?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Although more than one hundred million beneficiaries were administered COVID-19 vaccine until 20th February, 2022 in Bangladesh; however, proportionally a low turnout has been recorded in rural places and a substantial gap exist among the people living in rural and urban areas concerning the ratio of receiving vaccine. This study aims to investigate COVID-19 vaccine acceptance intention and to identify the potential factors influencing vaccine acceptance and hesitancy among the rural community in Bangladesh. A bilingual, self-administered anonymous questionnaire was developed, and data were collected between 10th June 2021 and 14th August 2021 through face-to-face interview. 655 rural people participated in this cross-sectional study, and sampling was done randomly. Descriptive statistics and binary logistic regressions were used to explore and rationalize study objectives. Out of 655 rural participants, 552 (84.3%, 95% CI 81.2─86.8) responded to accept COVID-19 vaccine; however, minor fractions (n = 5, n% = 0.8, 95% CI 0.12–1.4) of rural community had willingness to pay (WTP) for a COVID-19 vaccine. The result of binary regression showed that “safety,” “side effects,” “effectiveness,” and “trust” had highly significant (p <.01) and positive correlation with vaccine acceptance intention. “Rumor” had moderately significant (p <.05) and negative association while “gender” had insignificant correlation with vaccine acceptance intention. Easy and constant access to evidence-based and trustworthy information on vaccination consequences is imperative for resource-less remote people. Health communication regarding safety, side effect, and effectiveness of vaccines were identified as the most important predictor to convert vaccines to vaccinations and for ensuring mass immunization against COVID-19 in Bangladesh.
Introduction
The corona virus disease 2019 (COVID-19) affected community people from all walks of life and imposed a heavy disease burden around the world. The treatment protocol is facing challenges because still there is lacking of precise antiviral therapy for COVID-19.Citation1 Since vaccination is the most effective and fundamental therapeutic tool to eradicate contagious pandemic virus,Citation2 like many other countries in the world, Bangladesh has moved forward with its vaccination policies and mass inoculation programs. The government of Bangladesh has launched the biggest-ever mass vaccination program to vaccinate 80% (over 130 million) of the country’s total population with the vaccines in four different phases.Citation3 To achieve country-wide massive vaccination programs, the regulatory authority Directorate General of Drug Administration (DGDA) has given approval of seven vaccine candidates to use for Bangladeshi people, and Moderna COVID-19 vaccine was the latest candidate included in this platform for emergency use in the country.Citation4 Initially, the government published a priority list and decided to provide vaccines to different frontline workers and people at the age of over 55 years in the first phase. Due to the lower population enrollment in vaccination program, the policymakers decided to drop down the age limit to 40 years and since then, the percentage of people taking vaccination has increased in the country quite sharply. In continuation of its performance in grappling with the worst pandemic situation of the century, the government has shown its credibility in demonstrating the essences of vaccination to protect citizens from further infections and associated complications from the corona virus.
Meanwhile, it has been learned from numerous media outlets that percentage of people receiving vaccines is high in cities and a substantial gap still exists among the people living in rural, semi-urban, and urban areas concerning the ration of receiving vaccines. Bangladesh is a highly dense populated countryCitation5 and in fact most of the peoples living in rural areas and many on the street of cities do not have adequate access to information about COVID-19 vaccinations. On the other hand, ensuring of extensive and nation-wide vaccination coverage could remarkably reduce the severity of symptoms and infection rate through controlling the syndrome,Citation6 thereby contributing in higher standards of public health, lowering morbidity and mortality rates in community.Citation7 Taken all together, Bangladesh government set to launch a massive COVID-19 vaccination drive through in-spot registration among the rural community in unions and wards for the people of 30 years of age and above under the mass immunization programs. The government planned to cover 10 million people in a week mainly focused on the community who are living at union and wards levels. Consequently, walk-in vaccination at centers in unions and wards started from 7 August, 2021 to ensure the pooled coverage of the remote people as a pilot project.Citation8,Citation9 To accomplish successful implementation of a mass vaccination drive in the union and ward levels, it is important to examine the prospective challenges in the process because response to a vaccine can be understood as a continuum ranging from outright refusal to active demand for immediate acceptance.Citation10 In this aspect, several studies indicated that vaccine hesitancy; low acceptance intention and refusal decision would be the biggest challenges in Low and Middle Income Countries (LMICs)Citation11and even also in developed countries.Citation12
Reportedly, hesitancy or refusal of a vaccine refers to the unwillingness to uptake it, when the service is available to deliver a particular vaccine.Citation13 It is worth mentioning that hesitation in getting a vaccine lead to a massive outbreak of disease previously,Citation14 since vaccine always remains a dilemma among a large group of people.Citation15 Vaccine hesitancy has been identified as one of the top ten threats for global healthCitation16 and vaccine hesitancy is considered as a social phenomenon and it appears as a therapeutic crisis among the hesitant people worldwide. Acceptance rate of a particular vaccine varied among the different countries and vaccine hesitancy intensely relays on the psychological behavior of acceptors, individual’s and social characteristics and vaccine-related factors.Citation17
