ABSTRACT
Measles can have a substantial negative impact not only on people’s health but also on their finances, especially in developing countries. This study evaluates the household risk of catastrophic health expenditure (CHE) due to measles, according to regions and wealth quintiles. The CHE risk due to measles was computed based on (1) the likelihood of health service utilization to treat measles, (2) out-of-pocket (OOP) expenditure and indirect costs associated with disease treatment, and (3) household consumption expenditures. I derived the CHE risk associated with measles, conditional on contracting the disease, across regions and wealth quintiles in Nigeria, using secondary data sources for health-care utilization, OOP expenditures, and consumption expenditures. There was a large variation in CHE risk according to regions and wealth quintiles. Among the poorest households, those in the northeast and northwest would have the highest risk of CHE, up to 17%, while those in the southwest would have the lowest risk of 5%. For all regions, as the wealth increases, the CHE risk would decrease. There would be zero or very little CHE risk among the richest households in any regions. Given the proven efficacy of measles vaccines, immunizations can prevent households, especially poorer households in northeast and northwest regions, from facing the CHE risk due to measles.
Introduction
Measles is highly contagious and deadly without vaccination. It is estimated that measles killed over 200,000 people across the globe in 2019, and over 70% of the reported measles cases were found in Africa.Citation1 Furthermore, Nigeria, the focus of the study, has the largest number of measles cases in the world in 2021, with more than 6700 cases.Citation2
Measles can have a substantial negative impact not only on people’s health but also on their finance.Citation3 Immunization can not only save millions of lives, but it can also save millions of health expenditures necessary to treat measles. In other words, vaccination against measles works as a financial risk protection (FRP).
The impact of vaccines on economic benefit has been discussed in the literature. It has been proven that vaccines are highly cost-effective in preventing diseases as compared to other interventions.Citation4,Citation5 It was shown that an investment of $34 billion for the immunization programs in developing countries saved $586 billion in the reduction of cost of illness.Citation6
The economic consequences of vaccine-preventable diseases have also been studied in African countries.Citation7–9 However, the study on the economic consequence of measles in Nigeria is limited, despite its importance due to the heavy burden of the disease in the country.
Thus, this paper intends to quantify the potential impact of measles vaccines on financial risk protection. In particular, I focus on the incidence of catastrophic health expenditures (CHEs) as an indicator of FRP in this paper. CHE is defined as OOP medical expenditures surpassing a certain threshold of income or consumption expenditures. This is one of the first papers to evaluate the household risk of CHE as a result of contracting measles in Nigeria. I investigate differences in CHE risks according to regions and wealth quintiles. I hypothesize that CHE risks will differ substantially according to wealth level and by regions because CHE risks depend on the relative OOP costs of disease treatment to the household expenditure, as well as the likelihood of service utilization for disease treatment.
Methodology
In this section, I present the main approach to estimate the risk of facing CHE as a consequence of contracting measles, conditional on being affected by measles in Nigeria.
Modeling risk of CHE due to measles
Generally, for a household, the risk of facing CHE, conditional on contracting measles, will depend on (i) the likelihood of health-care utilization to treat measles; (ii) the amount of OOP health expenditures and indirect costs associated with measles treatment; and (iii) the level of household total consumption expenditures. All three subcomponents could vary with the wealth level. Here, in this study, the wealth is proxied by the asset level of households (poorest, poorer, middle, richer, and richest) in the population.
I used the likelihood of seeking treatment for fever as a proxy for the health-care utilization for measles by zone and wealth quintile drawing from Nigeria demographic and health survey (DHS) conducted in 2018 (). I used the treatment-seeking behavior for fever as a proxy for measles as the first symptom of measles is fever, and a similar approach was taken in the previous studies.Citation9,Citation10 The wealth quintile in DHS data was predefined by DHS according to the asset level of each household.
Table 1. Health service utilization (%) by region and wealth quintiles in Nigeria.
