ABSTRACT
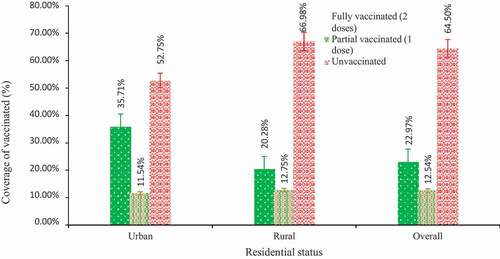
This cross-sectional study was conducted in September 2021 among 1,045 Bangladeshi older adults aged 60 years or above to explore the COVID-19 vaccination coverage and its associated factors. We used a semi-structured questionnaire to collect data on participants’ sociodemographic and lifestyle characteristics, and COVID-19 related information (selected based on an extensive literature review). A multinomial logistic regression model was used to identify the factors independently associated with vaccine receipt. Nearly, two-thirds of the participants (64.5%) were unvaccinated and 12.5% received a single dose. Among the unvaccinated, approximately 94% reported that there was a problem in accessing the vaccine. We found that participants with formal schooling had 42% lower risk of being unvaccinated (RRR (Relative Risk Ratio) = 0.58, 95% CI 0.42–0.80) or 39% lower risk of receiving a single dose (RRR = 0.61, 95% CI 0.39–0.96) than the participants having no formal schooling. The middle family monthly income groups had 65% higher risk (RRR = 1.65, 95% CI 1.17–2.32) and rural participants had 84% higher risk (RRR = 1.84, 95% CI 1.26–2.70) of not receiving vaccines compared to their counterparts. Also, the participants with non-communicable chronic conditions had a significantly lower risk of being unvaccinated (RRR = 0.49, 95% CI 0.35–0.68) or receiving a single dose (RRR = 0.49, 95% CI 0.31–0.77) compared to their counterparts. This finding may help strengthen the existing efforts to maximize vaccine coverage among older populations in Bangladesh and reach herd immunity to break the transmission chain and gain greater overall population protection more rapidly.
Introduction
Globally, various preventive measures including mask mandates,Citation1 social distancing,Citation2 quarantines,Citation3 isolation,Citation4 lockdowns,Citation5,Citation6 and travel restrictionsCitation7 have been enforced to control the spread of COVID-19. Many of these measures have influenced the way of life and thus affected the physical, psychosocial, and economic health and well-being of all populations across the globe.Citation8–10 However, mass vaccination has been regarded as the most efficient means of controlling the spread and severity of the COVID-19 pandemic.Citation9
As of December 2021, 8.75 million doses of 25 approved vaccinesCitation11 have been administered across 184 countries, with an average of 39.8 million doses being administered per day.Citation12 At the current rate, global estimates project that it will take another four months until 75% of the population have received at least one dose of the COVID-19 vaccine.Citation12 Considering the devastating impact of COVID-19 on human beings,Citation13 it becomes imperative to strengthen mass vaccination programs, especially in lower- and middle- income countries (LMICs). Additionally, with some countries experiencing the third wave of COVID-19,Citation9 it is pertinent to prioritize the most vulnerable groups for the vaccination, including people whose age and medical conditions increase their risk of poor COVID-19 outcomes if they become infected among the populations.Citation14,Citation15
Like many other LMICs, Bangladesh started mass COVID-19 vaccination on February 8, 2021.Citation16 As of September 2021, and despite significant efforts, Bangladesh has been able to vaccinate around 10% of its populationCitation17 and continues to struggle to vaccinate the older population groups due to myriad barriers, including vaccine hesitancy (delay in acceptance or refusal of vaccination).Citation16 Vaccine hesitancy has been identified as the most significant barrier against vaccinating mass populations, which hinders high vaccination coverage – the percentage of the vaccinated population.Citation18 However, achieving high vaccination coverage requires rigorous monitoring of vaccination rates and identifying its subsequent barriers and associated factors.
Worldwide, there is a dearth of literature on COVID-19 vaccination rate among older population and the associated factors. However, several studies have discussed Bangladesh’s limited capacity to transport COVID-19 vaccines within a short period, supply-chain management challenges, rumors, stigma, and disinformation as potential barriers to achieving high vaccination coverage.Citation19,Citation20 Furthermore, existing studies in Bangladesh have primarily emphasized COVID-19 vaccine hesitancy,Citation16 associated challengesCitation2, and individuals willingness to vaccinate against COVID-19.Citation21 However, no study examined the COVID-19 vaccination coverage among older people and its associated factors in Bangladesh.
