ABSTRACT
Widespread vaccine uptake is critical for ending the COVID-19 pandemic. As public health officials focus on overcoming vaccine hesitancy, simultaneously boosting hope may be equally important in the US. We analyzed data from an online cross-sectional survey conducted in June 2021. Participants were 11,955 US adults (ages 18–83) of various ethnicities, living in urban and rural settings. Of these, 71.3% had some college education. Mean age was 32.3 years and 72.4% reported being vaccinated against COVID-19. Main measures were COVID-19 self-reported vaccination status (vaccine uptake), vaccine hesitancy (Adult Vaccine Hesitancy Scale), and hope (Adult Hope Scale). The US grand mean hope score fell within the low-hope range. COVID-19 vaccine uptake was positively associated with hope, even after adjusting for vaccine hesitancy, gender, age, ethnicity, income, and urban vs. rural residence. The strong relationship between hope, vaccine confidence and vaccine uptake persisted across US populations at risk for low vaccine uptake. Our mediation analysis revealed that, for every unit increase in hope, the probability of being vaccinated went up by 5% points. Of this association, 52% was not mediated by vaccine hesitancy, but rather through a direct pathway from hope to vaccine uptake. Mediation analyses of US populations at risk of low vaccine uptake revealed similar findings. Hope may play an important role in vaccine uptake by reducing vaccine hesitancy and by directly enhancing vaccine uptake. Especially in populations at risk of low vaccine uptake, vaccine interventions that boost hope may augment public health efforts to increase US vaccination rates.
Introduction
More than a year has passed since the first vaccines for COVID-19 were approved, yet less than 70% of adults in the United States are fully vaccinated and less than 50% have received a booster shot.Citation1 Failure to achieve herd immunity (75–85% of the population vaccinated) raises the risk of new variants emerging and new surges of infection and disease.Citation2
In parallel, researchers have documented a “crisis of despair” in the US, that pre-dates the pandemic.Citation3 This growing sense of hopelessness in the US has been compounded by a series of “cascading collective traumas”, including an economic recession, ongoing race-driven social unrest and weather-relateddisasters.Citation4 The mental health consequences of these stresses profoundly affect American society Citation4 and raise the question: could a national deficit of hope be impeding vaccine uptake and fueling vaccine hesitancy in the US?
Hope has been defined as a cognitive variable that results from both an individual’s sense of agency and their perception of available pathways toward achieving their goals.Citation5 Individual differences in hope can be measured using validated tools that demonstrate internal consistency and test-retest reliability.Citation5,Citation6 Other research suggests that hope is a flexible state - one that can be influenced by external inputs, such as entertainment media exposures and education.Citation7,Citation8 As a cognitive counterpart of planning, hope is also a critical component of initiative-taking and research suggests that hope boosts cognitive resolve, even in the face of uncertainty.Citation9
While no large-scale studies to date have documented the relationship between hope, vaccine hesitancy and vaccine uptake in the US, an exploratory study conducted in Israel investigated the emotional drivers of vaccine uptake and identified hope as the only factor associated with willingness to be vaccinated.Citation10
Especially for US populations at risk of low vaccine uptake (including Black Americans, those living in rural areas, low-income and low-education groups)Citation11 vaccine hesitancy may not be the main barrier to uptake—nor the easiest to overcome.Citation12,Citation13 Black Americans, for example, may have legitimate cause for vaccine-related uncertainty, given the history of unethical research involving communities of color in the US.Citation2,Citation12 For Americans with low incomes or no college education, low levels of hope may thwart messages from the public health community that are too narrowly focused on reducing vaccine hesitancy.Citation2,Citation3,Citation14
Sociodemographic differences in vaccine uptake aggravate existing disparities in COVID-19 morbidity and mortality.Citation2,Citation13,Citation15 This translates into a pressing need for studies exploring both the factors that contribute to vaccine hesitancy as well as those that may influence vaccine uptake directly, across all demographic groups. While some researchers have explored lack of trust as a predictor of vaccine hesitancy and low vaccine uptakeCitation16 no theoretical frameworks have linked vaccine hesitancy and vaccine uptake with hope.
As a result, the public health community may be underestimating the importance of harnessing emotions—especially positive emotions, like hope, in the decision-making process that leads to vaccine uptake.Citation14 Here, we explore the direct and indirect relationships between hope, vaccine hesitancy and vaccine uptake, in a large sample of US adults.
