ABSTRACT
Introduction: This study aimed to investigate HPV vaccination intention among adult married women aged 27 to 45 years and its associated factors, and their spouse/partner’s influence on HPV vaccination decision-making.
Methods: This is a cross-sectional, questionnaire-based study. Study participants were recruited through simple random sampling of patients attending obstetrics and gynecology outpatient clinics in a university teaching hospital. Participants were selected based on a computer-generated list of a random list of patients attending the clinic.
Results: A total of 794 complete responses were received (response rate 88.2%). The mean age of the respondents was 32.2 years with a standard deviation (SD) of ±3.9 years.The vast majority (85.3%) would communicate with their spouse/partner with regard to HPV vaccination decision-making. Nearly 30% (over half were of the Malay ethnic group) perceived their spouse/partner would not consent to their HPV vaccination. Over half (54.9%) reported joint decision-making, and 9.1% (the majority of whom were Malay) reported that HPV vaccination was dependent on their spouse/partner’s decision. Intention to vaccinate against HPV was high (74.5%). Factors influencing HPV vaccination intention were spouse/partner’s consent to HPV vaccination (odds ratio [OR] = 4.51; 95% confidence interval [CI], 3.08–6.62), being a postgraduate student (OR = 4.55; 95% CI, 2.13–9.72 vs. unemployed/housewife), average household income MYR2000–4000 (OR = 2.09; 95%CI, 1.16–3.78 vs. below MYR2000), and an HPV-related knowledge score of 9–20 (OR = 1.60; 95% CI, 1.10–2.32 vs. score 0–8).
Conclusion: Findings highlight the importance of culture-centered interventions to enhance male partner’s awareness and support for the HPV vaccination of married women.
Introduction
The incidence (55.34%) and mortality (54.09%) of cervical cancer in Southeast Asia ranked at the top of the Asian regions.Citation1 In Malaysia, cervical cancer ranks as the third most common cancer among women in general and the second most frequent cancer among women between 15 and 44 years of age.Citation2 Human papillomavirus (HPV) was detected in 92.5% of cervical cancer cases, 95.9% of squamous cell carcinomas and 84.3% of adenocarcinomas in Malaysian women.Citation3 The HPV vaccine was introduced in 2006 in Malaysia, and in 2010, HPV vaccination was integrated into the National Immunization Program, where free HPV vaccine was offered to all girls in secondary school (year seven), which is usually the age of 13 in the index year.Citation4
Although younger women are at the greatest risk for the acquisition of HPV infection, the risk of acquiring new HPV infections continues until midlife for most women.Citation5 Evidence has indicated that up to two-thirds of adult females aged 24 to 45 years are susceptible to infections from HPV 6, 11, 16 and 18.Citation6,Citation7 Various studies reported two peak points of HPV infection in women, with the first high peak at less than 25 years of age and the second peak around 45 years of age and older.Citation8–10 Given the continued risk that adult women face and research showing that HPV vaccination is efficacious, safe and immunogenic in women up to the age of 45 years,Citation11,Citation12 in 2018, the licensure of HPV vaccination was extended through the age of 45 years.Citation13 Currently, the 9-valent HPV vaccine for persons 27 to 45 years of age has a shared clinical decision-making recommendation.Citation14 Because 9-valent HPV vaccine provides 5 additional oncogenic types versus the 4-valent vaccine and 7 additional oncogenic types versus the 2-valent vaccines, it almost certainly offers greater protection against HPV-related cancers in adult women.
The significant influence of knowledge, attitudes and beliefs about HPV infections on HPV vaccination intention has been well-studied and reported in a systematic review.Citation15 Numerous studies have been published assessing the attitudes or intention to receive HPV vaccination among adult women up to the age of 45 years.Citation16–19 However, little has been reported on the HPV vaccination intention among Southeast Asian women, especially in Muslim majority countries where sensitivity toward sexually transmitted infections is prominent. It is important to identify barriers to the acceptance of HPV vaccination among adult women in societies with strong traditional and religious cultures, such as in Southeast Asian countries, especially for women who are married.