Illness-related costs associated with the treatment of measles included several components: OOP direct medical costs, OOP transportation costs to health facilities, and indirect costs (). For the amount of OOP health expenditures, I used WHO CHOICE for Nigeria.Citation11 As the information in WHO CHOICE was based in the USD 2007, I converted the cost information to the values in 2018 using the inflation rate. According to their calculation, it costs $10.5 for inpatient treatment, while it costs $2.43 for outpatient treatment. For OOP transportation costs, I used $1.06 for outpatient care and $6.86 for inpatient care, based on Memirie et al. (2017), due to limited data availability in Nigeria.Citation12 These cost estimates are not far from the transportation costs to clinic for other services in the Nigerian context.Citation13,Citation14 Indirect costs had two components: an estimated “wage rate” and a number of workdays lost due to inpatient stays. For the wage rate, I used mean annual consumption expenditures per adult equivalent according to region and wealth quintile. I assumed that the average bed day is 4 d with 25% probability of hospitalization.Citation9,Citation15
Table 2. Cost information and other parameters that do not change across regions and wealth quintiles.
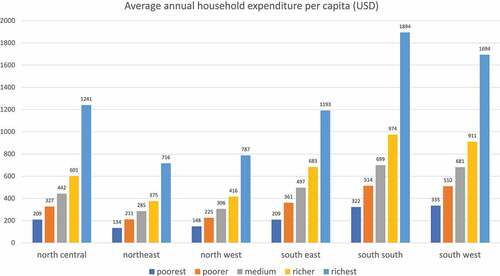
The annual consumption expenditure was drawn from Nigeria Living Standards Survey (NLSS), which is the national representative survey conducted from 2018 to 2019.Citation16 I calculated the average annual consumption per capita according to region and wealth quintile (). I used the different dataset (NLSS) for estimating the annual consumption expenditure because of the lack of information on the consumption expenditure in DHS data. Households in NLSS were divided into five based on the level of the annual consumption expenditure, and the average consumption expenditure in each of five quintiles was considered the level of consumption for each wealth quintile. Although the wealth quintile defined in DHS data would not perfectly match with the quintile based on the consumption expenditure in NLSS data, we assumed that there was a positive correlation between them. Throughout the paper, we used the wealth quintile definition made in DHS dataset. We used the conversation rate of 1 naira = USD 0.0027 (2018).
Figure 1. Average annual household expenditure per capita (USD by region and wealth quintiles) in Nigeria.
With the information above, I could derive a risk of facing a CHE case as a result of contracting measles. Employing the methods from Riumallo-Herl et al. (2018),Citation17 I estimated the number of cases of CHE associated with measles in each region at each wealth quintile. A case of CHE for measles was counted when total patient-incurred expenditures, which is the total OOP costs of medical, transportation, and indirect costs, surpassed 20% of total annual consumption expenditures. I also used alternative thresholds of 10% and 40% in sensitivity analyses to find the consistent results. Finally, I reported, per wealth quintile in each region of Nigeria, on the risk of facing CHE conditional on contracting measles.
All simulations were conducted using R statistical software (version 3.6.0) and STATA (version 15.1).
Results
The CHE estimation depends on the levels of health service utilization, OOP expenditure and time losses for disease treatment, and the consumption expenditures of households. First, I present the distribution of consumption expenditure according to region and wealth quintile (). Northeast region has the lowest consumption expenditure for all the wealth quintile. The poorest households in the northeast on average spend $134 annually for consumption, while the richest households spend $716. Northwest also has the low level of consumption expenditure. On the other hand, south-south and southwest regions are the richest regions in Nigeria: the poorest households in these regions spend about $330 for consumption, and this is much higher than the expenditure level among the medium households in northeast, $285. The richest households in south-south region spend the most, $1,894.
Now I report on the variations in CHE risk due to measles across region and wealth quintiles (). On average, households in the northeast would have the highest CHE risk of 9.4%, while households in the southwest would have the lowest CHE risk of 1.0%.
Table 3. Catastrophic health expenditure (CHE) risk (%) by region and wealth quintile in Nigeria.
Among the poorest households, those in the northeast and northwest would have the highest risk, up to 17%, while those in the southwest would have the lowest risk of 5%. For all regions, as the wealth increases, the CHE risk would decrease. However, the reduction gradient from the poorest to poorer and to medium differs by region. The CHE risk decreases drastically as the wealth level increases in southern regions (southeast, south-south, and southwest). For example, the CHE risk decreases from 8.7%, 0.01%, and 0% from the poorest, the poorer, to the medium households in south-south region. On the other hand, the gradient of the reduction is much more modest in the northeast and northwest. For example, the CHE risk remains above 12% for the poorest, the poorer, and the medium households in northeast, and then, it decreases to 3% for the richer households. There would be zero or very little CHE risk among the richest households in any regions.
