ABSTRACT
This study aimed to 1) determine the prevalence and contents of vaccine hesitancy among pregnant women during the coronavirus disease 2019 (COVID-19) pandemic and 2) evaluate its association with maternal sociodemographic factors. A cross-sectional survey was conducted between August and December 2020 among pregnant women between 28 and 32 weeks of gestation who received antenatal care at four clinics and hospitals in Niigata City, Japan. Vaccine hesitancy was assessed using the Parent Attitudes about Childhood Vaccines survey, and associations between vaccine hesitancy and sociodemographic factors were analyzed. In total, 113/200 (56.5%) subjects responded to the survey. Overall, 46/113 (40.7%) pregnant women were resistant or hesitant to receive the vaccine. Women with vaccine hesitancy were more likely to fear adverse reactions (concern 79.6%, not concerned 15.9%, and not sure 4.4%), safety (concerned 69.0%, not concerned 23.9%, and not sure 7.1%), and efficacy (concerned 47.8%, not concerned 35.4%, and not sure 16.8%) compared to those without vaccine hesitancy (P < .01, < .01, and <.01, respectively). In the multivariate logistic regression analyses, primipara women had higher rates of vaccine hesitancy than multipara pregnant women (odds ratio: 2.38, P = .04). In conclusion, the prevalence of vaccine hesitancy among pregnant Japanese women, especially primipara women, was higher than that in other countries during the COVID-19 pandemic. Their major concerns were adverse reactions, safety, and the efficacy of childhood vaccines. Further strategies are needed to provide appropriate vaccine information to prevent vaccine-preventable diseases in both infants and children.
Introduction
With the spread of the coronavirus disease 2019 (COVID-19) remaining unresolved, many people are promoting vaccination in the hope that it will be the key to end or slow down the spread of COVID-19. In contrast, a certain percentage of people have refused or are hesitant to get vaccinated because of the uncertainty surrounding a new infectious disease, anxiety over the rapid development and implementation of new vaccines, distrust of experts and science, inconvenience of the vaccination system, and uncertain national policy.Citation1,Citation2
Vaccine hesitancy is defined as a delay in accepting or rejecting a vaccine even though immunization services are available.Citation3 It also includes beliefs and attitudes about vaccines, including individuals who stand between complete rejection and complete acceptance of vaccines.Citation4 Globally, vaccine hesitancy is a threat to the struggle against vaccine-preventable diseases (VPD).Citation5–7 Vaccine hesitancy in general has been widely studied in Western countries, with high prevalence rates ranging from 8.9% to 28.2%.Citation6–11
Japan has been reported to have one of the lowest levels of trust in vaccines worldwide.Citation12 For example, the Japanese government suspended active recommendations for human papillomavirus (HPV) vaccination in 2013, and adverse events after HPV vaccination were widely distributed by the media without scientific evidence.Citation13 HPV vaccination coverage in Japan decreased from 68.4%–74.0% in the 1994–98 birth cohort to 0.6% in the 2000 birth cohort after the active recommendation was stopped.Citation14 The low vaccination rate of HPV vaccine has persisted, and in part, has affected vaccines in general.
