ABSTRACT
Getting vaccinated against SARS-CoV-2 lowers the risk of severe infections. In Hong Kong, two vaccine types are offered: CoronaVac by Sinovac Biotech (Sinovac), and Comirnaty by BioNTech-Fosun Pharma (BioNTech). However, a low vaccine uptake rate is observed. This study primarily aimed to determine the population of medical students who underwent COVID-19 vaccination, and to identify factors associated with their decision on timing and vaccine type. Current medical students from The University of Hong Kong (HKU) were invited to participate in this cross-sectional survey study from 16 September to 31 December 2021. The main outcome measures were the vaccine uptake rate, primary reasons for vaccine-seeking behavior, vaccine hesitancy and vaccine preference, as well as information sources. All questions were of a multiple-choice format, with a free response option for questions pertaining to reason exploration. Overall, 214 medical students participated in the study, with all questionnaires analyzed. Amongst the 98.1% that completed 2 doses, 93.4% selected BioNTech and 6.6% selected Sinovac. Significant associations were observed between year groups and vaccine timing (p = 0.00989). The primary reason to seek vaccination was immunity against COVID-19 (53.5%), while the fear of potential side effects (61.6%) accounted for vaccine hesitancy. The BioNTech vaccine was favored for its higher efficacy against COVID-19 (87.4%). Information sources were mainly from HKU professors (64.6%) and social media (59.9%). The study found a high vaccine uptake rate amongst medical students, contrary to the situation observed in the Hong Kong general population at the time of the study.
New knowledge added by this study
This is the first paper evaluating the attitudes and behaviours of Hong Kong medical students towards the COVID-19 vaccine.
High COVID-19 vaccine uptake observed amongst HKU medical students, with a predilection towards Comirnaty by BioNTech-Fosun Pharma for the first and second dose.
Clinical medical students are more likely to get their COVID-19 vaccine earlier than preclinical medical students.
Immunity against COVID-19 was the most compelling reason for students to get vaccinated, whilst fears over side effects was the main reason for vaccine hesitancy.
Implications for clinical practice or policy
Policies promoting mandatory vaccinations and greater inconvenience for those unvaccinated are useful and should be strictly enforced to further increase vaccination uptake.
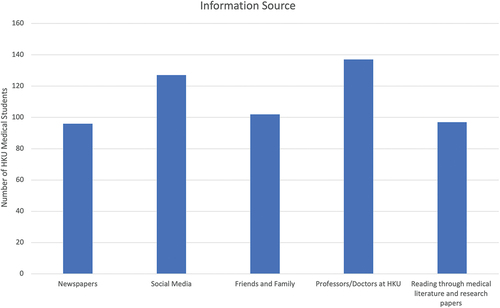
More regulation has to be put in place on vaccine-related information obtained from social media.
Introduction
The primary objective of this study is to determine the COVID-19 vaccine uptake rate among Hong Kong medical students, and to identify factors associated with their decision on timing and type of vaccination received. The secondary objectives include: exploring underlying reasons associated with vaccination-seeking behaviors, vaccine hesitancy and vaccine preferences; identifying resources utilized by medical students for COVID-19 vaccine information.
This study is cross-section questionnaire surveyed targeted toward HKU medical students. In summary, 214 medical students had participated in the surveys, with 98.1% of the students having received 2 doses, at the time completing the survey. A large majority of the students (93.4%) who had received the vaccines opted for the BioNTech vaccine. Significant associations have been observed for reasons to receive the vaccine and factors affecting the decision for different vaccine manufacturers, which will be discussed in detail in the Discussion.
