4
Recently, there are reported cases where parents refuse to complete their children’s vaccination. Reported by Bedford et al.,Citation5 vaccination safety scare has led to long-term reductions in coverage, as evidenced by reduced coverage of Measles-Mumps-Rubella (MMR) vaccine in many countries post the suggested the association with autism. While most people vaccinate according to the recommended schedule, this success is being challenged by individuals and groups who choose to delay or refuse vaccine.Citation6
Edward Janner was the first person to the introduced vaccine against smallpox in 1796. It happens, when he discovered that daily house cleaners with cowpox were immune to smallpox.Citation7 Meanwhile, in the history of the sentiment anti-vaccination, there was a growth of the anti-vaccine group in England. This was due to a study by Andrew Wakefield, published in the Journal Lancet in 1998, claiming that the vaccine causes autism. In his study of 12 autism children, linking the problem is due to the measles, mumps, and rubella (MMR) injection. According to his study, the substance in MMR vaccine named thimerosal that functions to stabilize the vaccine is associated with the cause of autism. Since then, the anti-vaccine group has become increasingly contagious.
According to the Centers for Disease Control and Prevention,Citation8 the studies have shown that there was no link between receiving the vaccine and developing of autism. In 2011, a study by DeStefanoCitation9 of the Institute of Medicine (IOM) on eight vaccines given to children and adults found that with rare exceptions, these vaccines are very safe. Additionally, in the previous 14 years’ study from numerous countries, it is shown that there were no linking vaccines to autism.Citation10 The transmission can happen when people have direct contact with the contaminated urine of infected animals or indirectly through the exposure to water or soil that contaminated with urine or secretion of infected animals.
For the past few years, a measles outbreak was detected in many European countries during July 2014–June 2015.Citation11 In 2015, it was estimated that 61% of children who have measles have no immunization; in which 28% are not immunized, and 33% of children are not eligible for injection.Citation12 According to Mohd Azizi et al.,Citation13 for the past decades, Malaysia has achieved more than 95% immunization coverage among infants and young children.
However, the cases of vaccine refusal have been increased from 470 cases to 1292 cases in the year 2013–2014. The increase of cases was regarding the number of parents with children aged below 2 years that refusing the vaccination for their child. More worsen; the diphtheria cases had become more distinct with the reemergence in June 2016. Further, investigation revealed that deceased infants did not receive the complete set of recommended vaccination, which they lead to the complication developed by the infection.Citation14 Previous studies on childhood immunization have reported that the misconception for the knowledge and negative attitudes among parents regarding the immunization.Citation15 According to Ministry of Health Malaysia,Citation12 the infant stage is the most vulnerable time for children to develop their immune system. Parents’ knowledge and attitude regarding immunization are the most important factors on the immunization status of their children.Citation16 Much has been published regarding childhood immunization in Malaysia.Citation17–25 Nevertheless, a number on immunization is little available on immunization coverage in institutes of higher education. Due to that, this study was conducted to determine the level of knowledge and attitude regarding infant-vaccination among married staff in science-based and non-science-based faculties in UPM, Selangor.
Material and methods
Study location and study design
A cross-sectional study was conducted between June 2021 to August 2021 involves 97 staff in two different types of faculty in Universiti Putra Malaysia (UPM), Selangor. UPM has 16 faculties which include non-science-based categories (Economics and Management, Modern Languages and Communication Design and Architecture and Educational Studies) and another science-based (Agriculture, Engineering, Computer Science and Information Technology, Medicine and Health Sciences, Science, Veterinary Medicine, Biotechnology and Biomolecular Sciences, Food Science and Technology, Forestry and Environment). The total university staff is 7,968 was obtained from website.
Sample size and sampling method
Sample size estimation was done using a formula as described by Lemeshow et al.Citation26 The sampling method used has two stages, which were cluster and simple random sampling, respectively. In stage one, by applying cluster sampling, all the faculty in UPM was divided into two groups, which was science-based and non-science-based. Then, two faculties from each category were selected by using fishbowl technique. Consequently, the purposive sampling method was used to choose the respondent based on the inclusion criteria.
