ABSTRACT
The coronavirus disease 2019 (COVID-19) pandemic has had substantial impacts, including disruptions in routine vaccinations. In Taiwan, COVID-19 was relatively controllable, and the reduction in routine vaccinations was not profound. The impact of the pandemic on vaccination remained unclear. We collected vaccination uptake data at our hospital and analyzed the weekly trends of different vaccines. We calculated the monthly number of vaccinations and compared consumption before and during the COVID-19 pandemic (year 2019 vs years 2020 and 2021). Except for self-paid pneumococcal conjugate vaccines (PCV13), a mild (14.6%, p < .001) monthly decrease in government-funded routine vaccination and a moderate (28.2%, p = .018) monthly decrease in self-paid vaccination were observed during the COVID-19 pandemic. Interestingly, an unexpected surge of PCV13 vaccination occurred with a 355.8% increase. The shortage of COVID-19 vaccines and the potential benefits of PCV13 against COVID-19 may have contributed to this surge. In conclusion, our study found an obvious disruption of vaccination rates in Taiwan during the COVID-19 epidemic. However, an increase in PCV13 vaccination was also observed, and the important role of the infodemic was emphasized.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic fueled by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in widespread threats and impacts.Citation1,Citation2 As of 30 November 2021, there were more than 250 million infected people and approximately 5 million deaths.Citation1 A substantial impact on routine vaccination was also observed, raising global concerns about the potential risks of other vaccine-preventable diseases.Citation3–5 Lockdowns, the collapse of the medical system, the availability of vaccination clinics and the fear of gathering in public areas may have contributed to this reduction in routine vaccinations. More than 90% of countries experienced disruptions of medical services and vaccination to some extent.Citation4,Citation6 A 19.8% reduction in measles-mumps-rubella vaccination (MMR) was observed in England in early 2020.Citation7 Compared with the same period in previous years, a 21.5% decline in noninfluenza childhood vaccine doses was reported in Michigan in 2020.Citation8 An obvious decline of 52.5% in routine vaccination was observed in Pakistan during the pandemic.Citation9 Briefly, the disruption of vaccination was a common and important phenomenon during the COVID-19 pandemic.
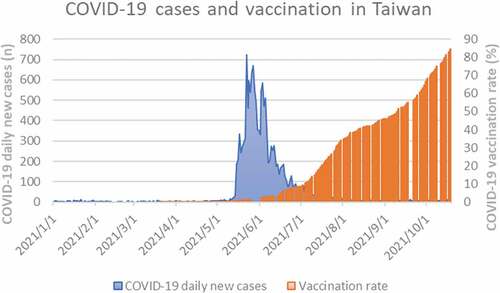
Several aggressive strategies related to COVID-19 have been implemented in Taiwan since early 2020, and the situation is relatively controllable.Citation10,Citation11 As of 30 April 2021, there were 1128 confirmed cases (47 cases per million residents).Citation1 COVID-19 vaccines made by AstraZeneca were introduced in Taiwan in March 2021. However, the COVID-19 vaccines were not widely available, and acceptance of vaccination against SARS-CoV-2 was not high initially.Citation12 The uptake of the vaccine remained low, with only 0.24% of the population vaccinated with the first dose as of late April 2021 (). An unexpected surge developed with a seven-fold increase (8511 confirmed cases, 357 cases per million residents) within one month in May 2021, resulting in public anxiety. People rushed into medical units for COVID-19 vaccines, but a shortage of vaccines was an important issue. Most people were unable to receive vaccination during the epidemic. Some countries donated COVID-19 vaccines to Taiwan to help control the epidemic, including Japan, the United States, Lithuania, Slovakia, and the Czech Republic. Vaccinations against COVID-19 have increased rapidly since July 2021, and the coverage of the first dose reached 50% by September 2021. As public anxiety developed during the epidemic, people looked for surrogate vaccinations against COVID-19 due to the COVID-19 vaccine supply shortage and the perceived risk of infection. Meanwhile, a study was published in mid-March 2021 that observed a lower risk of COVID-19 in individuals with pneumococcal conjugate vaccination (PCV13).Citation13 This article was reported in the mass media, and Taiwanese medical authorities agreed with the benefits of PCV13 vaccination. However, they noted that further studies were required to confirm the findings and clarify the underlying mechanisms, and that there was no need to receive self-paid PCV13 during the epidemic. However, people who were unable to receive COVID-19 vaccination surged into hospitals for self-paid PCV13 and the stock of PCV13 was rapidly exhausted. The adequacy of vaccine supply became an important concern during the COVID-19 pandemic.