A unique aspect of barriers to HPV vaccination among adult married women in Southeast Asian countries is the spouse/partner’s influence on vaccination decisions. Particularly in Muslim countries, fathers or husbands were identified as the primary decision makers for the administration of the HPV vaccine to women.Citation20,Citation21 In some cultures, women need approval from their husbands to vaccinate their children against HPV, and young women need approval from their fathers for HPV vaccination.Citation20–22 Men’s disapproval is a major barrier to women’s use of healthcare services,Citation23,Citation24 and there is growing recognition of the importance of men’s involvement in facilitating women’s access to healthcare.Citation25,Citation26
In Malaysia, free vaccination is provided for 13-year-old school girls. Parental consent for adolescent girls’ HPV vaccination was very high (96–98%) and Malaysia’s school-based HPV immunization programme achieved coverage of over 95%.Citation4 However, no study has yet reported the opinions of married adult women on their intention to receive HPV vaccination, since the HPV vaccine has been approved for use among adults aged 27 through 45 years. Moreover, little is also known about the level of knowledge and attitudes toward HPV and HPV vaccination among married adult women in Malaysia. Malaysia is a Muslim majority country, of which approximately 60% of the total population are Muslim. It is widely recognized that acceptance of the HPV vaccine is influenced by the level of knowledge and attitudes toward HPV and HPV vaccination.Citation27–29 Therefore, the main aims of our study were to investigateHPV vaccination intention among adult married women aged 27 to 45 years and its associated factors. The factors investigated were 1) knowledge about HPV and HPV vaccination, 2) health beliefs regarding HPV and HPV vaccination and spouse/partner’s influence on HPV vaccination decision-making.
Materials and methods
Study participants
Study participants were patients attending obstetrics and gynecology outpatient clinics in a university teaching hospital located in an urban area in Kuala Lumpur, Malaysia. Participants were selected based on a computer-generated list of a random list of patients attending the clinic. Since the HPV vaccine has been approved for use among adults aged 27 through 45 years,Citation14 the inclusion criteria were: 1) females age 27 to 45 years, 2) ever been married, and 3) have not previously received any HPV vaccine.
Instruments
The questionnaire consisted of several sections that assessed 1) demographic characteristics, knowing someone with cervical cancer, and sexual behavior, 2) HPV-related knowledge, 3) health beliefs, and 4) intention to receive HPV vaccination and spouse/partner’s influence on HPV vaccination decision-making.
In the knowledge section, respondents answered a series of questions regarding HPV infection and its relationship to cervical cancer and genital warts (20-item scale). Response options were ‘true’, ‘false’ and ‘don’t know’. A correct response was given a score of 1, and an incorrect or ‘don’t know’ response was given a score of 0. The total possible knowledge score ranged from 0 to 20, with higher scores representing higher levels of knowledge.
Health beliefs regarding HPV and HPV vaccination were assessed based on the Health Belief Model (HBM) constructs as a theoretical framework.Citation30–32 The questions on health beliefs regarding HPV and HPV vaccination based on HBM constructs were adapted from previous studies.Citation33,Citation34 Questions included perceived susceptibility to HPV (three items), perceived severity of HPV infection (three items), perceived benefits of HPV vaccine (three items), perceived barriers to getting vaccination against HPV (two items), and cue to action (one item). The importance of mass media as a source of information on HPV and HPV vaccination has been reported in a local study.Citation35 Hence, cue to action, the last construct in the HBM, postulate that exposure to information about HPV vaccination delivered via mass media might constitute a cue to action for individuals to make decision in HPV vaccination. The response options were ‘agree’ and ‘disagree’.
The last section of the questionnaire firstly queried participants about their intention to receive the HPV vaccination and spouse/partner’s influence on HPV vaccination decision-making. The options available were ‘Yes, definitely’, ‘Yes, chance quite high’, ‘No, moderate chance’ and ‘No, definitely not’. Questions about spouse/partner’s influence on HPV vaccination covered 1) communication about HPV vaccination decision-making, 2) whether decision-making was joint or individual, and 3) consent to HPV vaccination.
The electronic questionnaire was presented in both English and Bahasa Malaysia (Malaysia national language). The validity of the questionnaire was established using a panel of experts that consisted of academicians and clinicians. The panel of experts performed content validation of all the items. The Bahasa Malaysia version of the questionnaire was forward, back-translated and reviewed by the research team. Interviews were conducted either in English or Bahasa Malaysia.
Ethical considerations
This study was approved by the University of Malaya Research Ethics Committee (UNREC), Kuala Lumpur, Malaysia (Reference code: UM.TNC2/UMREC − 494). Respondents were informed that their participation was voluntary. All the participants read and signed informed consent.