Data collection
Inclusion criteria
Staff in the chosen faculty who have married and have children.
Instrument
The primary tool of this study was a questionnaire, which involved three parts: The first part of the questionnaire reflects on the socio-demographic characteristics of the respondents. This part includes the educational level, type of faculty, work classification, family income, decision-maker for immunization, source of information about Vaccination and from where their children get the vaccination. The second was the knowledge item regarding the general question on childhood vaccination such as the advantages and disadvantages of vaccines. The third and last parts were related to the attitude of the parents toward the vaccination regarding the acceptance of vaccination and the opinion of parents toward safety and effectiveness of the vaccination as a primary prevention of infectious disease either they refuse vaccination for their children and the underlying factors of the refusal. The reliability of the questionnaire in this study was 0.8. This questionnaire was modified from the previous study.Citation27 A pilot study was conducted for internal consistency of the questionnaire. The Cronbach’s alpha values around 0.7.
Study approval
The research proposal was submitted and approved by the Research Ethics Committee (JKEUPM) of University Putra Malaysia (JKEUPM-2-17-184) before the data collection started.
Data analysis
Data analysis was conducted using SPSS version 22. The correct response for knowledge of the respondents were assigned 1 and incorrect response assigned 0. The responses were added together to generate a total knowledge score ranging from a minimum of 0–15, and the overall score was referring to Modified Bloom’s cut off.Citation28 A score of 80–100% of correct response meant an excellent knowledge; a score of 50–79% put a scorer in a moderate level and a poor knowledge with a score less than 50% of the correct response. This scoring applies the same for the attitude. Higher score of attitude 80–100, 50–79 for moderate attitude, and <50 for low attitude, respectively. Response to attitude was on a 4-point Likert-type scale. Descriptive and chi-square test and Fisher’s Exact test were used in this study.
Results
A total of 97 respondents that were selected, all participated and completed the questionnaire giving a response rate of 100%. shows that most of the respondents consist of female staff, 68 (70.0%). Malay 94 (96.90) was the highest respond in this study, as most of the staff in UPM consist of Malay staff. More than half 84 (86.6) of the couple make a decision together for their children immunization, and most of them, 68 (70.1) get it from government hospital/clinics. Most of respondents 50 (51.50) were age more than 35, and 39 (40.20) of them have a moderate family monthly income. Doctor 75 (77.3) and internet 64 (66.0) were the primary sources of vaccine information. Distribution of respondents’ according to faculty was almost the same, but for the occupation, the non-academic staff was more which was 67 (69.1) compared to academic staff 30 (30.9).
Table 1. Distribution of sociodemographic
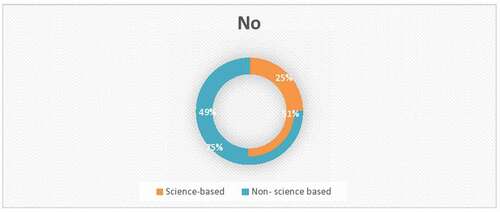
Based on , shows the prevalence of infant vaccination by faculty among the staff of UPM. Of the 97 respondents, 4 (4.1%) had refuse infant vaccination. For science-based faculty, only one (2.1%) respondent of 48 refuses infant vaccination, while for non-science-based faculty, 3 (6.5%) of 49 respondents choose to refuse infant vaccination.
shows that 78 (80.4) of the respondents have high knowledge, and only 2 (2.1) have in-depth knowledge. While for attitude, 49 (50.5) have a moderate attitude and only 1 (1.0) shown low attitude regarding infant vaccination.