Methods
Study setting and participants: Eligible participants (adult volunteers aged 18 years and older living in the US), were recruited and their informed consent obtained via the Prolific Academic Research Platform (ProA: https://www.prolific.co/). ProA is an online research subject pool designed to support scientific research. Participants enroll on the platform and they are then recruited at random from a large user base and paid a small amount for their time participating. The platform maintains strict ethical standards around the recruitment, consenting and privacy of study participants.Citation17
Data for this cross-sectional survey was collected in June 2021, via the web survey platform Gorilla (www.gorilla.sc). Gorilla is a secure, online survey distribution and data collection platform, which has been used for secure data collection in prior studies.Citation18,Citation19
Our survey was nested within a randomized controlled trial, described elsewhere.Citation20 The trial aimed to explore the effect of vaccine promotion media on vaccine hesitancy.
Variables: Participants in our cross-sectional study responded to the adult Vaccine Hesitancy Scale (aVHS)Citation21 a validated scale for measuring COVID-19 vaccine hesitancy in adults.Citation22 The scale was adapted from the validated 14-item WHO SAGE Vaccine Hesitancy Scale to focus on adult COVID-19 vaccinations.Citation23 Participants also responded to the validated Adult Hope Scale.Citation5,Citation6 This scale consists of 12 items, of which 4 are distractors. Of the 8 items that contribute to the overall hope score, 4 items assess “agency” (the respondent’s belief that they are capable of achieving a positive outcome) and the remaining 4 items assess “pathways” (the respondent’s belief that there are available pathways leading to a positive outcome.) Theoretically, participants can score between 8–64, although, prior research suggests that scores generally fall between 25–64, with “low hope” defined as a score below 46.Citation24 As recommended in the literature, we referred to this scale as “The Future Scale” in our survey.Citation6
Scoring: We aggregated the 14 vaccine hesitancy items on a scale of 1–5, with lower scores corresponding to greater vaccine hesitancy. We present these scores as “vaccine confidence” (ie: the complement of vaccine hesitancy). We calculated participants’ hope levels by aggregating the 8 Adult Hope Scale items on a scale of 1–8.Citation24,Citation25 Participants self-reported sociodemographic data, including ethnicity, income, rural or urban residence and education. Participants also self-reported vaccination status by responding ‘yes’ or ‘no’ to the statement: “I have already been vaccinated against COVID-19 with one of the new available vaccines.” This approach to measuring vaccine uptake is supported by the documented high validity of self-reported vaccination status.Citation26
Analysis: We present exploratory analysis of the scale variables described above using means and standard deviations. For the Hope score, we calculated the grand mean for all participants included in the sample. To demonstrate the gap, we calculated the mean values by vaccination uptake status for all participants and by different self-reported sociodemographic sub-groups (as described above). The categorical variables, including vaccine uptake, are presented as frequencies and percentages. We used regression models with adjustment for covariates including income <50k, Black ethnicity, rural residence, and no college education. Binary logit regression was used for models which had vaccine uptake as their outcome, and linear regression was used for those with hope and vaccine confidence as their outcome.
To determine the mediation effect of hope on vaccine uptake, through the pathway of vaccine confidence, we added vaccine confidence as a predictor to the regression model of vaccine uptake on hope. The reduction in the effect estimates between the unadjusted and adjusted model was inferred as the magnitude of the indirect effect mediated by vaccine confidence. We express these results respectively as regression coefficients, with 95% confidence intervals. All analysis were performed in R (R Core Team, 2018). We performed our mediation analysis and generated the plot using the “Mediation” package in R.Citation27
Ethics: We obtained ethics approval from the Stanford University IRB on January 12th, 2021, protocol # 59503.
Results
Of 12,000 adults who volunteered and consented to participate, 11,955 completed all parts of the surveys (a high 99.6% response rate typical of online studies conducted on ProA).Citation17 The mean age of participants was 32.3 years (SD 10.1), 10.4% of participants identified as Black American, 46.0% male, 71.3% had at least some college education and 23.5% lived in a rural area. Overall, 72.4% answered “yes” to the COVID-19 vaccine uptake question, indicating that they had received at least one dose of the COVID-19 vaccine. The mean vaccine confidence score in our study was 54.9 (SD 9.4). Of all participants, 27.6% indicated that they were unwilling to accept a COVID-19 vaccination, closely aligning with US vaccine hesitancy data collected one year prior to our study, in June 2020.Citation21
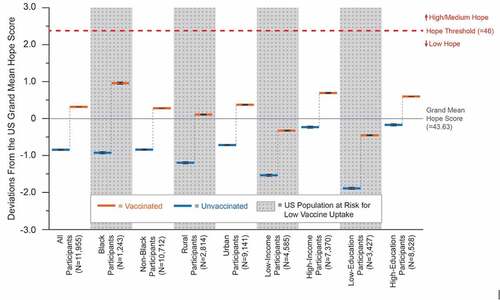
The grand mean hope score was 43.63 (SD 5.6), which falls within the “low-hope” range, as defined by Snyder et al. 2002.Citation24 Across demographic groups, the mean hope scores of unvaccinated participants were significantly lower than those of vaccinated participants. illustrates deviations from the grand mean hope score by demographic group and vaccination status.
