ABSTRACT
Men involvement in HPV vaccine advocacy is important in a patriarchal society. This study aimed to investigate the influence of men on HPV vaccination of adult women. An online cross-sectional survey was undertaken between June and August 2019. Participants were fathers of children enrolled in schools in Fujian Province. A total of 1953 participants responded to our survey. Just over 60% reported they would definitely or likely support their spouse/partner to receive HPV vaccine. Physician recommendation (adjusted odds ratio [aOR] = 5.68, 95%CI = 3.89–6.86) and spouse/partner communication about HPV vaccination (aOR = 5.30, 95%CI = 3.72–7.55) were significant covariates associated with higher willingness to support women’s HPV vaccination. Perceiving HPV vaccination as only for women who have had multiple sex partners and HPV vaccination as a sensitive topic were significantly associated with lower willingness to support HPV vaccination. Over two-thirds (67.3%) reported joint HPV vaccination decision-making and 2.8% reported that it was entirely the man’s decision. The role of men in HPV vaccine acceptance and hesitancy among adult women is evident in China and warrants educational interventions to target men to enhance women’s HPV vaccination uptake.
Introduction
Cervical cancer is the third most common cancer in women worldwide, which accounts for considerable morbidity and mortality, and poses a great burden on the healthcare system.Citation1 In China, cervical cancer ranks as the sixth most common cancer among all women, the third most common cancer among women 15–44 years old, and 3.8% of women in the general population are estimated to have a high-risk HPV-16 and/or HPV-18 infection at any given point in time.Citation2 In 2018, China reported a total of 106,430 new cervical cancer cases and 47,739 deaths, corresponding to 18·7% of all diagnoses and 15·3% of all deaths from cervical cancer worldwide.Citation3,Citation4 HPV vaccination is the most effective method to prevent HPV infections, and, in conjunction with HPV screening, can potentially eliminate cervical cancer.Citation5 The World Health Organization (WHO) has recommended HPV vaccinations to young adolescent girls between the ages of 9 and 14.Citation6 HPV vaccination is also recommended for women through to the age of 26 years.
Although younger women are at greatest risk of the acquisition of HPV infection, HPV infections in mid-adult women are prevalent.Citation7,Citation8 Findings from a global review reported that genital HPV infection in women is predominantly acquired in adolescence, with the peak prevalence in most countries among women under 25 years of age.Citation9 Further, two-thirds of adult women aged 24 to 45 years are susceptible to HPV 6, 11, 16, and 18.Citation8 The inclusion of additional HPV types in the 9-valent HPV vaccine offers great potential to expand protection against more high-risk HPV types in adult women. To date, research continues to shows the benefit of HPV vaccination in adult women. Recent evidence suggests that adult women are also susceptible to acquiring new HPV infections and continue to face the risk of developing cervical cancer.Citation10,Citation11 Clinical data shows that HPV vaccination is efficacious, safe and immunogenic in women up to the age of 45 years.Citation12 In 2018 the licensure of the 9-valent vaccine was extended for both men and women through the age of 45 years based on shared clinical decision making.Citation13
Sensitivity toward sexually transmitted infections among adult women is exceptionally heightened in many Asian cultures. Hence, acceptability of vaccines against sexually transmitted diseases among adult women—especially married women—is challenging. Numerous studies have been published assessing the attitudes or intention to receive HPV vaccination among adult women up to the age of 45 years in Western countries.Citation14,Citation15 However, relatively little has been studied about the acceptability of HPV vaccination among adult women in China. A recent study found only 58.3% of women in China between the age of 27 and 45 reported that they intended to obtain the HPV vaccine, and the study also revealed that women’s spouses/partners have a profound influence on their HPV vaccination intention.Citation16 This has highlighted the importance of the influence of men in the HPV vaccine acceptance and hesitancy of women in China. There is growing recognition of the role men may play in women’s health-seeking behaviors.Citation17,Citation18 The influence of male partners in women’s reproductive health and reproductive healthcare seeking is evident in other countries.Citation19,Citation20 With regard to HPV vaccination, studies reported that in some cultures, women need approval from their husbands to vaccinate their daughters against HPV, and young women need approval from their fathers for HPV vaccination.Citation21–23 It is important to overcome spouse/partner barriers to the acceptance of HPV vaccination, particularly in societies in which males dominate, such as in China.