Statistical analysis
Descriptive statistics were presented as mean (± standard deviation [SD]), median (interquartile range [IQR]), and frequency distribution. The reliability of the knowledge scale was evaluated by assessing the internal consistency of the items representing the knowledge score. The 23 knowledge items in the study sample had a reliability (Kuder-Richardson 20) of 0.881. Simple logistic regression analyses were first to investigate factors associated with intention to receive the HPV vaccination followed by multivariable logistic regression analysis. All variables found to have a statistically significant association (two-tailed, p-value <0.05) with intention to receive the HPV vaccination in the simple logistic regression analyses were entered into multivariable logistic regression analyses using a simultaneous forced-entry model (enter method). Odds ratios (ORs), 95% confidence intervals (95% CIs) and p-values were calculated for each independent variable. The model fit was assessed using the Hosmer-Lemeshow goodness of fit test.Citation36 The significance level was set at p < 0.05. All statistical analyses were performed with the Statistical Package for the Social Sciences, version 20.0 (SPSS, IBM Corp., Armonk, NY, USA).
Results
Characteristics of participants
A total of 900 patients were approached and invited to answer the survey between 20th February and 9th September 2019. In total, 794 completed responses were received. The response rate was 88.2%. A summary of the characteristics of the respondents is provided in the first column of . The majority of the respondents were 31–35 years of age (41.6%) and 27–30 years of age (38.7%). The mean age of the respondents was 32.2 years with a standard deviation (SD) of ±3.9 years. The majority reported an annual household income of MYR2000–3999 (48.6%) and MYR4000–6000 (25.1%). Also, there was a relatively high representation of postgraduate students (14.6%) in the study, as recruitment of participants was conducted in a teaching hospital attached to a tertiary educational institution.
Table 1. Factors associated with HPV vaccination intention (N = 794).
Knowledge about HPV and HPV vaccination
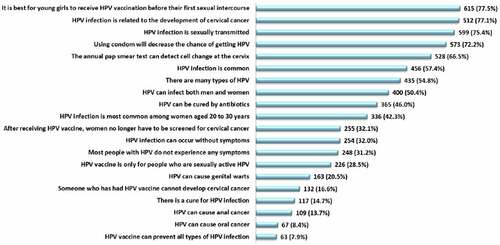
shows the proportion of correct responses on knowledge items. The most common erroneous belief was that the HPV vaccine can prevent all types of HPV infection, with only about 8% of participants providing the correct response. A high proportion of participants were also not aware that HPV infection can cause oral (91.6%) and anal cancers (86.3%). Only 32% were aware that HPV infection can occur without symptoms. The mean and SD for total knowledge score was 8.3 (SD ±3.9) out of a possible score of 20, and the median was 8 (IQR, 6.0–11.0). The knowledge scores of the study participants ranged from 0 to 20. Knowledge scores were categorized as high or low based on the median split; as such, a total of 389 (49.0%) participants were categorized as having a high score (9–20) and 405 (51.0%) participants were categorized as having a low score (0–8).
shows the significant factors associated with level of knowledge. Participants with professional and managerial occupations and high average monthly household income had significantly higher knowledge about HPV and HPV vaccination. Other demographic characteristics were not significantly associated with level of knowledge. Participants who became sexually active at younger ages reported significantly higher knowledge about HPV and HPV vaccination.
Table 2. Significant demographics and sexual behavior factors associated with knowledge about HPV and HPV vaccination in the multivariable logistic regression analysis.
Health beliefs regarding HPV and HPV vaccination
The first and second column of shows the responses to the HBM items. The majority of study participants viewed women have a high susceptibility to contracting HPV in their lifetime (87.9%). They also viewed that women have a high susceptibility to genital warts (76.3%) and cervical/vulvar cancer (83.4%). Perception of severity was highest for cervical/vulvar cancer (92.3%), followed by HPV infection (88.5%), and genital warts (83.9%). A large majority also perceived the benefits of having HPV vaccines in the prevention of HPV infection (92.6%), cervical/vulvar cancer (89.8%), and genital warts (89.7%). Regarding the perceived barriers to getting vaccinated, a large majority (64.1%) expressed time constraints and only 20.2% expressed the fear of severe side effects as barriers to HPV vaccination. Only one-third of participants reported being exposed often to information about HPV vaccination delivered via mass media.
Spouse/partner influence in HPV vaccination decision-making
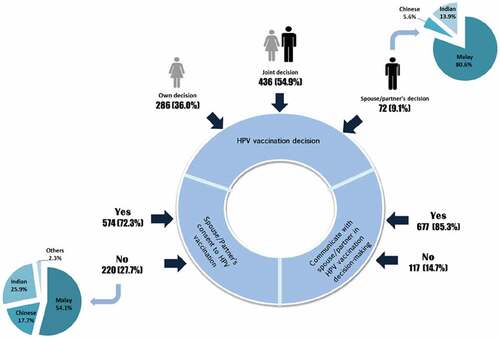
As shown in , the majority (85.3%) of the study participants reported that they would communicate with their spouse/partner before deciding on HPV vaccination. A total of 72.3% of participants perceived their spouse/partner would consent to their HPV vaccination. The remaining 27.7% who reported their spouse/partner would not consent, over half (54.1%) were Malay Muslims. In regards to the decision for HPV vaccination, slightly over half (54.9%) reported that HPV vaccination was dependent on joint approval between themselves and their spouse/partner. A total of 36.0% of participants reported the decision to obtain HPV vaccination was solely their decision, and 9.1% of participants reported that their HPV vaccination decision was dependent on their spouse/partner’s approval. The vast majority of participants who reported the decision for HPV vaccination was entirely dependent on their spouse/partner’s decision were Malay Muslims (80.6%).