To evaluate the status of vaccine hesitancy, the Parent Attitudes about Childhood Vaccines (PACV) survey was used, which is specifically designed to identify parents who are hesitant about vaccines.Citation15 This questionnaire has been validated and used to evaluate vaccine hesitancy in the United States.Citation8–10 High PACV scores have been found to coincide with vaccine-hesitant behavior, and parents with high PACV scores have been reported to have higher rates of under-immunization in their children among their children.Citation6,Citation7
During the early stages of the COVID-19 pandemic, people in Japan refrained from visiting clinics or hospitals to avoid the risk of infection, which affected vaccination rates in children. A recent survey of childhood immunization practices in four cities in Japan found that the decrease in vaccine doses administered between 2016–2019 and 2020 was most apparent in March and April 2020, just before or coincident with the declaration of the nationwide COVID-19 emergency.Citation16 This decrease in vaccine doses was more apparent in infants without significant recovery in the second half of 2020, which gave rise to a major concern that unvaccinated infants were vulnerable to VPD.Citation16
Effective educational interventions for parents should be delivered as early as possible.Citation17–21 Delays in initial vaccination in infancy can affect adherence to the immunization schedule and increase the risk of VPD. Educational interventions are particularly effective during the perinatal period,Citation18–21–Citation23 which increases knowledge and improves the immunization status.Citation20,Citation24
Given that the COVID-19 epidemic will continue in the future, vaccine withholding is likely to continue and could increase the risk of VPD in infants and children. To prevent further increases in the number of infants and children whose parents are vaccine-hesitant, it is important to intervene at an early stage to reduce parental anxiety against immunization. To maintain a high immunization rate among infants and children, it is important that parents understand the necessity of immunization and are motivated to immunize their infants and children.Citation25 Thus, there is an urgent need to investigate vaccine hesitancy among parents, especially in pregnant women, to protect infants from VPD.
The objective of this study was to determine the prevalence of vaccine hesitancy among pregnant women during the COVID-19 pandemic and identify factors associated with vaccine hesitancy. Determining these factors will allow us to consider strategies for eliminating or reducing the factors for vaccine hesitancy to protect infants and children from VPDs.
Patients and methods
Study design and setting
This was a cross-sectional, descriptive survey. The participants were recruited from four private obstetrics clinics and hospitals in Niigata from August 1 to 31 December 2020. Niigata City is located approximately 200 miles (322 km) north of Tokyo and has a population of approximately 800,000. The approximate number of deliveries at each hospital ranges from 500 to 800 per year.
Subjects
Pregnant women aged 18 years or older were recruited during gestational weeks 28–32 at antenatal classes or during prenatal examinations at the participating hospitals. All pregnant women who could communicate in Japanese were eligible for participation. Women with cognitive impairment and those for whom the investigation was an unacceptable physical or mental burden, as judged by investigators or medical professionals, were excluded. The medical staff at each hospital approached pregnant women to determine their eligibility. At the outpatient department, obstetric staff handed a letter explaining the survey to pregnant women, who were then asked if they were interested in participating in the study. Women who expressed interest completed the survey after signing the consent form.
Survey items
The PACV survey has 15 items and comprises three domains: (1) behavior, (2) safety and efficacy, and (3) general attitude. The PACV has good internal consistency with Cronbach’s alpha coefficients ranging from 0.74 to 0.84 in the three domains.Citation8 Permission to use the data was obtained from the participants for use in this study.
The 15-item self-administered questionnaire was translated into Japanese according to procedures and guidelines.Citation26,Citation27 The translation from English to Japanese was performed by a translator who was familiar with both languages and thoroughly understood the purpose of the questionnaire. Back-translation from Japanese to English was performed by another translator who was not familiar with the purpose of the questionnaire.
Subsequently, the back-translated questionnaire was compared with the original English version, and the accuracy of the Japanese version was confirmed by three researchers. In addition, the questionnaire was validated by ten mothers who had infants and/or toddlers before the survey was conducted. The mothers were asked to read and respond to a translated version of the questionnaire. All cooperating mothers understood the content and confirmed that there were no problems with the Japanese version of the PACV.
The PACV responses were assigned scores of 2 for hesitant responses, 1 for unsure responses, and 0 for non-hesitant responses. The scores for each item were summed and the total score was calculated on a scale of 0 to 30. For participating pregnant women who were expecting their first child, the maximum total score was 24 because they were unable to answer specific questions related to previous experiences with an existing child (#3, #4, and #13).Citation15 Item scores were summed in a non-weighted fashion to obtain the total raw scores, which were converted to a scale ranging from 0 to 100 using simple linear transformation and accounting for missing data. The PACV scores were dichotomized into two categories: non-hesitant (score <50) and hesitant (score ≥50), in accordance with previous literature.Citation9,Citation15
Power and statistical analyses
We assumed that 30% of the participants would be vaccine-hesitant, and assuming a power of 0.80, an alpha of 0.05, and a dropout rate of 20%, the minimum sample size required for our study was 167. Univariate analyses were performed to determine the associations between vaccine hesitancy and sociodemographic factors using the χ2 test. The associations between vaccine hesitancy and sociodemographic factors were further investigated using multivariate logistic regression analyses. All variables with p < .10 at univariate level were entered into the multivariate model. The variable which was reported to be associated with childhood vaccination status in the previous studies was also included in the model. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. The significance level was set at p < .05.