The authorities in China approved Cervarix in 2016, Gardasil in 2017 and subsequently Gardasil-9 in 2018. HPV vaccination rates in China remain critically low. A total of 11.0% of female students in a multicenter study of 136 universities in China reported having been vaccinated against HPV.Citation24 A recently publish local literature reported that between 2018 and 2020, a total of 21,597,400 doses of HPV vaccine were administered in women aged 9–45 years in Mainland China, with an estimated cumulative vaccination rate of 2.24%, with the highest in Beijing, Shanghai and Zhejiang (8.28%, 7.37%, and 4.68%), and the lowest in Tibet Autonomous Region, Qinghai Province and Xinjiang Uygur Autonomous Region (.06%, .39%, .46%).Citation25 In China, 9-valent HPV vaccine is recommended for adult women 20–45 years of age. To date, little is known about men’s opinions about HPV vaccination and their support of their spouse/partner receiving HPV vaccination. HPV vaccine hesitancy that stems from the spouse/partner being unsupportive of HPV vaccination is an important issue that needs to be addressed, as is the reverse; namely, spousal support increasing confidence in HPV vaccination. Therefore, this study aimed to investigate the willingness of men to support their spouse/partner to have the HPV vaccine and their influence on HPV vaccination decision-making. Factors influencing the willingness of men to support their spouse/partner to have the HPV vaccine were explored. The factors investigated were demographic characteristics, sexual behavior and history of sexually transmitted infections, HPV-related knowledge, Health Belief Model (HBM) constructs, and communication with spouses about HPV vaccination
Materials and methods
Study participants
Study participants were fathers of primary school children in the Yongding district of Longyan City, South-east of Fujian. A total of 78 primary schools in Fujian province agreed to assist in the data collection, with 27,756 students enrolled in these schools during the data collection period. Principals of schools were briefed about the study and school administrators were requested to assist in sending out an online survey link to all students’ fathers’ contact details in the school record. A universal sampling method was used to recruit all parents of students in the schools. The inclusion criteria included (1) participants being students’ fathers; (2) having a spouse/partner that has not been vaccinated against HPV; and (3) having a spouse/partner of eligible age of receiving the HPV vaccine. Of note, this study was part of a regional cohort study of parental perspectives on HPV vaccination. The finding of parental intention to vaccinate daughters against HPV infection has been published.Citation26 This paper reports the finding of male participants’ willingness to support their spouse/partner’s HPV vaccination uptake.
The sample size was calculated based on a response rate of 50%, confidence interval of 99%, margin error of 5%, and an estimated total of 27,756 parent population. The calculated sample size required for this study was 379. The sample size was multiplied by the predicted design effect of two to account for the use of convenience sampling and an online survey. Hence the minimum survey sample size was set to 758 (379 x 2) participants.
Prior to data analyses, data cleaning and validations were undertaken. Individuals who do not meet the inclusion criteria and straight-line responses were removed.
Instruments
The questionnaire consisted of four sections. The first section assessed demographic characteristics (age, place of birth, present locality of residence, marital status, participants’ highest educational level, spouse/partner’s highest educational level, occupational types, annual household income), sexual behavior and history of sexually transmitted infections.
The second section assessed participants’ HPV-related knowledge (15-items). The questions were adapted from previous studies related to the assessment of HPV-related knowledge in China.Citation14,Citation22 Response options were true, false and don’t know. A correct response was given a score of 1, and incorrect or don’t know responses were given a score of 0. The total possible knowledge score ranged from 0 to 15. A normality test was conducted and the knowledge score was found not normally distributed, hence, the scores were categorized as high or low based on the median split with a higher score range representing higher levels of knowledge. The internal reliability of the 15-item knowledge scale, which was evaluated with the Kuder-Richardson 20, was .94, indicating very good internal consistency.