In this study, we aimed to assess the COVID-19 vaccination coverage and the factors associated with it among the older population in Bangladesh. This is a critical piece of research in understanding the state of vaccination coverage in Bangladesh, particularly among the most vulnerable. To our knowledge, this study is the first of its kind in Bangladesh, which has explored the coverage of COVID-19 vaccination and its associated factors among the Bangladeshi older adults, which could be crucial in designing more effective policies to increase vaccination coverage among this high-risk population group.
Materials and methods
Study design and participants
This cross-sectional study was conducted remotely through telephone interviews. The study was conducted by the Aureolin Research, Consultancy and Expertise Development (ARCED) Foundation in September 2021. The primary challenge for this study was to develop a sampling frame to select participants. Thus, we utilized our pre-established registry, which included households from all eight administrative divisions of Bangladesh as a sampling frame. Considering 50% prevalence with a 5% margin of error, at the 95% confidence level, 90% power of the test, and 95% response rate, a sample size of 1096 was calculated. However, 1045 approached eligible participants responded to the study with an overall response rate of approximately 94%. Based on the population distribution of older adults by geography in Bangladesh, we adopted probability proportionate to size (of the eight-division) approach to select older adults in each division.Citation23 The inclusion criterion was the minimum age of 60 years, and the exclusion criteria included adverse mental conditions (clinically diagnosed schizophrenia, bipolar mood disorder, dementia/cognitive impairment), a hearing disability, or inability to communicate.
Measures
Outcome measure
This study considered the present COVID-19 vaccination status among the eligible population in Bangladesh as an outcome variable. The participants were asked the following questions: “Did you receive any COVID-19 vaccination?” The responses were (0 = 2 doses (fully vaccinated), 1 = 1 dose (partially vaccinated) and 2 = Unvaccinated).
Explanatory variables
An extensive review of the literature was carried out before selecting the variables.Citation20,Citation21,Citation24–26 Explanatory variables considered in this study were age (categorized as 60–69, and ≥70), gender (male or female), marital status (married or single), formal education (yes or no), family size (≤4 or >4), family income in Bangladeshi Taka (BDT) (<5,000, 5,000–10,000, >10,000), residence (urban or rural), current occupation (employed, unemployed, or retired), living arrangements (living alone or with family), walking distance to the nearest health center (<30 min or ≥30 min), memory or concentration problems (no problem or low memory or concentration), presence of non-communicable chronic conditions (yes or no), concerned about COVID-19 (hardly, sometimes or often), overwhelmed by COVID-19 (hardly, sometimes or often), difficulty in earning during COVID-19 (yes or no), perceived isolation (hardly, sometimes or often), frequency of communication with friends and family during COVID-19 (less than previous or same as previous), perceived that family members are non-responsive (yes or no), and perceived that they required additional care during COVID-19 (yes or no). Self-reported information on preexisting medical conditions, such as arthritis, hypertension, heart diseases, stroke, hypercholesterolemia, diabetes, chronic respiratory diseases, chronic kidney disease, and cancer, were collected.
Data collection tools and techniques
A pre-tested semi-structured questionnaire was used to collect the information through a telephone interview. Data collection was accomplished electronically using SurveyCTO mobile app (https://www.surveycto.com/) by trained research assistants, recruited based on previous experience of administering health surveys in the electronic platform. The research assistants were trained extensively before the data collection through Zoom meetings.
The English version of the questionnaire was first translated to Bengali language and then back-translated to English by two researchers to ensure the contents’ consistency. The questionnaire was then piloted among a small sample (n = 10) of older adults to refine the language in the final version. The tool used in the pilot study did not receive any corrections/suggestions from the participants concerning the contents developed in the Bengali language.
Statistical analysis
In the descriptive analyses, the characteristics of the study participants were expressed using frequencies and percentages). The association between COVID-19 vaccination status and the variables of greatest interest was analyzed using the chi-square tests with a 5% level of significance. In the analytical exploration, the multinomial logistic regression (MLR) model is the best analytical approach to predict an ordinal dependent variable (i.e., the present COVID-19 vaccination status). Our outcome variable (i.e., the present COVID-19 vaccination status) consisted of three categories: 1 = unvaccinated, 2 = partially vaccinated (single dose received), and 3 = fully vaccinated (two doses received).