Data were recorded and analyzed using the Statistical Package for Social Sciences (version 24.0; IBM Corp., Armonk, NY, USA). Two-tailed p-values were used for all statistical tests.
This study was approved by the Niigata University Medical Research and Ethics Committee (approval number: 2020–0001).
Results
Baseline information of the pregnant women
The sociodemographic data of the pregnant women are presented in . A total of 200 questionnaires were distributed and 113 (56.5%) were returned. The median age was 31.7 years (IQR 28.2–34.0), with a range of 18 to 41 years. Approximately two-thirds (67.3%) of the pregnant women were aged >30. Comparing the age distribution of primipara (N = 52) and multipara (N = 60), 23.9% of primipara was distributed in 25–30 years and 21.2% of multipara was distributed in 31–35 years. When we compared the age distribution between the two groups, no significant difference was observed (P = .24). Less than half (43.4%) had attended university or received higher education, and 56% had an annual household income of 5,000,000 Yen (approximately US$45,500, US$1 = 110 yen) and above. Approximately half of them (53.1%) were multipara and 67.3% were employed.
Table 1. Sociodemographic characteristics of study population (N = 113).
Maternal responses to the parent attitudes about childhood vaccines
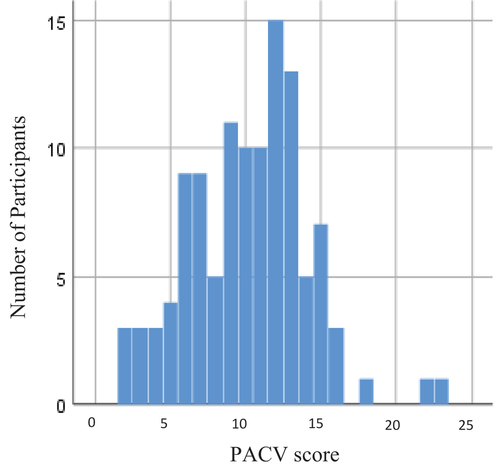
The distribution of the overall score is shown in ; 46 of 113 (40.7%) pregnant women were considered vaccine-hesitant. The median PACV raw score of the pregnant women was 10 (P25 = 7, P75 = 13), with 11% scoring ≤5. The responses to PACV are summarized in .
Table 2. Maternal responses to the parent attitudes about childhood vaccines (PACV) survey.
When we evaluated the responses to each question, the responses to Item 2, which is considered hesitance to get vaccines, were high in adverse events (#6, 79.6%), vaccine safety (#7, 69.0%), and concern that vaccination might not prevent the disease (#8, 47.8%) ().
In terms of VPD perceptions, most VPDs were serious (#3, 83.2%), and the majority of women disagreed that it was better for their children to develop immunity by getting sick than by getting vaccines (#4, 89.4%), while more than half agreed that the number of vaccines by simultaneous vaccination should be reduced (#5, 57.6%).
Regarding trust in their doctor, over half of the mothers were confident in their child’s doctor (#1, 61.9%) and agreed that they were able to discuss their concerns about vaccines with their children’s doctors (#11, 57.5%). When we compared the number of subjects in each questionnaire, there were significant differences among the three groups (P < .01, except #5, P < .05) and between scores of 2 and 0 (P < .01 except #5, P < .014; #8, P = .18; #9, P = .28).