The third section determined health beliefs toward HPV and HPV vaccination. The questions in this section were based on constructs from the HBM theoretical framework.Citation27 Questions included perceived susceptibility to HPV (3-items), perceived severity of HPV infection (1-item), perceived barriers in support of spouse/partner HPV vaccination (6-items), and cues to action (2-items). The response options were agree and disagree.
The questionnaire has one item that asked participants on communication with spouses about HPV vaccination. They were asked whether their spouse/partner ever talked about HPV vaccination with them. The response option was yes or no.
Subsequently, the participants were asked if they would willing to support their spouse/partner if the spouse/partner intends to receive HPV vaccine. The response options were: definitely; quite a high chance; moderate chance; chance was quite low; and definitely not.
The last question was about men’s influence on spouses/partners’ HPV vaccination decisions. Each participant was asked whether, if their spouse/partner wanted to take the HPV vaccine, would the decision depend entirely on the spouse/partner’s decision, depend entirely on the participant’s decision or be a joint decision.
Statistical analysis
Graphical figures were used to summarize the proportions of correct responses on HPV knowledge, willingness to support spouse/partner to take HPV vaccination and influence on spouses/partners’ HPV vaccination decision. Multivariable logistic regression analysis was performed to investigate factors associated with willingness to support spouse/partner HPV vaccination. The independent variables in the multivariable logistic regression were demographic characteristics, sexual behavior and history of sexually transmitted infections, HPV knowledge, HBM constructs, and communication about HPV vaccination. All variables found to have a statistically significant association (two-tailed, p-value <.05) with willingness to support spouse/partner to take HPV vaccination in the univariate analyses were entered into multivariable logistic regression analyses using a simultaneous forced-entry model (enter method). Adjusted odds ratio (aORs), 95% confidence intervals (95% CIs) and p-values were calculated for each independent variable. The model fit was assessed using the Hosmer–Lemeshow goodness-of-fit test.Citation28
All statistical analyses were performed with the Statistical Package for the Social Sciences, version 20.0 (SPSS, IBM Corp., Armonk, NY, USA).
Ethical approval
This study was approved by the Medical Ethics Committee at the Fujian Medical University, Fuzhou, China. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire. They were also informed that all responses were collected and analyzed without identifiers. Online consent was obtained from the participants. Online consent was obtained from the participants. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire. They were also informed that all responses were collected and analyzed without identifiers.
Results
Characteristics of participants, sexual behavior and history of sexually transmitted infections
A total of 1953 participants responded to our survey between June 2019 and January 2020. In the assumption that the survey link reached all the 27,756 student’s fathers, the response rate is 7.0%. A summary of the characteristics of the respondents is provided in the first column of . The majority of the respondents were 35–44 years of age (60.8%) and most either reported an annual household income of below CNY50,000 (44.3%) or between 50,000 and 120,000 (43.4%). Over half (56.6%) reported their highest educational attainment as secondary high school or below. The majority reported never (33.6%) or sometimes (39.0%) using a condom during sexual intercourse. Only 6.3% reported having had a history of sexually transmitted infection.
Table 1. Factors associated with willingness to support spouse/partner to take HPV vaccination (N = 1953)
Knowledge about HPV and HPV vaccination
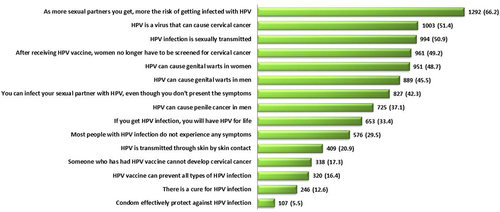
shows the proportion of correct responses on knowledge items in ascending order. The most common erroneous beliefs were that the use of a condom can effectively protect against HPV infection and that there is a cure for HPV infections. Many also wrongly believed that HPV vaccine can prevent all types of HPV infections. The mean and standard deviation (SD) for the total knowledge score was 5.3 (SD ±4.2), out of a possible score of 15. The median was 5 (interquartile range (IQR), 1.0–9.0). The knowledge scores of the study participants ranged from 0 to 14. Based on the median split, a total of 970 (49.7%) participants were categorized as having a high score (6–15) and 983 (50.3%) participants were categorized as having a low score (0–5).