Discussion
I evaluated the risk of experiencing CHE conditional on being infected by measles in Nigeria. The analysis was based on secondary data sources on health service utilization, OOP expenditure, time and wage losses for disease treatment, and consumption expenditure. The measles CHE risk was computed across wealth quintiles in six geographical regions in Nigeria.
Through this modeling exercise, I found that the risk of CHE due to measles would vary greatly according to wealth quintiles and regions. Wealth quintiles were poorest, poorer, medium, richer, and richest. There are six regions in Nigeria: north central, northeast, northwest, southeast, south-south, and southwest.
The variation in CHE risk across six regions mostly coincides with the variation in consumption expenditure across these regions: if the average consumption expenditure in a region was higher, then the CHE risk in the region was lower. The average consumption expenditure was the lowest in northeast and northwest regions, and the CHE risk in these two regions was the highest: over 9%. On the other hand, the average consumption was the highest in south-south and southwest, and the CHE risk in these regions was the lowest: 1.5–2.3%. This correlation generally holds because richer households have less chance of experiencing the catastrophic expenditure from measles treatment as compared to poorer households who have tighter budget constraints.
Generally, poorer households have the lower likelihood of health service utilization to minimize the risk of catastrophic health expenditure. Unlike this general trend, however, southwest regions, one of the regions with the highest consumption expenditure, have lower health service utilization than northeast and northwest regions for any wealth quintiles. Rather, the poorest regions, northeast and northwest, have relatively high health service utilization. This high health service utilization with lower wealth level pushes the CHE risk higher in northeast and northwest regions, while the low health utilization with high wealth level keeps the CHE risk low in southwest region.
Across wealth quintiles in each region, the CHE risk decreases as the wealth level increases from the poorest to the richest. This finding is consistent with the literature.Citation9 There was zero or very little CHE risk among the richest quintile, while the CHE risk was over 10% among the poorest quintile on average. However, the gradient of the reduction of CHE risk from poorer to richer households differs by region. Northeast and northwest regions observed the similar CHE risk among the poorest, poorer, and medium households, while other regions observed a rather drastic reduction in CHE risk from the poorest to the poorer households. This result in the northeast and northwest is because the increase in the consumption expenditure across wealth quintiles was almost canceled out with the increased likelihood of health service utilization, while other regions observed that the increase in consumption expenditure across wealth quintiles was more than the increase in the likelihood of health service utilization.
The primary purpose of this paper was to evaluate the CHE risk in the case of measles contraction, independent of the measles vaccination status. This exercise showed that there was substantial variation in CHE risk across regions and wealth quintiles, which indicated the potential benefit of vaccination, if it was introduced sufficiently and equally across the country. However, as the vaccination coverage varies substantially across different groups in Nigeria, the actual benefit of vaccination on CHE risk will vary substantially, which could be evaluated in the future study.
This study has some limitations. First, there were data constraints, including the lack of local and recent data on measles prevalence and incidence, mortality and morbidity burden, measles-related OOP costs and associated time losses, and care-seeking and health service utilization for measles treatment. Therefore, we referred to past studies or made assumptions. Future work should focus on obtaining more accurate data so that the estimates of CHE risks could be more accurate. Second, we did not consider the correlation between the severity of disease and financial impoverishment. For example, the poor have the low health service utilization because of budget constraints, and they might utilize the health services only when the disease symptom is severe. In this case, the wealth level of households might be correlated with the medical costs of treatment.
Conclusion
The risk of experiencing CHE conditional on being infected with measles in Nigeria varied across regions and wealth quintiles. While the richest wealth quintile has almost no risk of CHE, the poorest wealth quintile faces higher risk of CHE, over 10%. Northeast and northwest regions face the highest risk of CHE among all the size regions. These results indicate that enhancing the vaccination coverage among the poorest households and in the northern regions has the potential to mitigate the overall CHE risk of measles and reduce the financial inequality across subgroups.
Disclosure statement
No potential conflict of interest was reported by the author.
