ABSTRACT
The aim of the United Nations’ Sustainable Development Goal (SDG)3 is to ensure healthy lives and promote well-being for all, at all ages; including reducing maternal and child mortality, combating communicable and non-communicable diseases, and achieving Universal Health Coverage (UHC). UHC aims to provide everyone with equal access to quality essential and comprehensive healthcare services including preventions, interventions, and treatments, without exposing them to financial hardship. Making progress toward UHC requires significant investment in technical and financial resources and countries are pursuing the implementation of cost-saving measures within health systems to help them achieve UHC. Whilst many countries are far from attaining UHC, all countries, particularly low- and middle-income countries, can take steps toward achieving UHC. This paper discusses key data showing how immunization is a fundamental, cost-effective tool for reducing morbidity and mortality associated with infectious disease in all populations, creating more productive communities, reducing treatment costs, and consequently, facilitating social and economic advancement. Immunization is key to advancing toward UHC by relieving the burden that diseases place on the healthcare services, freeing essential resources to use elsewhere within the healthcare system. Immunization is an essential, readily available strategy that countries can deploy to achieve UHC and the SDG3 agenda.
Introduction
In September 2015, the United Nations adopted 17 Sustainable Development Goals (SDGs) as a global call-to-action for continued progress in a range of social and economic development areas, with the aim of achieving a better and more sustainable future for all. SDG3 aims to ensure healthy lives and promote well-being across all ages, by achieving targets such as reducing the global maternal mortality ratio (to <70 per 100,000 live births), ending preventable deaths among children <5 years of age, ending epidemics (AIDS, tuberculosis, malaria, neglected tropical diseases), and combating other communicable (including hepatitis and water-borne diseases) and non-communicable diseases (NCD). These targets are achievable with Universal Health Coverage (UHC) (.Citation1-4
Figure 1. United Nations SDG3.Citation1

UHC means that all people and communities have equal access to essential and comprehensive healthcare services without causing financial hardship.Citation4 Equal access to healthcare addresses the most significant causes of diseases and death and ensures that the quality of those services is good enough to improve the health of the people who receive them.Citation4 UHC is considered an overarching goal for health targets across all SDGs, including SDG3. Central to UHC are three pillars: 1) Equal access to essential and comprehensive healthcare services aimed at extending the coverage of essential services, care, medicines and interventions to all that need them; 2) Quality of healthcare services to improve the health conditions of those receiving these services and allow access to new services, medicines, and interventions; 3) Financial risk protection to ensure that people accessing healthcare services are not put at risk of financial harm or pushed into poverty.Citation1–4
At least half of the global population does not have full coverage of essential healthcare services. To achieve UHC there is the need to strengthen healthcare systems.Citation4 Strategies are needed that promote sustainable funding of healthcare systems, equitable access to healthcare, and the training, education and retention of the healthcare workforce. Critical elements in achieving UHC include investment in primary healthcare to ensure that people receive comprehensive integrated health promotion, disease prevention, treatment, rehabilitation and palliative care. Investing in the healthcare workforce, ensuring good governance, developing systems to allow adequate procurement and supply of medicines and health technologies, and providing well-functioning health information systems will all contribute to UHC.
One of the challenges of UHC is the limited resources available to countries. High costs of care, inadequate/no insurance coverage, and lack of available services and culturally competent care are constraints which prevent countries from providing essential healthcare services to all that need them. Limited resources also restrict the development of new technologies, interventions and medicines. However, many countries at varying stages of economic development (e.g. Chile, Colombia, Cuba, Rwanda, Sri Lanka, Thailand), have shown that it is possible to make substantial progress toward UHC.Citation5 Implementing the UHC agenda requires technical and financial resources; therefore, cost-effective interventions help to ensure progress.Citation5 Here, we discuss the importance of immunization in directly preventing infectious diseases, and the indirect impacts that will facilitate the achievement of UHC and SDGs.