Taiwan has a unique national health insurance program characterized by broad coverage of residents and most childhood vaccinations are government-funded. Briefly, there are five levels of medical care units in Taiwan, including medical centers, regional hospitals, local hospitals, private clinics, and public health centers. Childhood vaccinations are provided in all medical units and the record of vaccination is uploaded in the national immunization registration information system. The vaccine coverage rate is high and the national vaccination rate ranges from 90.9% to 99.3% before the COVID-19 pandemic.Citation14 As the epidemic continued and became more serious, stricter infection control measurements were implemented by the government and hospitals, including mask-wearing, social distancing, temporary closure of schools and restaurants, and prohibition of hospital visits since mid-May 2021.Citation15 The lockdown was not executed, and hospitals and local clinics continued to provide medical services. However, people were afraid of becoming infected in hospitals and avoided hospital visits. There was a substantial decrease in unnecessary hospital visits and vaccinations, but the degree of reduction was not investigated. Therefore, we conducted this retrospective hospital-based study to explore the impact of COVID-19 on vaccinations in Taiwan during the COVID-19 pandemic and the epidemic surge in 2021, including self-paid PCV13 vaccinations.
Methods
Study design and data collection
Our study was approved by the Institutional Review Board of the MacKay Memorial Hospital, Taipei, Taiwan (approval number 20MMHIS140e) and conducted in Hsinchu MacKay Memorial Hospital, a regional hospital with approximate 500 beds in north Taiwan. First, we extracted the daily new cases of confirmed COVID-19 in Taiwan and the COVID-19 vaccination rate to demonstrate the epidemiology of COVID-19 in Taiwan.Citation1 Furthermore, we retrospectively collected various vaccine consumption data from our hospital between 1 January 2019 and 18 October 2021 and compared the trends of vaccine uptake. We investigated both government-funded vaccines and self-paid vaccines, including pneumococcal vaccines (13-valent conjugate vaccine, PCV13; and 23-valent polysaccharide vaccine, PPSV23); diphtheria and tetanus toxoid with acellular pertussis, inactivated polio, and Haemophilus influenzae type b vaccine (DTaP-Hib-IPV); tetanus, diphtheria toxoids, acellular pertussis, and inactivated polio vaccine (Tdap-IPV); tetanus, diphtheria toxoids, and acellular pertussis vaccine (Tdap); hepatitis B vaccine (HBV); hepatitis A vaccine (HAV); Japanese encephalitis vaccine (JE); varicella vaccine (VR); measles, mumps, and rubella vaccine (MMR); rotavirus vaccine (Rotarix and Rotateq); human papillomavirus vaccine (HPV); and zoster vaccine (zoster). The daily consumption of each vaccine was extracted and analyzed. Since the COVID-19 pandemic initiated in early 2020 and we compared the monthly vaccine uptake for individual vaccine in different years. Furthermore, the first confirmed case was identified on 20Jan2020 and we divided the study into two periods: pre-pandemic (January 2019 to December 2019) and pandemic (January 2020 to September 2021) periods. We calculated and compared the monthly vaccine uptake of the two periods. We summarized the uptake of individual vaccines and then compared the monthly uptake of self-paid PCV13 vaccines, all government-funded vaccines (NIP vaccines), and all self-paid vaccines. Furthermore, to investigate the impact of the COVID-19 surge in 2021, we also compared the monthly vaccine uptake in pre-2021 surge period (January 2019 to April 2021) and 2021 surge period (June 2021 to September 2021).