Regression analyses revealed that hope was significantly positively associated with vaccine uptake (Beta coefficient: 0.18, 95%CI − 0.12 to 0.23). Hope was also significantly positively associated with vaccine confidence (0.74, 95%CI − 0.51 to 0.97). As anticipated, vaccine confidence was significantly positively associated with vaccine uptake (0.17, 95%CI − 0.16 to 0.17). Surprisingly, we observed a strong independent association between hope and vaccine uptake (0.12, 95%CI − 0.05 to 0.19), even after adjustment for vaccine confidence. presents the regression analyses of hope on vaccine confidence and vaccine uptake by demographic group.
Table 1. Regression analyses of hope on vaccine confidence and vaccine uptake.
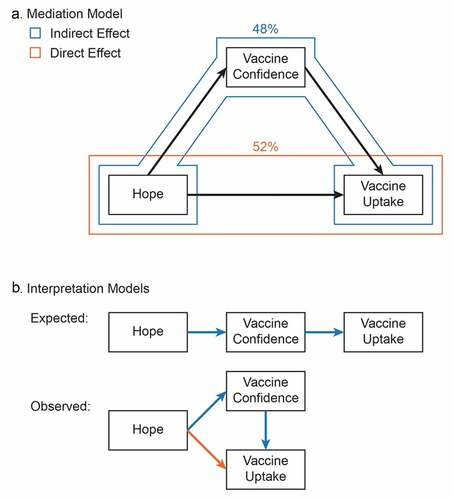
Our mediation analysis revealed that for every point increase in mean hope score, likelihood of vaccine uptake went up by 5.4 points across all participants. Of this, 2.8 points (52% of the total effect) was attributable to the direct pathway between hope and vaccine uptake. shows the mediation analysis model of hope with vaccine confidence and vaccine uptake.
Discussion
This study is the first of its kind attempting to quantify the association between hope, vaccine hesitancy and vaccine uptake in the US. We observed significant associations between hope, vaccine hesitancy and vaccine uptake, as well as a generally low grand mean hope score across all US participants. This finding contrasts with the significantly higher grand mean hope score observed across a similar number of adult participants (N = 12,000) in China, who were involved in the parallel sister trial.Citation20 The mean hope score in this parallel study population fell within the medium hope score range. (F. Yu, personal communication, December 2021).
Low hope has been highlighted as a serious problem in the US, pre-dating the pandemic. Researchers have suggested that the current crisis of despair could be fueling nativist politics, vulnerability to misinformation and skepticism about science.Citation3 In the context of a documented US crisis of despairCitation3 and a series of cascading collective traumas (an economic recession, race-driven social unrest and weather-related disasters)Citation4 these observations support our hypothesis that low hope could be a significant impediment to universal vaccine uptake in the US.
Contrary to our initial expectation—that the relationship between hope and vaccine uptake would be almost entirely mediated by vaccine hesitancy—we found that more than half of this relationship resulted from a direct pathway between hope and vaccine uptake. As a cognitive counterpart to planning, researchers suggest that hopefulness can liberate us from beliefs that reduce our confidence in the world around us, threatening to leave us in a state of “numbed inaction”Citation9
The direct pathway between hope and vaccine uptake observed in this study aligns with calls for additional research on the emotional drivers of vaccine uptakeCitation14 as well as the potential for integrating these drivers into innovative, globally scalable, public health messages.Citation28 Prior research underscores the need for more nuanced public health messages.Citation29 This could include messages that lie at the intersection of health communication and entertainment, that harness narratives to activate positive emotions like hope, and could prove to be powerful tools for promoting vaccine uptake.Citation7,Citation14,Citation30,Citation31
Limitations of this study include a study population that was more educated, and slightly younger than the general US population, likely because this was an online survey. The low grand mean hope score we observed in this study population, (juxtaposed with the observation that less educated participants had lower hope scores) could suggest that hope in the general US population may, in fact, be even lower than the grand mean score documented here. If this is the case, boosting hope could be an even more urgent public health goal.