Health beliefs regarding HPV and HPV vaccination
The first and second column of shows the responses to the HBM items. Slightly over half (53.9%) viewed that the chance of their spouse/partner getting an HPV infection was low. The majority disagreed that HPV vaccination is only important when a woman has had many sex partners (66.4%) and HPV infection is not important enough to get vaccinated against (76.5%). Regarding perceived barriers, over half (63.4%) regarded HPV vaccination as expensive. The majority disagreed that HPV infections are not serious (89.6%). Many were not clear about possible side-effects of HPV vaccination (74.8%) and disagreed that taking the HPV vaccine is a sign of having a history of multiple sex partners (75.1%). Under cue to action, the majority (77.8%) reported that they will persuade their spouse/partner to take HPV vaccine if there is a recommendation from doctor.
Communication bout HPV vaccination
Findings on communication about HPV with the spouse/partner revealed that only 20.5% reported that their spouse/partner ever mentioned HPV vaccination to them.
Influence on spouse/partner intention to receive the HPV vaccine
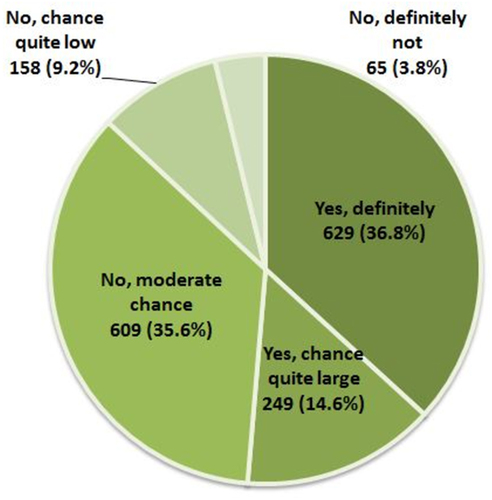
As shown in , half (50.7%) reported they would yes definitely support their spouse/partner to have the HPV vaccine and 10.5% reported yes, quite a high chance. shows the factors associated with willingness to support spouse/partner to take HPV vaccination. Participants who were unemployed were less willing to support their spouse/partner having the HPV vaccination than the self-employed (aOR .59, 95% CI .39–.89). Participants with a history of sexually transmitted infections (aOR 1.29, 95% CI 1.03–1.62) and having a higher HPV knowledge score (aOR 1.29, 95%CI 1.03–1.62) were more likely to show higher support. Those who expressed disagree that HPV infection is not important to get vaccinated against (aOR 1.73, 95% CI 1.29–2.32), HPV vaccination is only for women who have multiple sex partners (aOR 1.41, 95% CI 1.09–1.82) and HPV vaccination is a sensitive topic (aOR 1.53, 95%CI 1.21–1.94) were more likely to show support for their spouse/partner vaccination. Recommendation from physician (aOR 5.68, 95% CI 3.89–6.86) and communication regarding HPV vaccination (aOR 5.30, 95% CI 3.72–7.55) were the strongest covariates influencing higher support for the spouse/partner’s HPV vaccination.
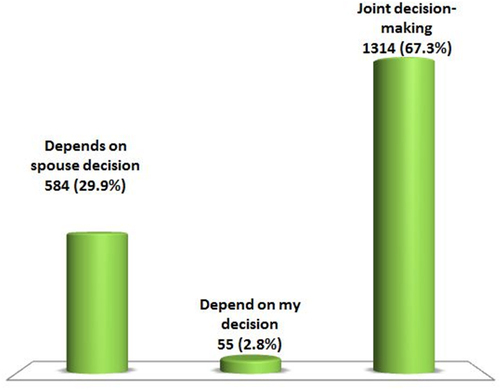
Over two-thirds reported joint HPV vaccination decision-making (67.3%) and only 2.8% reported that the spouse/partner HPV vaccination decision is entirely made on the participant’s decision ().