An adjusted multinomial logistic regression models were used to identify the potential factors that have a significant role in the higher risk of unvaccinated or partially vaccinated among the most vulnerable and high-risk populations in Bangladesh. Although, there are several model-based variable selection techniques (e.g., Backward elimination, Forward selection, Stepwise selection, and all-possible subset selection). According to the assumption and nature of the data, the study applied a backward elimination criterion with the Akaike information criterion (AIC) for variable selection technique to select variables (i.e., with all potential covariates, ) for the final model with a conventional probability value (p-value) threshold of 0.05. In this study, we applied the backward elimination criteria procedure for variable selection method, which is the simplest of all variable selection methods with potential benefits and easy algorithm as follows: i) This method starts with a full model that considers all of the variables to be included in the model; ii) Variables then are deleted one by one from the full model until all remaining variables are considered to have some significant contribution to the outcome; iii) The variable with the smallest test statistic (a measure of the variable’s contribution to the model) less than the cutoff value or with the highest p value greater than the cutoff value – the least significant variable – is deleted first; iv) Then the model is refitted without the deleted variable and the test statistics or p values are recomputed; v) Again, the variable with the smallest test statistic or with the highest p value greater than the cutoff value is deleted in the refitted model. This process (i–v) is repeated until every remaining variable is significant at the cutoff value. The cutoff value associated with the p value is sometimes referred to as ‘p-to-remove’ and does not have to be set at 0.05. Our main objective was to develop a simple prediction model with easy and routinely available variables. While a set of variables can have significant predictive ability, a particular subset of them may not. Unfortunately, both forward selection and stepwise selection do not have the capacity to identify less predictive individual variables that may not enter the model to demonstrate their joint behavior. However, backward elimination has the advantage to assess the joint predictive ability of variables as the process starts with all variables being included in the model. Backward elimination also removes the least important variables early on and leaves only the most important variables in the model. Adjusted relative risk ratio (RRR) and associated 95% confidence interval (CI) are reported. All analyses were performed using the statistical software package Stata/SE 14.0 (StataCorp, College Station, TX, USA).
Table 1. Characteristics of the participants (N = 1045)
Table 2. Percent unvaccinated and bivariate analysis (N = 1045)
Ethics approval
The institutional review board of the Institute of Health Economics, University of Dhaka, Bangladesh, approved the study protocol (Ref: IHE/2020/1037), and the guidelines of the Declaration of Helsinki were followed in every stage of the study. All participants enrolled in the study provided voluntary verbal informed consents.
Results
Characteristics of the participants
summarizes the characteristics of all the 1045 study participants where 19.0% were from Khulna Division, 75.6% aged 60–69 years, 59.3% male, and 76.5% were currently married. Over half of the participants (51.7%) had no formal schooling, 44.9% had a monthly family income of BDT 5000–10000, 66.8% had a large family size with more than 4 members, 82.6% were residing in rural areas, and 61.1% were either unemployed or retired during the survey period. Around 95% of the study participants resided with their family members, 55.6% resided less than 30 minutes of walking distance from the nearest health center, 64.7% did not suffer from any memory or concentration problems, and 57.2% suffered from any non-communicable chronic conditions. Majority (66.7%) of the participants reported that they were concerned about COVID-19, and 67.9% were overwhelmed by the pandemic, however, 72.7% mentioned that they were not feeling themselves at the highest risk of COVID-19. Moreover, 72.3% faced difficulty in earning during COVID-19, 62.8% did not have change in frequency of communication with friends and family during COVID-19 than previous, 68.7% did not feel isolated from others, 70.6% did not feel that family members were non-responsive, and 73.7% did not feel that they required additional care during the pandemic.
