ABSTRACT
This study aimed to assess vaccine willingness, and the reasons why respondents were not likely to receive COVID-19 vaccine prior to and during the COVID-19 vaccine rollout. This cross-sectional survey (n = 5,130) was conducted between January and April 2021 in South Australia, Australia. Weighted multiple logistic regression was performed to assess the association between sociodemographic/health factors and outcome measures. The percentage of respondents who stated they were very likely to get vaccinated fluctuated between 50% and 78% during the survey period. The willingness of receiving COVID-19 vaccination was significantly lower among women than men (aOR: 0.70) and higher among adults ≥50 years (aOR: 1.82 for 50–69 years and aOR: 3.01 for ≥70 years vs 16–29-year olds). Other factors significantly associated with higher willingness were ≥Year 12 education (aOR: 2.50 for Year 12/TAFE/certificate/diploma vs <Year 12 education; aOR: 1.44 for bachelor’s degree or higher vs <Year 12 education), highest socioeconomic level vs lowest socioeconomic level (aOR: 1.75), and unpaid work/retirement/other vs unemployment (aOR: 1.77). Other factors such as being Aboriginal, not being married, not having chronic illness, and/or culturally and linguistically diverse backgrounds were identified to be significantly related to low confidence in vaccine safety, perceived low risk of disease and/or perceived lack of information. Parents or caregivers were significantly less willing for their child to be vaccinated compared to people in general (OR: 0.62). Targeted campaigns to improve uptake need to include appropriate messaging about vaccine safety and disease burden in addition to strategies to improve access to less willing groups.
KEYWORDS:
Introduction
At the end of 2019, a novel coronavirus (SARS-CoV-2) was first identified during an outbreak that emerged in Wuhan, the capital city of the Hubei Province, China. It has rapidly spread, resulting in a global pandemic.Citation1 The COVID-19 pandemic has had a severe impact on public health, daily life, and economies around the world. The pandemic has led to a significant loss of human life around the world and key challenges have been the emergence of new variants of the virus, and how quickly vaccines could be rolled out to the community.Citation2 The economic and social disruption caused by the pandemic is overwhelming: tens of millions of people are at risk of falling into extreme poverty-living on less than $2 a day, while the number of undernourished people, estimated at nearly 690 million in 2020.Citation3 In Australia, it was reported that there were almost four times as many deaths caused by COVID-19 in the lowest socioeconomic group compared with the highest socioeconomic group, and age-standardized mortality rates were 2.6 times as high.Citation2 Massive vaccination against SARS-CoV-2 infection is considered the most promising approach for ending the pandemic.Citation4 The development and high uptake of vaccines is essential to combat the pandemic.Citation5 Case numbers of COVID-19 due to the Omicron variant are rapidly increasing around the world. Among the 257,337 sequences uploaded to GISAID, a global genomic data sharing platform, with specimens collected from 23 March to 21 April 2022, 256,684 (99.7%) were Omicron.Citation6 WHO has warned that the Omicron variant should not be perceived as mild and still presents a serious risk to the health systems, although disease severity seems to be less than with the Delta variant. COVID-19 vaccines not only protect people from the variants currently in circulation including Omicron but are also likely to offer protection against severe disease including hospitalizations and ICU admissions and deaths due to future mutations of circulating variants.Citation7 South Australia has its highest daily number of COVID-19 cases on record in April 2022.Citation8 It was initially expected that 85% of the eligible Australian population including 5–16 year-olds would need to be fully vaccinated with two doses of COVID-19 vaccines to achieve herd immunity.Citation9 Although the second-dose vaccine coverage has reached >95% in people over the age of 16 in Australia,Citation10 strong evidence has indicated that booster doses of COVID-19 vaccines are required to increase protection against infection with the Omicron variant.Citation11 It is now recommended to receive COVID-19 booster vaccination for anyone aged 16 and older who has completed their two-dose COVID-19 vaccination in Australia.Citation11 However, only 52.4% of eligible population received the booster vaccinations.Citation10 The COVID-19 vaccines play a critical role in preventing deaths, Intensive Care Unit admissions, and hospitalization caused by COVID-19 infections. The success of vaccine rollout depends on very high vaccine acceptance and uptake to fight further waves of COVID-19 infections. There has been an urgent need to understand the attitudinal and behavioral drivers in order to inform community-led communication strategies to build trust and optimize COVID-19 vaccine uptake.
In surveys conducted during the initial wave of the pandemic, more than 80% of participants indicated that they would receive the COVID-19 vaccine.Citation12,Citation13 In a survey study, willingness to vaccinate was higher among Australians in April 2020. However, the survey was repeated in July–August and December 2020 showing willingness to vaccinate against COVID-19 decreased over time.Citation14 In a longitudinal survey, after a large decline in vaccine willingness was observed between August 2020 and January 2021,Citation15 the survey data were collected again in April and August 2021 showing that although vaccine willingness did not decrease further there were still several sub-populations that remained hesitant about COVID-19 vaccination.Citation16,Citation17 It is likely that population attitudes toward COVID-19 vaccine will fluctuate with the waves of the pandemic, necessitating regular tracking of vaccine confidence among different population groups to ensure public health campaigns remain responsive to community vaccine sentiments. In parent surveys conducted before and after the vaccine rollout, higher vaccine hesitancy or refusal was demonstrated among parents.Citation17–20
Using survey data collected from a representative sample with a large sample size, including parents and caregivers, to accurately identify the key factors associated with COVID-19 vaccine willingness and concerns, is essential to inform public health messaging and communication strategies for effectively promoting the COVID-19 vaccine in targeted groups.