Intention to obtain HPV vaccination
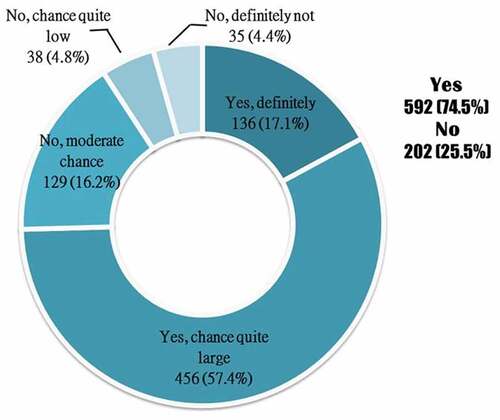
shows the responses of the participants to their intention to obtain the HPV vaccination. In total, 74.5% (n = 592) reported Yes, definitely/chance quite high, whereas 25.5% (n = 202) reported No, moderate chance/chance quite low/definitely not. As shown in , variables that were significantly associated with intention to obtain HPV vaccination in the univariate analysis were religion, occupational type, average monthly household income, knowledge about HPV and HPV vaccination, perception of no severe side effects after receiving HPV vaccination, perceived spouse/partner’s consent to HPV vaccination, and having the ability to make their own decision for HPV vaccination.
In the multivariable logistic regression model, the significant socio-demographic characteristics associated with HPV vaccination intention were occupational type and average household income, whereby students (OR = 4.55; 95% CI, 2.13–9.72) and participants with an average household income MYR2000–4000 (OR = 2.09; 95% CI, 1.16–3.78) had the largest significant ORs in HPV vaccination intention. A high knowledge score (9–20) (OR = 1.60; 95% CI, 1.10–2.32 vs. knowledge score 0–8) was also significantly associated with HPV vaccination intention. None of the health belief items were significant covariates in the multivariable model. Spouse/partner’s consent to HPV vaccination (OR = 4.51; 95% CI, 3.08–6.62) was a strong significant covariate in the multivariate model.
Discussion
A mean and median knowledge score lower than the midpoint of the scale implies most women lack basic knowledge about HPV and HPV vaccination; hence, this warrants attention. The present study identifies specific knowledge deficits that should be the target of awareness-raising education programmes for adult women. These include unawareness of the HPV types covered by different HPV vaccines, and most importantly, many women were not aware that HPV infection also causes other cancers, such as oral and anal cancers apart from cervical cancer. Many women in this study also lack knowledge that HPV infection can be asymptomatic. Our findings imply that it is important to educate women that most HPV infections are typically transient and asymptomatic and that viral infection can run its course asymptomatically. The present study highlights the socioeconomic disparities in HPV-related knowledge. Two socioeconomic indicators, namely higher level of occupation and income, were associated with higher levels of HPV-related knowledge, which implies the need particularly to targetHPV education interventions in women from low socioeconomic backgrounds.
In this study, most participants demonstrated positive health beliefs grounded in the constructs of the HBM. High perceptions of susceptibility to infection, severity of HPV disease, and perceived benefits of HPV vaccines were also reported. Another important finding was that women in this study reported the greatest barrier to HPV vaccination was the time constraint. Most women in this study were employed, postgraduate students or housewives. This is perhaps due to the reason that most of the women in this study are challenged by other responsibilities in their careers and household chores, causing them to feel constrained by time for HPV vaccination. This finding suggests that the implementation of workplace vaccination programs would enhance HPV vaccine uptake among working women. It would also be beneficial if the current school-based HPV vaccination programme, whereby health teams administer HPV vaccines to school adolescent girls, also provide services to vaccinate the mothers of school-aged children in the school settings, thus providing convenience for mothers to obtain the HPV vaccine. While mass media is useful in providing information about HPV,Citation37 only one-third of our study participants reported having been frequently exposed to information about HPV vaccination from mass media, implying that a paucity of publicity on HPV vaccination reached the adult women in our study. Studies outside Malaysia found media campaigns that positively promote immunization can increase public knowledge and improve HPV vaccine uptake rates.Citation38,Citation39 As such, a publicity drive to increase awareness about HPV vaccination that has been extended for women up to 45 years old should be enhanced.