Coverage of COVID-19 vaccination
shows the COVID-19 vaccination coverage among the study participants. The majority (64.5%) of the study participants reported not receiving a single dose of vaccine for COVID-19. Only 23.0% of the participants received double doses of COVID-19 vaccine and 12.5% received a single dose. The bivariate analysis is presented in . We found that the share of unvaccinated participants was relatively higher in Mymensingh Division (71.0%), among female (67.1%), among participant without formal schooling (69.6%), in the lowest income group (71.9%), and among rural participants (67.0%). On the other hand, the share of partially vaccinated participants was relatively higher in Khulna Division (14.7%), among male (14.7%), among participant without formal schooling (13.2%), in the highest income group (15.6%) and among rural participants (12.8‰). The majority (93.8%) of the unvaccinated participants reported that inadequate access to the COVID-19 vaccine was the primary reason for not receiving the COVID-19 vaccine (data not shown).
Factors associated with not receiving the vaccine
shows the factors independently associated with not receiving the COVID-19 vaccine among the study participants in the final adjusted model. Not receiving a vaccine or receiving a single dose only was associated with formal schooling, family monthly income, residence type, and non-communicable chronic conditions.
Table 3. Factors associated with vaccination coverage among the participants (N = 1045)
The participants with formal schooling had around 42% lower risk of being unvaccinated (RRR = 0.58, 95% CI 0.42–0.80) or 39% lower risk of receiving a single dose (RRR = 0.61, 95% CI 0.39–0.96) than the participants having no formal schooling. The middle family monthly income groups had a higher risk (RRR = 1.65, 95% CI 1.17–2.32) of not receiving COVID-19 vaccines. We also found that residents from rural areas had 84% higher odds of not receiving vaccines (RRR = 1.84, 95% CI 1.26–2.70). Moreover, participants with having non-communicable chronic conditions had lower risk of being unvaccinated (RRR = 0.49, 95% CI 0.35–0.68) or receiving a single dose (RRR = 0.49, 95% CI 0.31–0.77) compared to those without non-communicable chronic conditions.
Discussion
This study examined the COVID-19 vaccination coverage rates and its associated factors among the older population in Bangladesh. Our study found that the overall, 23% of the study population was fully vaccinated for COVID-19 until September 2021. The majority of older people (64.5%) were unvaccinated against COVID-19, and problems in accessing vaccines were the main reason for the low vaccination coverage rates among older people. Findings of binary logistic regression analyses showed that ‘not receiving vaccines/being unvaccinated’ was associated with formal schooling, monthly family income, residence type, difficulty in earning during COVID-19 and preexisting non-communicable chronic conditions. There is a growing body of studies on vaccination against COVID-19 in BangladeshCitation16,Citation21 and worldwide.Citation16,Citation20,Citation24–26 However, these studies do not examine the factors associated with low vaccination coverage among older people in resource-limited settings like Bangladesh. Our study extends previous literature through a cross-sectional analysis of the COVID-19 vaccination coverage and its associated factors in Bangladesh.
The current study’s estimated vaccination coverage rate (23%) was substantially below the government of Bangladesh’s targets to inoculate 80% of its population.Citation22 There is limited specific data on COVID-19 vaccination coverage rates in older adults globally to compare our findings with. However, our study’s vaccination coverage rates among older people are broadly comparable with the coverage rates among adults (≥16 years) in Nepal (21.87%; 28.50%) as of 4 October,Citation27 Indonesia (17.2%; 12.93) as of 22 SeptemberCitation28 and Vietnam (9.6%; 40.5%) as of 19 September.Citation29 Furthermore, our study’s vaccination coverage rates were lower than similar lower-middle-income countries, including Sri Lanka (53%; 66%) as of 22 September,Citation30 Cambodia (93%; 99%) of as 27 September,Citation31 and Timor-Leste (30.7%; 53.90%) as of 14 September,Citation32 and several high-income countries such as Australia (44.3%; 65%) and the USA (56%; 65.1%) as of 30 September.Citation33 This suggests an unequal coverage of the COVID-19 vaccines among older adults in low-, middle-, and high-income countries.