Table 2. Level of knowledge and attitude
Based on , there was a significant association between educational level and the level of knowledge (p-value = .019). shows that there was no significant association between socio-demographic and attitude (p-value > 0.05). In addition, shows that there is no significant association between knowledge and attitude between these two different types of faculty.
Table 3. Association between socio-demographic and knowledge
Table 4. Association between socio-demographic and attitude
Table 5. Comparison of knowledge and attitude between staff in science-based and non-science-based faculty
Discussion
Overall, the level of knowledge on infant-vaccination among UPM staff was considered as high with 78 (80.4%), while most of them have moderate attitude 49 (50.5%). This might be due to nowadays of messages and vaccination policy much more easily obtained from healthcare providers and immunization coverage by hosting immunization program. This result is consistent with other studies showed that parents who obtained information from healthcare providers were more likely to have better knowledge on childhood immunization.Citation29,Citation30 In addition, the majority of respondents in this study had moderate attitude. Possible reasons for this attitude might be due to parents living in urban area has good availability and easy to get access can contribute to favorable attitude toward infant vaccination. The results of the current study are supported by Zhang et al.Citation31 shows that the urban population has acceptance and their positive attitude toward acceptance of vaccination. For item, vaccination is used to cure disease, and given starting after birth, there was 1% of the respondent that answer no. Most of the respondent know that vaccine is vital to prevent disease in the community, and they agreed that they need more information about the vaccine.
The association between knowledge and socio-demographic (age, gender, educational level, and monthly income) among the staff have been studied. The result shows that there is a significant association (χ2 = 4, p-value = .019) between knowledge and the educational level as the p-value is less than 0.05. This might be due to the fact that university staff are easy to get more information than the general population which makes them advantageous over part of the others society. This finding was consistent with Ahmed Abdulrahman et al.,Citation15 which stated that there is a significant association between educational level and knowledge on vaccination. As reported by Tauil et al.,Citation32 low educational level and low socioeconomic status were both associated with incomplete or delayed vaccination.
However, for the gender, monthly income and age show that there is no significant association as all the p-value is more than 0.05. For the age aspects, this finding contrasts with the previous study by Omar et al.Citation4 conducted in Saudi Arabia, which showed that there is an association between paternal age and knowledge and attitude toward child vaccination.
The high level of knowledge shows female has a high percentage of which 56 (82.35%), compared to male, only 22 (75.86%). In the study by Qutaiba et al.Citation33 shows that there is a significant association between parent’s gender and knowledge regarding immunization. Mother’s knowledge is an important factor to decision makers for childcare and vaccine decision.Citation34–38 However, male partners were often cited as being against vaccinating the children.Citation39–44 The total number of staff that refuse infant-vaccination was 4 (4.1%). For science-based faculty, only one (2.1%) respondent of 48 refuses infant vaccination, while for non-science-based faculty, 3(6.5%) of 49 respondents choose to refuse infant-vaccination. From the previous, the study by Danova et al.Citation45 stated that there were 2.29% cases of refusal, which is a statistically significant increase in trend. A majority, 3 (3.1%) of the respondent who refuses vaccination agree that time constraint and poor quality of information is the main reason why they do not vaccinate their children. The hectic schedule of work was one of the factors of the time constraints. These findings were constant with the study by Lim et al.,Citation46 which stated that the majority of the parents claimed to be busy with work as a result of not vaccinating their children. As reported by Danova et al.,Citation45 it was stated that there was an association between sources of information and refusal of vaccination. In that study, it is shown that refusing parents have been mostly looking for information about vaccination on web pages which not all the information given there is the real fact which is low quality. Other than that, Forster et al.Citation47 stated that parent’s distrust in the government originated from historic health scares that remained in their memories, believing that government conceals information also one of the vaccine hesitancy factors.
The level of knowledge and attitude on infant-vaccination have been studied among staff in science-based and non-science-based faculty. The p-value is >0.05 where (x2 = 2, p-value = .256), which show that there is no significant association between knowledge and attitude between these two different types of faculty. This was due to them have access vaccination coverage from the same geographical area to immunization service which educated them to increase their knowledge and attitude toward infant immunization uptake.
