ABSTRACT
Aim
We aimed at assessing the published literature on different prophylactic screening and vaccination options in inflammatory bowel disease (IBD) patients between 1980 and 2020. Special attention was attributed to latest data assessing covid-19 vaccinations.
Methods
We have queried PubMed for all available IBD-related entries published during 1980–2020. The following data were extracted for each entry: PubMed unique article ID (PMID), title, publishing journal, abstract text, keywords (if any), and authors’ affiliations. Two gastrointestinal specialists decided by consensus on a list of terms to classify entries. The terms belonged to four treatment groups: opportunistic infections, prophylactic screening, prophylactic vaccinations/treatment, and routine vaccines. Annual trends of publications for the years 1980–2020 were plotted for different screening, vaccinations and infection types. Slopes of publication trends were calculated by fitting regression lines to the annual number of publications.
Results
Overall, 98,339 IBD entries were published between 1980 and 2020. Of those, 7773 entries belonged to the investigated groups. Entries concerning opportunistic infections showed the sharpest rise, with 19 entries and 1980 to 423 entries in 2020 (slope 11.3, p < .001). Entries concerning prophylactic screening rose from 10 entries in 1980 to 204 entries in 2020 (slope 5.4, p < .001). Both entries concerning prophylactic vaccinations/treatments and routine vaccines did not show a significant rise (slope 0.33 and slope 0.92, respectively). During the COVID 19 pandemic, a total of 44 publications were identified. Of them, 37 were relevant to vaccines and immune reaction. Nineteen publications (51%) were guidelines/recommendations, and 14 (38%) assessed immune reaction to vaccination, most of them (11, 61%) to mRNA vaccines.
Conclusions
During the past two decades, along with a rapid increase in biologic therapy, publications regarding opportunistic infections and prophylactic screening increased in a steep slope compared to the two decades in the pre-biologic area. During the COVID-19 pandemic, most publications included vaccination recommendations and guidelines and only 38% included real-world data assessing reaction to vaccinations. More research is needed.
Introduction
Crohn’s disease (CD) and Ulcerative colitis (UC) are chronic inflammatory bowel diseases (IBD) involving the gastrointestinal (GI) tract. While in CD inflammation may affect the whole GI tract from mouth to anus, inflammation in UC mainly affects the colon. Both diseases may cause significant morbidity and diminished quality of life.Citation1–5 Disease behavior is usually characterized by periods of exacerbations with active symptomatic disease and periods of remission.Citation6
Disease pathogenesis is believed to be multifactorial and is influenced by genetic susceptibility, environmental factors such as diet, smoking, and bacterial and viral infections, gut microbiota, and immunological abnormalities.Citation7–9
As dysregulation of the innate immune system with production of pro-inflammatory cytokines and epithelial damage is the characteristic of IBD, most treatment options consist of immune modulation therapies.Citation10 During the last two decades, major progress was achieved in the field of IBD treatment, with the introduction and approval of biologic treatment.Citation11 These highly efficient therapies became the cornerstone of IBD treatment.Citation11 Modulating the immune system, these new therapies expose the patients to various potential infections, and guidelines for prophylactic vaccinations and pre-treatment were issued.Citation12
Current computational power and machine learning development provoked the “text-mining” technique. This method enables broad-scale data extraction.Citation13 Text-mining may be employed to characterize trends and examine dynamics in a research field.Citation14
During the last two decades, the biologic era revolutionized the entire therapeutic approach in IBD and provoked new prophylactic strategies for infection prevention and treatment.
We believe that the text mining technique can enlighten and clarify these trends and point at therapeutic development and tendencies in the last few decades and the upcoming years.
The COVID-19 pandemic ingested more challenges regarding its effect on immune-deficient patients and vaccinations’ effectivity in these patients
Therefore, in our current study, we aimed at assessing published literature on IBD-related infections and vaccinations in the past four decades. Special attention was attributed to data assessing COVID 19 vaccinations.
Materials and methods
Dataset
The U.S. National Center for Biotechnology Information (NCBI) provides public application programming interfaces (APIs) that allow programmatic access to the PubMed database. The publicly available PyMed Python library was used to query the PubMed API.