Reducing disease burden
The widespread use of vaccines has eradicated smallpox, almost completely eradicated polio, and substantially reduced the incidence and mortality associated with vaccine-preventable diseases (VPDs).Citation6 Although the goal to interrupt the transmission of wild polio in 2014 was missed, there has been substantial progress in eliminating it through vaccination, and by 2019 only two countries (Pakistan, Afghanistan) reported wild polio.Citation7 There are >30 vaccines against various VPDs with others in development;Citation6 these vaccines have not only significantly reduced the burden of disease in settings where they have been deployed but have reduced the global burden and mortality ().Citation9 Annually, an estimated 2–3 million deaths are prevented by vaccination programs.Citation8 Despite this progress, infectious diseases continue to cause a substantial burden worldwide. In 2017, >2 million deaths worldwide were due to VPDs ().Citation8 It is estimated that one in five children globally are not vaccinated with available vaccines and ~890,000 deaths in children <5 years of age are attributable to diseases preventable by vaccines currently recommended by the World Health Organization (WHO; excluding measles).Citation10,Citation11
Figure 2. Global deaths caused by some of the most common and serious VPDs in 2017.Citation8

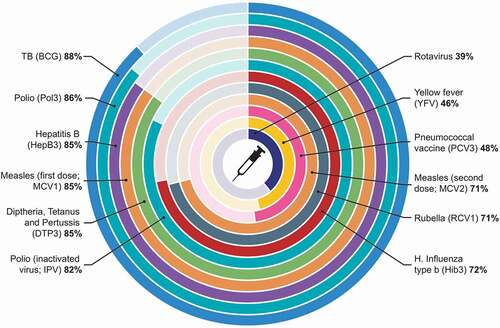
Figure 3. Global vaccination coverage: Percentage of children aged 1 year vaccinated against VPDs in 2019.Citation8
The persistence of VPDs originates from the inability to introduce the appropriate vaccines or to provide adequate vaccination coverage. Immunization campaigns can help reduce this persistence. For example, by the end of 2019 almost 350 million people across 24 of the 26 countries in the ‘African meningitis belt’ had been vaccinated with the MenAfriVac through the introduction of immunization campaigns.Citation12 If concerted efforts are made to properly implement immunization programs using the currently available vaccines, the challenges of low coverage and lack of access could be overcome, leading to a further reduction in the burden of VPDs as needed to achieve UHC.
Reducing maternal and infant mortality
Pregnant women and young infants have increased susceptibility to certain infectious diseases and/or are at high risk of experiencing severe disease if infected.Citation13,Citation14,Citation15 For young infants worldwide, it is estimated that infectious diseases cause >4 million babies to die before their first birthday each year, with 63% dying within their first month.Citation16 Accordingly, SDG3 health targets aim to reduce global maternal mortality and to end preventable deaths in children <5 years of age by 2030.Citation1
Infectious diseases remain a major cause of morbidity and mortality in early life, with infants typically experiencing worse symptoms compared with older children and adults. Additionally, most vaccines offer less protection to newborns than adults, and few are recommended for those <8 weeks of age.Citation14,Citation17 This period of susceptibility in early infancy may be mitigated by the presence of antibodies transferred from the mother during pregnancy. Immunization during pregnancy can boost maternal antibodies and provide protection to the pregnant woman and the fetus, which persists for a few months after birth. This provides some protection to the infant, until they reach the age where vaccinations can be administered. Maternal immunization has demonstrated protection against several early-life infections and the WHO and US Centers for Disease Control and Prevention recommend influenza, tetanus, diphtheria and acellular pertussis vaccines for all pregnant women; vaccines against hepatitis A and B, meningococcal and pneumococcal diseases are recommended for pregnant women at risk of infection.Citation15,Citation18
Although significant progress has been made over the past decade regarding the implementation of maternal immunization programs, several barriers remain to widespread acceptance, and vaccination rates in pregnant women remain suboptimal in many countries (even where national programs are in place).Citation18 Many countries have not introduced maternal vaccinations into their immunization programs; other countries have implemented only a few. Reasons may include a lack of awareness regarding the burden and the impact of these diseases in pregnancy and neonates, the associated risks of infection and the benefits of vaccination during pregnancy; the limited efficacy and safety data available for vaccines during pregnancy; and/or no global or local recommendations.Citation18 Strategies to facilitate uptake may include educating the community and healthcare providers (HCPs) about the benefits of maternal immunization, advocacy among governments to provide recommendations for appropriate vaccines during pregnancy, and effective communication around the risk of disease and the safety and efficacy of available vaccines. Improved maternal vaccination rates and reduced mortality associated with VPDs in mothers and newborns will help achieve UHC and SDG3 targets.