Overall, participants in this study indicated they would communicate with their spouse/partner before making decisions about HPV vaccination, implying an important role of men in the HPV vaccination of women. The importance of the support of men in HPV vaccination is further evident because a considerable proportion of women in this study reported joint decision-making with regard to HPV vaccination. Women seeking HPV vaccination may be perceived as promiscuous, disloyal to their husband/partner or even condoning extramarital sexual conduct.Citation40 It remains a challenge for women to communicate about vaccination against a sexually transmitted infection in a marital context. It is unknown if women would fear provoking mistrust and conflict if they communicate their intention for vaccination against a sexually transmitted infection to their husbands. Therefore, the importance of educating married couples about a healthy communication style with regard to HPV vaccination would be useful to enhance HPV vaccine uptake.
A finding of utmost importance in this study was that a considerable proportion of participants reported their spouse/partner would not allow them to receive HPV vaccination. In Asian communities, obedience to husbands is a social norm.Citation41 Husband disapproval of HPV vaccination may result in women being denied access to HPV vaccination. In particular, this study found the majority of Malay Muslim participants perceived their husbands would disapprove of them receiving the HPV vaccination. In regard to vaccination decision, as compared to other ethnic groups, a higher proportion of Malay Muslim participants reported that the decision to receive the HPV vaccination was entirely dependent on their spouse/partner, implying the value of respect and obedience toward husbands among the Malay women in Malaysia. It remains a challenge for Malay Muslim women to obtain approval from their spouses for HPV vaccination, as prohibition against both premarital and extramarital sex are strong in Islam. In a previous study in Malaysia, Muslim parents viewed that adolescent girls did not need HPV vaccination in a family with a proper religious upbringing,Citation42 likewise Muslim spouse/partners perceived that HPV vaccination in a marital context was unnecessary.
Findings on the intention to receive HPV vaccination revealed that most women in this study had positive intentions to obtain HPV vaccination. The HPV vaccination intention among adult women in this study (74.5%) is higher than those reported in a recently published study among adult women of a similar age range in mainland China (58.3%).Citation43 In Malaysia, HPV vaccines became available in the year 2006. In contrast, the authorities in China approved the first HPV vaccine in 2016, a decade after the United States Food and Drug Administration’s licensure in 2006. This perhaps explains the relatively higher HPV vaccination intention reported by our study participants. In the present study, spouse/partner’s consent to HPV vaccination was a strong predictor of women’s intention to receive the HPV vaccine in the multivariable analysis. This was similarly found in the study by Lin et al., 2020, where adult women reported that spousal decision on HPV vaccination greatly influence their HPV vaccination intention.Citation43 The consistent findings across the two studies amplify the important role of men in encouraging HPV vaccination in adult women. Men play an undeniably important role in providing permission to their spouse/partners to receive vaccination against a sexually transmitted infection. Married women in most Asian sociocultural contexts will seek their husband’s permission regarding their own healthcare before making a decision.Citation44 Most Southeast Asian women associate asking permission with being respectful toward their husbands.Citation45 In many cases, women are not able to override their husband’s decision. It is unknown how married men would respond to their wives seeking HPV vaccination. A previous local study conducted when the HPV vaccine was just introduced in Malaysia revealed that men would like to be informed and also take part in the decision-making process for their daughters.Citation21 Culture-centered interventions are needed, considering the ethnic differences in men’s influences on HPV vaccine decision-making. Health interventions that target and involve men are strongly associated with enhanced and better reproductive health outcomes in women.Citation24 Thus, HPV-related health information geared towards the male partners of women should be initiated as soon as possible in Malaysia.
The multivariable analysis also found that higher socio-economic status was associated with a significantly higher intention for HPV vaccination. Participants who were in employment also expressed significantly higher HPV vaccination intention. Identification of socio-economic factors associated with vaccination intention can inform efforts to target community and clinical interventions to improve HPV vaccination uptake. Further knowledge is also a significant factor influencing HPV vaccine uptake, as in many other studies in Asia.Citation46 Hence, this indicates that HPV-related awareness is highly essential for married adult women to enhance HPV vaccination intention.
The major limitation of the study is that adult married women were recruited from a teaching hospital attached to a tertiary institution in an urban area. Therefore, the study participants may not be representative of adult women in general in Malaysia and particularly women in rural settings. This study is also under-representative of lower-educated women. Thus, HPV vaccination intention may be lower among Malaysian adult women in general, and it is also possible that Malaysian men, in general, are more hesitant toward their wives receiving HPV vaccination than that found in this study. The second limitation is the use of a cross-sectional study design. Cross-sectional data cannot be used to infer causality. The third limitation is that the responses were based on self-reporting of data and may be subject to self-reporting bias and a tendency to report socially desirable responses. Therefore, the results should be interpreted with caution.