Low vaccination coverage found among the older adults in the current study may be due to Bangladesh’s vaccination distribution plan’s limited emphasis on older people, which did not prioritize and include older people in the first stage of the first vaccination phase.Citation34 Furthermore, although the country has a favorable reputation for vaccine management globally,Citation22 it has limited capacity to transport, supply and distribute COVID-19 vaccines within a short time across different segments (e.g. older adults) of people across the country.Citation19 The country has limited ultra‐low temperature freezers and cold-chain facilities for storing mRNA vaccines in rural areas, thus potentially lowering vaccination coverage.Citation20,Citation35 Our study’s findings also identified two primary reasons for not receiving vaccines: problems in accessing vaccines and misconceptions about vaccines. Evidence indicates that maybe older people were hesitant or unsure about receiving vaccines.Citation21 Social stigma, marked by stereotypes and misconceptions, may also prevent older people from receiving adequate and accurate information about the benefits of receiving vaccines.Citation21,Citation36 Long queues and waiting periods at vaccination centers and jabs shortage also restricted them from getting vaccinated.Citation37 Our findings suggest that Bangladesh should strengthen its efforts to address vaccine misinformation and misconceptions, which contribute to vaccine hesitancy among older people and to distribute adequate COVID-19 vaccines urgently among them to increase vaccination coverage.
Our study revealed that older people with formal schooling were less likely to remain unvaccinated. We did not come across any study in Bangladesh and globally on this to compare our findings with. Evidence indicates that older people with formal education tend to be aware of the benefits of being vaccinated against COVID-19Citation24,Citation26 and the importance of herd immunity.Citation38 This awareness may shape their vaccination intentionCitation24 and prompt them to get vaccinated instead of remaining unvaccinated.Citation39 Furthermore, educated individuals have increased exposure to vaccination campaign programs and mass media (print and live news) and social media, which publish vaccine information, thus making them aware of COVID-19 vaccines.Citation24,Citation40 However, a study in the US found that individuals relying on social media for COVID-19 vaccine-related information were less likely to accept the COVID-19 vaccine.Citation26 Several studies established that educated participants were more knowledgeable of COVID-19 vaccines than uneducated ones, thus shaping their vaccine intention.Citation22,Citation35 Our findings suggest that it is crucial to undertake an aged-focused approach for promoting education campaigns for increasing the COVID-19 vaccine uptake among older adults in Bangladesh.
Our study’s findings also revealed that Bangladeshi older people with limited family income, those experiencing earning difficulty and living in rural areas were more likely to remain unvaccinated. This implies that policy promoting the COVID-19 vaccine campaigns targeting the rural and economically vulnerable people has not achieved promising results yet in Bangladesh, where most people live in rural areas and under poverty.Citation41 One probable reason for remaining unvaccinated is that older people may consider the COVID-19 vaccines as a bigger health risk than the coronavirus itself.Citation25 Fatalistic beliefs and rumors related to COVID-19 vaccines may also prevent them from receiving COVID-19 vaccines.Citation36,Citation42 Maybe people with limited income, earning difficulty and those living in rural areas have little vaccine awareness and knowledge.Citation20,Citation22 Furthermore, they have inadequate access to the internet facilities required for an app-based COVID-19 vaccine registration process.Citation20 COVID-19-related side effects (e.g. pain, fever, nausea, and fatigue)Citation20 and the perception that older people die after receiving vaccines may further restrict their intention to receive COVID-19 vaccines.Citation43 Moreover, they were not motivated to receive vaccines.Citation22 They may not be able to go to the vaccination centers since vaccination centers are not within walking distance. Our findings contrast with existing evidence, suggesting that rural respondents were more enthusiastic about COVID-19 vaccine uptake.Citation22 The results of our study indicate that it is vital to deploy a unique team for disseminating COVID-19 vaccine information among the poor, vulnerable, and rural older people and motivating them to get vaccinated against COVID-19.
Our study found that participants without preexisting non-communicable chronic conditions were more likely to be unvaccinated or receiving single dose of vaccine. This could be because older people without preexisting health conditions did not visit health-care workers since they have limited confidence in Bangladesh’s healthcare system.Citation21 Evidence suggests that individuals’ frequency of visiting hospitals, doctors, and pharmacies was positively associated vaccine uptake since health-care workers and pharmacists inform and encourage them to get vaccinated.Citation44 Also, older adults may believe that they did not have a compromised immune system, which prompted them to remain unvaccinated. Furthermore, as noted above, COVID-19-related side effects may discourage them from getting vaccinated.Citation20 This indicates that there is still a need for motivating older individuals who do not have preexisting chronic conditions.