Arce JS et al. 2021Citation18 conducted a cross-sectional study on 45,928 peoples in LMICs of Asia, Africa, and South American countries showed that COVID-19 vaccine hesitancy was 20% and 40%, respectively. The author also indicated that side effects and effectiveness were the potential factors for a people considered to be vaccinated.Citation18 In India, among 358 participants in first phase of vaccination 30% was hesitant while 8%, 29%, and 44% peoples were concerned on safety, adequate information, and side effect issues, respectively.Citation19 Similarly, a global survey shown that among the 6639 respondents, 22.5% were hesitant on vaccine of which 50.37% mentioned about side effect, as a major determinant of their vaccination decisions.Citation20 Whilst to date, several factors have been identified which are potentially associated with COVID-19 vaccine acceptance and hesitancy reported in both of Asian countries and global perspectives included safety and efficacy,Citation21–23 vaccine effectiveness,Citation24 fear and anxiety,Citation21 information sufficiency,Citation25 anti-vaccine beliefsCitation26,Citation27and communication.Citation28 Hossain et al., 2021Citation29 conducted a cross-sectional study on Bangladeshi adult peoples, he found that 41.1% was COVID-19 vaccine hesitant. The author reported that vaccine efficacy, side effects, and perceived anti-vaccination beliefs were the major considerations in the COVID-19 vaccine acceptance intention.Citation29
Bangladesh, likewise other countries around the world, is undertaking to fight against COVID-19 pandemic. For ensuring country-wide COVID-19 vaccination, the government of Bangladesh made an agreementCitation30 with a leading pharmaceuticals of the country, Beximco Pharmaceutical Limited requesting to purchase COVID-19 vaccine from the Serum Institute of India, the world’s largest vaccine manufacturer licensed from AstraZeneca to manufacture “COVISHIELD” vaccine for supplying to low- to middle-income countries (LMICs).Citation31 However, besides Serum Institute Bangladesh government completed additional purchase agreement with some other vaccine manufacturers across the world target to vaccinate at least 80% of the total population.
Mass vaccinations including rural people against COVID-19 have emerged as a key preventive strategy because the second wave of pandemic has triggered a massive humanitarian crisis with unprecedented numbers of hospitalization and deaths in Bangladesh. As the mass inoculation program in ward and union level in Bangladesh was making its way on 7 August, tensions raised among rural people regarding the vaccine. Along with vaccine deployment and distribution policies, adequate research attention should be paid to understand the complex interplay of a variety of individual’s psychological and social aspects and the vaccine itself influences acceptance and hesitancy to ensure crude coverage with COVID-19 vaccines.Citation32 To the best of knowledge till date, there was no exploratory studyCitation33,Citation34 had been investigated on key influential factors of COVID-19 vaccine acceptances intention and hesitancy among the rural community in Bangladesh. Since the COVID-19 vaccine roll out in union and ward level was inaugurated through implementing a pilot project on 7 August, 2021 in Bangladesh, it became very relevant to assess the vaccine acceptance intention and to identify the actual antecedents influencing COVID-19 mass vaccination among the rural community. Therefore, the objectives of the current study were to investigate COVID-19 vaccine acceptance intention and to identify the major factors influencing the COVID-19 vaccine acceptance and hesitancy among the rural community in Bangladesh.
Methods
Study and questionnaire design
A validated and anonymous semi-structured multi-items questionnaire was adopted by reviewing evidence from recent studies on COVID-19 vaccination published in LMICs and global perspectives.Citation18–29 The questionnaire was originally developed in English language and then translated by the expert to native language (Bengali) because translating into native language was considered as a key task in capturing the respondent’s perception in a survey-based study. The items in the preliminary questionnaire were validated by a panel of public health experts from reputed universities in Bangladesh to ensure the relevance and clarity of the questionnaires. The first part of questionnaire contains the demographic information where the participants were asked about age, gender, occupation, educational level, religion etc, while the later part of the questionnaire comprised of predictor construct of COVID-19 vaccine acceptance.
Respondents
We carried out this cross-sectional study by applying self-administered anonymous questionnaire to those who were capable to understand the questionnaires and fill it out. Face-to-face interview approach was conducted for illiterate and semi-literate respondents. At first, we selected several upazila of Southeast part in Bangladesh for the data collection purpose and the data were collected randomly from selected wards and unions of Southeast areas of the country. The areas were selected based on the convenience of data collection. According to the latest census of 2020, out of a population over 160 million in Bangladesh, approximately 66.88% were residing in rural places, of them, at least 46.72% was women and girls. Although the adult literacy rate in rural areas stood at 65.4%; however, 58% of urban and 40% of rural males above 60 years of age are literate, while the rate is only 24% among urban and 12% among rural females over 60.
The eligibility criteria for the participants were: (i) to sign a consent form agreeing to the study objectives and provide anonymous data on COVID-19 vaccine and vaccination, (ii) residence of union or ward level of those selected areas and (iii) age of 18 years and above.