The following data were extracted for each entry: PubMed unique article ID (PMID), title, publishing journal, abstract text, keywords (if any), and authors’ affiliations. The search was performed on January 7, 2022.
Inclusion criteria
The entire MEDLINE/PubMed database was used as the source for this article. We retrieved all available IBD-related entries. The search was conducted in entries’ titles, abstracts, and keywords using the medical subject headings (MeSH) terms “ulcerative colitis” OR “Crohn” OR “inflammatory bowel disease”.
We have limited the entries to those published from January 1, 1980, to December 31, 2020.
Two gastrointestinal specialists (A.L and E.S) decided by consensus on a list of terms to classify entries (). The terms list was determined according to the Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease.Citation15 All terms were specifically addressed in the consensus.
Table 1. List of terms used to classify entries into four infections and vaccination groups: Opportunistic infections, prophylactic screening, prophylactic vaccinations/treatment, and routine vaccinations
The terms belonged to four groups: opportunistic infections, prophylactic screening, prophylactic vaccinations/treatment, and routine vaccines. The search was conducted on the entire available PubMed entries’ titles and abstracts. All terms were specified.
A further detailed analysis was performed for COVID-19-related publications. These publications were obtained using the search terms COVID-19 and SARS-CoV-2.
Data processing
Data processing and result visualization were written in Python (Ver. 3.6.5, 64 bits). Each title, study abstract, and authors’ affiliations were lowercased. Statistical significance was established at a 2-sided P < .05. Descriptive statistics were reported using counts with percentages for categorical variables.
Annual trends of publications for the years 1980–2020 were plotted for different screening, vaccinations and infection types. Slopes of publication trends were calculated by fitting regression lines to the annual number of publications (with × being the year of publication and Y being the annual publication number). Standard errors (SE) and P-values were calculated for the linear regression lines.
Results
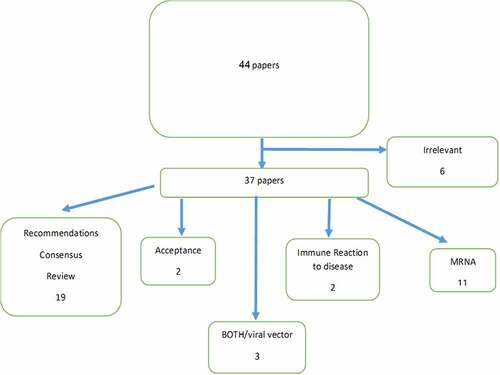
Overall, 98,339 IBD-related entries were published between 1980 and 2020. Of those, 7773 (7.9%) entries belonged to four investigated groups (). Study’s inclusion flow chart is shown in .
The plots of the trends of publications for the different groups are presented in .
Figure 2. Publication trends of vaccines and opportunistic infections in IBD patients during the past four decades.
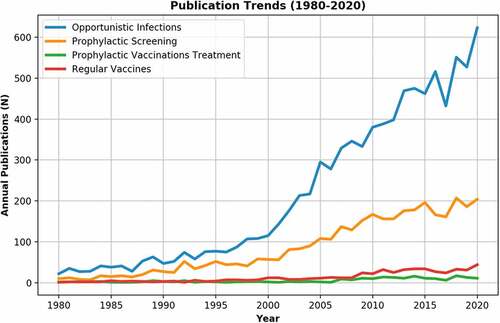
Opportunistic infections were by far the most studied subject, comprising 83.3% of all infection and vaccination publications. Furthermore, entries concerning opportunistic infections showed the sharpest rise, with 19 entries published in 1980 to 423 entries published in 2020 (slope 11.3, p < .001, SE 0.69)
Opportunistic infection publications were followed by prophylactic screening (45.3%), routine vaccines (6.8%) and prophylactic vaccinations/treatment (2.7%). Entries concerning prophylactic screening rose from 10 entries in 1980 to 204 entries in 2020 (slope 5.4, p < .001, SE 0.24). Both entries concerning prophylactic vaccinations/treatments and routine vaccines did not show a significant rise (slope .33, p < .001, SE 0.04, and slope 0.92, p < .001, SE 0.07, respectively). Opportunistic infections that had the majority contribution to the steep rise in PubMed entrees included tuberculosis (1901 publications, 24.5%), candida (1607 publications, 20.7%), clostridium (1046 publications, 13.5%), and CMV (687 publications, 8.8%).