Strengths and limitations
Our study has several strengths. First, this study is unique because, to the best of our knowledge, it is the first study that explicitly examined older adults’ COVID-19 vaccination coverage rate and its associated factors in Bangladesh and globally. Second, the study area and population were distinctive because Bangladesh has the lowest COVID-19 vaccination coverage rate in South Asia,Citation45 and older people were one of the most prioritized groups globally.Citation46 Despite these strengths, the current study’s findings can be considered in the context of several limitations. First, our research was cross-sectional in nature; so, causality cannot be established. Second, data on COVID-19 vaccination coverage and associated factors were self-reported, often subject to non-disclosure. Third, most participants were from rural areas, limiting the generalizability of the findings to the entire older population living in urban and rural areas in Bangladesh. Fourth, this study did not thoroughly examine why older people did not receive COVID-19 vaccines. This suggests that future research should be focused on providing insights into the reasons for low vaccination coverage among older people using a mixed-methods approach.
Conclusion and policy implications
The present study revealed that the COIVID-19 vaccination coverage was low among the older population in Bangladesh and a particular concern for older people with no formal education, who belonged to a low-income family and were suffering from non-communicable chronic conditions. These findings have significant policy implications and suggest that the relevant stakeholders, policymakers, and development partners should prioritize the older population undertaking targeted strategies to increase vaccination coverage among this vulnerable group of population. Evidence indicates that many Bangladeshi people had difficulties with COVID-19 vaccine registration, which are concerns for older people with limited health and digital literacy.Citation47 Therefore, the Government should take immediate action to ease their registration process. The use of volunteers can be of crucial importance in this regard. Previous researchCitation21 also documented a higher refusal rate of COVID-19 vaccination among the older population in Bangladesh, which is often mediated through their religious values, socio-demographic profile and perceived efficacy of vaccines and side effects.Citation48
Furthermore, there are high levels of misconceptions regarding COVID-19 among the older people in Bangladesh,Citation49 leading to higher vaccine hesitancy among them. Therefore, policymakers and public health practitioners must consider disseminating COVID-19 vaccination-related appropriate messages targeting the older population.Citation48,Citation50 Local leaders and Imams (religious leaders), who are respected and valued in the community, can play a pivotal role in sharing this information with the older population. In disseminating the COVID-19 vaccination-related information among the aged people, it could be practical to use audio-visual materials instead of leaflets or written documents because of older people’s limited literacy and education.Citation51 Additionally, community health workers, an integral part of the health systems in low- and middle- income countries, including Bangladesh,Citation52 can contribute to the widespread dissemination of COVID-19 vaccine-related information explicitly targeting the older people in Bangladesh.
Availability of data and material
The data is available on reasonable request from the corresponding author.
Acknowledgments
We acknowledge the role of Sadia Sumaia Chowdhury (Programme Manager, ARCED Foundation) and Md. Zahirul Islam (Project Associate, ARCED Foundation) for their support in data collection for this study.
Disclosure statement
The authors have no conflict of interest to disclose.
Additional information
Funding
References
- Schauer SG, Naylor JF, April MD, Carius BM, Hudson IL. Analysis of the effects of COVID-19 mask mandates on hospital resource consumption and mortality at the county level. South Med J. 2021;114(9):597. doi:10.14423/SMJ.0000000000001294.
- Anwar S, Nasrullah M, Hosen MJ. COVID-19 and Bangladesh: challenges and how to address them. Front Public Health. 2020;8:154. doi:10.3389/fpubh.2020.00154.
- Wells CR, Townsend JP, Pandey A, Moghadas SM, Krieger G, Singer B, McDonald RH, Fitzpatrick MC, Galvani AP. Optimal COVID-19 quarantine and testing strategies. Nat Commun. 2021;12(1):1–8. doi:10.1038/s41467-020-20742-8.
- Niu Y, Xu F. Deciphering the power of isolation in controlling COVID-19 outbreaks. Lancet Global Health. 2020;8(4):e452–e3. doi:10.1016/S2214-109X(20)30085-1.
- Guzzetta G, Riccardo F, Marziano V, Poletti P, Trentini F, Bella A, Andrianou X, Del Manso M, Fabiani M, Bellino S, et al. Impact of a nationwide lockdown on SARS-CoV-2 transmissibility, Italy. Emerg Infect Dis. 2021;27(1):267. doi:10.3201/eid2701.202114.
- Lancet T. India under COVID-19 lockdown. Lancet (London, England). 2020;395(10233):1315. doi:10.1016/S0140-6736(20)30938-7.