Improving quality of life in the aging population
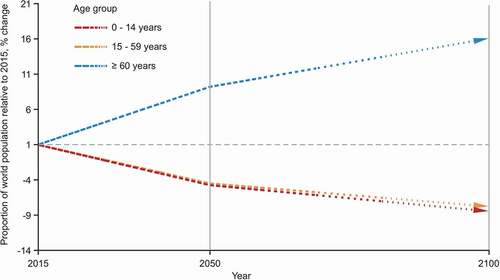
Life expectancy increased by 8.8 years between 1990 and 2021, which has resulted in a growing aging population.Citation19 By the end of this decade the number of people aged ≥60 years will increase by over 50%, to 1.4 billion, whereas the increase in younger age groups will be less dramatic ().Citation21 Although this is a good indicator of improved health, one of the resulting challenges is the increased susceptibility to VPDs, and other chronic illness and NCDs, among the older population. Increases in population aging results in a “double burden” of disease, requiring regions to adapt quickly to coping with a growing number of communicable diseases and NCDs simultaneously.Citation22 Immunosenescence, underlying medical conditions, and poor nutrition among elderly individuals can contribute to increased susceptibility to infectious diseases. Additionally, infectious diseases can trigger cardiovascular complications such as stroke, myocardial infarction and heart failures, conditions that are more prevalent in aging populations.Citation23 Changing demographic trends are beginning to be associated with changes in the epidemiology of VPDs;Citation24 the prevalence of many VPDs is now higher in adults than in children with 42,000 adults and 300 children dying from VPDs each year in the US.Citation25
Figure 4. Increase in the world population relative to 2015, by broad age group, 2015–2100.Citation20
There is a need to address the challenges of VPDs over the life course, especially in older adults, and to ensure that the increasing lifespans are matched with an increased number of years spent in good health (health span). Immunization can play a crucial role in improving adult health by allowing aging individuals to remain healthy and contribute to society and the economy for longer.Citation26 A prospective cohort study in Hong Kong on outpatients aged ≥65 years with chronic illness found that patients receiving pneumococcal and influenza vaccines had fewer deaths, cases of pneumonia and overall hospital admissions compared with unvaccinated patients. The Hong Kong government now provide pneumococcal and flu vaccinations free of charge for seniors.Citation27 Introduction of the herpes zoster vaccine in adults aged ≥50 years has significantly reduced the burden of illness, resulting in increased quality of life in older populations.Citation28 These data highlight the benefits that may be gained through vaccinations, beyond protection from specific VPDs. Vaccination programs aimed at aging populations will support an increasing health span and benefit economies globally.Citation26
Aging populations experience more frequent and severe infections compared with younger populations due to increased vulnerability, therefore prevention of infection is critically important.Citation23,Citation29 However, challenges exist regarding vaccinations in elderly populations: immunosenescence contributes to decreased immune responses following vaccination; they are not often the target for routine vaccination programs; they tend to be harder to reach populations; adult vaccination is a relatively new concept compared with childhood vaccinations, which means there is a lack of infrastructure as well as public awareness regarding the benefits of vaccination among adults and the elderly.Citation29 For example, the well-established Expanded Program of Immunization targets pediatric populations specifically, contributing to childhood vaccination programs being more successful even in countries where both adult and child vaccinations are recommended.Citation30 Increasing the awareness of the importance of adult vaccinations to HCPs and the community is an urgent unmet need. Governments should expand and establish policies and infrastructure necessary to enhance adult vaccinations.