Statistical analyses
For comparing the monthly uptake of vaccines in different years, one-way Analysis of Variance (ANOVA) was applied. Independent t tests were used to compare monthly vaccine uptake in the pre-pandemic and pandemic periods. A p value less than 0.05 was considered to indicate statistical significance. The prevalence of confirmed cases and the uptake of vaccines were plotted using Microsoft Office, version 2019 (Microsoft Corp, New Mexico, USA). Linear regression analyses were performed using the equation of linear trend estimation, y=αx+ß. The R2 values were calculated, which represented the degree of dispersion between individual data and the regression line. A higher R2 value indicated lower discrepancies between data and a more reliable fitted regression line. We used SPSS, version 23.0 (IBM Corp, Armonk, NY, USA) for statistical analyses.
Results
Epidemiology of COVID-19 and COVID-19 vaccine uptake
As of 18 October 2021, 16,337 confirmed cases of COVID-19 were diagnosed in Taiwan (). A surge of confirmed cases developed between 15 May 2021 and 3 July 2021 (more than 50 cases per day). The vaccine rate was 0.78% on 15 May 2021 and 9.55% on 2 July 2021. A rapid increase in the vaccination rate has occurred since July 2021, and the vaccine rate for the first dose was 84.7% as of 18 October 2021.
Impact of COVID-19 on vaccine uptake
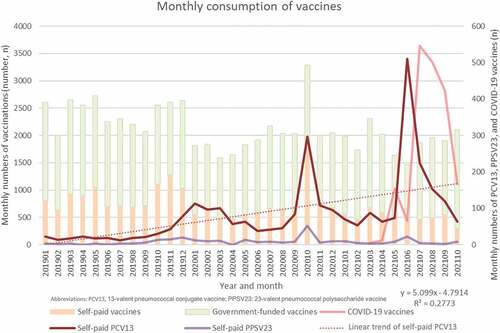
In total, there were 18,617, 15,745, and 26,399 vaccinations at our hospital in 2019, 2020, and 2021, respectively. We summarized the monthly vaccine uptake of individual vaccines in Supplementary . Furthermore, we plotted the monthly uptake of vaccines in ; a substantial reduction of routine childhood vaccine uptake was observed since January 2020 and the vaccine uptake recovered after April 2020 with a peak in October 2020. Following the COVID-19 surge in 2021, there was a gradual decline in vaccine uptake since March 2021, and vaccine uptake recovered after July 2021. A rapid increase in COVID-19 vaccine uptake since July 2021 was also observed. The monthly vaccine uptake in different years was summarized in and significant differences were observed in several government-funded vaccines after COVID-19 pandemic: all NIP vaccines, PCV13, HBV, VR, MMR, and JE. Self-paid vaccines were also impacted, including all self-paid vaccines, RV5, and Tdap. Furthermore, summarizes the comparison of monthly vaccine uptake in the pre-pandemic and pandemic periods. Significant reductions of both NIP and self-paid vaccines were observed in the pandemic period (NIP vaccines: −14.6%, p < .001; self-paid vaccines: −28.2%, p = .018). Significant decreases of government-funded PCV13, VR, MMR, JE and self-paid RV5 and Tdap were noted. A significant increase of HBV and both government-funded and self-paid PCV13 were disclosed. We further compared the monthly vaccine uptake in pre-2021surge period with 2021 surge period. A mild decrease in NIP vaccines (8.9%) and a moderate decrease in self-paid vaccines (35.2%) were observed during the epidemic period. There was a statistically significant decrease in rotateq (27.5%, p = .002) and JE (40.2%, p = .023) vaccination. Nonsignificant decreases in RV1, HPV9, HAV, Tdap, HBV, DTaP-Hib-IPV, VR, MMR, and Tdap-IPV vaccination were also observed. A nonsignificant increase in HBV and self-paid VR vaccination were also noted. There were no statistically significant differences in the uptake of other vaccines.
Table 1. Monthly vaccine uptake in different years.