Discussion
A local study reported that men have a disproportionately low level of knowledge about HPV and its health association compared to women.Citation29 Similarly, in the present study, the median knowledge score of 5 out of a possible 15 implies a remarkably low level of knowledge about HPV and HPV vaccination among men, hence this warrants serious attention. The present study also identifies specific knowledge deficits that should be the target of awareness-raising education programmes for men in China. These include unawareness of the HPV types covered by different HPV vaccines. It is important to educate men that most HPV infections are typically transient and asymptomatic. As men play an important role in the transmission of HPV, it will be important to educate men that HPV infections are not curable. Also, men should be educated about the direct effects of HPV infection on male health, i.e., anal and oropharyngeal cancers and genital warts. This information will help to enhance men’s perceptions of the severity of HPV infections and their susceptibility to HPV diseases, thus potentially motivating protection measures, including encouraging female partners to get vaccinated.
In this study, most participants demonstrated a moderate perceived susceptibility of their spouse/partner contracting an HPV infection. It is important to impart the fact that HPV is the most common viral infection of the reproductive tract and that most sexually active women and men will be infected at some point in their lives and multiple HPV infections is also common.Citation30 In China, the prevalence of HPV infection remains at a high level. A systematic review of published literature from January 2000 to May 2017 reported that the national HPV prevalence in China was 15.5%.Citation31 Further, a pooled epidemiological studies published from January 2000 to June 2018 on high-risk HPVs in mainland Chinese women revealed that the overall infection rate of high-risk HPVs among these women was 19.0%.Citation32 Therefore educating the public about high susceptibility of getting an HPV infection is an important priority in healthcare promotion.
Although many men in the present study viewed HPV infection as having severe health consequences and believed that getting vaccinated against it as important, it is worrisome that one-third reported that HPV vaccination is only important when a person has had multiple sex partners. As sexual behavior is a significant risk factor for cervical cancer development in China,Citation33 destigmatizing the link between sexual behavior and HPV vaccination is imperative. Further, this study also uncovered important barriers to spouse/partner HPV vaccination, namely not having enough information about the HPV vaccine to be able to decide on spouse/partner vaccination, the high cost of the vaccine, the fear of unknown potential long-term side effects of HPV vaccination and sexual sensitivity surrounding HPV vaccination. All of these issues could serve to heighten hesitancy about, and decrease confidence in, HPV vaccine among women. Our findings suggest that the main construct of the HBM, namely the perception of the severity of and susceptibility to HPV infection, and perceived barriers will be essential components in health promotion interventions targeting men to promote their spouse/partner’s HPV vaccine uptake.
The finding that only 51.4% of respondents were supportive of their spouse/partner receiving HPV vaccination implies that more effort is needed to encourage men to support their spouse/partner in HPV vaccine uptake. The multivariable regression findings of this study provides some important insights into targeted intervention to enhance men’s support of their spouse/partner’s HPV vaccine uptake. Firstly, a higher socio-economic background, level of knowledge, and risk perception of HPV infection were significant factors influencing higher support in spouse/partner HPV vaccination. Our finding suggests that raising the level of knowledge and imparting the perception of susceptibility to HPV infection among men is warranted. As the current cost of HPV vaccines in China may be an issue for low-income households, subsidizing the cost of the vaccines could address the financial barrier. Secondly, the multivariable analyses also found that the perception that HPV vaccination is only necessary for people who have had multiple sex partners and that HPV vaccination is a sensitive topic significantly influences lower willingness in supporting women’s HPV vaccination. Therefore, destigmatizing the sensitivity of sexual issues surrounding HPV infection and vaccination is essential to enhance men’s support in spouse/partner HPV vaccination uptake. Recommendation from a physician and couples communication regarding HPV vaccination were found to be strong significant factors influencing support in vaccination. Therefore, physicians play an important role in communicating with men about the importance of HPV vaccination for their spouse/partner. Likewise, a previous study suggests that physician recommendation for HPV vaccination is important.Citation34 Furthermore, women are also encouraged to break communication barriers about HPV vaccination with their spouse/partner. It remains a challenge for women to communicate about vaccination against a sexually transmitted infection in a marital context. Women may find communication with their spouse about HPV vaccination difficult, believing that it would imply unacceptable sexual behavior, disloyalty to their husband/partner or even the condoning of extramarital sexual conduct. Therefore, educating married couples of the need for effective communication about HPV vaccination and cervical cancer prevention is crucial. Recently, China’s marriage registries have introduced premarital counseling to help couples prepare for marriage and to curb the rising divorce rate.Citation35 It would be useful to include the provision of counseling for HPV infection and vaccination in the premarital counseling services to enhance HPV vaccine uptakes.