Protecting the unprotected
Regardless of vaccination coverage, there will always be some individuals that continue to be unprotected for various reasons (e.g. primary vaccine failure, vaccine refusal, age or medical conditions contraindicating vaccination).Citation31,Citation32 Herd immunity is indirect protection from infectious diseases that occurs when a sufficient proportion of a population becomes immune to the infection through vaccination or previous infection. This prevents or reduces transmission of the disease and reduces the risk of exposure for individuals lacking immunity.Citation33
Given that herd immunity is only conferred when high vaccination coverage is achieved and sustained within the general population, efforts should be made to improve the coverage of available vaccines to stop the endemicity or recurrence of VPDs. The persistence of such infections not only makes it harder to reach the targets of SDG3, but carries the risk of outbreaks which diverts financial and medical resources that could be channeled into other areas to facilitate sustainable development and achievement of SDGs and UHC.
Disease outbreaks
The world is challenged by frequent outbreaks of infectious diseases, sometimes with devastating effects. Although some disease outbreaks occur where a vaccine does not exist, a significant proportion of outbreaks arise from diseases where vaccines are available (e.g. cholera, measles, pertussis). These outbreaks are often a result of low immunization coverage leading to a gradual buildup of susceptible individuals within the general population, until these reach the level needed to sustain an outbreak. Outbreaks can also be caused by humanitarian emergencies associated with the resettlement of large numbers of individuals in overcrowded temporary locations, often with poor sanitary conditions, inadequate supply of safe drinking water, and limited access to healthcare. Outbreaks often result in disability and socioeconomic disruptions, and unacceptably high morbidity and mortality rates. At the epicenter of the Ebola epidemic in West Africa in 2014, previous gains in economic growth were reversed with losses in gross domestic product of ~$219 million USD in Sierra Leone, $188 million USD in Liberia and $184 million USD in Guinea,Citation34 and 17.8 million International Dollars in the Democratic Republic of the Congo.Citation35 Furthermore, public health crises can result in the breakdown of health systems leading to epidemics of other VPDs. For example, the measles outbreak observed after the Ebola epidemic in West Africa highlights the importance of maintaining vaccination coverage even during public health emergencies.Citation36 Similarly, as of February 2021 the COVID-19 pandemic had not only affected >108 million people and caused >2 million deaths,Citation37 but it has also had an overwhelming impact on every aspect of the economy and health systems, both globally and at a country level. The total economic cost of the COVID-19 crisis in the US alone is estimated at >$16 trillion or 90% of the annual gross domestic product.Citation38 Similar levels of economic distress have been reported in other countries.Citation39 Additionally, the COVID-19 pandemic has had a considerable impact on global routine vaccination rates. In 2020, global estimated coverage for the diphtheria, tetanus and pertussis (DTP3) vaccine fell to 76.7%, whilst global coverage of the measles (MCV1) vaccine dropped to 78.9%; it is estimated that an additional 8.5 and 8.9 million children missed DTP3 and MCV1 doses, respectively, by the end of 2020 due to the COVID pandemic.Citation40 In high-burden settings, a recent study has suggested that deaths due to tuberculosis and malaria over the next 5 years could increase by up to 20% and 36%, respectively, as a result of the disruption to health services caused by the COVID-19 pandemic.Citation41 Strengthening and addressing the existing shortfalls of routine vaccination services during pandemics will be essential in repairing the damage caused by COVID-19. Planning how to safely deliver routine vaccinations during future pandemics will also be key in preventing any future disruptions to routine vaccination services.Citation42
Furthermore, there is still a great need for new vaccines that can prevent and reduce the impact of outbreaks of both endemic and emerging infectious diseases; a need that has been exemplified by the COVID-19 pandemic. The traditional phases of clinical trials require significant investment and resources, and the lengthy nature of these processes could be described as a bottleneck. Outbreaks are often sporadic, and as the process for bringing a vaccine from research to the clinic can take a long time with earlier technologies, vaccines may be unavailable when they are most needed.Citation43,Citation44 New technologies may provide faster access to vaccines in times of outbreaks where vaccines are not already established. The development of genetic screening allows entire bacterial and viral genomes