Sample and data collection
Due to the prevalence of COVID-19 pandemic, we ensured compliance with community health measures such as wearing face mask and maintaining social distancing strictly. The study conducted among the cohort of rural community people and data were collected from 10 June 2021 to 14 August, 2021 when massive vaccination among rural community was yet to be started. Random sampling technique was used for 655 respondents by interviewing face-to-face approach. Since the binary logistic regression is used, it is evident that, for observational studies with large sample size, taking a minimum sample size of 500 is necessary to derive the binary logistic regression statistics that represent the parameters. The other recommended rules of thumb are event per variable (EPV) of 50 and the formula; n = 100 + 50i, where i indicates number of independent variables incorporated to in the final model.Citation35 To avoid the potential source of non-response bias, the questionnaire was distributed among rural people of the country and encourages them to participate in this study. There was no missing data in final data set used for descriptive statistics and logistic regression analysis.
Study tools and survey instruments
The questionnaire included sections on socio-demographic characteristics; willingness to accept a COVID-19 vaccine, probable factors associated with vaccine uptake intention, important attributes of rural people toward a COVID-19 vaccine and participant’s willingness to pay for a vaccine. The revised questionnaire was subsequently pre-tested on 20 participants from rural community; who, later were excluded from the final analysis. Binary logistic regression tools were used to analyze the correlations and, significance level between predictor variables and outcome variable was examined at 95% CI.
Study variables
The study had two objectives. The first objective was to assess the COVID-19 vaccine acceptance intention among the rural people and the second objective was to identify the key factors influencing their vaccine acceptance intention and hesitancy. To address the first objective, the response variable of study we measured as willingness to uptake a new vaccine and the responses were measured as a binary variable (1=Yes, 0=No). The socio-demographic characteristic and other categorical variables such as age, profession, monthly income, educational level, gender, marital status, religion, existence of co-morbidity and COVID-19 experiences of the respondents was also captured. For the second objective, we examined the impact of some psychological, social, and vaccine-related factors on the outcome of variable dichotomized into 1=Yes and 0=No. Additionally, important attributes of rural people toward a COVID-19 vaccine and vaccination were also measured by 1=Yes and 0=No. Willingness to pay (WTP) for a vaccine was measured using one item statement (I am willing to pay for a COVID-19 vaccine) and the responses were measured by 1=Yes and 0=No.
Equations for regression model
The general form of logistic regression is as follows:
where y is the linear combination function while defined as EquationEquation (1)(1)
(1) and its value varies from - ∞ to +∞, x1, x2 … … .xm are explanatory variables and the parameters b1, b2 … … bm are slope coefficient of the logistic regression model. The dependent variable (z) is denoted as a binary response variable, (0 or 1). If z is value 1 (z = 1) means the presence of vaccine uptake intention, and value 0 (z = 0) indicates the reservation of vaccination. The computational algorithms are as follows:
Here, P is referred as the probability of vaccine uptake intention, x=vector of explanatory variables and B represents the regression coefficient to be estimated. Function of y is represented as logit (p), i,e., the log (to base e) of the odds or likelihood ratio that the dependent variable z is 1.
Usually EquationEquations (2)(2)
(2) and (Equation3
(3)
(3) ) are written as logit (P) or the log odd ratio as follows:
B reflects the degree of influence of predictor variables on the vaccine uptake intention.
Data analysis
Descriptive statistics expressed as weighted frequencies and percentages was performed on the categorical and socio-demographic characteristics of the respondents. We had no missing data in the extracted data set that we performed analysis for descriptive statistics and logistic regression. A non-parametric data analysis tool (binary logistic regression) was applied to find out the key predictive factors of COVID-19 vaccine acceptance and hesitancy. Model summary was evaluated by Nagelkerke R2 value and goodness-of-fit for binary model was assessed by using Omnibus Tests of Model Coefficients and Hosmer and Lemeshow tests.Citation36 Microsoft excel (version 10) was used for accounting the sample from technical data sheet and imported the data set to the SPSS accordingly. The entire analysis was conducted by using the IBM SPSS statistical package (version 25). The minimum significance level (p value) was set at the value of 0.05.
Results
Respondents’ characteristics
displays the socio-demographic characteristics of the study populations. A total of 655 eligible respondents participated in this study. We examined for eligibility and confirmed the eligible participants by using the previously set standard. 369 (56.3%) male and 286 (43.7%) female participated in the study. The minimum age was 18 years and maximum was 75 years while mean age was 35.13 years. As a result, majority of the participants 233 (35.5%) were youth age ranges of 30–39 years. The minimum monthly income of the participants was 500 Bangladeshi Taka (BDT) and the maximum was 35,000 BDT. Although the mean income was calculated as 5802 BDT; however, the highest 418 (63.8%) participants had monthly income level of 0–5000 BDT. According to the latest data published from the Bangladesh Bureau of Statistics (BBS), out of population over 160 million in Bangladesh about 24% of population in Bangladesh is still illiterate and this study captured 13.6% of total respondents were illiterate. The highest count 162 (33.9%) of the rural community had elementary or primary education. In professional diversification, the majority 155 (23.7%) was reported as house keeper. Among the total participants, 537 (82.0%) was Muslim by religion and 523 (79.8%) was married. 578 (88.2%) respondents had no severe illness or co-morbidity and 82 (12.5%) reported COVID-19 infected previously. Most importantly, 552 (84.3%, 95% CI 81.2─86.8) of rural people responded to accept a COVID-19 vaccine any time.