Our findings suggest that men’s support for spouse/partner receipt of HPV vaccine is crucial. This is evident in the fact that over two-thirds of men in this study reported joint decision-making and nearly 3% reported that the decision regarding the HPV vaccination of their spouse/partner depends solely on the man’s decision. Married women in most Asian sociocultural contexts seek their husband’s permission regarding their own healthcare before making a decision. Most Asian women associate asking permission with being respectful toward their husbands. In many cases, women are not able to override their husband’s decision.Citation19,Citation20 Strong support and encouragement from their spouse/partner may reduce HPV vaccine hesitancy among women and increase confidence in vaccination. Therefore the development of targeted approaches, both in the workplace and community-based, to encourage men and make them more willing to support their spouse/partner’s vaccination would be useful. A programme promoting HPV vaccination in China should target men as past research has shown that involving men in women’s health is strongly associated with enhanced and better health outcomes in women.Citation36
This study has some limitations. First, our study participants were fathers of students recruited from a list of available contacts in the school registries. In addition, the study has a low response rate. Therefore, the study participants are not representative of all men in the study population and the entire men population in mainland China. The second limitation is that the study was conducted only in the Fujian province, thus the study population may not be representative of the general population of adult men in China as a whole or in other provinces. Third, the responses were based on self-reporting of data and may be subjected to self-reporting bias and a tendency to report socially desirable responses, therefore, the results should be interpreted with caution. Despite these limitations, the sample was large and sociodemographically diverse and the findings provide a useful initial indication of how interventions with men around HPV vaccination need to be structured.
Conclusion
It is crucial to enhance men’s willingness to support their spouse/partner to get vaccinated against HPV infection. Men were also found to play a prominent role in women’s HPV vaccination decision-making. In essence, our data highlight the need to involve men in combating HPV vaccine hesitancy in women, an issue that is particularly relevant in male-dominated societies. This information can inform the development or modification of HPV immunization intervention programmes in a manner that is tailored to include both men and women to boost confidence and overcome HPV vaccination hesitancy. This study has provided insights on the importance of including men in the promotion of HPV vaccination in women in China.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
Authors’ contribution
Li Ping Wong, Yulan Lin, Zhijian Hu and GD Zimet contributed to the study conception and design. Data collection was performed by Yulan Lin, and Zhijian Hu. Data analysis was performed by Li Ping Wong and Haridah Alias. The first draft of the manuscript was written by Li Ping Wong and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics approval
This study was approved by the Medical Ethics Committee at the Fujian Medical University, Fuzhou, China. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire. They were also informed that all responses were collected and analyzed without identifiers.
Disclosure statement
Outside of the present work GZ has served as a consultant and advisory committee member for Merck regarding HPV vaccination and as an advisory committee member for Moderna regarding COVID-19 vaccination. He has also received investigator-initiated research funding from Merck, administered through Indiana University. The other authors declare that they have no conflict of interest.
Additional information
Funding
References
- World Health Organization (WHO). Cervic Uteri; 2021 Jan [accessed 2021 Dec 5]. https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf
- ICO/IARC HPV Information Centre. 2021 Oct 22 [accessed 2021 Dec 5]. https://hpvcentre.net/statistics/reports/CHN_FS.pdf
- Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. ICO/IARC information centre on HPV and cancer (HPV Information Centre). Human papillomavirus and related diseases in China. Summary Report 2019 June 17. [accessed 2021 Dec 5].
- de Martel C, Georges D, Bray F, Ferlay J, Clifford GM. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Global Health. 2020;8(2):e180–10. doi:10.1016/S2214-109X(19)30488-7.