Conclusion
Spouse/partner’s influence on the decision-making of married women with regard to HPV vaccination was prominent in this study. The majority of participants would communicate with their spouse/partner in the HPV vaccination decision-making process. A considerable proportion of women would depend entirely on their spouse/partner’s approval for HPV vaccination. The perception that their spouse/partner would not consent for them to receive HPV vaccination was evident. Malay women generally reported the decision for HPV vaccination was dependent on their spouse/partner’s approval, and many believed that their spouse/partner would not consent to their HPV vaccination. Intention to vaccinate was generally positive among married women in Malaysia. However, spouse/partner’s consent for HPV vaccination was the main factor influencing HPV vaccination intention. Other influential factors were socio-economic background and having good HPV-related knowledge. The study highlighted the importance of awareness and support from male partners for HPV vaccination on the intent of women to receive HPV vaccination. Based on these findings, culturally and ethnically targeted HPV health interventions are warranted for both men and women. This study adds to the body of evidence on the importance of engaging men to support HPV vaccination of adult women.
Authors contribution
LPW, GDZ, YL, ZH contributed to the study conception and design. LPW and GDZ conceived the study. FNS and HA collected the data. LPW and HA analyzed the data. The first draft of the manuscript was written by LPW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosure statement
Dr Zimet has received honoraria from Sanofi Pasteur for his work on the Adolescent Immunization Initiative and an honorarium and travel support from Merck & Co., Inc. to present at an HPV vaccine symposium.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Phan NHD, Nguyen TT, Vo NT, Le TTT, Tran TBH, Truong PK, Ai Huyen Le TD, Duc Lao T. Epidemiology, incidence, mortality of cervical cancer in Southeast Asia and their relationship: an update report. Asian J Pharm Res Health Care. 2020;12(3):1–10. doi:10.18311/ajprhc/2020/25208.
- ICO/IARC Information Centre on HPV and Cancer. (2021 July 27) China human papillomavirus and related cancers, fact sheet 2017 [Retrieved Dec 30 2019]. http://www.hpvcentre.net/statistics/reports/CHN_FS.pdf.
- Abdul Raub SH, Isa NM, Zailani HA, Omar B, Abdullah MF, Mohd Amin WA, Noor RM, Ayub MC, Abidin Z, Kassim F, et al. Distribution of HPV genotypes in cervical cancer in multi- ethnic Malaysia. Asian Pac J Cancer Prev. 2014;15(2):651–56. doi:10.7314/apjcp.2014.15.2.651.
- Muhamad NA, Buang SN, Jaafar S, Jais R, Tan PS, Mustapha N, Lodz NA, Aris T, Sulaiman LH, Murad S. Achieving high uptake of human papillomavirus vaccination in Malaysia through school-based vaccination programme. BMC Public Health. 2018;18(1):1402. doi:10.1186/s12889-018-6316-6.
- Burger EA, Kim JJ, Sy S, Castle PE. Age of acquiring causal human papillomavirus (HPV) infections: leveraging simulation models to explore the natural history of HPV-induced cervical cancer. Clin Infect Dis. 2017;65(6):893–99. doi:10.1093/cid/cix475.
- Brotherton JM, Mullins RM. Estimating coverage of the National HPV Vaccination Program: where are we at? Med J Aust. 2009;191(3):188. doi:10.5694/j.1326-5377.2009.tb02738.x.
- Weisberg E, Bateson D, McCaffery K, Skinner SR. HPV vaccination catch up program - utilisation by young Australian women. Aust Fam Physician. 2009;38(1–2):72–76.
- Smith JS, Melendy A, Rana RK, Pimenta JM. Age-specific prevalence of infection with human papillomavirus in females: a global review. J Adolesc Health. 2008;43(4):SS5–41. doi:10.1016/j.jadohealth.2008.07.009.
- Chan PK, Chang AR, Yu MY, Li WH, Chan MY, Yeung AC, Cheung TH, Yau TN, Wong SM, Yau CW, et al. Age distribution of human papillomavirus infection and cervical neoplasia reflects caveats of cervical screening policies. Int J Cancer. 2010;126(1):297–301. doi:10.1002/ijc.24731.