In this study, the abundance of Malay respondents may because Malay constitute the highest percentage, which is 68.6% of the population in Peninsular Malaysia.Citation48 Most of the respondents, 75 (77.3%), choose a doctor as their primary source of information regarding immunization. These findings were constant with Enkel et al.,Citation49 which stated that those who expressed more significant concerns about vaccines were likely to get the information from medical professionals. This finding is consistent with other studies reported that the physicians are important role of giving the correct information delivery of vaccinations during childhood and to influence parents decisions to make the right decisionCitation50–55 compare than Internet-based vaccine information that reaches parents contains antivaccine content quite obvious.Citation56–59
Limitations
This study only targeted the UPM staff in specific faculty. Hence, the finding of this study may not be generalized to other communities. Besides, the researcher has limited access to approach academic staff, as most of them have a packed schedule. Due to that, the number of academic respondents who return the questionnaire was less than half compared to non-academic staff. Nonetheless, this study has strength that provides knowledge and attitude and associated factors of infant vaccination among staff university which data limited in this area and can be a baseline data for undertake any further intervention.
Conclusion
The study revealed that over half of the respondents had immense knowledge regarding infant vaccination. However, the attitude was moderate. Despite the findings of this study, the educational level plays an important role to improve the knowledge regarding infant vaccination. As the doctor was the primary source for getting information about vaccination, therefore, the healthcare professionals or doctor should take benefit from this study result by educating parents by planning more open and effective communication with them because this knowledge and attitude can affect their compliance to the completion of vaccination.
Acknowledgments
The authors would like to thank, Mr. Azrin Shah Abu Bakar who had contributed to this study. The authors would also like to thank all staff involved in the study for their support and cooperation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Lim KK, Chan YY, Ani AN, Rohani J, Norfadhilah ZAS, Santhi MR. Complete immunisation coverage and its determinants among children in Malaysia: findings from the National Health and Morbidity Survey (NHMS) 2016. Public Health. 2017;153:52–7. doi:10.1016/j.puhe.2017.08.001.
- Ministry of Health Malaysia and the Department of Islamic Development Malaysia. Frequently asked questions on vaccines and immunisation. 2014 [accessed 2019 Jul 22]. World Health Organization. 22 July 2019. http://www.myhealth.gov.my/en/frequently-asked-questions-on-vaccines-and-immunisation/.http://www.infosihat.gov.my/infosihat/isusemasa/faq_vaccines_immunisation/pdf/faq_vaccines_immunisation.pdf .
- World Health Organization. Vaccines. 2017 [accessed 2019 Jul 22]. http://www.who.int/topics/vaccines/en/on2017/november16.
- Omar Alfahl S, Alharbi KM. Parents’ knowledge, attitude, and practice towards childhood vaccination, Medina, Saudi Arabia 2017. Neonatal Pediatr Med. 2017;3(1):1–8. doi:10.4172/2572-4983.1000126.
- Bedford H, Attwell K, Danchin M, Marshall H, Corben P, Leask J. Vaccine hesitancy, refusal, and access barriers: the need for clarity in terminology. Vaccine. 2017:1016–18. doi:10.1016/j.vaccine.2017.08.004.
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, and Larson HJ. Vaccine hesitancy, and healthcare providers. Vaccine. 2016;34(52):6700–06. doi:10.1016/j.vaccine.2016.10.042.
- Stefan R. Edward Jenner and the history of smallpox and vaccination Proc (Bal Univ Med Cent). 2005;18(1):21–25 doi:10.1080/08998280.2005.11928028.
- Centers for Disease Control and Prevention. Vaccines do not cause autism. 2015 [accessed 2019 Jul 22]. https://www.cdc.gov/vaccinesafety/concerns/autism.html .