Vaccination plays an important role in combating the latest global pandemic caused by the COVID-19 virus. One proposed major benefit of a high vaccination rate across a local population is herd immunity, which is defined as ‘the indirect protection of unvaccinated persons, whereby an increase in the prevalence of the vaccine immunity prevents circulation of infectious agents in unvaccinated susceptible populations.Citation1 There are widespread effects that are posed by a suboptimally controlled outbreak. Not only are infectious diseases the leading cause of death worldwide, they can also have detrimental economic consequences. In fact, economic models have shown that the a decrease in global GDP can be as great as 27% during a coronavirus outbreak, with social distancing measuring being the leading cause for the economic downturn.Citation2 A previous study had suggested that a COVID-19 vaccine with 100% efficacy was reported to require an uptake rate of over 60 to 72%, while a vaccine with 80% efficacy requires a higher uptake rate of 75 to 90%, in order for herd immunity to take effect.Citation3 The University of Hong Kong’s (HKU) Professor KY Yuen, a world-renowned virologist, had also determined an uptake rate of over 90% as necessary to control the pandemic in Hong Kong.Citation4
However, the latest developments have suggested that herd immunity against COVID-19 is unlikely to be achievable. Major reasons reported include a decline in vaccine effectiveness with time, and reports of newly emerged variants infecting recovered and vaccinated individuals.Citation5,Citation6 Nonetheless, vaccination still plays a vital role in reducing the risk of a severe disease, hospitalization and death.Citation5,Citation7
The Hong Kong government has purchased 22.5 million vaccines for a population of 7.5 million people, equally from 3 manufacturers—Sinovac Biotech (Sinovac), BioNTech-Fosun Pharma (BioNTech) and AstraZeneca-Oxford in December 2020.Citation8 However, shipments from AstraZeneca-Oxford were suspended over vaccine-induced thrombotic thrombocytopenia.Citation9 Getting vaccinated is encouraged but not mandated by Hong Kong law, and the individual has free choice to determine the type of vaccine, Sinovac or BioNTech, received.
Vaccine hesitancy, one of the top ten threats to global health, is defined as a delay in acceptance or refusal of vaccination despite availability of vaccination services.Citation10,Citation11 Previous studies reported a growing prevalence of vaccine refusal in recent years,Citation12 with a similar phenomenon observed in Hong Kong.
As of the 5th of January 2022, 75% of the Hong Kong population have received at least one shot of the vaccine. This is lower than many high-income regions, including the United Kingdom at 76%, China at 87% and Singapore at 88%.Citation13,Citation14
Reasons for vaccine hesitancy include the perceived low risk of contracting the disease, perceived low efficacy of the vaccine, fear of side effects, and low perceived trustworthiness of vaccine manufacturers.Citation15 A global survey conducted in two separate time frames observed improvements in attitudes toward COVID-19 vaccination in most countries, contrary to the situation in Hong Kong.Citation15 Specifically, vaccine acceptance decreased significantly amongst the working population between the local first and third wave.Citation16 A questionnaire study recorded vaccine acceptance to be 34.5%, significantly lower than the government target of 70%.Citation16,Citation17 This could be attributable to fears over safety and side effects of the vaccines, exacerbated by concurrent negative reports from clinical trials.Citation18 Additionally, it is observed that a period of reduced intention to receive COVID-19 vaccination coincides with a decreased number of confirmed cases.Citation19
Healthcare workers are important role models, having a duty to promote vaccine uptake through their own vaccine-seeking behavior.Citation20 Unfortunately, during the period of mid-March to late-April 2020, only 63% of Hong Kong nurses reported an intention to receive the vaccine,Citation19 lower than the reported world average of 74%.Citation21 Although medical students are not technically healthcare workers, these expectations should nonetheless be applied, supporting the fundamental science underpinning the medical profession. Currently, there is no local data indicating the magnitude of acceptance for vaccines by medical students. A population-based study has projected acceptance rates to be 40% amongst people aged 18 to 24, but this cannot reflect actual attitudes of a niche sub-population of medical students.Citation22
With the latest outbreak ongoing since January 2022, the fifth wave in this locality, it is clear that the pandemic is not under adequate control. It will be useful to understand the reasons for vaccine hesitancy amongst these students, if present, as the implications identified from this cohort may also be applicable to the broader group of healthcare workers. Such knowledge would be able to guide public health measures taken to bolster the vaccination rates among this subpopulation, which may have the knock-on effects of increasing vaccine acceptance in the region as a whole.
Methods
Study design
This was a cross-sectional questionnaire survey. All current HKU medical students were invited to participate during the enrollment period from 16 September 2021 to 31 December 2021. The link to the online questionnaire was posted on Facebook and WhatsApp groups used exclusively by all HKU medical students. The online survey was hosted on the Google Forms® platform, in English, requiring 3 minutes to complete. It was anonymous in nature, with the last 5 digits of the student identification number collected to prevent duplication and miscounts. The collected results are only reviewed by members of the research team, ensuring data confidentiality.