Association between maternal sociodemographic characteristics and vaccine hesitancy ()
Vaccine hesitancy was significantly associated with educational level. Vaccine-hesitant women were more likely to be high-school graduates or lower (P = .03). Other sociodemographic characteristics, such as age (P = .53), household income (P = .08), number of children (P = .06), and employment status (P = .27), were not significantly associated with vaccine hesitancy.
Multivariate analyses
In the multivariate logistic regression analyses (), primipara women had higher rates of vaccine hesitancy than multipara pregnant women (OR: 2.38, P = .04). Other sociodemographic factors such as maternal educational level (P = .16), household income (P = .29), and maternal employment status (P = .60) were not significantly associated with vaccine hesitancy in the multivariate model.
Table 3. Associations of socio-demographic characteristics and vaccine hesitancy.
Table 4. Logistic regression analysis of factors associated with vaccine hesitancy.
Discussion
This study assessed the prevalence of vaccine hesitancy in pregnant women during the COVID-19 pandemic in Japan using the objective PACV scale. Notably, we observed a high rate of vaccine hesitancy (40.8%) among pregnant women in Japan.
Vaccine hesitancy rates in pregnant women have been reported to vary widely based on country and location. Using the same PACV survey, in Europe and the United States,Citation8–11 the rates of vaccine hesitancy range from 20 to 30%. In Asian countries, the data are only available for Malaysia, with a relatively low rate of 8.0–11.6%.Citation28,Citation29 The rates were correlated with subjects’ backgrounds, including religion, culture, medical system, education, etc.; vaccine-hesitant mothers were more likely to be non-Malay and non-Muslim. Additionally, employed pregnant women and those with monthly earnings exceeding MYR2000 (approximately 480US$) were less likely to be vaccine-hesitant. Moreover, hesitancy was less prevalent among those with more than one child.
During the COVID-19 pandemic, it is important to have confidence in the COVID-19 vaccines. In a previous study related to the acceptance of the COVID-19 vaccines in Japan, the percentage of participants who agreed to receive the vaccine was only 62.1% in January 2021.Citation30 This finding is consistent with the fact that people in Japan do not have enough confidence in vaccines in general,Citation12 despite vaccination being the only active preventive measure for infection and/or severe disease during the pandemic.
Although vaccination rates are high for routine vaccines in the national immunization program in Japan, higher rates of vaccine hesitancy were observed. This may indicate that people can become skeptical regarding vaccination if the effectiveness of vaccines against VPDs is not apparent. In addition, The Japanese have a cultural background that emphasizes social norms, and previous studies have shown that social norms including injunctive social norm and descriptive social norm for childhood immunization increased after childbirth compared to during pregnancy.Citation24 Thus, actual vaccination rates do not reflect the rates of vaccine hesitancy. However, higher rates of vaccine hesitancy may lead to lower vaccination rates.
Delays in childhood vaccination can lead to epidemics of VPDs. We expect that the COVID-19 pandemic will continue in the future, and the disadvantages related to avoiding infant health checkups and vaccination during this time will have a significant impact. It is necessary to actively encourage parents to compensate for the delay in receiving these vaccines.
Among pregnant women with vaccine hesitancy, adverse reactions and vaccine safety are the biggest concerns. In the current study, the rates of responses to items considered hesitant to vaccinate, and adverse events and vaccine safety were high,, which is consistent with a previous study of Malaysian pregnant women, in which 39–40% participants were concerned about adverse reactions and 35–37% were concerned about safety.Citation21,Citation22 The current results suggest that concerns about the adverse reactions and safety of vaccines are major reasons for hesitancy and avoidance of vaccines in Japan.
In the Vaccine Confidence Project, which was conducted in 149 countries around the world from 2015 to 2019, Japan ranked the lowest (149th) in the world, and only 17% of respondents strongly agreed that vaccination is safe.Citation12 An event that potentially contributed to this increased skepticism about vaccine safety was the campaign against HPV vaccination that began in 2013, which largely focused on adverse events. This trend did not change even after the government stated that no studies have proven a causal link between HPV vaccination and adverse health effects.Citation31 Importantly, this debate about a single vaccine has had a significant impact on the perception of vaccine safety in general. In addition, less than 60% of the pregnant women agreed to discuss their concerns about vaccines with their pediatricians, and only 61% had confidence in the pediatricians. A previous study demonstrated that healthcare providers’ vaccine recommendations in the vaccination decision-making process are critical, and healthcare providers are the most influential people in vaccination decision-making.Citation32 The results of this study showed that only two-thirds of participants trusted their healthcare providers, indicating a low level of confidence in this setting in Japan.