- DeStefano F. Vaccines, and autism: evidence does not support a causal association. Clin Pharmacol Ther. 2007;82(6):756–59. doi:10.1038/sj.clpt.6100407.
- The importance of childhood immunisation. 2016 [accessed 2019 Jul 22]. https://immunise4life.my/who-needs-to-be-immunised/on2017/October/20 .
- Cvjetkovic SJ, Jeremic VL, Tiosavljevic DV. Knowledge and attitudes toward vaccination: a survey of Serbian students. J Infect Public Health. 2017;10(5):649–56. doi:10.1016/j.jiph.2017.05.008.
- Ministry of Health Malaysia. Childhood immunisation coverage, 2015. Health Fact; 2016.
- Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. doi:10.1016/j.vaccine.2017.04.010.
- Balbir Singh HK, Badgujar VB, Yahaya RS, Rahman SA, Sami FM, Badgujar S, Govindan SN, Ansari MT. Assessment of knowledge and attitude among postnatal mothers towards childhood vaccination in Malaysia. Hum Vaccin Immunother. 2019;15(11):2544–51. doi:10.1080/21645515.2019.1612666.
- Ahmed Abdulrahman YM. Parents′ knowledge and attitudes on childhood immunization, Taif, Saudi Arabia. J Vaccines Vaccin. 2014;05(1):1–5. doi:10.4172/2157-7560.1000215.
- EPHIEE, ICF. Ethiopia mini demographic and health survey 2019: key indicators. Rockville, Maryland, USA: EPHI and ICF; 2019.
- Hussin H, Marzo RR, Mamat N, Safee NF, Omar N, Yin TS. The barriers of child immunization completion among parents in the community health centre, Johor Bahru. J Pharm Res Int. 2020;32(4):48–58. doi:10.9734/JPRI/2020/v32i430425.
- Rumetta J, Abdul-Hadi H, Lee Y. A qualitative study on parents’ reasons and recommendations for childhood vaccination refusal in Malaysia. J Infect Public Health. 2019;13(2):199–203. doi:10.1016/j.jiph.2019.07.027.
- Islahudin F, Shah NM, Hasim N. Determinants of childhood vaccine hesitancy among Malaysian youths. Determinants of childhood vaccine hesitancy among Malaysian youths. Arch Pharm Pract. 2019;11:15–22.
- Aziz S, Iqbal MZ, Iqbal MS, Mohiuddin SG, Sivadasan S, Veerasamy R, Ali AN, Prajapati SK, Chandran JM. Attitude towards vaccination: a cross-sectional study among the parents in Sungai Petani, Kedah, Malaysia. Int J Pharm Sci Res. 2018;10(5):2465–72. doi:10.13040/IJPSR.0975-8232.10(5).2465-72.
- Abdullah AC, Nor Afiah MZ, Rosliza AM. Predictors for inadequate knowledge and negative attitude towards childhood immunization among parents in Hulu Langat, Selangor, Malaysia. Malaysian J Public Health Med. 2018;18:102–12.
- Abdullah AC, Nor Afiah MZ, Rosliza AM. Practice of childhood immunizations among parents and their associated factors in Hulu Langat, Selangor, Malaysia. Int J Public Health Clin Sci. 2016;3:94–104.
- Ansari MT, Jamaluddin NN, Ramlan TA, Zamri N, Majeed S, Badgujar V, Sami F, Hasnain MS, Singh HKB. Knowledge, attitude, perception of Muslim parents towards vaccination in Malaysia. Hum Vaccin Immunother. 2021;17(3):785–90. doi:10.1080/21645515.2020.1800325.
- Ahmad NA, Jahis R, Kuay LK, Jamaluddin R, Aris T. Primary immunization among children in Malaysia: reasons for incomplete vaccination. J Vaccines Vaccin. 2017;8:358. doi:10.4172/2157-7560.1000358.