to be analyzed; this has led to reverse vaccinology, where specific gene products of pathogens and potential vaccine candidates can be identified within days.Citation45 In addition, techniques using platforms to develop vaccines are increasingly being used (e.g. viral vectors, mRNA and self-amplifying mRNA, structural vaccinology); platform technology takes the same basic components of a vaccine to use as a backbone, yet is adaptable for use against different pathogens by inserting new genetic or protein sequences.Citation46 Recurring use of a platform not only allows rapid development of new vaccines but will increase confidence in the overall safety profile of vaccines. Such technologies have been used to develop the various influenza vaccines and have facilitated the rapid development of an unprecedented number of COVID-19 vaccines in a significantly condensed timeframe, thereby averting prolonged morbidity and mortality.Citation47
Cost savings
Immunization is a cost-effective public health intervention.Citation48 Vaccines are relatively cheap, and reduce deaths, disability and healthcare costs, simply by preventing diseases. Eradication of smallpox, which cost ~$100 million USD in total, generates estimated annual savings of $1.35 billion USD, in addition to saving millions of lives. Similarly, the polio eradication campaign, if it can be achieved, is estimated to generate savings of ~$1.5 billion USD each year.Citation49
Economic analyses of the costs (vaccines, supply chains, service delivery, human resource capacity strengthening, expanded immunization programs) and benefits (avoided cost of illness, morbidity and mortality) of vaccinations show that immunization is an excellent investment.Citation50 One study demonstrated that increased coverage of six key vaccines over 10 years across 72 low-income countries would save 6.4 million lives and result in an estimated saving of $6.2 billion USD in treatment costs and $1.2 billion USD in lost productivity among those providing care to loved ones.Citation51 Gains from increased productivity due to vaccination reached $145 billion USD (96% of the total cost of illness). India and Indonesia alone accounted for >60% of the treatment costs that could be saved from vaccination against pneumonia.Citation51 In a more recent analysis, the International Vaccine Access Center estimated that the return on investment for immunization against ten key pathogens in 73 Global Alliance for Vaccines and Immunization-eligible countries will be 20.6 according to a cost-of-illness approach or 53.7 according to a value-of-a-statistical-life approach, between 2021 to 2030.Citation50 The total economic benefits of increased vaccine coverage and introduction of new vaccines will exceed $781 billion USD from 2021 to 2030.Citation50 Furthermore, at a conference of health ministers in Africa, it was noted that between 2016 and 2020, Africa will require $17 billion USD for vaccines and vaccination services but are expected to derive benefits of $224 billion USD in direct returns and savings from vaccines and the management of VPDs.Citation52
These analyses show that vaccines are not only lifesaving, but they are a smart economic investment. For a few dollars per child, vaccines can prevent diseases and disabilities that last a lifetime, saving millions of dollars in potential healthcare spending. Families freed from the crippling costs of medical care for VPDs can instead spend more on food and education.
Conclusions
Attaining UHC is a goal for all countries, yet low health investment and prioritization of interventions are major challenges that need to be overcome. Immunization is a readily available, cost-effective intervention that should be prioritized. Investment in immunization programs promises significant reduction in morbidity and mortality from VPDs as required for UHC. In addition, immunization has high economic returns, constituting a cost-effective or even cost-saving approach, with dividends that countries can invest to further strengthen healthcare systems and other sectors. To embrace the benefits of vaccinations and immunization programs there is a need to implement strategies to circumvent the current challenges, such as legislating the use of appropriate vaccines, allocation of adequate domestic financial resources to national and local healthcare systems to enhance access to vaccines and improve vaccination coverage, and raising awareness on a large scale amongst the community and HCPs about the value of vaccines. Strong national immunization programs are required to increase and maintain vaccination coverage. Context-specific communication mediums (e.g. radio, television, mobile phones, social media, and administrative, traditional and religious leaders) can be leveraged to target particularly hard-to-reach areas and communities with sub-optimal vaccination coverage. Vaccines are a viable and readily available cost-effective resource that all countries can utilize to help them in attaining UHC and achieving SDGs.