Our study aimed to assess vaccine willingness and determine sociodemographic and health factors influencing public attitudes toward COVID-19 vaccine prior to and during the COVID-19 vaccine rollout.
Methods
Study design and data sources
This study used a cross-sectional survey design. The South Australian Population Health Survey (SAPHS) is an ongoing state-wide population-level survey used to implement this study in Australia. The SAPHS is managed by Wellbeing SA—a state government agency within the Health Portfolio. Wellbeing SA has been collecting population-level data on the health and wellbeing of South Australians since 2002. Data are collected every month on overall health status, health service utilization, chronic conditions, cancer prevention, disability and carers, risk factors (biomedical, protective, and behavioral), food security, mental health, wellbeing, and disadvantage and inequity. Survey questions are developed in consultation with a broad range of stakeholders, to ensure the questions asked in the SAPHS are most appropriate to measure and monitor current disease trends, health service use, and health and lifestyle behavior. All questions are pilot tested when they are inserted into the survey. Some questions are from validated tools, while others are derived from national datasets. In preparation for the COVID-19 vaccine rollout, questions were included in the SAPHS to monitor the vaccine acceptance and confidence in vaccine safety in the South Australian population. The vaccination questions were derived from questions being asked by the Commonwealth Department of Health. The only data regarding COVID-19 vaccine attitudes were presented in the manuscript.
A probability-based, dual-frame sample of South Australian residents was selected using random digit dialing. Standard de-duplication and weighting procedures for the dual overlapping frames were administered. As the SAPHS is a population-level survey, the only inclusion criteria were that respondents be residents of South Australia with access to a telephone. The data collector was able to conduct interviews in selected languages other than English (e.g. Greek, Arabic, and Vietnamese). For selected persons aged 15 years or younger, a parent/guardian proxy completed the interview on their behalf.
Informed verbal consent was obtained prior to the survey commencing. Once a person has consented to participate, the survey took approximately 20 min to complete. The participant might choose to be contacted at an alternative time or day that was most suitable for them. Participants could choose to skip questions during the interview and could withdraw their consent to participate in the survey at any time.
The only condition of the survey respondents was to be residents of South Australia. Potential respondents were contacted in the first instance to assess eligibility and then invited to participate in the survey. Participants were asked if they reside in South Australia and for their postcode.
Data collection
Data were collected using computer assisted telephone interviewing. To maximize participation, respondents were also offered the option of completing the survey on-line by receiving a unique hyperlink. The data presented in this paper were collected from 4 January to 30 April 2021 in South Australia, Australia. The cooperation rateCitation21during this time frame was 64.2%.
Respondents were asked about their willingness to get vaccinated against COVID-19. If respondents did not state that they were very likely to get vaccinated, they were asked what would prevent them from considering being vaccinated against COVID-19. Reasons were grouped by themes in the analyses: 1) vaccine safety concerns; 2) a low perceived risk of infection; 3) vaccine effectiveness concerns; 4) perceived lack of information; and 5) general vaccine refusal. Respondents were also asked if they thought the vaccines were safe (Table S1).
Statistical analysis
Data were presented by various population subgroups of sociodemographic and health characteristics. Socio-Economic Index For Areas (SEIFA) quintiles were presented according to the definition from the Australian Bureau of StatisticsCitation22 using the respondent’s postcode and suburb. As a proxy for respondents who are culturally and linguistically diverse, the respondent’s country of birth (COB) was divided into two broad categories: English-speaking countries and non-English-speaking countries. Respondents who were born in Australia, the United Kingdom, Ireland, the United States of America, New Zealand, Canada, and South Africa are included in the English-speaking background category. All other respondents were included in the non-English speaking background category.Citation23 Health outcomes presented in the analyses were self-reported based on whether the respondent had even been told by a doctor or nurse they had a chronic condition. Aboriginal was used in this document respectfully as an all-encompassing term for Aboriginal and Torres Strait Islander people, health, and culture.
The predictor variables comprised of age, gender, Aboriginal identification, SEIFA, marital status, educational attainment, employment status, COB, area of residence, presence of chronic conditions, and presence of a mental health condition. In addition, a binary variable was created to indicate whether respondents had completed the survey before or after the implementation of the COVID-19 vaccination program. In Australia, the COVID-19 vaccine rollout commenced on 22 February 2021. Household income was not included as 25% of respondents answered “don’t know” or preferred not to say.