Additional information
Funding
References
- Patel MK, Goodson JL, Alexander JP, Kretsinger K, Sodha SV, Steulet C, Gacic-Dobo M, Rota PA, McFarland J, Menning L, et al. Progress toward regional measles elimination—worldwide, 2000–2019. Morbidity Mortality Weekly Rep. 2020;69(45):1700. doi:10.15585/mmwr.mm6945a6.
- World Health Organization. Global measles outbreaks. 2021 [accessed 2021 Aug 3]. https://www.cdc.gov/globalhealth/measles/data/global-measles-outbreaks.html.
- Thompson KM, Odahowski CL. The costs and valuation of health impacts of measles and rubella risk management policies. Risk Anal. 2016;36(7):1357–4. doi:10.1111/risa.12459.
- Bloom DE, Canning D, Weston M. The value of vaccination. World Econ. 2005;6:15–16.
- Ehreth J. The global value of vaccination. Vaccine. 2003;21(7–8):596–600. doi:10.1016/S0264-410X(02)00623-0.
- Ozawa S, Clark S, Portnoy A, Grewal S, Brenzel L, Walker DG. Return on investment from childhood immunization in low-and middle-income countries, 2011–20. Health Aff. 2016;35(2):199–207. doi:10.1377/hlthaff.2015.1086.
- Ayieko P, Akumu AO, Griffiths UK, English M. The economic burden of inpatient paediatric care in Kenya: household and provider costs for treatment of pneumonia, malaria and meningitis. Cost Eff Resour Alloc. 2009;7:3. doi:10.1186/1478-7547-7-3.
- Griffiths UK, Dieye Y, Fleming J, Hajjeh R, Edmond K. Costs of meningitis sequelae in children in Dakar, Senegal. Pediatr Infect Dis.
- Chang AY, Riumallo-Herl C, Perales NA, Clark S, Clark A, Constenla D, Garske T, Jackson ML, Jean K, Jit M, et al. The equity impact vaccines may have on averting deaths and medical impoverishment in developing countries. Health Aff. 2018;37(2):316–24. doi:10.1377/hlthaff.2017.0861.
- World Health Organization. Measles: key facts. 2019. https://www.who.int/news-room/fact-sheets/detail/measles.
- World Health Organization. Estimation of unit costs for general health services: updated WHO-CHOICE estimates technical background report. 2011 [accessed 2021 Jul Mar 2011. http://www.who.int/choice/cost-effectiveness/inputs/health_service/en/.
- Memirie ST, Sisay Metaferia Z, Norheim OF, Levin CE, Verguet S, Arne Johansson K. Household expenditures on pneumonia and diarrhoea treatment in Ethiopia: a facility-based study. BMJ Global Health. 2017;2(1):e000166. doi:10.1136/bmjgh-2016-000166.
- Olumide AO, Shmueli A, Omotade OO, Adebayo ES, Alonge TO, Ogun GO. Economic costs of terminal care for selected non-communicable diseases from a healthcare perspective: a review of mortality records from a tertiary hospital in Nigeria. BMJ Open. 2021;11(4):e044969. doi:10.1136/bmjopen-2020-044969.
- Ezeoke OP, Onwujekwe OE, Uzochukwu BS. Towards universal coverage: examining costs of illness, payment, and coping strategies to different population groups in southeast Nigeria. Am J Trop Med Hyg. 2012;86(1):52. doi:10.4269/ajtmh.2012.11-0090.
- Zimmermann M, Frey K, Hagedorn B, Oteri AJ, Yahya A, Hamisu M, Mogekwu F, Shuaib F, McCarthy KA, Chabot-Couture G. Optimization of frequency and targeting of measles supplemental immunization activities in Nigeria: a cost-effectiveness analysis. Vaccine. 2019;37(41):6039–47. doi:10.1016/j.vaccine.2019.08.050.
- Nigeria National Bureau of Statistics (NBS). Living Standards Survey 2018-2019. 2019. https://microdata.worldbank.org/index.php/catalog/3827.
- Riumallo-Herl C, Chang AY, Clark S, Constenla D, Clark A, Brenzel L, Verguet S. Poverty reduction and equity benefits of introducing or scaling up measles, rotavirus and pneumococcal vaccines in low-income and middle-income countries: a modelling study. BMJ Global Health. 2018;3(2):e000613. doi:10.1136/bmjgh-2017-000613.