Ethics statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Supplemental Material
Download PDF (1.8 MB)Acknowledgments
Authors thank MediTech Media for editorial assistance and manuscript coordination, on behalf of GSK Vaccines. Dr Michael Patan provided medical writing support and Dr Danielle Lindley coordinated manuscript development and editorial support. All authors contributed equally to the development of this review and approved the final version; no author received funding for the development of this manuscript. The authors would also like to thank Professor Joseph Okeibunor and Dr Anil Dutta for their contribution to the development of this manuscript.
Disclosure statement
JCdM and JMK declare no conflict of interest. IV, DC, MD, OC and MOCO are employed by, and have stock ownership in, the GSK Group of Companies.
Supplementry material
Supplemental data for this article can be accessed publisher’s website.
Additional information
Funding
References
- United Nations. Goal 3: ensure healthy lives and promote well-being for all at all ages; 2020.
- European Public Health Alliance. Universal Health Coverage, sustainable development and the pillar of social rights: implications and opportunities for the European Public Health Alliance; 2016.
- Universal Health Coverage 2030. Universal Health Coverage advocacy guide; 2018. https://www.uhc2030.org/fileadmin/uploads/uhc2030/Documents/Key_Issues/Advocacy/Advocacy_Guide_7_Jan_2019_gradient_r2.pdf .
- World Health Organization. Universal Health Coverage. https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- World Health Organization. The world health report 2010 – health systems financing: the path to universal coverage. Geneva: World Health Organization; 2010. https://apps.who.int/iris/bitstream/handle/10665/44371/9789241564021_eng.pdf?sequence=1&isAllowed=y .
- World Health Organization. State of the world’s vaccines and immunization. World Health Organization; 2009. http://apps.who.int/iris/bitstream/handle/10665/44169/9789241563864_eng.pdf?sequence=1 .
- World Health Organisation. Polio endgame strategy 2019–2023; 2019. https://apps.who.int/iris/bitstream/handle/10665/329948/WHO-Polio-19.04-eng.pdf?sequence=1&isAllowed=y .
- Vanderslott S, Dadonaite B, and Roser M. Our world in data; 2019. https://ourworldindata.org/vaccination# .
- Abubakar I, Tillmann T, Banerjee A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;385:117–8.
- Reid M, Fleck F. The immunization programme that saved millions of lives. Bull World Health Organ. 2014;92:314–15.
- World Health Organization. Global immunization data; 2010. https://www.who.int/immunization/newsroom/global_immunization_data_english_may2010.pdf .
- World Health Organization. Immunization coverage; 2020. https://web.archive.org/web/20210220050552/https://www.who.int/news-room/fact-sheets/detail/immunization-coverage
- Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370:2211–18. doi:10.1056/NEJMra1213566.
- Kollmann TR, Kampmann B, Mazmanian SK, Marchant A, Levy O. Protecting the newborn and young infant from infectious diseases: lessons from immune ontogeny. Immunity. 2017;46:350–63. doi:10.1016/j.immuni.2017.03.009.
- Centers for Disease Control and Prevention. Pregnancy and vaccination; 2019. https://www.cdc.gov/vaccines/pregnancy/pregnant-women/need-to-know.html .
- Engmann C, Fleming JA, Khan S, Innis BL, Smith JM, Hombach J, Sobanjo-ter Meulen A. Closer and closer? Maternal immunization: current promise, future horizons. J Perinatol. 2020;40:844–57. doi:10.1038/s41372-020-0668-3.
- Keener A. Tailoring vaccines for older people and the very young. Nature. 2019;575:S48–S50. doi:10.1038/d41586-019-03638-6.