Participant consent was obtained with the button click of “I agree” on the online consent form, replacing the need of the participant’s signature. After completion of the survey, participants were encouraged to share the questionnaire link with their colleagues on social media platforms, increasing survey enrollment. A snowball sampling strategy was employed to finalize the study.
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Ref: UW 21–618).
Data collection
The data collection period, 16 September 2021 to 31 December 2021, commenced after the availability of the vaccines to the public, at 26 February 2021 and 10 March 2021 for Sinovac and BioNTech respectively.Citation23 Vaccination priority was given to citizens over the age of 60 and healthcare staff, inclusive of medical students. For analysis purposes, vaccines received before June 2021 were deemed ‘early’, while vaccines received during or after June 2021 were ‘delayed.
Additionally, the HKU medical curriculum is hierarchically tiered into two groups: Clinical and Preclinical students. Preclinical students consist of students from Year 1, 2 and 3 with minimal clinical exposure, while Clinical students consist of students from Year 4, 5 and 6 with regular patient interaction and hospital visits.
The questionnaire (Appendix 1) comprised a total of 24 questions in 5 sections: 1) consent form 2) demographics 3) vaccinated 4) unvaccinated 5) information sources. However, not all sections were attempted, with the individual being redirected to various sections depending on their responses.
For section 1, the participant’s signature of consent would be replaced with the button click of “I agree”. Section 2 collects data of the participant’s gender, year group, last 5 digits of the student identification number, and vaccination status. Vaccinated participants were directed to Section 3, exploring further into reasons for vaccination and possible hesitation, as well as vaccine preference. If unvaccinated, participants would be directed to Section 4, evaluating intention and preference for vaccination, and reasons for hesitancy. Finally, all participants would indicate their information sources in Section 5, to account for their observed attitudes and behavior. All questions are of a multiple-choice (MCQ) format, with a free response option for questions pertaining to reason exploration.
Sample size
The online sample size calculator powered by Survey Monkey® was used to calculate the minimum sample size. With 1527 HKU medical students, the minimum sample size generated by the software was 174 for a 95% confidence interval and 7% margin of error, with no follow-up conducted.
Statistical analysis
Statistical analyses were performed using Microsoft Excel, Version 16.56. Descriptive statistics, inclusive of frequencies and percentages, were used to analyze the demographic characteristics of participants. Chi-squared tests were performed to compare the mean vaccine timing against demographic categories such as year group, gender and vaccine type. A p-value of less than 0.05 indicated statistical significance.
Results
With a minimum sample size of 174, our study exceeded the target and recruited 214 medical students. This constituted 14% of all 1527 HKU medical students. All 214 responses were analyzed, with none excluded due to incomplete or missing data. There were 111 (51.9%) males and 103 (48.1%) females participating, with the majority from Year 5 (53.3%). Additionally, 210 (98.1%) students have completed 2 doses, with 199 (93.4%) selecting BioNTech and 14 (6.6%) selecting Sinovac, as shown in .
Table 1. Table of demographics and vaccination status.
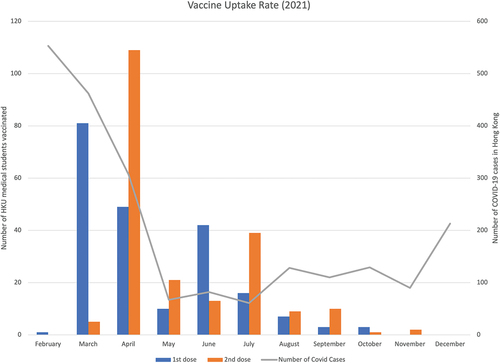
The Sinovac and BioNTech vaccines were available from 26 February 2021 and 10 March 2021 respectively,Citation23 with priority given to citizens over the age of 60 and healthcare staff, inclusive of medical students. Detailed vaccine uptake rate is reflected on , documenting numbers of both first and second doses administered in the different months of 2021. March saw the greatest number of medical students receiving their first dose at 81 (38.2%), and April recorded the highest number of medical students receiving their second dose at 109 (51.2%).
Figure 1. Vaccine uptake rate amongst HKU medical students against total number of COVID-19 cases in Hong Kong.