Table 1. Respondents demography.
Descriptive statistics findings
The descriptive statistic of independent variables and the outcome variable is shown in .
Table 2. Descriptive statistics of variables.
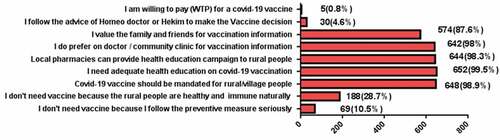
presents the result of some important attributes toward COVID-19 vaccine and vaccination among rural people. Interestingly, the WTP for a COVID-19 vaccine is scored very low (n= 5, n% = 0.8, 95% CI 0.12–1.4) among the rural community in Bangladesh.
Model summary
discusses the model summary; in order to identify the key predictors associated with vaccine uptake intention, a binary logistic regression model was applied. The most common assessment of overall model fit in the logistic regression is the likelihood ratio test. The joint impact of independent variables on the dependent variable was determined by using Nagelkerke R Square test that explained the model summary.
Table 3. Model summary.
The result of Cox and Snell R2 indicates that outcome variable was explained as 46%─80% by the independent variables in the predictive model which is assumed to be very good level.
Goodness of model fit
In , the s p- value of Omnibus Tests of Model Coefficients is significant, less than 0.05 which indicates a very good model fit.
Table 4. Omnibus tests of model coefficients.
According to the analysis of “”, the p- value is .440 which is insignificant in Hosmer and Lemeshow Test indicates a good model fit. Hence, our fitted logistic model is a good fit for testing of both assumptions.
Table 5. Hosmer and Lemeshow test.
Binary logistic regression model
displays the result of correlation analysis of explanatory variables with the dependent variables in the binary regression analysis model. According to the result of regression analysis, the predictor variables “safety”, “side effects”, “effectiveness”, and “trust” had highly significant (p <.01) and positive correlation with vaccine acceptance intention among the rural community. The result also revealed that “rumor” has moderately significant (p <.05) and negative association with outcome variable while categorical variable “gender” had no significant correlation with the vaccine uptake intention.
Table 6. Logistic regression analysis.
and represent the value of chi-square test and odds ratio for categorical variable “gender”. According to the , male group was 1.2 times more responsive in receiving vaccine which was found insignificant at Pearson chi-Square test result in . Hence, statistically no group was identified as a vaccine hesitant risky group in implementing mass vaccination.
Table 7. Chi-square tests result.
Table 8. Risk group estimation.
Discussion
The government of Bangladesh formally launched the COVID-19 vaccination programs since 7 February 2021 by administering Oxford/AstraZeneca vaccine and attempted to extend the immunization coverage country-wide. The average number of persons that have already been vaccinated is substantially different between urban and rural areas. As a result, to reinforce the country-wide mass vaccination programs, this cross-sectional survey aimed to examine the willingness to uptake the COVID-19 vaccine among the rural community and to investigate the factors that predict their willingness to be vaccinated with an approved vaccine in Bangladesh. According to the findings of our study, approximately 85% of the rural peoples had the COVID-19 vaccine uptake intention anytime while the remaining had the reservation. A cross-sectional online survey conducted across 9 LMICs included Bangladesh showed the prevalence of COVID-19 vaccine acceptance varied from 76.4% to 88.8%.Citation11 A similar study carried out among 10 LMICs showed that, more than 80% people in Asia, Africa, and South African regions had the willingness to accept a COVID-19 vaccine.Citation37 These findings are consistent with our study result.
Several factors modify vaccination decisions and determine whether an individual will refuse, delay, or accept a vaccine. Personal decision-making regarding vaccination is complex and influenced by psychological, emotional, societal, cultural, spiritual, and vaccine-related factors.Citation38 The binary regression model of this study demonstrated that “safety”, “side effect”, “effectiveness”, and “trust” has highly significant and positive correlation with the vaccine uptake intention among the rural people in Bangladesh. Perceived vaccine safety is highly determined by the magnitude of side effects and safety margin. Acceptance of a newly launched vaccine depends upon the level of individual’s trust regarding the vaccine safety, effectiveness, and adverse effect prevalence.Citation39,Citation40 Safety issue regarding the COVID-19 vaccination was primary concern among 45% in Indian population,Citation24 39.1% in Saudi Arabia,Citation41 47.8% in China,Citation42 46%Citation43 in Qatar and 25.5% in BangladeshCitation23 reported from Asian countries while 60.4% found in Africa and Middle East.Citation44 In the same line, side effect was primary consideration to receive a COVID-19 vaccine identified 44.1% in India,Citation19 79.45% in China,Citation45 26.3% in JordanCitation46 and 31.4% in TurkeyCitation47of Asian continents while 40% in LMICs of Asia, Africa, and South American countries.Citation18 Vaccine effectiveness was one of the key determinants that emphasized effectiveness of COVID-19 vaccine that might increase public intention to get vaccinated. Consequently, vaccine effectiveness has been recognized as an important factor to accept a COVID-19 vaccine among 53.8% people in India,Citation24 49.9% in Saudi Arabia,Citation41 16% in Qatar,Citation43 and 14.7% in JordanCitation46 reported from in Asia while 14.1% in United StatesCitation48 and 15.1% in LMICs.Citation11 Trust in vaccine discovery, public health experts and domestic health systems as well as government actions are important drivers of vaccine acceptance globally. Arguably, trust is an intrinsic and potentially modifiable component of successful uptake of a COVID-19 vaccine. Our findings shown that trust in health actors was strongly associated with vaccine uptake intention and can contribute to public compliance in vaccination process. Therefore, trust has already been identified as one of the most critical antecedents for making a vaccination decision among 18.1% people in JordanCitation46 and 31.4% in TurkeyCitation47 in Asian region, 65% in Portugal,Citation39 33.5% in SloveniaCitation49 and 20.2% in GermanyCitation50 while 28.5% reported in multi-ethnic areas.Citation51 For developing a sustainable vaccine confidence to public, rebuilding and restoring the public trust would act as a clarified response to accept a COVID-19 vaccine.Citation52,Citation53 All these recent scientific evidences are supportive to our study findings.