In addition, the limited opportunities to fully discuss vaccine concerns with professionals during the COVID-19 epidemic may be more difficult to build trust, not only because it was hard to obtain the necessary information from health care providers during the COVID-19 epidemic than before, but also because of the limited opportunities to fully discuss vaccine concerns with professionals. During the current pandemic, there was a temporary interruption in face-to-face services, such as postnatal checkups and infant visits by midwives after delivery. It is possible that the reduced opportunities and time for providing information on childhood immunizations in general during the COVID-19 pandemic have had a negative impact on the availability of accurate information on vaccines and immunization, resulting in increased exposure to misinformation from the Internet, social network system, and other sources. As the new vaccines are being promoted, we must be more concerned than ever about the impact of misinformation and rumors on vaccines.Citation33 It is necessary to establish alternative opportunities that can provide sufficient information without requiring face-to-face interactions, and further collaboration with various professionals may be required.
At the same time, methods of educational intervention will need to be considered. Motivational interviewing, a collaborative, goal-oriented style of communication with particular attention to change, has been a successful and accepted technique in this field. A previous study using motivational interviewing techniques for postpartum mothers was effective to increase infantile vaccination coverage.Citation34 It has been shown that using the motivational interviewing approach allows for a respectful and empathetic discussion of immunization concerns and builds a strong relationship between parents and health care providers. Motivational interviewing is an effective tool for overcoming vaccine hesitancy, with building trust with health care providers.Citation34
In the current study, vaccine hesitancy was found to be associated with maternal status of the child. In contrast, there was no association with age, household income, maternal education level, or employment status. Mothers who had no experience with childhood vaccination were more vaccine-hesitant. Mothers who have a first-born child may not have enough understanding of the VPD and the importance of vaccines compared to mothers who have given birth before. Parents who were uncertain about following the recommended vaccine schedule and first-born children were more likely to need additional vaccine information.Citation35 Health care providers play a major role in providing reliable and accurate information to first-time mothers; however, simultaneously, strengthening information literacy, including social networks, is an important intervention. Additionally, it is necessary to establish a platform on which people of any educational level can access information as easily as before the COVID-19 pandemic.
This study has some limitations. First, the sample size was smaller than expected. The dropout rate was most likely associated with self-selection of the study participants, and it was possible to decrease the likelihood of detecting potential differences. In addition, convenient sampling of the participants and data collection in a hospital setting may have contributed to selective bias. The generalizability of the present findings may be limited, as the participants were recruited from one region with a limited sample size. Second, the convenience sampling of the participants and data collection in a hospital setting may have contributed to selection bias. Third, the participants were likely to be interested in the content of the study. A self-selection bias may have affected the results of the present study. Last, this study did not examine if only those who are hesitant to vaccinate themselves were also hesitant to vaccinate their children, or there were differences between hesitancy to vaccinate themselves and hesitancy to vaccinate their children. Further studies related to this issue are warranted in the future. Additionally, the cross-sectional design makes it difficult to infer causality.
Conclusion
The prevalence of vaccine hesitancy in pregnant women in Niigata, Japan was higher than in other countries. Being primipara was found to be an independent risk factor for vaccine hesitancy; however, the causes of vaccine hesitancy were multifactorial and interrelated. Most parents were concerned about the safety, adverse reactions, and efficacy of vaccines in children, and if opportunities to provide adequate information are decreased under the COVID-19 pandemic, this could potentially increase the number of people with vaccine hesitancy and ultimately lead to vaccine refusal, especially for certain high-risk groups.