- Liao G, Jiang X, She B, Tang H, Wang Z, Zhou H, Ma Y, Xu W, Xu H, Chen W, et al. Multi-Infection patterns and co-infection preference of 27 human papillomavirus types among 137,943 gynecological outpatients across China. Front Oncol. 2020;10:449. doi:10.3389/fonc.2020.00449.
- Castellsagué X, Muñoz N, Pitisuttithum P, Ferris D, Monsonego J, Ault K, Luna J, Myers E, Mallary S, Bautista OM, et al. End-of-study safety, immunogenicity, and efficacy of quadrivalent HPV (types 6, 11, 16, 18) recombinant vaccine in adult women 24-45 years of age. Br J Cancer. 2011;105(1):28–37. doi:10.1038/bjc.2011.185. Advance online publication 2011 May 31
- Skinner SR, Szarewski A, Romanowski B, Garland SM, Lazcano-Ponce E, Salmerón J, Del Rosario-Raymundo MR, Verheijen RH, Quek SC, da Silva DP, et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 4-year interim follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet. 2014;384(9961):2213–27. doi:10.1016/S0140-6736(14)60920-X.
- U.S. Food and Drug Administration. (2018, Oct 5). FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old [Retrieved Dec 30, 2019]. https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old.
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68(32):698–702. doi:10.15585/mmwr.mm6832a3.
- Santhanes D, Yong CP, Yap YY, Saw PS, Chaiyakunapruk N, Khan TM. Factors influencing intention to obtain the HPV vaccine in South East Asian and Western Pacific regions: a systematic review and meta-analysis. Sci Rep. 2018;8(1):3640. doi:10.1038/s41598-018-21912-x.
- Black LL, Zimet GD, Short MB, Sturm L, Rosenthal SL. Literature review of human papillomavirus vaccine acceptability among women over 26 years. Vaccine. 2009;27(11):1668–73. doi:10.1016/j.vaccine.2009.01.035.
- Dempsey AF, Brewer SE, Pyrzanowski J, Sevick C, O’-Leary ST. Acceptability of human papillomavirus vaccines among women older than 26 years. Vaccine. 2015;33(13):1556–61. doi:10.1016/j.vaccine.2015.02.018. Advance online publication 2015 Feb 19
- Liau A, Stupiansky NW, Rosenthal SL, Zimet GD. Health beliefs and vaccine costs regarding human papillomavirus (HPV) vaccination among a U.S. national sample of adult women. Prev Med. 2012;54(3–4):277–79. doi:10.1016/j.ypmed.2012.02.002.
- Weiss TW, Rosenthal SL, Zimet GD. Attitudes toward HPV vaccination among women aged 27 to 45. ISRN Obstet Gynecol. 2011;2011:670318. doi:10.5402/2011/670318.
- De Groot AS, Tounkara K, Rochas M, Beseme S, Yekta S, Diallo FS, Tracy JK, Teguete I, Koita OA, Seale H. Knowledge, attitudes, practices and willingness to vaccinate in preparation for the introduction of HPV vaccines in Bamako, Mali. PLoS One. 2017;12(2):e0171631. doi:10.1371/journal.pone.0171631.
- Wong LP. Role of men in promoting the uptake of HPV vaccinations: focus groups’ finding from a developing country. Int J Public Health. 2010;55(1):35–42. doi:10.1007/s00038-009-0072-4.
- Sathian B, Babu MGR, van Teijlingen ER, Banerjee I, Roy B, Subramanya SH, Rajesh E, Devkota S. Ethnic variations in perception of human papillomavirus and its vaccination among young women in Nepal. Nepal J Epidemiol. 2017;7(1):647–58. doi:10.3126/nje.v7i1.17757.
- Chekole MK, Kahsay ZH, Medhanyie AA, Gebreslassie MA, Bezabh AM. Husbands’ involvement in family planning use and its associated factors in pastoralist communities of Afar, Ethiopia. Reprod Health. 2019;16(1):33. doi:10.1186/s12978-019-0697-6.
- Ganle JK, Dery I. ‘What men don’t know can hurt women’s health’: a qualitative study of the barriers to and opportunities for men’s involvement in maternal healthcare in Ghana. Reprod Health. 2015;12(1):93. doi:10.1186/s12978-015-0083-y.
- Morgan R, Tetui M, Muhumuza Kananura R, Ekirapa-Kiracho E, George AS. Gender dynamics affecting maternal health and health care access and use in Uganda. Health Policy Plan. 2017;32(Suppl_5):v13–v21. doi:10.1093/heapol/czx011.
- Namasivayam A, Osuorah DC, Syed R, Antai D. The role of gender inequities in women’s access to reproductive health care: a population-level study of Namibia, Kenya, Nepal, and India. Int J Womens Health. 2012;4:351–64. doi:10.2147/IJWH.S32569.