During the COVID-19 pandemic, a total of 44 publications were identified. presents the publications related to COVID 19 vaccines during the pandemic. Of them. Thirty-seven were relevant to vaccines and immune reaction. Nineteen publications (51%) were guidelines/recommendations, and 14 (38%) assessed immune reaction to vaccination, most of them (11, 61%) to mRNA vaccines.
Discussion
Immune modulation therapies, which constitute the cornerstone of IBD treatment, expose patients to various opportunistic infections.Citation12 Therefore, pre-treatment screening and vaccinations are now part of IBD treatment guidelines.Citation15
Notably, during the past two decades, enhanced progress was achieved in the field of IBD treatment.
Since the introduction of the first biologic treatment for IBD (infliximab) at the end of the millennium,Citation16 more biologics and non-biologic immunomodulating medications offering various mechanisms of action were added to therapeutic arsenal, and many more are still in pipeline.Citation10 These innovative medications opened new horizons in IBD treatment and enabled more ambitious therapeutic goals as mucosal healing and deep remission.Citation17 However, as the use of new immunosuppressive drugs and multi-drug regimens became common, more treatment-related infections became prevalent and necessitated specific preventive protocols. Data assessing specific potential infections were of major interest for both caregivers and patients, as some of these infections might be preventable using pre-treatment screening and vaccinations (e.g. TB and herpes zoster), and many others will be better treated when early diagnosed—pending caregiver awareness for potential infections.Citation18,Citation19
Consequently, in our current study, we applied a text mining approach to observe and analyze IBD infection and vaccination publications in the past four decades, aiming to achieve some comprehension about treatment trends and development over the years with specific focus on the last two decades.
We believe that the text mining technique can enlighten and clarify these trends and point directly at treatment development and tendencies in the last few decades and the upcoming years.
According to our results, approximately 83.3% of the literature published on IBD infections and vaccinations was issued in the last two decades, with an increasing number each year.
Opportunistic infections were by far the most studied subject, comprising 86.9% of all infection and vaccination publications. We believe that this specific rise and focus on publications regarding opportunistic infections resulted from the rising awareness, as data accumulated, of treatment risks, and, moreover, to the unquestionable clinical value of early detection of these infections and for preventive measurement when feasible.
Opportunistic infection publications were followed by prophylactic screening (45.3%), routine vaccines (6.8%) and prophylactic vaccinations/treatment (2.7%).
Furthermore, opportunistic infection publications showed the steepest slope (slope 11.3, p < .001), which indicates the most rapid growth in publication rate. Publications increased approximately ×20 from 1980 to 2020. These numbers reflect the accelerated rate of new medications development and implementation in the IBD field during the last few years, all of them based on immune modulation and the increase in disease prevalence and incidence and the rising global disease burden.Citation20
Publications regarding prophylactic screening rose ×20 from 1980 to 2020 (slope 5.4, p < .001), reflecting the increased interest and awareness of opportunistic infection risk following immune-modulating therapies for IBD.Citation12
Publications concerning prophylactic vaccinations/treatments and routine vaccines did not show a significant rise (slope 0.33, and slope 0.92, respectively), probably as there was no change in approach toward routine vaccinations.