Table 2. Monthly vaccine uptake in pre-pandemic/pandemic periods and pre-2021 surge/2021 surge periods.
Surge of PCV13 uptake
shows a gradual decline in routine vaccine uptake since the COVID-19 pandemic, including government-funded PCV13 (−25.7%, p < .001, ). However, uptake of the self-paid PCV13 increased during the study period (355.8% increase, p < .001). Meanwhile, a journal article was published on 9 March 2021, and the potential benefits of PCV13 against COVID-19 were reported in the mass media starting in late May 2021, when COVID-19 vaccines were unavailable. Interestingly, there was a surge in PCV13 vaccination beginning in May 2021 (y = 0.599x-4.7914, R2 = 0.2773). As a result, the inventory of PCV13 ran out quickly in mid-June-2021. Comparing the monthly uptake before April 2021 and after June 2021, a nonsignificant increase in PCV13 vaccination was observed (306.5% increase, p = .122; ).
Discussion
A disruption of routine vaccination during the COVID-19 epidemic was common: a mild reduction in NIP vaccines (14.6%) and a moderate reduction in self-paid vaccines (28.2%) were observed during the pandemic. The impact of the COVID-19 pandemic on vaccination was substantial, and the risks of contracting vaccine-preventable diseases was an important concern during the pandemic. Interestingly, a surge of PCV13 vaccination was observed (355.8% increase of self-paid PCV13), reinforcing the power of mass media as a double-edged sword during the COVID-19 pandemic.
The impact of the COVID-19 pandemic on health care was extensive and universal. The WHO Pulse survey showed a 23% global reduction in medical services and a 70% partial or complete disruption of routine vaccination.Citation4 The disruption of vaccination during the COVID-19 pandemic has been reported in many areas, and we summarized some reports in .Citation7–9−Citation16–22 The magnitude of reduction varied in different countries with different disease prevalence, infection control measurements, study populations, vaccine strategies, vaccine feasibility, and medical resources. A wide range of reductions was observed, and our findings were consistent with previous studies. The observed reduction was attributed to a combination of factors, such as disruptions of medical services or vaccination practices, lockdowns, school closures and stay-at-home policies, insufficient supplies of personal protective equipment and medical staff and health care provider shortages.Citation4,Citation6,Citation23,Citation24 In Piché-Renaud’s study investigating reasons for the disruption, 78% of patients and 27% of staff were concerned about the risk of contracting COVID-19.Citation22 Seven percent of medical units lacked medical staff for illness or self-isolation, and 9% encountered vaccine shortages or supply issues. The period of the Taiwan epidemic was short, and no strict lockdown was implemented. The supply of vaccines and personal protective equipment were sufficient. Most reductions in vaccination resulted from the perceived risk of contracting COVID-19 in public areas or hospitals. In short, the disruption of vaccination was an important issue during the COVID-19 pandemic, and our study showed similar results.
Table 3. Disruption of immunizations in some countries during COVID-19 pandemic.
It is clear that there may be collateral damage due to the disruption of routine vaccinations. A resurgence of vaccine preventable diseases may occur and trigger another wave of health threats after the COVID-19 pandemic.Citation25,Citation26 Furthermore, even during the pandemic, coinfection and superinfection are not uncommon, although some diseases are vaccine-preventable. Various pathogens causing coinfection or superinfection have been reported in patients with COVID-19, including viruses, bacteria, and fungi.Citation27,Citation28 Coinfection or superinfection may complicate diagnosis and treatment and increase disease severity and mortality.Citation27,Citation29 A meta-analysis showed that the pooled incidences of coinfection and superinfection were 19% and 24%, respectively.Citation28 Some coinfections involved diseases that were vaccine-preventable, and a disruption of vaccination could exacerbate the clinical course and result in poor outcomes. For example, PCV13 is highly effective against invasive pneumococcal disease (IPD). Compared with IPD monoinfection, patients with coronavirus and pneumococcal coinfection had a 7.8-fold higher fatality rate.Citation30 The role of coinfection is crucial during the COVID-19 pandemic, and a disruption of vaccination can be hazardous.