- Vojtek I, Dieussaert I, Doherty TM, Franck V, Hanssens L, Miller J, Bekkat-Berkani R, Kandeil W, Prado-Cohrs D, Vyse A, et al. Maternal immunization: where are we now and how to move forward? Ann Med. 2018;50:193–208. doi:10.1080/07853890.2017.1421320.
- Macrotrends. World life expectancy 1950-2021; 2021. https://www.macrotrends.net/countries/WLD/world/life-expectancy .
- United Nations. World population prospects; 2015. https://population.un.org/wpp/publications/files/key_findings_wpp_2015.pdf .
- United Nations. World population ageing; 2015. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf .
- Tyagi P. Double burden of communicable and non-communicable disease in old age in South Asia; 2014. https://www.helpage.org/silo/files/double-burden-of-disease-report.pdf .
- Quinton LJ, Walkey AJ, Mizgerd JP. Integrative physiology of pneumonia. Physiol Rev. 2018;98:1417–64. doi:10.1152/physrev.00032.2017.
- Gonfiantini M, Carloni E, Gesualdo F, Pandolfi E, Rizzuto E, Iannazzo S, Iannazzo S, Ciofi Degli Atti ML, Villani A, Tozzi AE, et al. Epidemiology of pertussis in Italy: disease trends over the last century. Eurosurveillance. 2014;19:20921. doi:10.2807/1560-7917.ES2014.19.40.20921.
- Office of Disease Prevention and Health Promotion. Immunization and infectious diseases; 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases .
- Garau J, Hodin MW, and Kalache A. Global coalition on aging; 2013. https://globalcoalitiononaging.com/wp-content/uploads/2018/07/life-course-immunization_gcoa-for-web-1.pdf .
- Hung IF, Leung AY, Chu DW, Leung D, Cheung T, Chan C-K, Lam C, Liu S-H, Chu C-M, Ho P-L, et al. Prevention of acute myocardial infarction and stroke among elderly persons by dual pneumococcal and influenza vaccination: a prospective cohort study. Clin Infect Dis. 2010;51:1007–16. doi:10.1086/656587.
- Curran D, Oostvogels L, Heineman T, Matthews S, McElhaney J, McNeil S, Diez-Domingo J, Lal H, Andrews C, Athan E, et al. Quality of life impact of an adjuvanted recombinant zoster vaccine in adults aged 50 years and older. J Gerontol A Biol Sci Med Sci. 2019;74:1231–38. doi:10.1093/gerona/gly150.
- Weinberger B, Grubeck‐Loebenstein B. Vaccines for the elderly. Clin Microbiol Infect. 2012;18:100–08. doi:10.1111/j.1469-0691.2012.03944.x.
- Mantel C, Cherian T. New immunization strategies: adapting to global challenges. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2020;63:25–31. doi:10.1007/s00103-019-03066-x.
- Cesaro S, Giacchino M, Fioredda F, Barone A, Battisti L, Bezzio S, Frenos S, De Santis R, Livadiotti S, Marinello S, et al. Guidelines on vaccinations in paediatric haematology and oncology patients. BioMed Res Int. 2014;2014:707691. doi:10.1155/2014/707691.
- National Center for Immunization and Respiratory Diseases. General recommendations on immunization — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommendations Rep 2011;60:1–64.
- Kim TH, Johnstone J, Loeb M. Vaccine herd effect. Scand J Infect Dis. 2011;43:683–89. doi:10.3109/00365548.2011.582247.
- United Nations. Socio-economic impact of ebola virus disease in West African countries; 2015. https://www.undp.org/content/dam/rba/docs/Reports/ebola-west-africa.pdf .
- Kirigia JM, Muthuri RNDK, Muthuri NG. The monetary value of human lives lost through ebola virus disease in the Democratic Republic Of Congo in 2019. BMC Public Health. 2019;19:1218. doi:10.1186/s12889-019-7542-2.