- National Cancer Institute. Human Papillomavirus (HPV) vaccines; 2021 May 25 [accessed 2021 Dec 5]. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
- World Health Organization. Draft: global strategy towards the elimination of cervical cancer as a public health problem; 2020 Apr 5 [accessed 2021 Dec 5]. https://www.who.int/publications/m/item/draft-global-strategy-towards-eliminating-cervical-cancer-as-a-public-health-problem
- Ferris DG, Brown DR, Giuliano AR, Myers E, Joura EA, Garland SM, Kjaer SK, Perez G, Saah A, Luxembourg A, et al. Prevalence, incidence, and natural history of HPV infection in adult women ages 24 to 45 participating in a vaccine trial. Papillomavirus Res. 2020;10:100202. doi:10.1016/j.pvr.2020.100202.
- Muñoz N, Manalastas R Jr, Pitisuttithum P, Tresukosol D, Monsonego J, Ault K, Clavel C, Luna J, Myers E, Hood S, et al. Safety, immunogenicity, and efficacy of quadrivalent human papillomavirus (types 6, 11, 16, 18) recombinant vaccine in women aged 24–45 years: a randomised, double-blind trial. Lancet. 2009;373(9679):1949–57. doi:10.1016/S0140-6736(09)60691-7.
- Smith JS, Melendy A, Rana RK, Pimenta JM. Age-Specific prevalence of infection with human papillomavirus in females: a global review. J Adolesc Health. 2008;43(4): S5-e1. doi:10.1016/j.jadohealth.2008.07.009.
- Winer RL, Hughes JP, Feng Q, Xi LF, Lee SK, O’-Reilly SF, … & Koutsky LA, Koutsky LA. Prevalence and risk factors for oncogenic HPV infections in high-risk mid-adult women. Sex Transm Dis. 2012;39(11):848–56. doi:10.1097/OLQ.0b013e3182641f1c.
- Kombe Kombe AJ, Li B, Zahid A, Mengist HM, Bounda GA, Zhou Y, Jin T. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Public Health. 2021:1003. doi:10.3389/fpubh.2020.552028.
- Skinner SR, Szarewski A, Romanowski B, Garland SM, Lazcano-Ponce E, Salmerón J, et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 4-year interim follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet. 2014;384(9961):2213–27. doi:10.1016/S0140-6736(14)60920-X.
- U.S. Food and Drug Administration. FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old; 2018 Oct 5 [accessed 2021 Dec 5]. https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old
- Black LL, Zimet GD, Short MB, Sturm L, Rosenthal SL. Literature review of human papillomavirus vaccine acceptability among women over 26 years. Vaccine. 2009;27(11):1668–73. doi:10.1016/j.vaccine.2009.01.035.
- Weiss TW, Rosenthal SL, Zimet GD. Attitudes toward HPV vaccination among women aged 27 to 45. Int Sch Res Notices. 2011;2011:670318. doi:10.5402/2011/670318.
- Lin Y, Lin Z, He F, Chen H, Lin X, Zimet GD, Alias H, He S, Hu Z, Wong LP, et al. HPV vaccination intent and willingness to pay for 2-,4-, and 9-valent HPV vaccines: A study of adult women aged 27–45 years in China. Vaccine. 2020;38(14):3021–30. doi:10.1016/j.vaccine.2020.02.042.
- Ganle JK, Otupiri E, Parker M, Fitzpatrick R. Socio-Cultural barriers to accessibility and utilization of maternal and newborn healthcare services in Ghana after user-fee abolition. J Matern Child Health. 2015:1–14. doi:10.12966/ijmch.02.01.2015.
- Chekole MK, Kahsay ZH, Medhanyie AA, Gebreslassie MA, Bezabh AM. Husbands’ involvement in family planning use and its associated factors in pastoralist communities of Afar, Ethiopia. Reprod Health. 2019;16(1):1–7. doi:10.1186/s12978-019-0697-6.
- Dudgeon MR, Inhorn MC. Men’s influences on women’s reproductive health: medical anthropological perspectives. Soc Sci Med. 2004;59(7):1379–95. doi:10.1016/j.socscimed.2003.11.035.
- Namasivayam A, Osuorah DC, Syed R, Antai D. The role of gender inequities in women’s access to reproductive health care: a population-level study of Namibia, Kenya, Nepal, and India. Int J Women’s Health. 2012;4:351. doi:10.2147/IJWH.S32569.