Amongst respondents, there is a significant association between year group and vaccine timing, specifically, 71% of clinical year students and 51.9% of preclinical year students underwent early vaccination (p = 0.00989). No significant association was found between vaccine timing against gender (p = 0.269) or vaccine type (p = 0.459).
Underlying reasons associated with vaccine hesitancy
Overall, 66.2% received early vaccination, while 33.8% received delayed vaccination. Of the minority of medical students that sought delayed vaccination, the fear of potential serious side effects (61.6%) was the most popular reason for vaccine hesitancy, followed by the desire to wait and assess outcomes of others who have received the vaccine (54.8%), and a busy work-study schedule (39.7%), as summarized in . One student reflected the “fear that vaccin(ation) will affect my mood when taking DSE (Diploma of Secondary Education)”.
Table 2. Table of underlying reasons associated with vaccine hesitancy.
Unvaccinated
Only 1 out of the 214 participants was unvaccinated. The Year 4 student expressed his intention to be vaccinated with Sinovac, with the main reason being the acquisition of a vaccine passport. His dominant reason for vaccine hesitancy is the fear over potential serious side effects.
Underlying reasons associated with vaccine preference
Out of the 199 medical students that opted for the BioNTech vaccine, 87.4% selected BioNTech primarily due to its higher efficacy against COVID-19. showcases other secondary reasons, including vaccine passports (71.2%) and it being offered at the HKU Community Vaccination Center (55.4%). “KY Yuen” and “recommendation by HKU professors” were recorded from the free responses, indicating the important role medical doctors play in influencing vaccine preference. The fact that only the BioNTech vaccine is offered at HKU vaccination centers is also a psychological push factor to receive this vaccine over others. One student reflected “other developed countries’’ decisions to utilize mRNA technology vaccines instead of inactivated viruses’, highlights the influence of global public health and political matters over vaccine preference.
Table 3. Table of underlying reasons associated with BioNtech selection.
Conversely, within the 14 medical students that selected Sinovac, 85.7% were aware of Sinovac’s lower efficacy.Citation24 When being asked of the reasons for the selection of Sinovac as tabulated in , 42.9% primarily preferred its inactivated virus technology, and 35.7% favored its fewer reported side effects. Notably, one student wrote “mRNA long term effects unknown” in the free response option.
Table 4. Table of underlying reasons associated with Sinovac selection.
Underlying reasons associated with vaccination-seeking behavior
summarizes reasons medical students adopt for vaccination. Immunity against COVID-19 was identified as the primary reason for vaccination in the majority of medical students (53.5%), with another significant 24.9% being most motivated by the Hospital Authority’s (HA) arrangement to exclude vaccinated students from mandatory COVID tests in clinical areas. The top 3 secondary reasons for vaccination include the contribution to herd immunity (61.9%), duty of a medical student (59.9%) and the fear of infecting others (58.4%). Free responses recorded “parental pressure” and “recommendation of HKUMED”, indicating a subtle role societal pressure plays into vaccination seeking behavior. “Hall requirements” indicates the effectiveness of mandatory measures to perpetuate vaccine seeking behavior. Similarly, in the hypothetical absence of weekly COVID testing mandated by HA, 13.2% of medical students reflected their refusal to get vaccinated.
Table 5. Table of underlying reasons associated with vaccination-seeking behavior.
Information sources
summarizes the sources medical students utilize to acquire information regarding the vaccines. The most popular source was via professors and doctors at HKU (64.6%), followed by social media (59.9%) and friends and family (48.1%).
Discussion
The novel finding of this study was the overwhelming preference toward the BioNTech vaccine amongst medical students in Hong Kong. Despite the earlier availability of the Sinovac Biotech vaccine, 93.4% (n = 199) of respondents chose to receive the BioNTech vaccination, with 87.4% (n = 174) of respondents citing a higher vaccine efficacy as the most important reason for their decision. This study also reported a high vaccination rate amongst medical students, with 98.1% (n = 210) of respondents receiving two doses of the vaccine by 31 December 2021. Only one individual has yet to receive any vaccination due to fears over potential side effects. Another significant discovery from this study was the difference in vaccine uptake behavior between clinical and preclinical students, with clinical year students opting to receive the vaccine at an earlier date compared to their preclinical colleagues. Furthermore, this study confirmed that external factors, such as vaccine availability, government regulations, and misinformation, play an important role in influencing vaccine acceptance.