- Suk JE, Paez Jimenez A, Kourouma M, Derrough T, Balde M, Honomou P, Kolie N, Mamadi O, Tamba K, Lamah K, et al. Post-Ebola measles outbreak in Lola, Guinea, January-June 2015(1). Emerg Infect Dis. 2016;22:1106–08. doi:10.3201/eid2206.151652.
- World Health Organization. Weekly epidemiological update - 16 February 2021; 2021.
- Cutler DM, and Summers LH. The COVID-19 pandemic and the $16 trillion virus. JAMA. 2020;324:1495–96. doi:10.1001/jama.2020.19759.
- Mandel A, Veetil V. The economic cost of COVID lockdowns: an out-of-equilibrium analysis. Econ Disaster Clim Chang. 2020;4:431–51. doi:10.1007/s41885-020-00066-z.
- Causey K, Fullman N, Sorensen RJ, Galles NC, Zheng P, Aravkin A, Danovaro-Holliday MC, Martinez-Piedra R, Sodha SV, and Velandia-González MP, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398:522–34. doi:10.1016/S0140-6736(21)01337-4.
- Hogan AB, Jewell BL, Sherrard-Smith E, Vesga JF, Watson OJ, Whittaker C, Hamlet A, Smith JA, Winskill P, and Verity R, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e1132–e41. doi:10.1016/S2214-109X(20)30288-6.
- Ota MO, Badur S, Romano-Mazzotti L, Friedland LR. Impact of COVID-19 pandemic on routine immunization. Ann Med. 2021;53:2286–97. doi:10.1080/07853890.2021.2009128.
- Plotkin S, Robinson JM, Cunningham G, Iqbal R, Larsen S. The complexity and cost of vaccinemanufacturing–an overview. Vaccine. 2017;35:4064–71. doi:10.1016/j.vaccine.2017.06.003.
- Pronker E, Weenen T, Commandeur H, Osterhaus A, Claassen H. The gold industry standard for risk and cost of drug and vaccine development revisited. Vaccine. 2011;29:5846–49. doi:10.1016/j.vaccine.2011.06.051.
- Nabel G. Diseñando las vacunas del mañana. N Engl J Med. 2013;368:551–60. doi:10.1056/NEJMra1204186.
- Vandeputte J, Saville M, Cavaleri M, Friede M, Hacker A, Mueller SO, Rizzi R, Smith D, Thirstrup S, Wagner R, et al. IABS/CEPI platform technology webinar: is it possible to reduce the vaccine development time? Biologicals. 2021;71:55–60. doi:10.1016/j.biologicals.2021.04.005.
- Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580:576. doi:10.1038/d41586-020-01221-y.
- Greenwood B. The contribution of vaccination to global health: past, present and future. Philoso Trans R Soc Lond B Biol Sci. 2014;369:20130433. doi:10.1098/rstb.2013.0433.
- Doherty M, Buchy P, Standaert B, Giaquinto C, Prado- Cohrs D. Vaccine impact: benefits for human health. Vaccine. 2016;34:6707–14. doi:10.1016/j.vaccine.2016.10.025.
- Sim SY, Watts E, Constenla D, Brenzel L, Patenaude BN. Return on investment from immunization against 10 pathogens in 94 low- and middle-income countries, 2011-30. Health Affairs (Project Hope). 2020;39:1343–53. doi:10.1377/hlthaff.2020.00103.
- Stack ML, Ozawa S, Bishai DM, Mirelman A, Tam Y, Niessen L, Walker DG, Levine OS. Estimated economic benefits during the ‘decade of vaccines’ include treatment savings, gains in labor productivity. Health Aff. 2011;30:1021–28. doi:10.1377/hlthaff.2011.0382.
- Mihigo RM, Okeibunor JC, O’Malley H, Masresha B, Mkanda P, Zawaira F. Investing in life saving vaccines to guarantee life of future generations in Africa. Vaccine. 2016;34:5827–32. doi:10.1016/j.vaccine.2016.06.036.