- Yusof NYM, Zulkefli NAM, Ismail S, and Rashid MFA . Inadequate health literacy on childhood immunization and its predictors among antenatal mothers. Malaysian J Med Health Sci. 2017;13(3):43–50 .
- Lemeshow S, Hosmer DW Jr, Klar J, Lwanga SK. Part 1: statistical methods for sample size determination. Adequacy Sample Size Health Stud. 1990:247. doi:10.1186/1472-6963-14-335.
- Lahajang AM, Rasyidah Z, Qamarina A. Knowledge, attitude, and practice on childhood vaccination among staff in UPM. Serdang, Selangor, Malaysia: Project paper (Doctor of Medicine (MD)) - Universiti Putra Malaysia; 2014.
- Enquselassie F, Ayele W. Knowledge, attitude, and practice (KAP) towards screening for cervical cancer among Adama University female students. Vaccine. 2015:40–45.
- Al-lela OQB, Bahari MB, Bahari MB, Al-Qazaz HK, Salih MRM, Jamshed SQ, Elkalmi RM. Are parents’ knowledge and practice regarding immunization related to pediatrics’ immunization compliance? a mixed method study. BMC Pediatr. 2014;14(1):1–7. doi:10.1186/1471-2431-14-20.
- Zhang X, Wang L, Zhu X, Wang K. Knowledge, attitude and practice survey on immunization service delivery in Guangxi and Gansu, China. Soc Sci Med. 1999;49(8):1125–27. doi:10.1016/s0277-9536(99)00199-9.
- GebreEyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, Mewahegn AA, Feleke DG, Chanie ES. Knowledge, attitude, and practices of parents about immunization of infants and its associated factors in Wadla Woreda, North East Ethiopia, 2019. Pediatric Health Med Ther. 2021;12:223–38. doi:10.2147/PHMT.S295378.
- Tauil MDC, Paula A, Sato S, Waldman EA. Factors associated with incomplete or delayed vaccination across countries: a systematic review. Vaccine. 2016;34(24):2635–43. doi:10.1016/j.vaccine.2016.04.016.
- Qutaiba B, Al-Lela O, Bahari MB, Al-Qazaz HK, Salih MR, Jamshed SQ, Elkalmi RM. Are parents’ knowledge and practice regarding immunisation related to pediatrics’ immunisation compliance? A mixed-method study. BMC Paediatr. 2014;14(1):20. doi:10.1186/1471-2431-14-20.
- Wu AC, Wisler-Sher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, Benin AL. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern Child Health J. 2008;12(6):766–73. doi:10.1007/s10995-007-0302-4.
- Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prev Med. 2000;31(1):49–55. doi:10.1006/pmed.2000.0677.
- Rahman MM, Islam MA, Mahalanabis D. Mothers’ knowledge about vaccine preventable diseases and immunization coverage of a population with high rate of illiteracy. J Trop Pediatr. 1995;41(6):376–78. doi:10.1093/tropej/41.6.376.
- Al-Ayed IH. Mothers’ knowledge of child health matters: are we doing enough? J Family Community Med. 2010;17(1):22. PMID: 22022667. doi:10.4103/1319-1683.68785.
- Angelillo IF, Ricciardi G, Rossi P, Pantisano P, Langiano E, Pavia M. Mothers and vaccination: knowledge, attitudes, and behaviour in Italy. Bull World Health Organ. 1999;77(3):224. PMID: 10212512.
- Malande OO, Munube D, Afaayo RN, Annet K, Bodo B, Bakainaga A, Ayebare E, Njunwamukama S, Mworozi AE, Musyoki MA. Barriers to effective uptake and provision of immunization in a rural district in Uganda. PloS One. 2019;14:2 e0212270. doi:10.1371/journal.pone.0212270.
- Zewdie A, Letebo M, Mekonnen T. Reasons for defaulting from childhood immunization program: a qualitative study from Hadiya zone, Southern Ethiopia. BMC Public Health. 2016;16:1240. doi:10.1186/s12889-016-3904-1.