The preference for vaccines with a higher efficacy shown in this study, is in accordance with results from other studies: Kreps et al. reported that American adults had a strong preference toward two-dose mRNA vaccines, over one-dose viral vector vaccines, when data on the vaccine’s superior efficacy was reported.Citation25 In a survey study conducted in France, Schwarzinger et al. found that public acceptance of COVID-19 vaccines increased as reported efficacy rises.Citation26 Borriello et al. reported that an efficacy is a major driver of choice amongst the Australian population.Citation27 This is consistent with the literature as an efficacy of 95% is cited for the BioNTech vaccine, and 65.9% for the Sinovac vaccine. Despite the lower efficacy rate, 6.5% of individuals (n = 14) opted for the Sinovac Biotech vaccine. 42.9% of these individuals (n = 6) cited a preference for the inactivated virus technology as the most important reason for choosing the Sinovac vaccine. A reduced side effect profile, when compared to the BioNTech vaccine, was the second most important reason for preferring the Sinovac vaccine; 35.7% of individuals (n = 5) share this opinion. The Community Vaccination Center at Ap Lei Chau Sports Center, organized by the medical faculty of the University of Hong Kong, formally commenced operations on 16 March 2021. The vaccination center, which prioritized medical students, solely administered the BioNTech vaccine, which may have influenced the decision of medical students to choose this vaccine over alternatives. Nearly 50% of respondents cited this as a reason for choosing the BioNTech vaccine over Sinovac. Other reasons for preferring BioNTech included vaccine passports, fewer reported side effects and preference for mRNA technology.
The difference in vaccine acceptance behaviors between preclinical and clinical year students could have different explanations. Firstly, clinical year students are required to attend clinical teaching sessions in hospitals, which increases the risk of contracting the COVID-19 virus. Secondly, clinical year students have a greater understanding of the importance of vaccination in developing immunity against the virus. Lucia et al. found that clinical year students in America were more likely to participate in a vaccine trial than their preclinical counterparts. Finally, the mandatory weekly COVID-19 testing, enforced by the Hospital Authority for unvaccinated medical students, provided a powerful incentive for students to get immunized; 13.2% of survey participants would have refrained from getting vaccinated had this regulation not passed. An additional 24.9% of survey respondents specified such an arrangement as the most important reason for getting vaccinated. The enforcement of daily, self-financed COVID-19 testing for unvaccinated medical students has positively influenced the vaccine seeking behavior of a substantial proportion of our cohort, which raises the issue of whether the government should follow suit to increase the societal vaccine uptake rate. Increased regulations on entertainment, for example, may incentivize more unvaccinated individuals to get immunized; improving the current vaccination rate, of at least one dose received, of 75%.
The vaccination uptake rate seen in our study corresponds with the initial availability of the vaccines in Hong Kong, as March saw the greatest number of individuals receiving their first dose: 38.2% (n = 81) of respondents. April saw the greatest number of individuals receiving their second dose, with 51.2% (n = 109) of respondents doing so. This coincides with the recommended 28 days between first and second dose for Sinovac Biotech, and at least 21 days for BioNTech. Due to packaging defects detected in a shipment of BioNTech-Fosun Pharma vaccines, the government suspended all BioNTech vaccinations on 26 March 2021, amidst safety concerns. Vaccination of the BioNTech vaccines, however, resumed on 5 April 2021, after thorough investigations discovered that the cause of the defect was attributed to poor transport conditions, as opposed to tampering of the production quality. This incident, in conjunction with the end-of-year university examinations, may explain the dip in vaccine uptake amongst medical students in the months of May and June.
Social media was listed as the second most cited source of information for our cohort of students, falling shortly behind recommendations from HKU teaching staff. With a greater proportion of individuals utilizing social media, these networking sites serve as a notable agent for the dissemination of information including the propagation of misinformation and fake news. Misinformation about vaccine safety, hypothetical political incentives, and exaggerated vaccine side effect profiles may negatively influence vaccine confidence. It is, therefore, of utmost importance that a greater emphasis is placed on reporting accurate information and dispelling misinformation.