Secondly, we did not measure other factors associated with vaccine uptake, including political affiliations, religious beliefs or trust in science, although the relationship between hope and trust has been documented.Citation32
Finally, while our study included participants from all 50 US states, the number of participants from each state was not proportional to the population of each state. This suggests that our sample may not have been perfectly representative of the entire US population. However, the percentage of participants who indicated that they were unwilling to be vaccinated (27.6% in our study) was comparable to prior US vaccine hesitancy data (27.3% in a June 2020 US survey).Citation21 This alignment suggests that, with regard to vaccine hesitancy, our sample may well be representative of the US public.
The strong association between hope and vaccine uptake, observed in this study suggests that foundational public policy efforts to boost hope and address the crisis of despair in the US, could yield powerful, concurrent improvements in vaccine uptake. Additionally, the documented interconnections between hope and trustCitation32 and between trust in science and vaccine confidenceCitation33suggest that boosting all of these could work synergistically in favor of improved vaccine uptake. Hope has already been identified as an important therapeutic target in other health fields that, when boosted, can influence patient outcomes.Citation34
Public health interventions, such as innovative, scalable social media campaignsCitation28 and narrative, hope-inspiring approaches from the entertainment industryCitation7 have the potential to boost hope in the US. Our findings suggest that deploying hope-inspiring interventions, like these, could trigger a highly desirable “side effect” in the US: improved vaccine uptake. Especially for populations at risk of low vaccine uptake, broadening the focus of our vaccine promotion efforts—beyond standard factual messages aimed at reducing vaccine hesitancy through the provision of information—may yield a new generation of more equitable and effective interventions. Such interventions would contribute to a win-win situation for the US and the world as we work together to definitively end the COVID-19 pandemic.
Disclosure statement
No potential conflict of interest was reported by the author(s)
Additional information
Funding
References
- Prevention CfDCa. COVID data tracker. U.S. Department of Health & Human Services. [accessed 2021 Dec 1]. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people
- Hildreth JE, Alcendor DJ. Targeting COVID-19 vaccine hesitancy in minority populations in the US: implications for herd immunity. Vaccines. 2021;9(5):489. doi:10.3390/vaccines9050489.
- Graham C. America’s crisis of despair: A federal task force for economic recovery and societal well-being. Brookings Blueprints for American Renewal & Prosperity. 2021 [accessed 2021 Dec 1]. https://www.brookings.edu/research/americas-crisis-of-despair-a-federal-task-force-for-economic-recovery-and-societal-well-being/
- Silver RC, Holman EA, Garfin DR. Coping with cascading collective traumas in the United States. Nat Hum Behav. 2021;5(1):4–5. doi:10.1038/s41562-020-00981-x.
- Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C, Harney P, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. 1991;60(4):570.
- Snyder C, Harris C, Anderson J, Holleran S, Irving L, Sigmon S, Yoshinobu L, Gibb J, Langelle C, Harney P. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. 2007;60:570–85. doi:10.1037/0022-3514.60.4.570.
- Prestin A. The pursuit of hopefulness: operationalizing hope in entertainment media narratives. Media Psychol. 2013;16(3):318–46. doi:10.1080/15213269.2013.773494.
- Kortte KB, Stevenson JE, Hosey MM, Castillo R, Wegener ST. Hope predicts positive functional role outcomes in acute rehabilitation populations. Rehabil Psychol. 2012;57(3):248. doi:10.1037/a0029004.
- Pettit P. Hope and its place in mind. Ann Am Acad Pol Soc Sci. 2004;592(1):152–65. doi:10.1177/0002716203261798.
- Mayer Y, Etgar S, Shiffman N, Bloch Y, Mendlovic S, Lurie I. Hope as a predictor for COVID-19 vaccine uptake. Hum Vaccines Immunother. 2021;17:1–5.
- Al‐amer R, Maneze D, Everett B, Montayre J, Villarosa AR, Dwekat E, Salamonson Y. COVID‐19 vaccination intention in the first year of the pandemic: a systematic review. J Clin Nurs. 2022;31(1–2):62–86. doi:10.1111/jocn.15951.
- Corbie-Smith G. Vaccine hesitancy is a scapegoat for structural racism. Am Med Assoc. 2021; 2: e210434-e210434.