Acknowledgments
We would like to thank all study participants. We are also grateful to Dr. Naoto Sekizuka at Sekizuka Clinic, Dr. Masaharu Hirokawa at Niitsu Obstetric Clinic, Dr. Yasuaki Yamamoto at the Royal Heart Clinic, and Drs. Isao Hasegawa and Takehiro Serikawa at Saiseikai-Niigata Hospital.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–7. PMID: 32591957. doi:10.1007/s10198-020-01208-6.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. PMID: 33082575. doi:10.1038/s41591-020-1124-9.
- MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. PMID: 25896383. doi:10.1016/j.vaccine.2015.04.036.
- Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences and call to action. Vaccine. 2015;33(Suppl 4):D66–D71. doi:10.1016/j.vaccine.2015.09.035.
- Dubé E, Gagnon D, MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: review of published reviews. Vaccine. 2015;33(34):4191–203. PMID: 25896385. doi:10.1016/j.vaccine.2015.04.041.
- Oladejo O, Allen K, Amin A, Frew PM, Bednarczyk RA, Omer SB. Comparative analysis of the parent attitudes about childhood vaccines (PACV) short scale and the five categories of vaccine acceptance identified by Gust et al. Vaccine. 2016;34(41):4964–68. PMID: 27566902. doi:10.1016/j.vaccine.2016.08.046.
- Siddiqui M, Salmon DA, Omer SB. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother. 2013;9(12):2643–48. PMID: 24247148. doi:10.4161/hv.27243.
- Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–605. PMID: 21763384. doi:10.1016/j.vaccine.2011.06.115.
- Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013;167(11):1065–71. PMID: 24061681. doi:10.1001/jamapediatrics.2013.2483.
- Strelitz B, Gritton J, Klein EJ, Bradford MC, Follmer K, Zerr DM, Englund JA, Opel DJ. Parental vaccine hesitancy and acceptance of seasonal influenza vaccine in the pediatric emergency department. Vaccine. 2015;33(15):1802–07. PMID: 25744225. doi:10.1016/j.vaccine.2015.02.034.
- Williams SE, Morgan A, Opel D, Edwards K, Weinberg S, Rothman R. Screening tool predicts future underimmunization among a pediatric practice in Tennessee. Clin Pediatr (Phila). 2016;55(6):537–42. PMID: 26581360. doi:10.1177/0009922815615823.
- de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi:10.1016/S0140-6736(20)31558-0.
- Gilmour S, Kanda M, Kusumi E, Tanimoto T, Kami M, Shibuya K. HPV vaccination programme in Japan. Lancet. 2013;382(9894):768. PMID: 23993189. doi:10.1016/S0140-6736(13)61831-0.
- Hanley SJ, Yoshioka E, Ito Y, Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385(9987):2571. PMID: 26122153. doi:10.1016/S0140-6736(15)61152-7.
- Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, Martin DP. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7(4):419–25. PMID: 21389777. doi:10.4161/hv.7.4.14120.
- Aizawa Y, Katsuta T, Sakiyama H, Tanaka-Taya K, Moriuchi H, Saitoh A. Changes in childhood vaccination during the coronavirus disease 2019 pandemic in Japan. Vaccine. 2021;39(29):4006–12. PMID: 34059371. doi:10.1016/j.vaccine.2021.05.050.
- Glanz JM, Wagner NM, Narwaney KJ, Shoup JA, McClure DL, McCormick EV, Daley MF. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad Pediatr. 2013;13(5):481–88. PMID: 24011751. doi:10.1016/j.acap.2013.05.030.
- Návar AM, Halsey NA, Carter TC, Montgomery MP, Salmon DA. Prenatal immunization education the pediatric prenatal visit and routine obstetric care. Am J Prev Med. 2007;33(3):211–13. PMID: 17826581. doi:10.1016/j.amepre.2007.04.027.
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED. Holmboe ESQualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–41. PMID: 16651306. doi:10.1542/peds.2005-1728.