In contrast to the decline in routine vaccinations, the reverse pattern of a surge in PCV13 uptake caught our attention. The initial name of COVID-19 was “Wuhan pneumonia” and people believed in the protective efficacy of vaccines against “pneumonia”, such as pneumococcal vaccines. Furthermore, Lewnard’s study played an important role in the surge of PCV13 vaccinations during the Taiwanese epidemic; they found a significantly reduced risk of COVID-19 diagnosis, hospitalization, and mortality in individuals with PCV-13 (adjusted hazard ratios: 0.65, 0.68, and 0.68, respectively).Citation13 The benefits against COVID-19 were not observed in individuals with PPSV23 vaccination. Protection against virus-associated community-acquired pneumonia in subjects with PCV13 vaccination was reported in a previous study.Citation31 Virus-bacteria interactions and alterations of subsequent host immune responses may contribute to the observed reduced risks. However, concomitant nasal colonization and host-bacteria immune interaction may not be the only reason for the protection provided by non-COVID-19 vaccines. A similar lower risk of COVID-19 was also reported in people with Bacillus Calmette–Guérin vaccine (BCG) and MMR vaccination.Citation32,Citation33 Trained immunity incited by BCG and other live vaccines may explain the beneficial off-target effects. Vaccine-induced metabolic and epigenetic changes will enhance innate immunity and reduce the risk of subsequent SARS-CoV-2 infection. Briefly, PCV13 vaccination is effective against pneumococcal infection and colonization and may have collateral benefits with other viral infections, such as SARS-CoV-2. Further studies are warranted to confirm the benefits and clarify the underlying mechanisms.
In addition to reverse increase of self-paid PCV13 uptake, a significant increase of government-funded HBV is also noted (35.3%, p < .001). The possible explanation may be reduced delivery in local clinics and the immediate HBV vaccination after birth. The vaccination schedule of HBV is birth, 1-month-old, and 6-month-old in Taiwan and the first dose is administered within 48 hours after birth.Citation14 Hsinchu MacKay Memorial Hospital is also famous for the gynecology & obstetrics, and pediatrics. During the pandemic, medical services of delivery provided at local clinics may be reduced due to insufficient personal protective equipment and diagnostic testing. Delivery will be performed at hospitals and neonates will receive the first dose of HBV at hospitals. The second and third doses of HBV may be shifted to local clinics or postponed as other government-funded vaccines. However, further details and nationwide surveillance are required to investigate the impact of COVID-19 on HBV vaccination and underlying mechanism.
During the pandemic, public anxiety was common, and we are inundated with information, both true and false. An infodemic is too much information during a disease outbreak, which leads to confusion and risk-taking behaviors.Citation34,Citation35 As the use of social media, the internet and digitization become widespread, information spread rapidly, and the infodemic had a considerable impact.Citation35,Citation36 False information regarding disease transmission, treatment, and vaccination spread and caused harmful outcomes. Confusion of “Wuhan pneumonia” and “pneumococcal vaccination” and reports of the potential collateral benefits of PCV13 vaccination for COVID-19 spread rapidly, and we observed a surge in PCV13 uptake. There was an insufficient COVID-19 vaccine supply during the epidemic, and people were anxious about getting COVID-19. Although the report claimed there was no need to urgently receive PCV13 vaccination during the pandemic, people rushed to medical units for PCV13 vaccinations. Our study indicated the role of the infodemic, a double-edged sword for vaccination.