Consequently, the 5 most highly cited articles in this searchCitation21–25 evaluated different opportunistic infections during IBD treatment. The most cited paper,Citation21 published in the New England journal of medicine in 2001 reported for the first time the high risk of active tuberculosis during infliximab treatment and suggested active screening before treatment initiation. This was the first swallow in a long series of publications revealing opportunistic infections during specific immunosuppressive treatments and recommendations for pre-treatment screening and vaccinations.Citation22–25
COVID-19 pandemic has forced major changes in healthcare systems worldwide. As vaccines became available, data regarding their efficacy in various background medical conditions and therapies started to accumulate. In IBD, 37 papers are currently available. Of them, most papers (51%) include recommendations and consensus statements, and 38% assesses immune reaction to vaccination—most of them (79%) mRNA vaccines. These data are preliminary, as data are still accumulating these days, yet emphasize the importance of disease prevention in IBD patients.
Our study has a few limitations. This analysis only provides a high-level look at the field. The sheer number of publications prohibits a manual analysis of the records. A list of terms was determined based on current data in the literature, specifically the latest ECCO guidelines and consensus between two senior IBD specialist physicians. However, different terms might have achieved different results. The data were extracted from MEDLINE/PubMed. Other options such as Google Scholar were not included and might have reached different results. Also, subgroup analysis based on the place of the study and type of article was not performed and can be further analyzed in future works.
Furthermore, the rise in immunotherapies during the last decades is a trend in other autoimmune diseases and not specific to IBD. Most of the immunotherapies in the IBD field are used for other indications as well, the most common are rheumatoid arthritis (RA) and psoriasis.Citation26
In conclusion, according to our high-level publications trend analysis, during the past two decades, along with the rapid increase in biologic therapy, publications regarding opportunistic infections and prophylactic screening increased in a steep slope compared to the two decades in the pre- biologic area. On the contrary, publications assessing regular vaccines did not change along the last four decades. These data reflect the increased interest in preventing and treating potential infections during immunomodulating therapy. We believe that this trend will continue and enhance, as more treatment options will be offered to our IBD patients and more data will accumulate regarding potential specific infection risks.
During the COVID-19 pandemic, most publications included vaccination recommendations and guidelines and only 38% included real-world data assessing the reaction to vaccinations. More research in this area collecting real-world data is needed for wider and better patient care and for better understanding the needs during the current rapidly changing pandemic.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Love JR, Irvine EJ, Fedorak RN. Quality of life in IBD. J Clin Gastroenterol. 1992;14:15–6. doi:10.1097/00004836-199201000-00005.
- Casellas F, Arenas JI, Baudet JS, Fábregas S, García N, Gelabert J, Medina C, Ochotorena I, Papo M, Rodrigo L, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis. 2005;11:488–96. doi:10.1097/01.MIB.0000159661.55028.56.
- Rubin GP, Hungin AP, Chinn DJ, Dwarakanath D. Quality of life in patients with established inflammatory bowel disease: a UK general practice survey. Aliment Pharmacol Ther. 2004;19:529–35. doi:10.1111/j.1365-2036.2004.1873.x.
- Casellas F, López-Vivancos J, Badia X, Vilaseca J, Malagelada J-R. Influence of inflammatory bowel disease on different dimensions of quality of life. Eur J Gastroenterol Hepatol. 2001;13:567–72. doi:10.1097/00042737-200105000-00017.
- Canavan C, Abrams KR, Hawthorne B, Drossman D, Mayberry JF. Long-Term prognosis in Crohn’s disease: factors that affect quality of life. Aliment Pharmacol Ther. 2006;23:377–85. doi:10.1111/j.1365-2036.2006.02753.x.
- Latella G. Crucial steps in the natural history of inflammatory bowel disease. World J Gastroenterol. 2012 Aug 7;18(29):3790–99. doi:10.3748/wjg.v18.i29.3790.
- Monteleone G, Fina D, Caruso R, Pallone F. New mediators of immunity and inflammation in inflammatory bowel disease. Curr Opin Gastroenterol. 2006;22(4):361–64. doi:10.1097/01.mog.0000231808.10773.8e.
- Kaser A, Zeissig S, Blumberg RS. Inflammatory bowel disease. Annu Rev Immunol. 2010;28(1):573–621. doi:10.1146/annurev-immunol-030409-101225.
- Guan Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. 2019 Dec 1;2019:7247238. doi:10.1155/2019/7247238. PMID: 31886308; PMCID: PMC6914932.