- Vannice KS, Salmon DA, Shui I, Omer SB, Kissner J, Edwards KM, Sparks R, Dekker CL, Klein NP, Gust DA. Attitudes and beliefs of parents concerned about vaccines: impact of timing of immunization information. Pediatrics. 2011;127(Suppl 1):S120–6. PMID: 21502250. doi:10.1542/peds.2010-1722R.
- El-Mohandes AA, Katz KS, El-Khorazaty MN, McNeely-Johnson D, Sharps PW, Jarrett MH, Rose A, White DM, Young M, Grylack L, et al. The effect of a parenting education program on the use of preventive pediatric health care services among low-income, minority mothers: a randomized, controlled study. Pediatrics. 2003;111(6 Pt 1):1324–32. PMID: 12777548. doi:10.1542/peds.111.6.1324.
- Bjornson GL, Scheifele DW, Gold R. Assessment of parent education methods for infant immunization. Can J Public Health. 1997;88(6):405–08. PMID: 9458569. doi:10.1007/BF03403916.
- Zúñiga de Nuncio ML, Nader PR, Sawyer MH, De Guire M, Prislin R, Elder JP. A prenatal intervention study to improve timeliness of immunization initiation in Latino infants. J Commun Health. 2003;28(2):151–65. PMID: 12705316. doi:10.1023/a:1022651631448.
- Saitoh A, Nagata S, Saitoh A, Tsukahara Y, Vaida F, Sonobe T, Kamiya H, Naruse T, Murashima S. Perinatal immunization education improves immunization rates and knowledge: a randomized controlled trial. Prev Med. 2013;56(6):398–405. PMID: 23524116. doi:10.1016/j.ypmed.2013.03.003.
- Awadh AI, Hassali MA, Al-Lela OQ, Bux SH, Elkalmi RM, Hadi H. Does an educational intervention improve parents’ knowledge about immunization? Experience from Malaysia. BMC Pediatr. 2014;14:254. PMID: 25284603. doi:10.1186/1471-2431-14-254.
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–91. PMID: 11124735. doi:10.1097/00007632-200012150-00014.
- Guillemin F, Bombardier C, Beaton D. Cross-Cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–32. PMID: 8263569. doi:10.1016/0895-4356(93)90142-n.
- Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. PMID: 28434687. doi:10.1016/j.vaccine.2017.04.010.
- Kalok A, Loh SYE, Chew KT, Abdul Aziz NH, Shah SA, Ahmad S, Mohamed Ismail NA, Abdullah Mahdy Z. Vaccine hesitancy towards childhood immunisation amongst urban pregnant mothers in Malaysia. Vaccine. 2020;38(9):2183–89. PMID: 32001070. doi:10.1016/j.vaccine.2020.01.043.
- Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, Takamiya T, Odagiri Y, Fukushima N, Kikuchi H, et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines (Basel). 2021;9(3):210. PMID: 33802285. doi:10.3390/vaccines9030210.
- Suzuki S, Hosono A. No association between HPV vaccine and reported post-vaccination symptoms in Japanese young women: results of the Nagoya study. Papillomavirus Res. 2018;5:96–103. PMID: 29481964. doi:10.1016/j.pvr.2018.02.002.
- Wiley KE, Massey PD, Cooper SC, Wood N, Quinn HE, Leask J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: a cross sectional survey. Vaccine. 2013;31(37):3972–78. PMID: 23777954. doi:10.1016/j.vaccine.2013.06.015.
- Larson HJ. Stuck: how vaccine rumors start–and why they don’t go away. In Oxford University Press; 2020. p. 1–32. Chapter1,Chapter2.
- Gagneur A, Lemaître T, Gosselin V, Farrands A, Carrier N, Petit G, Valiquette L, De Wals P. A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health. 2018;18:811. doi:10.1186/s12889-018-5724-y.
- Napolitano F, D’-Alessandro A, Angelillo IF. Investigating Italian parents’ vaccine hesitancy: a cross-sectional survey. Hum Vaccin Immunother. 2018;14(7):1558–65. PMID: 29641945.Table 1. doi:10.1080/21645515.2018.1463943.