Strengths and limitations of the study
The strength of our study is that it is the first study to investigate the impact of COVID-19 on routine vaccinations in Taiwan. We also observed an interesting surge of PCV13 vaccinations. However, our study was subject to some limitations. First, there are many important factors affecting vaccine uptake and supply. A rapid consumption of self-paid PCV13 vaccines resulted in an exhaustion of storage in mid-June 2021. Therefore, the trend of an increase was sharp and obvious, but the difference was not statistically significant during the epidemic surge in 2021. Second, our study was conducted in a local hospital, and people might avoid hospitals and receive routine vaccination at local clinics. Children may receive routine vaccination in different medical units, consumption of vaccine numbers is not exactly representative of vaccination coverage. Furthermore, Taiwan experienced a short epidemic period, and the long-term impact remains unclear. Nationwide surveillance with vaccine coverage and long-term follow-up is valuable. Finally, the prevalence of COVID-19, government policy, medical resources, vaccine recommendations, coverage rates, and supply changed rapidly, and the impact of COVID-19 on routine vaccinations varied in different situations.
Conclusion
In conclusion, our study found a mild (14.6%) monthly decrease in government-funded routine vaccinations and a moderate (28.2%) monthly decrease in self-paid vaccinations in Taiwan during the COVID-19 pandemic. Similar trends are observed in the short period of epidemic surge in 2021. Interestingly, we observed a surge in self-paid PCV13 uptake following the report of potential collateral protection of PCV13 against COVID-19. Further studies are warranted to elucidate the impact of infodemics as double-edged swords for routine vaccination.
Authors’ contributions
NCC, KHL, CCC, and CYL involved in conceptualization; NCC, KHL, CCC, SYH, SLW, CJW, HHK, and CYL collected data. KHL, HC, CHL, and CYL performed analysis; SYH, SLW, YLT and CYL were responsible for methodology and validation; NCC wrote the first draft. NCC, KHL, and CCC contributed to this work equally. All authors have read and agreed to the published version of the manuscript.
Ethical approval and consent to participate
It was approved by the Institutional Review Board of the MacKay Memorial Hospital, Taipei, Taiwan (approval number, 20MMHIS140e).
Acknowledgement
Our manuscript has been edited for English language, grammar, punctuation, and spelling by American Journal Experts, the editing brand of Research Square Company. We thank everyone’s efforts to combat COVID-19.
Data availability statement
The datasets used for the analysis in the present study are available from the corresponding author on reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Our World in Data. Coronavirus Pandemic (COVID-19). [accessed 2021 Nov 30]. https://ourworldindata.org/coronavirus
- WHO. Coronavirus disease (COVID-19): Vaccines. [accessed 2021 Nov 30]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Causey K, Fullman N, Sorensen RJD, Galles NC, Zheng P, Aravkin A, Danovaro-Holliday MC, Martinez-Piedra R, Sodha SV, Velandia-González MP, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398:522–9. doi:10.1016/S0140-6736(21)01337-4.
- WHO. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 2020 Aug 27.
- Feldman AG, O’-Leary ST, Danziger-Isakov L. The risk of resurgence in vaccine-preventable infections due to coronavirus disease 2019-related gaps in immunization. Clin Infect Dis. 2021;73:1920–23. doi:10.1093/cid/ciab127.
- Harris RC, Chen Y, Côte P, Ardillon A, Nievera MC, Ong-Lim A, Aiyamperumal S, Chong CP, Kandasamy KV, Mahenthiran K, et al. Impact of COVID-19 on routine immunisation in South-East Asia and Western Pacific: disruptions and solutions. Lancet Regional Health – Western Pacific. 2021;10. doi:10.1016/j.lanwpc.2021.100140.
- McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, Bates C, Parry J, Walker JL, Scott JA, Smeeth L, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020;25. doi:10.2807/1560-7917.ES.2020.25.19.2000848.
- Bramer CA, Kimmins LM, Swanson R, Kuo J, Vranesich P, Jacques-Carroll LA, Shen AK. Decline in child vaccination coverage during the COVID-19 pandemic — Michigan Care Improvement Registry, May 2016-May 2020. Am J Transplant. 2020;20:1930–31. doi:10.1111/ajt.16112.
- Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, Soundardjee R, Dharma VK, Shah MT, Abdullah S, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 2020;38(45):7146–55. doi:10.1016/j.vaccine.2020.08.019.