- Wong LP. Role of men in promoting the uptake of HPV vaccinations: focus groups’ finding from a developing country. Int J Public Health. 2010;55(1):35–42. doi:10.1007/s00038-009-0072-4.
- De Groot AS, Tounkara K, Rochas M, Beseme S, Yekta S, Diallo FS, Tracy JK, Teguete I, Koita OA. Knowledge, attitudes, practices and willingness to vaccinate in preparation for the introduction of HPV vaccines in Bamako, Mali. PloS One. 2017;12(2):e0171631. doi:10.1371/journal.pone.0171631.
- Sathian B, Babu MR, Van Teijlingen ER, Banerjee I, Roy B, Subramanya SH, Rajesh E, Devkota S. Ethnic variations in perception of human papillomavirus and its vaccination among young women in Nepal. Nepal J Epidemiol. 2017;7(1):647. doi:10.3126/nje.v7i1.17757.
- You D, Han L, Li L, Hu JD, Zimet G, Alias H, Danaee M, Cai L, Zeng F, Wong LP, et al. Human papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: a multicenter study. Vaccines. 2020;8(1):31. doi:10.3390/vaccines8010031.
- Song Y, Liu X, Yin Z, Yu W, Cao L, Cao L, Ye J, Li L, Wu J. Human papillomavirus vaccine coverage among the 9-45-year-old female population of China in 2018-2020. Chin J Vaccines Immunization. 2021;27:570–75.
- Lin Y, Su Z, Chen F, Zhao Q, Zimet GD, Alias H, & He S, Hu Z, Wong LP. Chinese mothers’ intention to vaccinate daughters against human papillomavirus (HPV), and their vaccine preferences: a study in Fujian Province. Hum Vaccines Immunother. 2021;17(1):304–15. doi:10.1080/21645515.2020.1756152.
- Champion VL, Skinner CS. The health belief model. Health Behav Health Edu. 2008;4:45–65.
- Hosmer DW Jr., Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. Hoboken (NJ): John Wiley & Sons; 2013.
- Chen G, Wu B, Dai X, Zhang M, Liu Y, Huang H, … & Wu Z, Wu Z. Gender differences in knowledge and attitude towards HPV and HPV vaccine among college students in Wenzhou, China. Vaccines. 2022;10(1):10. doi:10.3390/vaccines10010010.
- World Health Organization. Human papillomavirus (HPV) and cervical cancer; 2020 Nov 11 [accessed 2021 Dec 5]. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer#:~:text=What%20is%20HPV%3F-,Human%20papillomavirus%20(HPV)%20is%20the%20most%20common%20viral%20infection%20of,shortly%20after%20becoming%20sexually%20active
- Ma X, Wang Q, Ong JJ, Fairley CK, Su S, Peng P, Jing J, Wang L, Soe NN, Cheng F, et al. Prevalence of human papillomavirus by geographical regions, sexual orientation and HIV status in China: a systematic review and meta-analysis. Sex Transm Infect. 2018;94(6):434–42. doi:10.1136/sextrans-2017-053412.
- Li K, Li Q, Song L, Wang D, Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019;125(7):1030–37. doi:10.1002/cncr.32003.
- Li X, Hu SY, He Y, Hernandez Donoso L, Qu KQ, Van Kriekinge G, et al. Systematic literature review of risk factors for cervical cancer in the Chinese population. Women’s Health. 2018;14:1745506518816599. doi:10.1177/1745506518816599.
- Hswen Y, Gilkey MB, Rimer BK, Brewer NT. Improving physician recommendations for HPV vaccination: the role of professional organizations. Sex Transm Dis. 2017;44(1):42. doi:10.1097/OLQ.0000000000000543.
- XinhuaNet. China to introduce premarital counseling at marriage registries; 2020 Sep 10. [accessed 2022 Jan 30]. http://www.xinhuanet.com/english/2020-09/10/c_139356503.htm
- Oguntunde O, Nyenwa J, Yusuf FM, Dauda DS, Salihu A, Sinai I. The experience of men who participated in interventions to improve demand for and utilization of maternal and child health services in northern Nigeria: a qualitative comparative study. Reprod Health. 2019;16(1):1–9. doi:10.1186/s12978-019-0761-2.