- Madorsky TZ, Adebayo NA, Post SL, O’-Brian CA, Simon MA. Vaccine distrust: a predictable response to structural racism and an inadequate public health infrastructure. Am Public Health Assoc. 2021;111:S185–S188. doi:10.2105/AJPH.2021.306411.
- Chou WS, Budenz A. Considering Emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–22. doi:10.1080/10410236.2020.1838096.
- Siegel M, Critchfield-Jain I, Boykin M, et al. How the coronavirus lockdown impacts the impoverished in India. J Racial Ethnic Health Disparities. 2021;8:1–14. doi:10.1007/s40615-020-00905-5.
- Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med. 2020;173(12):964–73. doi:10.7326/M20-3569.
- Palan S, Schitter C. Prolific. ac—a subject pool for online experiments. J Behav Exp Finance. 2018;17:22–27. doi:10.1016/j.jbef.2017.12.004.
- Vandormael A, Adam M, Greuel M, Gates J, Favaretti C, Hachaturyan V, Bärnighausen T. The effect of a wordless, animated, social media video intervention on COVID-19 prevention: online randomized controlled trial. JMIR Public Health Surveillance. 2021;7(7):e29060. doi:10.2196/29060.
- Vandormael A, Hachaturyan V, Adam M, Favaretti C, Gates J, Bärnighausen T. Effect of a story-based, animated video to reduce added sugar consumption: a web-based randomized controlled trial. J Global Health. 2021:11. doi:10.7189/jogh.11.04064.
- Chen S, Forster S, Yang J, Yu F, Jiao L, Gates J, Wang Z, Liu H, Chen Q, Geldsetzer P, et al. Animated, video entertainment-education to improve vaccine confidence globally during the COVID-19 pandemic: an online randomized controlled experiment with 24,000 participants. Trials. 2022;23(1):1–10. doi:10.1186/s13063-022-06067-5.
- Akel KB, Masters NB, Shih S-F, Lu Y, Wagner AL. Modification of a vaccine hesitancy scale for use in adult vaccinations in the United States and China. Hum Vaccines Immunother. 2021;17(8):2639–46. doi:10.1080/21645515.2021.1884476.
- Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, Perez S, Rosberger Z. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36(5):660–67. doi:10.1016/j.vaccine.2017.12.043.
- Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165–75. doi:10.1016/j.vaccine.2015.04.037.
- Snyder CR, Shorey HS, Cheavens J, Pulvers KM, Adams VH III, Wiklund C. Hope and academic success in college. J Educ Psychol. 2002;94(4):820. doi:10.1037/0022-0663.94.4.820.
- Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL. Development and validation of the state hope scale. J Pers Soc Psychol. 1996;70(2):321–35. doi:10.1037//0022-3514.70.2.321.
- Siegler AJ, Luisi N, Hall EW, Bradley H, Sanchez T, Lopman BA, Sullivan PS. Trajectory of COVID-19 vaccine hesitancy over time and association of initial vaccine hesitancy with subsequent vaccination. JAMA Netw Open. 2021;4(9):e2126882. doi:10.1001/jamanetworkopen.2021.26882.
- Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014;59(5).
- Adam M, Barnighausen T, McMahon SA. Design for extreme scalability: a wordless, globally scalable COVID-19 prevention animation for rapid public health communication. J Global Health. 2020 ;10(1):010343. doi:10.7189/jogh.10.010343.
- Cataldi JR, O’-Leary ST. Addressing vaccine concerns: a hopeful path forward for vaccine confidence. Am Public Health Assoc. 2021;111:556–58. doi:10.2105/AJPH.2020.306150.
- Lazic A, Zezelj I. A systematic review of narrative interventions: lessons for countering anti-vaccination conspiracy theories and misinformation. Public Underst Sci. 2021;30(6):644–70. doi:10.1177/09636625211011881.
- Vilaythong AP, Arnau RC, Rosen DH, Mascaro N. Humor and hope: can humor increase hope? Humor Int J Humor Res. 2003;16(1). doi:10.1515/humr.2003.006.
- McGeer V. Trust, hope and empowerment. Australas J Philos. 2008;86(2):237–54. doi:10.1080/00048400801886413.
- Sturgis P, Brunton-Smith I, Jackson J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. 2021;5:1–7.
- Corn BW, Feldman DB, Wexler I. The science of hope. Lancet Oncol. 2020;21(9):e452–e459. doi:10.1016/S1470-2045(20)30210-2.