- Chang CM, Tan TW, Ho TC, Chen CC, Su TH, Lin CY. COVID-19: Taiwan’s epidemiological characteristics and public and hospital responses. PeerJ. 2020;8:e9360. doi:10.7717/peerj.9360.
- Chen CC, Tseng CY, Choi WM, Lee YC, Su TH, Hsieh CY, Chang C-M, Weng S-L, Liu P-H, Tai Y-L, et al. Taiwan Government-guided strategies contributed to combating and controlling COVID-19 pandemic. Front Public Health. 2020;8:547423. doi:10.3389/fpubh.2020.547423.
- Chiu NC, Chi H, Tu YK, Huang YN, Tai YL, Weng SL, Chang L, Huang DTN, Huang F-Y, Lin C-Y, et al. To mix or not to mix? a rapid systematic review of heterologous prime–boost covid-19 vaccination. Expert Rev Vaccines. 2021;20:1211–20. doi:10.1080/14760584.2021.1971522.
- Lewnard JA, Bruxvoort KJ, Fischer H, Vx H, Lr G, Jódar L, Gessner BD, Tartof SY. Prevention of COVID-19 among older adults receiving pneumococcal conjugate vaccine suggests interactions between Streptococcus pneumoniae and SARS-CoV-2 in the respiratory tract. J Infect Dis. 2021. doi:10.1093/infdis/jiab128.
- Taiwan Centers for Disease Control. Vaccine-Preventable diseases control. [accessed 2021 Nov 30]. https://www.cdc.gov.tw/En/Category/ListPage/4TFK95zgsUb9k8XYFFj2Dw
- Chiu NC, Chi H, Tai YL, Peng CC, Tseng CY, Chen CC, Tan BF, Lin C-Y. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective National Epidemiological Surveillance Study. J Med Internet Res. 2020;22:e21257. doi:10.2196/21257.
- DeSilva MB, Haapala J, Vazquez-Benitez G, Daley MF, Nordin JD, Klein NP, Henninger ML, Williams JT, Hambidge SJ, Jackson ML, et al. Association of the COVID-19 pandemic with routine childhood vaccination rates and proportion up to date with vaccinations across 8 US health systems in the vaccine safety datalink. JAMA Pediatr. 2021;176(1): 68–77. doi:10.1001/jamapediatrics.2021.4251.
- Khan A, Chakravarty A, Mahapatra J. Impact of COVID-19 pandemic on childhood immunization in a tertiary health-care center. Indian J Community Med. 2021;46:520–23. doi:10.4103/ijcm.IJCM_847_20.
- Mansour Z, Arab J, Said R, Rady A, Hamadeh R, Gerbaka B, Bizri AR. Impact of COVID-19 pandemic on the utilization of routine immunization services in Lebanon. PLoS One. 2021;16(2):e0246951. doi:10.1371/journal.pone.0246951.
- Moreno-Montoya J, Ballesteros SM, Rojas Sotelo JC, Bocanegra Cervera CL, Barrera-López P, De la Hoz-Valle JA Impact of the COVID-19 pandemic on routine childhood immunisation in Colombia. Arch Dis Child. 2021;107(3): e4. doi:10.1136/archdischild-2021-321792.
- Nuzhath T, Ajayi KV, Fan Q, Hotez P, Colwell B, Callaghan T, Regan AK. Childhood immunization during the COVID-19 pandemic in Texas. Vaccine. 2021;39(25):3333–37. doi:10.1016/j.vaccine.2021.04.050.
- Silveira MF, Tonial CT, Goretti KMA, Teixeira AMS, Hallal PC, Maria BMA, Horta BL, Hartwig FP, Barros AJD, Victora CG, et al. Missed childhood immunizations during the COVID-19 pandemic in Brazil: Analyses of routine statistics and of a national household survey. Vaccine. 2021;39(25):3404–09. doi:10.1016/j.vaccine.2021.04.046.
- Wang Q, Xiu S, Yang L, Han Y, Huang J, Cui T, et al. Delays in routine childhood vaccinations and their relationship with parental vaccine hesitancy: a cross-sectional study in Wuxi, China. Expert Rev Vaccines. 2022;21(1):135–143. doi:10.1080/14760584.2022.2008244.
- Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, Burey S, Feldman M, Morris SK. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario, Canada. Vaccine. 2021;39:4373–82. doi:10.1016/j.vaccine.2021.05.094.
- Dinleyici EC, Borrow R, Safadi MAP, van Damme P, Munoz FM. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum Vaccin Immunother. 2021;17:400–07. doi:10.1080/21645515.2020.1804776.
- Chiappini E, Parigi S, Galli L, Licari A, Brambilla I, Angela Tosca M, Ciprandi G, Marseglia G. Impact that the COVID-19 pandemic on routine childhood vaccinations and challenges ahead: a narrative review. Acta Paediatr. 2021;110:2529–35. doi:10.1111/apa.15949.
- Patel Murthy B, Zell E, Kirtland K, Jones-Jack N, Harris L, Sprague C, Schultz J, Le Q, Bramer CA, Kuramoto S, et al. Impact of the COVID-19 pandemic on administration of selected routine childhood and adolescent vaccinations — 10 U.S. Jurisdictions, March–September 2020. MMWR Morb Mortal Wkly Rep. 2021;70:840–45. doi:10.15585/mmwr.mm7023a2.
- Chen X, Liao B, Cheng L, Peng X, Xu X, Li Y, Hu T, Li J, Zhou X, Ren B, et al. The microbial coinfection in COVID-19. Appl Microbiol Biotechnol. 2020;104:7777–85. doi:10.1007/s00253-020-10814-6.
- Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS One. 2021;16:e0251170. doi:10.1371/journal.pone.0251170.
- He S, Liu W, Jiang M, Huang P, Xiang Z, Deng D, Chen P, Xie L. Clinical characteristics of COVID-19 patients with clinically diagnosed bacterial co-infection: a multi-center study. PLoS One. 2021;16(4):e0249668. doi:10.1371/journal.pone.0249668.
- Amin-Chowdhury Z, Aiano F, Mensah A, Sheppard CL, Litt D, Fry NK, Andrews N, Ramsay ME, Ladhani SN. Impact of the Coronavirus disease 2019 (COVID-19) pandemic on invasive pneumococcal disease and risk of pneumococcal coinfection with severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2): prospective National Cohort Study, England. Clin Infect Dis. 2021;72:e65–e75. doi:10.1093/cid/ciaa1728.
- Huijts SM, Coenjaerts FEJ, Bolkenbaas M, van Werkhoven CH, Grobbee DE, Bonten MJM. The impact of 13-valent pneumococcal conjugate vaccination on virus-associated community-acquired pneumonia in elderly: exploratory analysis of the CAPiTA trial. Clin Microbiol Infect. 2018;24:764–70. doi:10.1016/j.cmi.2017.10.006.
- Curtis N, Sparrow A, Ghebreyesus TA, Netea MG. Considering BCG vaccination to reduce the impact of COVID-19. Lancet. 2020;395:1545–46. doi:10.1016/S0140-6736(20)31025-4.
- Yengil E, Onlen Y, Ozer C, Hambolat M, Ozdogan M. Effectiveness of booster measles-mumps-rubella vaccination in lower COVID-19 infection rates: a retrospective cohort study in Turkish Adults. Int J Gen Med. 2021;14:1757–62. doi:10.2147/IJGM.S309022.
- Merchant RM, Lurie N. Social media and emergency preparedness in response to Novel Coronavirus. Jama. 2020;323:2011–12. doi:10.1001/jama.2020.4469.
- Zarocostas J. How to fight an infodemic. Lancet. 2020;395:676. doi:10.1016/S0140-6736(20)30461-X.
- Briand SC, Cinelli M, Nguyen T, Lewis R, Prybylski D, Valensise CM, Colizza V, Tozzi AE, Perra N, Baronchelli A, et al. Infodemics: a new challenge for public health. Cell. 2021;184:6010–14. doi:10.1016/j.cell.2021.10.031.