Anti-vaccination rumors and propaganda potentially lead to mistrust contributing in vaccine hesitancy that could be reduced by providing adequate scientific information to remote people. Our study result demonstrated that rumor had moderately significant and negative association with COVID-19 vaccine uptake intention. Fake news and misinformation is important predictor that influenced the acceptance intention of COVID-19 vaccine in South AsiaCitation54 and in Bangladeshi adult populations reported recently.Citation23,Citation29 Since rumors negatively impacted COVID-19 vaccine uptake intention; therefore, our findings suggested that reducing the associated rumors and propaganda would increase the mass vaccination coverage to rural community.
In this study, religious beliefs and conspiracy beliefs had insignificant effect on receiving COVID-19 vaccination by the rural community in Bangladesh. Although Hossain et al., 2021Citation29 collected data in first week of February, 2021 and evident that the Muslim dwellers in city corporation areas were more hesitant toward vaccination however, we collected the data from rural areas at the period when country-wide mass vaccination has rolled-out and community people were connected with vaccine awareness programs. Public were conscious about COVID-19 vaccine origin data which largely contributed them to avoid rumors and anti-vaccine beliefs including religious and conspiracy beliefs.
Since a significant portion (28.7%) of them believed that they do not need the vaccine because rural people are healthy and acquire herd immune naturally, so the authority should declare mandate the vaccine for rural people, otherwise large portions of population may avoid vaccination uptake due to their self-beliefs regarding acquired immunity in rural people naturally. Therefore, in , almost all respondents (98.9%) opined that COVID-19 vaccine should be mandated for rural population.
Although the government offered COVID-19 vaccine with free of cost to their citizens in Bangladesh, however, the study result shows that only 0.5% of the rural people had WTP for a COVID-19 vaccine. The current study did not fix the price ranges and values for a single dose of vaccine rather the study aimed to assess their future willingness to pay for a vaccine. The WTP for a newly promoted vaccine was found very low among rural community in Bangladesh. Actually the monthly income of the rural community was insufficient and the inside decision to pay for a vaccine is typically correlated with household income. The acceptance and hesitancy toward a new vaccine depends on cost-related concernsCitation32 and significantly associated with different household income.Citation55 We collected data from large sample size to ensure external validity or representativeness of the study findings. More clearly, 655 respondents living in rural areas were participated in this study. The variation in the respondents demography and sample size provide much strength to anticipate the generalizability of the study results in addressing the population and deliver health messaging to increase public interest on COVID-19 vaccination.
In Bangladesh, COVID-19 vaccination roll-out in union and word level was inaugurated through implementing a pilot project on 7 August 2021. Hence, in advance, it became very relevant to assess the vaccine uptake intention and exploring the key factors of COVID-19 vaccine acceptance intention among rural community. This is the first study that used a new analytical approach to identify potential factors that influences COVID-19 vaccine acceptance and hesitancy in rural places of Bangladesh. The application of new model in explaining the key factors of COVID-19 vaccination would add new value in the body of existing knowledge in the field. Few studies conducted on COVID-19 vaccine hesitancy in Bangladeshi adults and general people reported 40–55%Citation29,Citation56,Citation57 vaccine hesitancy rate and one study mentioned hesitancy rate approximately 25%.Citation23 As we discussed earlier, Bangladesh formally launched COVID-19 vaccination programs on the 7 of February, 2021 and these studiesCitation23,Citation29,Citation56,Citation57 were performed at the period when COVID-19 vaccination started in urban areas and nation-wide mass vaccination was not to be started yet. Therefore, relatively high vaccine hesitancy rate was observed among the respondents of those studies conducted in Bangladesh. On the other hand, current study was performed at June to August, 2021 when mass COVID-19 vaccination in union and ward level has been started successfully alongside urban areas. Afterward, mass people received vaccination information through educational campaigns and media communication, thereby generated adequate vaccine confidence throughout the country. Consequently, relatively low vaccine hesitancy rate (15.7%) among rural people was reported in this study.