- Adekunle A, Meehan M, Rojas‐Alvarez D, Trauer J, McBryde E. Delaying the COVID‐19 epidemic in Australia: evaluating the effectiveness of international travel bans. Aust N Z J Public Health. 2020;44(4):257–59. doi:10.1111/1753-6405.13016.
- Chaudhary FA, Ahmad B, Ahmad P, Khalid MD, Butt DQ, Khan SQ. Concerns, perceived impact, and preparedness of oral healthcare workers in their working environment during COVID-19 pandemic. J Occup Health. 2020;62(1):e12168. doi:10.1002/1348-9585.12168.
- Issanov A, Akhmetzhanova Z, Riethmacher D, Aljofan M. Knowledge, attitude, and practice toward COVID-19 vaccination in Kazakhstan: a cross-sectional study. Hum Vaccin Immunother. 2021;1–7.
- Saladino V, Algeri D, Auriemma V. The psychological and social impact of Covid-19: new perspectives of well-being. Front Psychol. 2020;11:2550. doi:10.3389/fpsyg.2020.577684.
- Craven J. COVID-19 vaccine tracker. 2020.
- Bloomberg. Covid-19 Vaccine Tracker. 2021.
- Alhassan GN, Adedoyin FF, Bekun FV, Agabo TJ. Does life expectancy, death rate and public health expenditure matter in sustaining economic growth under COVID-19: empirical evidence from Nigeria? J Public Aff. 2021;21(4):e2302. doi:10.1002/pa.2302.
- Mills MC, Salisbury D. The challenges of distributing COVID-19 vaccinations. EClinicalMedicine. 2021;31.
- Persad G, Peek ME, Emanuel EJ. Fairly prioritizing groups for access to COVID-19 vaccines. Jama. 2020;324(16):1601–02. doi:10.1001/jama.2020.18513.
- Hossain E, Rana J, Islam S, Khan A, Chakrobortty S, Ema NS, Ema NS. COVID-19 vaccine-taking hesitancy among Bangladeshi people: knowledge, perceptions and attitude perspective. Hum Vaccin Immunother. 2021;1–10. doi:10.1080/21645515.2021.2010426.
- Hassan K. Covid-19: less than 10% fully vaccinated in Bangladesh. Dhaka: Dhaka Tribune; 2021.
- Coustasse A, Kimble C, Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J Ambul Care Manage. 2021;44:71–75. doi:10.1097/JAC.0000000000000360.
- Huda MN, Uddin H, Hasan MK, Malo JS, Duong MC, Rahman MA. Examining Bangladesh’s responses to COVID-19 in light of Vietnam: lessons learned. Global Biosecur. 2021;3.
- Molla MMA, Disha JA, Yeasmin M, Ghosh AK, Nafisa T. Decreasing transmission and initiation of countrywide vaccination: key challenges for future management of COVID‐19 pandemic in Bangladesh. Int J Health Plann Manage. 2021;36(4):1014–29. doi:10.1002/hpm.3156.
- Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, Hossain MA, Arefin A, Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16(4):e0250495. doi:10.1371/journal.pone.0250495.
- Paul A, Sikdar D, Mahanta J, Ghosh S, Jabed MA, Paul S, Yeasmin F, Sikdar S, Chowdhury B, Nath TK, et al. Peoples’ understanding, acceptance, and perceived challenges of vaccination against COVID-19: a cross-sectional study in Bangladesh. PloS One. 2021;16(8):e0256493. doi:10.1371/journal.pone.0256493.
- BBS. Elderly population in Bangladesh: current features and future perspectives. Dhaka: Banglaedsh Bureau of Statistics, Ministry of Bangladesh, Government of Bangladesh; 2015.
- Chaudhary FA, Ahmad B, Ahmad P, Khalid MD, Butt DQ, Khan SQ. Concerns, perceived impact, and preparedness of oral healthcare workers in their working environment during COVID-19 pandemic. J Occup Health. 2020;62(1):e12168. doi:10.1002/1348-9585.12168.
- Guillon M, Kergall P. Factors associated with COVID-19 vaccination intentions and attitudes in France. Public Health. 2021;198:200–07. doi:10.1016/j.puhe.2021.07.035.
- Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39(7):1080–86. doi:10.1016/j.vaccine.2021.01.010.