- Chudy-Onwugaje KO, Christian KE, Farraye FA, Cross RK. A State-of-the-Art review of new and emerging therapies for the treatment of IBD. Inflamm Bowel Dis. 2019 Apr 11;25(5):820–30.
- Klang E, Barash Y, Soffer S, Shachar E, Lahat A. Trends in inflammatory bowel disease treatment in the past two decades-a high-level text mining analysis of PubMed publications. United European Gastroenterol J. 2021 Nov;9(9):1019–26. Epub 2021 Aug 25. doi:10.1002/ueg2.12138. PMID: 34431607; PMCID: PMC8598961.
- Borman ZA, Côté-Daigneault J, Colombel JF. The risk for opportunistic infections in inflammatory bowel disease with biologics: an update. Expert Rev Gastroenterol Hepatol. 2018 Nov;12(11):1101–08. doi:10.1080/17474124.2018.1530983.
- Thuraisingham B. Data mining: technologies, techniques, tools, and trends. Boca Raton: CRC Press; 2014.
- Song M, Kim SY. Detecting the knowledge structure of bioinformatics by mining full-text collections. Scientometrics. 2013;96:183–201. doi:10.1007/s11192-012-0900-9.
- Rahier JF, Magro F, Abreu C, Armuzzi A, Ben-Horin S, Chowers Y, Cottone M, de Ridder L, Doherty G, Ehehalt R, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014 Jun;8(6):443–68. Epub 2014 Mar 6. doi:10.1016/j.crohns.2013.12.013.
- Rutgeerts P, Baert F. New strategies in the management of inflammatory bowel disease. Acta Clin Belg. 1999 Oct;54(5):274–80. doi:10.1080/17843286.1999.11754245.
- Turner D, Ricciuto A, Lewis A, D’-Amico F, Dhaliwal J, Griffiths AM, Bettenworth D, Sandborn WJ, Sands BE, Reinisch W, et al. STRIDE-II: an Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021 Apr;160(5):1570–83. doi:10.1053/j.gastro.2020.12.031.
- Beaugerie L, Rahier JF, Kirchgesner J. Predicting, preventing, and managing treatment-related complications in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2020 May;18(6):1324–35. doi:10.1016/j.cgh.2020.02.009.
- Kirchgesner J, Lemaitre M, Carrat F, Zureik M, Carbonnel F, Dray-Spira R. Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases. Gastroenterology. 2018 Aug;155(2):337–46. doi:10.1053/j.gastro.2018.04.012.
- Windsor JW, Kaplan GG. Evolving epidemiology of IBD. Curr Gastroenterol Rep. 2019 Jul 23;21(8):40. doi:10.1007/s11894-019-0705-6.
- Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD, Siegel JN, Braun MM. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001 Oct 11;345(15):1098–104. doi:10.1056/NEJMoa011110.
- Hueber W, Sands BE, Lewitzky S, Vandemeulebroecke M, Reinisch W, Higgins PD, Wehkamp J, Feagan BG, Yao MD, Karczewski M, et al. Secukinumab, a human anti-IL-17A monoclonal antibody, for moderate to severe Crohn’s disease: unexpected results of a randomised, double-blind placebo-controlled trial. Gut. 2012 Dec;61(12):1693–700. doi:10.1136/gutjnl-2011-301668.
- Sandborn WJ, Su C, Panes J. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017 Aug 3;377(5):496–97.
- Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019 Dec;68(Suppl 3):s1–s106. Epub 2019 Sep 2. doi:10.1136/gutjnl-2019-318484.
- Reinisch W, Sandborn WJ, Hommes DW, D’-Haens G, Hanauer S, Schreiber S, Panaccione R, Fedorak RN, Tighe MB, Huang B, et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut. 2011 Jun;60(6):780–87. doi:10.1136/gut.2010.221127.
- Udalova I, Monaco C, Nanchahal J, Feldmann M, Gordon S. Anti-TNF therapy. Microbiol Spectr. 2016 Aug;4(4). doi:10.1128/microbiolspec.MCHD-0022-2015