- Babirye JN, Rutebemberwa E, Kiguli J, Wamani H, Nuwaha F, Engebretsen IMS. More support for mothers: a qualitative study on factors affecting immunisation behaviour in Kampala Uganda. BMC Public Health. 2011;11:723. doi:10.1186/1471-2458-11-723.
- Babalola S. Maternal reasons for non-immunisation and partial immunisation in northern Nigeria. J Paediatr Child Health. 2014;47:276. doi:10.1111/j.1440-1754.2010.01956.x.
- Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr. 2015;15:31. doi:10.1186/s12887-015-0345-4.
- Bangura JB, Xiao S, Qiu D, Ouyang F, Chen L. Barriers to childhood immunization in sub-Saharan Africa: a systematic review. BMC Public Health. 2020;20(1):1108. doi:10.1186/s12889-020-09169-4.
- Danova J, Salek J, Kocourkova A, Celko AM. Factors associated with parental refusal of routine vaccination in the Czech Republic. Cent Eur J Public Health. 2015;23(4):321–23. doi:10.21101/cejph.a4395.
- Lim WY, Amar-Singh HSS, Jeganathan N, Rahmat H, Mustafa NA, Yusof F-SM, Rahman R, Itam S, Chan CH, N-Julia MS, et al. Exploring immunisation refusal by parents in the Malaysian context. Cogent Med. 2016;3:1–8. doi:10.1080/2331205X.2016.1142410.
- Forster AS, Rockliffe L, Chorley AJ, Marlow LAV, Bedford H, Smith SG, Waller J. A systematic qualitative review of factors influencing parents’ vaccination decision-making in the United Kingdom. SSM Population Health. 2016;2:603–12. doi:10.1016/j.ssmph.2016.07.005.
- Department of Statistics, Malaysia. Population and demographics. 2018 [accessed 2019 July 22]. https://www.dosm.gov.my/v1/index.php?r=column/ctwoByCat&parent_id=115&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 .
- Enkel SL, Attwell K, Snelling TL, Christian HE. ‘Hesitant compliers’: qualitative analysis of concerned fully-vaccinating parents. Vaccine. 2017:6–10. doi:10.1016/j.vaccine.2017.09.088.
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–41. doi:10.1542/peds.2005-1728.
- Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000;106(5):1097–102. doi:10.1542/peds.106.5.1097.
- Sˇ Esˇkutė M, Tamulevičienė E, Levinienė G. Knowledge and attitudes of postpartum mothers towards immunization of their children in a Lithuanian tertiary teaching hospital. Medicina. 2018;54(1):2. doi:10.3390/medicina54010002.
- Kundi M, Obermeier P, Helfert S, Oubari H, Fitzinger S, Yun JA, Brix M, Rath B. The impact of the parent-physician relationship on parental vaccine safety perceptions. Curr Drug Saf. 2015;10(1):16–22. doi:10.2174/157488631001150407104320.
- Kennedy A, LaVail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff. 2011;30(6):1151–59. doi:10.1377/hlthaff.2011.0396.
- Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and perceived credibility of vaccinesafety information for parents. Pediatrics. 2011;127(Supplement1):S107–S12. doi:10.1542/peds.2010-1722P.
- Bean SJ. Emerging and continuing trends in vaccine opposition website content. Vaccine. 2011;29(10):1874–80. doi:10.1016/j.vaccine.2011.01.003.
- Davies P, Chapman S, and Leask J . Antivaccination activists on the world wide web. Arch Dis Child. 2002;87(1):22–25. doi:10.1136/adc.87.1.22.
- Wolfe RM, Sharp LK. Vaccination or immunization? The impact of search terms on the internet. J Health Commun. 2002;10(6):537–51. doi:10.1080/10810730500228847.
- Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30(25):3778–89. doi:10.1016/j.vaccine.2011.11.112.