The study had some limitations; the foremost of which was the sample size of the participants in comparison with number of rural population in Bangladesh. The study thus did not involve the largest numbers sample size to ascertain the generalizability of the current findings. As a result, non-response bias is a possibility as those who did not respond might have been more intention or hesitancy regarding the COVID-19 vaccination than the study respondents. This non-response would undermine the true prevalence of COVID-19 vaccine acceptance and hesitancy among rural community resulted in larger differences between those who were willing to receive a vaccine and those who were not. Secondly, this study assessed uptake intention of a COVID-19 vaccine and identified the associated influential factors of receiving a vaccine; this may differ from behavioral context. Still, with frequent changes in the perceived risk of disease, new approval and deployment of existing vaccines and the development of new COVID-19 vaccine themselves, individual’s behavioral context may be changed. Therefore, it is difficult to predict in-spot vaccine acceptance and hesitancy level, and there are some other relevant factors that could influence the COVID-19 vaccine acceptance intention to the rural people were truly unidentified in this study.
Even few months ago, the rural community of Bangladesh had to passionately wait to hear when they would get COVID-19 vaccine that would enable them to move freely as most of the country men had to stay at home to protect them from COVID-19 contamination for a long time. Since a substantial gap existed among the people living in rural and urban areas to be registered for receiving vaccines, so the rural community should be well communicated with vaccination information.
The authors would like to recommend that the government’s foremost step should have to be initiated for robust campaign in favor of vaccination. Of course, the government is carrying out different campaigns, but the intensity needs to be increased to encounter the fake news already conceptualized in rural places of Bangladesh. Government could consider using the potential of Union Digital Center (UDC), which is working at the Union Parishad (UP). They could also consider issuing a directive through the local government division to all the UDCs of the UPs to provide effective communication services to the rural people at a minimal price. This would facilitate the process of mass involvement in vaccination services. The government could also leverage UP’s potential to undertake comprehensive health educational campaigns to motivate people to receive COVID-19 vaccine. According to our study, it has been found that some people suffering from long-term co-morbidities such as hypertension, diabetes, chronic kidney disease, cancer, and asthmatic problem may have reservations in receiving vaccine. These people are confused about whether the vaccine will have any adverse side-effects, safe, and effective enough. To address the perception, the local government division should disseminate evidence-based scientific information to motivate these groups of people to be included under mass vaccination programs. In this aspect, further examination of key factors influencing COVID-19 vaccine hesitancy is urgent for getting more people under the vaccination program and to accomplish the ultimate goal of making a COVID-19 free Bangladesh.
Conclusions
Implementation of mass vaccination has already been shown to be a great success in reducing COVID-19 disease and its associated mortality and morbidity; however, achieving high acceptance and uptake rates is a fundamental aspect of successful COVID-19 vaccination effort. This study investigated the underlying factors of vaccine acceptance intention among rural community in Bangladesh because mass vaccinations against COVID-19 have been started in already. According to our study result, safety, side effect, and effectiveness of the vaccine and trust in the process significantly and positively correlated with the vaccine uptake while rumor impacted negatively. Hence, crude vaccination coverage throughout the country is empowered by ensuring sustainable public trust on vaccination and disseminating safety, side effect, and effectiveness data of a newly promoted vaccine toward rural community. The government, healthcare stakeholder, and vaccine policymaker should consider the practical strategies to minimize the existing vaccination gap between the urban and rural people. Evidence-based communication, mass media strategies, and effective policy on providing health educational campaigns in rural places could reduce anti-vaccination rumors thus improving COVID-19 vaccine acceptance among the marginalized people in Bangladesh. This paper highlighted a tentative roadmap and practical recommendation to properly achieve the mass vaccination drive by subduing its potential public health challenges in remote areas. With this study, we hoped to establish practical guidelines for ensuring mass public immunization programs and reinforce the vaccination among rural people in Bangladesh.
Author contributions
DNR conceptualized and designed the study and performed data acquisition statistical analysis, data interpretation, the original draft writing, and revised the manuscript. MNH performed data collection, assisted data curation, conducted preliminary analysis, and revised manuscript. MSA assisted with study design and execution, performed data interpretation, manuscript edition, revision and supervision. All authors have approved the final article version submitted.
Consent to participate
All participants provided objectives of the study and informed consent prior to study participations.
Ethical approval
The study did not require ethical approval as no clinical experimental procedure was conducted, and data were anonymously collected from participants who previously signed an informed consent.
Acknowledgements
All authors greatly acknowlede Professor Dr. Mohitosh Biswas, Department of Pharmacy, University of Rajshahi, Bangladesh for the helpful comments and suggestions provided for the manuscript.
Data availability statement
All data used for analysis in this manuscript are available from corresponding author or first author upon request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–9. doi:10.1016/S0140-6736(20)30183-5.
- Centers for Disease Control and Prevention (CDC). Ten Great public health achievements–united States, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60(19):619–23.
- United Nations Bangladesh. COVID-19 quarterly report: supporting the government response to the pandemic. 2020.