- Chan ZC, Chan TS, Ng KK, Wong ML. A systematic review of literature about women’s knowledge and attitudes toward human papillomavirus (HPV) vaccination. Public Health Nurs. 2012 ;29(6):481–89. doi:10.1111/j.1525-1446.2012.01022.x.
- Leung SOA, Akinwunmi B, Elias KM, Feldman S. Educating healthcare providers to increase human papillomavirus (HPV) vaccination rates: a qualitative systematic review. Vaccine X. 2019;3:100037. doi:10.1016/j.jvacx.2019.100037.
- Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG, Hozbor DF. Knowledge and awareness of HPV vaccine and acceptability to vaccinate in sub-Saharan Africa: a systematic review. PLoS One. 2014;9(3):e90912. doi:10.1371/journal.pone.0090912.
- Becker MH. The health belief model and personal health behavior. Health Educ Monogr. 1974;2(4):324–473. doi:10.1177/109019817400200407.
- Champion VL, Skinner CS. The health belief model. Health Behav Health Educ Theory Res Pract. 2008;4:45–65.
- Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–35. doi:10.1177/109019817400200403.
- Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–80. doi:10.1007/s12160-012-9366-5.
- Wong LP, Muhammad Yusoff RN R, Edib Z, Sam IC, Zimet GD. Nationwide survey of knowledge and health beliefs regarding human papillomavirus among HPV-vaccinated female students in Malaysia. PLoS One. 2016;11(9):e0163156. doi:10.1371/journal.pone.0163156.
- Wong LP, Sam IC. Ethnically diverse female university students’ knowledge and attitudes toward human papillomavirus (HPV), HPV vaccination and cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2010;148(1):90–95. doi:10.1016/j.ejogrb.2009.10.002.
- Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. Vol. 398. Hoboken, NJ, USA: John Wiley & Sons; 2013.
- Gollust SE, LoRusso SM, Nagler RH, Fowler EF. Understanding the role of the news media in HPV vaccine uptake in the United States: synthesis and commentary. Hum Vaccin Immunother. 2016;12(6):1430–34. doi:10.1080/21645515.2015.1109169.
- Kelly BJ, Leader AE, Mittermaier DJ, Hornik RC, Cappella JN. The HPV vaccine and the media: how has the topic been covered and what are the effects on knowledge about the virus and cervical cancer? Patient Educ Couns. 2009;77(2):308–13. doi:10.1016/j.pec.2009.03.018. Advance online publication 2009 Apr 22.
- Okuhara T, Ishikawa H, Okada M, Kato M, Kiuchi T. Newspaper coverage before and after the HPV vaccination crisis began in Japan: a text mining analysis. BMC Public Health. 2019;19(1):770. doi:10.1186/s12889-019-7097-2.
- Wong LP, Wong PF, Hashim MMAA M, Han L, Lin Y, Hu Z, Zhao Q, Zimet GD. Multidimensional social and cultural norms influencing HPV vaccine hesitancy in Asia. Hum Vaccin Immunother. 2020;16(7):1611–22. doi:10.1080/21645515.2020.1756670. Advance online publication 2020 May 19
- Xie Z. Regarding men as superior to women: impacts of Confucianism on family norms in China. China Popul Today. 1994;11(6):12–16. PMID: 12290499.
- Wong LP. Preventing cervical cancer through human papillomavirus vaccination: perspective from focus groups. J Low Genit Tract Dis. 2009;13(2):85–93. doi:10.1097/LGT.0b013e3181865f44. PMID: 19387128.
- Lin Y, Lin Z, He F, Chen H, Lin X, Zimet GD, Alias H, He S, Hu Z, Wong LP. HPV vaccination intent and willingness to pay for 2-,4-, and 9-valent HPV vaccines: a study of adult women aged 27-45 years in China. Vaccine. 2020;38(14):3021–30. doi:10.1016/j.vaccine.2020.02.042. Advance online publication.
- Ghose B, Feng D, Tang S, Yaya S, He Z, Udenigwe O, Ghosh S, Feng Z. Women’s decision-making autonomy and utilisation of maternal healthcare services: results from the Bangladesh Demographic and Health Survey. BMJ Open. 2017;7(9):e017142. doi:10.1136/bmjopen-2017-017142.
- Tonsing JC, Tonsing KN. Understanding the role of patriarchal ideology in intimate partner violence among South Asian women in Hong Kong. Int Soc Work. 2019;62(1):161–71. doi:10.1177/0020872817712566.
- Loke AY, Kwan ML, Wong YT, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8(4):349–62. doi:10.1177/2150131917742299. Advance online publication.