- World Health Organisation. Situation Update #77- Coronavirus Disease 2019 (COVID-19) WHO Country Office for Nepal; 2021.
- World Health Organisation. Coronavirus disease 2019 (COVID-19). Situation Report – 74; 2021.
- World Health Organisation. Viet Nam COVID-19 Situation Report #60; 2021.
- World Health Organisation. COVID −19 situation report- Sri Lanka; 2021.
- World Health Organisation. Cambodia coronavirus disease 2019 (COVID-19) Situation Report #65 W38; 2021.
- World Health Organisation. Coronavirus disease 2019 (COVID-19) Situation Report – 117 Timor-Leste; 2021.
- Our World in Data. Coronavirus (COVID-19) vaccinations; 2021.
- Dhaka Tribune. Bangladesh’s vaccination plan unveiled; 2021.
- Huda MN, Uddin H, Hasan MK, Malo JS, Duong MC, Rahman MA. Examining Bangladesh’s responses to COVID-19 in light of Vietnam: lessons learned. Global Biosecur J. 2021.
- Huda MN, Islam R, Qureshi MO, Pillai S, Hossain SZ. Rumour and social stigma as barriers to the prevention of coronavirus disease (COVID-19): what solutions to consider? Global Biosecur. 2020;1(4). doi:10.31646/gbio.78.
- Sakib SN. Bangladesh scraps ‘mass’ vaccination plan amid jabs shortage; 2021.
- Logan J, Nederhoff D, Koch B, Griffith B, Wolfson J, Awan FA, Basta NE. What have you HEARD about the HERD?’Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine. 2018;36(28):4118–25. doi:10.1016/j.vaccine.2018.05.037.
- Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):1–13. doi:10.1186/s12889-021-10816-7.
- Elgendy MO, Abdelrahim ME. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J Med Virol. 2021;93(12):6535–43. doi:10.1002/jmv.27199.
- Biswas RK, Rahman N, Islam H, Senserrick T, Bhowmik J. Exposure of mobile phones and mass media in maternal health services use in developing nations: evidence from urban health survey 2013 of Bangladesh. Contemp South Asia. 2021;29(3):460–73. doi:10.1080/09584935.2020.1770698.
- Williams LB, Fernander AF, Azam T, Gomez ML, Kang J, Moody CL, Bowman H, Schoenberg N. COVID‐19 and the impact on rural and black church Congregants: results of the C‐M‐C project. Res Nurs Health. 2021;44(5):767–75. doi:10.1002/nur.22167.
- Torjesen I. Covid-19: Norway investigates 23 deaths in frail elderly patients after vaccination. Br Med J Publ Group. 2021.
- Zhang D, Johnson K, Newransky C, Acosta CJ. Herpes zoster vaccine coverage in older adults in the US, 2007–2013. Am J Prev Med. 2017;52(1):e17–e23. doi:10.1016/j.amepre.2016.08.029.
- The Financial Express. Bangladesh’s Covid vaccination rate among lowest in South Asia, data reveals; 2021.
- Dhama K, Patel SK, Kumar R, Rana J, Yatoo MI, Kumar A, Tiwari, R, Dhama, J, Natesan, A, Singh, R, Harapan, H . Geriatric population during COVID-19 pandemic: problems, considerations, exigencies and beyond head title: geriatrics during COVID-19 pandemic. Frontiers in Public Health. 2020;8:562.
- Jahangir AR. Covid in Bangladesh: seniors far more likely to face the worst. Dhaka: United News of Bangladesh; 2021.
- Financial Express. Vaccination acceleration imperative for immunisingagainst Covid; 2021.
- Mistry SK, Armm A, Yadav UN, Irfan NM, Rayamajhee B, Stanners MN. COVID-19 related misconceptions among older adults in Bangladesh: findings from a cross-sectional study.F1000Research. 2021;10:216. doi:10.12688/f1000research.51597.1.
- Nutbeam D. The vital role of meaningful community engagement in responding to the COVID-19 pandemic. Public Health Res Pract; 2021;31.
- Speros CI. More than words: promoting health literacy in older adults. Ojin. 2009;14:5.
- Pallas SW, Minhas D, Pérez-Escamilla R, Taylor L, Curry L, Bradley EH. Community health workers in low-and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health. 2013;103:e74–e82. doi:10.2105/AJPH.2012.301102.