- Dhaka Tribune. Bangladesh-approves-emergency-use-of-moderna-covid-19-vaccine; 2021 Jun 06 https://www.dhakatribune.com/bangladesh/2021/06/29/bangladesh-approves-emergency-use-of-moderna-covid-19-vaccine?fbclid
- UN World Population prospects revision- United Nations population estimates and projections; 2019. https://worldpopulationreview.com/countries/Bangladesh-population?fbclid=IwAR2hWQtjV2cX21sIJW1arFMbaZ24sSN0qbnQ0ADx8ZvIFhYRV8mTmt5pCH8
- Eskola J, Liang X. WHO | SAGE working group dealing with vaccine hesitancy (March 2012 to November, 2014). [accessed 2021 Mar 5]. https://www.who.int/immunization/sage/sage_wg_vaccine_hesitancy_apr12/en/
- Andre F, Booy R, Bock H, Clemens J, Datta S, John T, Lee BW, Lolekha S, Peltola H, Ruff TA, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Org. 2008;86:140–46. doi:10.2471/blt.07.
- Dhaka Tribune. Bangladesh-set-to-launch-massive-covid-19-vaccination-drive. 2021 Aug 2. https://www.dhakatribune.com/bangladesh/2021/08/02/bangladesh-set-to-launch-massive-covid-19-vaccination-drive
- Foreign Brief Bangladesh government to launch mass vaccination campaign at union level. 2021 Aug 7. http://www.foreignbrief.com/daily-news/bangladesh-government-to-launch-mass-vaccination-campaign-at-union-level/
- Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–59. doi:10.1016/j.vaccine.2014.01.081.
- Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, Hasan MT, Colebunders R. Factors affecting COVID-19 vaccine acceptance: an international survey among Low-and Middle-Income Countries. Vaccines. 2021;9(5):515. doi:10.3390/vaccines9050515.
- Coustasse A, Kimble C, Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J Ambul Care Manage. 2021;44(1):71–75. doi:10.1097/JAC.0000000000000360.
- Lazer D, Ognyanova K, Green J, Matthew A, Druckman J, Gitomer A, et al. The COVID states project: a 50-State COVID-19 survey report #47: update on COVID-19 vaccine attitudes among healthcare workers. 2021.
- Larson H, de Figueiredo A, Karafillakis E, Rawal M. State of vaccine confidence in the EU 2018. Vol. 10. Luxembourg: Publications Office of the European Union; 2018. p. 241099. [accessed 2021 Feb 21].
- Kata A. Anti-Vaccine activists, Web 2.0, and the postmodern paradigm– an overview of tactics and tropes used online by the antivaccination movement. Vaccine. 2012;30(25):3778–89. doi:10.1016/j.vaccine.2011.11.112.
- World Health Organization. Vaccination: European commission and World Health Organization join forces to promote the benefits of vaccines, 2019. [accessed 2020 Jul]. https://www.who.int/news/item/12-09-2019-vaccination-european-commissionand-world-health-organization-join-forces-to-promote-the-benefits-of-vaccines
- Habersaat KB, Jackson C. Understanding vaccine acceptance and demand—and ways to increase them. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2020;63(1):32–39. doi:10.1007/s00103-019-03063-0.
- Arce JSS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Mobarak AM. COVID-19 vaccine acceptance and hesitancy in low and middle income countries, and implications for messaging. medRxiv. 2021.
- Suresh A, Konwarh R, Singh AP, Tiwari AK. Public awareness and acceptance of COVID-19 vaccine: an online cross-sectional survey, conducted in the first phase of vaccination drive in India. 2021.
- Riad A, Abdulqader H, Morgado M, Domnori S, Koščík M, Mendes JJ, … Kateeb E, Kateeb E. Global prevalence and drivers of dental students’ COVID-19 vaccine hesitancy. Vaccines. 2021;9(6):566. doi:10.3390/vaccines9060566.
- Chou WYS, Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–22. doi:10.1080/10410236.2020.1838096.
- Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12):e0008961. doi:10.1371/journal.pntd.0008961.
- Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, Hossain MA, Arefin A, Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16(4):e0250495. doi:10.1371/journal.pone.0250495.
- Sharun K, Rahman CF, Haritha CV, Jose B, Tiwari R, Dhama K. Covid-19 vaccine acceptance: Beliefs and barriers associated with vaccination among the general population in india. J Exp Biol Agric Sci. 2020;8(Special Issue 1):S210–S218. doi:10.18006/2020.8(Spl-1-SARS-CoV-2).S210.S218.
- Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, … Rubin GJ, Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVaccs), a nationally representative cross-sectional survey. Human Vacc Immunother. 2021;17(6):1612–21. doi:10.1080/21645515.2020.1846397.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. doi:10.3390/vaccines9010042.
- Islam MS, Kamal AHM, Kabir A, Southern DL, Khan SH, Hasan SM, Seale H. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021;16(5):e0251605. doi:10.1371/journal.pone.0251605.
- Rzymski P, Borkowski L, Drąg M, Flisiak R, Jemielity J, Krajewski J, Fal A. The strategies to support the COVID-19 vaccination with evidence-based communication and tackling misinformation. Vaccines. 2021;9(2):109. doi:10.3390/vaccines9020109.
- Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, Al Mamun A. COVID-19 Vaccine Hesitancy among the Adult Population in Bangladesh: a Nationally Representative Cross-sectional Survey. medRxiv. 2021.
- The Daily Star. Corona vaccine outbreak. 2021 Jan 14. https://www.thedailystar.net/
- Khan Sharun RS, Dhama K. Oxford-AstraZeneca COVID-19 vaccine (AZD1222) is ideal for resource-constrained low-and middle-income countries. Annal Med Surg. 2021.
- Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–77. doi:10.1007/s10900-020-00958-x.
- Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–51. doi:10.1016/j.puhe.2021.02.025.
- Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2021;9(1):16. doi:10.3390/vaccines9010016.
- Bujang MA, Sa’-At N, Bakar TMITA. Sample size guidelines for logistic regression from observational studies with large population: emphasis on the accuracy between statistics and parameters based on real life clinical data. Malaysian J Medi Sci. 2018;25(4):122. doi:10.21315/mjms2018.25.4.12.
- Hosmer DW Jr, Lemeshow S, Sturdivant RX Applied logistic regression. John Wiley & Sons. 2013; V(398)
- Js SA, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat Med. 2021.
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Human Vacc Immunother. 2013;9(8):1763–73. doi:10.4161/hv.24657.
- Villa A, Patton LL, Giuliano AR, Estrich CG, Pahlke SC, O’-Brien KK, … Araujo MW. Summary of the evidence on the safety, efficacy, and effectiveness of human papillomavirus vaccines: Umbrella review of systematic reviews. J Am Dental Assoc. 2020;151(4):245–54. doi:10.1016/j.adaj.2019.10.010.
- Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, … Nunes C. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi:10.3390/vaccines9030300.
- Almaghaslah D, Alsayari A, Kandasamy G, Vasudevan R. COVID-19 vaccine hesitancy among young adults in Saudi Arabia: a cross-sectional web-based study. Vaccines. 2021;9(4):330. doi:10.3390/vaccines9040330.
- Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8(3):482. doi:10.3390/vaccines8030482.
- Al-Mulla R, Abu-Madi M, Talafha QM, Tayyem RF, Abdallah AM. COVID-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines. 2021;9(6):665. doi:10.3390/vaccines9060665.
- Faezi NA, Gholizadeh P, Sanogo M, Oumarou A, Mohamed MN, Cissoko Y, Kafil HS. Peoples’ attitude toward COVID-19 vaccine, acceptance, and social trust among African and Middle East countries. Health Promot Perspect. 2021;11(2):171. doi:10.34172/hpp.2021.21.
- Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, Xiang YT. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17(6):1469. doi:10.7150/ijbs.58835.
- El-Elimat T, AbuAlsamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;16(4):e0250555. doi:10.1371/journal.pone.0250555.
- Kose S, Mandiracioglu A, Sahin S, Kaynar T, Karbus O, Ozbel Y. Vaccine hesitancy of the COVID‐19 by health care personnel. Int J Clin Pract. 2021;75(5):e13917. doi:10.1111/ijcp.13917.
- Palm R, Bolsen T, Kingsland JT. The effect of frames on COVID-19 vaccine resistance. Front Political Sci. 2021;3:41. doi:10.3389/fpos.2021.661257.
- Petravić L, Arh R, Gabrovec T, Jazbec L, Rupčić N, Starešinič N, Slavec A. Factors affecting attitudes towards COVID-19 vaccination: an online survey in Slovenia. Vaccines. 2021;9(3):247. doi:10.3390/vaccines9030247.
- Grüner S, Krüger F. The intention to be vaccinated against COVID-19: stated preferences before vaccines were available. Appl Econ Lett. 2020;1–5.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, … El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi:10.1038/s41591-020-1124-9.
- Badur S, Ota M, Öztürk S, Adegbola R, Dutta A. Vaccine confidence: the keys to restoring trust. Human Vacc Immunother. 2020;16(5):1007–17. doi:10.1080/21645515.2020.1740559.
- Cordero DA Jr. Rebuilding public trust: a clarified response to COVID-19 vaccine hesitancy predicament. J Public Health (Bangkok). 2021;43(2):e303–e304. doi:10.1093/pubmed/fdab020.
- Kanozia R, Arya R. “Fake news”, religion, and COVID-19 vaccine hesitancy in India, Pakistan, and Bangladesh. Media Asia; 2021. pp. 1–9.
- He K, Mack WJ, Neely M, Lewis L, Anand V. Parental perspectives on immunizations: Impact of the COVID-19 pandemic on childhood vaccine hesitancy. J Community Health. 2021;1–14.
- Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, Hossain MA, Al Mamun A. Health belief, planned behavior, or psychological antecedents: What predicts COVID-19 Vaccine Hesitancy better among the Bangladeshi Adults? MedRxiv. 2021.
- Hossain E, Rana J, Islam S, Khan A, Chakrobortty S, Ema NS, Bekun FV. COVID-19 vaccine-taking hesitancy among Bangladeshi people: knowledge, perceptions and attitude perspective. Human Vacc Immunother. 2021;24:1.