This study contributes to the literature by reporting the different factors influencing vaccination amongst medical students in Hong Kong. These results should be interpreted with a broader body of knowledge to ultimately improve the vaccination rate amongst other healthcare professionals and the general population. Our findings have prompted us to recommend the implementation of new government regulations that would only allow vaccinated individuals to enjoy certain premises such as fitness centers, places of amusement and catering services. Implementing such an arrangement would increase the vaccination rate amongst the general population as a similar arrangement has proved effective amongst medical students.
Strengths and limitations
Firstly, participation is voluntary, resulting in a low response rate of 214/1527 (14%). Potential response and self-selection bias may be present, as students who have not received the vaccination would be less keen to participate. Additionally, collection of nonparticipation reasons was not possible. In our study population, the majority of the participants belonged to the Year 5 cohort, having an average age of 23 years, and an equal ratio of males and females. All Year 5 medical students in our population received the COVID-19 vaccination, with all but 1 student receiving the full two doses. Compared to the Hong Kong medical students national average, our population’s demographic characteristics are similar. However, no data is available on the national medical students’ uptake rate and doses received. Therefore, true attitudes and behaviors, and vaccination uptake rate amongst medical students could not be established. Specifically, our study might over-report the uptake rate amongst HKU medical students. However, our collected 214 responses exceed the minimum sample size calculated of 174, which decreases measurement error. A larger-than-minimum sample size can be seen as a strength of our study, and lowers effects of biasness.
Secondly, this study only evaluates HKU’s medical students, one out of the two medical schools in Hong Kong. Additionally, other healthcare professionals, ranging from nurses, allied health workers, and traditional Chinese medicine practitioners, were excluded. Future studies can include the whole plethora of healthcare professionals in order to represent the healthcare profession fully. On the other hand, attitudes and behavior evaluation on a homogenous group of healthcare workers, specifically medical students, could be considered as a strength of the current study.
Thirdly, factors accounting for hesitancy and uptake identified in this study are not generalizable to the general public. Medical students are a special subgroup, equipped with higher degrees of medical knowledge that are not commonly available amongst members of society. Furthermore, medical students receive priority to vaccinations, rid of potential long waiting times and booking difficulties. Thus, the privilege medical students possess through knowledge and increased accessibility, cannot be extrapolated to the general public.
Lastly, this study did not evaluate attitudes and behavior of receiving a third booster shot. The survey was designed and approved in September 2021, months before the government’s revised recommendation regarding the third booster shot on 23 December 2021.Citation28 It is useful for future studies to evaluate attitudes and behaviors pertaining to future booster shots.
Conclusion
To our knowledge, this is the first paper evaluating the attitudes and behaviors of Hong Kong medical students toward the COVID-19 vaccine. The study confirmed a high vaccine uptake rate amongst students, with a remarkable preference for the BioNTech Fosun Pharma vaccine. Clinical year students were more likely to get the vaccine earlier compared to their preclinical year colleagues, which can be attributed to their higher risk of exposure. This study revealed that immunity against the virus was the most compelling reason for students to get vaccinated, whilst fears over side effects were the prevailing sentiment for vaccine hesitancy. Ultimately, much still needs to be done to promote vaccine seeking behavior, and reduce the spread of misinformation, for the world to return to normalcy.
Author contributions
Concept or design: NTY Ngai
Acquisition of data: CCH Yip, JR Khoo
Analysis or interpretation of data: NTY Ngai, JR Khoo
Drafting of the manuscript: all authors
Critical revision of the manuscript for important intellectual content: S Sridhar
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Ethics approval
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Ref: UW 21–618). Participant consent was obtained with the button click of “I agree” on the online consent form, replacing the need of the participant’s signature.
Supplemental Material
Download PDF (233.7 KB)Acknowledgements
We would like to thank Dr Abigail Wright, Dr Harry Wu and Dr Julie Chen, Medical Ethics and Humanities Unit, Li Ka Shing Faculty of Medicine, The University of Hong Kong, for their support and endorsement for the study to be conducted in the faculty.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2074761.
Additional information
Funding
References
- Kim TH, Johnstone J, Loeb M. Vaccine herd effect. Scand J Infect Dis. 2011:683–8 doi:10.3109/00365548.2011.582247.
- Verikios G. The dynamic effects of infectious disease outbreaks: the case of pandemic influenza and human coronavirus. Socio-Econ Plan Sci. 2020;71:100898. doi:10.1016/j.seps.2020.100898.
- Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. The Lancet: Lancet Publishing Group; 2020. p. 1614–16.
- Microbiologist says HK needs 90% vaccination rate. RTHKHK; 2021.
- Andrews N, Tessier E, Stowe J, Gower C, Kirsebom F, Simmons R, Gallagher E, Thelwall S, Groves N, Dabrera G, et al. Duration of protection against mild and severe disease by Covid-19 vaccines. N Engl J Med. 2022 ;386(4):340–50. doi:10.1056/NEJMoa2115481.
- Wong RSY. COVID-19 vaccines and herd immunity: perspectives, challenges and prospects. Malays J Pathol. 2021;43:1777.
- Chemaitelly H, Tang P, Hasan MR, AlMukdad S, Yassine HM, Benslimane FM, Al Khatib HA, Coyle P, Ayoub HH, Al Kanaani Z, et al. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N Engl J Med. 2021;385(24):e83. doi:10.1056/nejmoa2114114.
- The Government of Hong Kong Special Administrative R. HKSAR government donates 7.5 million doses of AstraZeneca COVID-19 vaccine to COVAX facility. The Government of Hong Kong Special Administrative Region; Press Releases 2021.
- Pottegård A, Lund LC, Karlstad Ø, Dahl J, Andersen M, Hallas J, Lidegaard Ø, Tapia G, Gulseth HL, Ruiz PLD, et al. Arterial events, venous thromboembolism, thrombocytopenia, and bleeding after vaccination with Oxford-AstraZeneca ChAdox1-S in Denmark and Norway: population based cohort study. The BMJ. 2021;373. doi:10.1136/bmj.n1114.
- MacDonald NE, Eskola J, Liang X, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- Ten threats to global health in 2019. World health organisation; 2019.
- Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low- and middle-income countries: a systematic review. Int J Public Health: Birkhauser Verlag AG. 2015;60(7):767–80. doi:10.1007/s00038-015-0715-6.
- The Government of the Hong Kong Special Administrative R. Hong Kong Vaccination Dashboard
- Me RH, Rodés-Guirao L, Roser M, Beltekian D. Coronavirus pandemic (COVID-19). Our World in Data.
- Ipsos. Global attitudes : COVID-19 vaccines. 2021.
- Wang K, Wong ELY, Ho KF, et al. Change of willingness to accept covid-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in hong kong, china: repeated cross-sectional surveys. Vaccines. 2021;9(1):1–15. doi:10.3390/vaccines9010062.
- Cheung E. Coronavirus: finally, Hong Kong hit the 70 per cent vaccination mark. but does it matter now and should it be aiming for 90 or even 100? South China Morning Post; 2021.
- Mahase E. Covid-19: oxford researchers halt vaccine trial while adverse reaction is investigated. BMJ (Clinical Research Ed). 2020;369:m2612. doi:10.1136/bmj.m2612.
- Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi:10.1016/j.ijnurstu.2020.103854.
- Report of the sage working group on vaccine hesitancy. 2014.
- Ipsos. Global attitudes on a COVID-19 vaccine. 2020.
- Wong MCS, Wong ELY, Huang J, Cheung AWL, Law K, Chong MKC, Ng RWY, Lai CKC, Boon SS, Lau JTF, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–56. doi:10.1016/j.vaccine.2020.12.083.
- Hong J. BioNtech vaccine uptake jumps in Hong Kong as younger residents qualify. Bloomberg; 2021.
- A head-to-head comparison of the Sinovac and BioNTech vaccine. OT&P Healthcare; 2022.
- Kreps S, Kriner DL, Sallam M. Communication about vaccine efficacy and COVID-19 vaccine choice: evidence from a survey experiment in the United States. PLoS One. 2022;17(3):e0265011. doi:10.1371/journal.pone.0265011.
- Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi:10.1016/S2468-2667(21)00012-8.
- Borriello A, Master D, Pellegrini A, Rose JM. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2021 Jan 15;39(3):473–79. doi:10.1016/j.vaccine.2020.12.032.
- Joint Scientific Committees on Vaccine Preventable D, Emerging, Zoonotic D, Chief Executive’s expert advisory p. Recommendation for 3rd dose COVID-19 vaccination. Hong Kong goverment; 2021.