Since ordinal logistic regression models did not demonstrate adequate fit, logistic regression models were used, defining the outcome as 1 if a respondent answered “very likely/confident” and 0 for any other responses. Answers 1–7 and 9–12 to the question regarding the reasons why they were not very likely to receive the COVID-19 vaccine were grouped by themes. Logistic regression was performed for each theme to investigate factors associated with the reasons for vaccine hesitancy or refusal. The outcome was defined as 1 if a respondent selected any response relevant to the group theme. If a respondent who answered “very likely” to the vaccine willingness question or did not select any response relevant to the group theme, the outcome was “0”.
Univariate and multiple logistic regression analyses were performed to test association between predictor variables and outcome measures. All the above-mentioned covariates with a p-value ≤0.20 on a univariate analysis of association with an outcome measure were included in a multivariate logistic model. All results presented in the descriptive tables and regression analyses were weighted. Raking was used to weight respondents incorporating various population characteristics (sex, age, area of residence, country of birth, dwelling status, marital status, education level, employment status, household size) to more closely reflect the South Australian population using benchmarks derived from the June 2016 ABS Census data. The weighting process ensured our findings were representative of the South Australian population. Adjustment to the demographic composition of the sample may cause variability in numbers for the unweighted and weighted populations.
Results
Study population
This survey was conducted in 5,130 South Australians between 4 January and 30 April 2021 including 4,484 respondents aged ≥16 years and 646 parents or caregivers answering questions on behalf of their child aged less than 16 years.
The response option “I have already been vaccinated” to the question of COVID-19 vaccine willingness was introduced on 7 April 2021 due to the expansion of the rollout to Phase 1b on 23 March 2021. These respondents (n = 85) who were vaccinated were excluded from the sample, as our analyses were based on respondents who had not yet been vaccinated and assessed their intention to vaccinate against COVID-19. shows the weighted and unweighted socio-demographic and health characteristics of both respondents aged ≥16 years and parents/caregivers. Finally, 4,400 (weighted n = 4,067) respondents aged ≥16 years were included in the weighted and adjusted regression analyses.
Table 1. Weighted and unweighted socio-demographic characteristics of ALL respondents (excluding the respondents who answered “I have already been vaccinated”).
Vaccine willingness
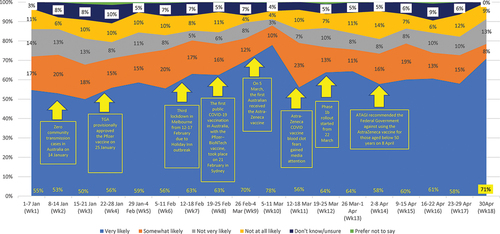
Of respondents aged ≥16 years, 60.1% indicated they were very likely to be vaccinated with COVID-19 vaccine (Table S2). Parent/guardian respondents were less likely to agree with their child receiving the vaccine compared to those ≥16 years (48.2% vs 60.1% very likely to get vaccinated; OR: 0.62 [95% CI, 0.50–0.76]). The likelihood of vaccination against COVID-19 was highest (weighted percentage: 77.9%) in early March following the first COVID-19 vaccinations being given (). This was followed by a second peak in late April.
Figure 1. Weighted likelihood rates of accepting COVID-19 vaccination by survey week and key events reported and announcements made during the survey period.
In the weighted and adjusted logistic model, age, gender, socioeconomic status, educational attainment, and COVID-19 vaccine rollout were associated with the intention to receive the COVID-19 vaccine (). The willingness to receive COVID-19 vaccination was lower among women, and higher among adults aged ≥50 years, people with the highest SEIFA quantile, those completing high-school education or higher, and those with unpaid work/retirement/other prior to the vaccine rollout.
Table 2. Weighted and adjusted odds ratios of likelihood (very likely) of getting COVID-19 vaccination in the subsample of respondents aged 16+ (comparing “very likely” with “somewhat/not very/not at all likely/don’t know”).
Confidence in vaccine safety
Eighty percent of people ≥16 years were either very confident (35.1%) or somewhat confident (46.1%) about vaccine safety (Table S3). In the weighted and adjusted logistic model, confidence in vaccine safety was lower among women, Aboriginal people, the unemployed, respondents with a non-English-speaking COB, and increased with years of age, education llevel,and socioeconomic advantage (Table S4). Confidence in vaccine safety reported by parents/caregivers on behalf of their child was lower than those respondents aged ≥16 years (27.2% vs 35.1% very confident).
Reasons for not considering COVID-19 vaccination
Among respondents aged ≥16 years (weighted n = 1,622) who were not “very likely” to be vaccinated, vaccine safety concerns (Tables S5 and S6), perceived low risk of infection (Tables S7 and S8), and perceived lack of information about COVID-19 vaccines (Tables S9 and S10) were the top three barriers to COVID-19 vaccination ( and Figure S1). Only a small proportion of respondents indicated that they were anti-vaccination (2.5%) (Table S11) or believed a COVID-19 vaccine would not be effective for this virus (5.2%) (Tables S12 and S13).
Figure 2. Reasons for not considering COVID-19 vaccination, by subgroup themes# (multiple responses allowed).
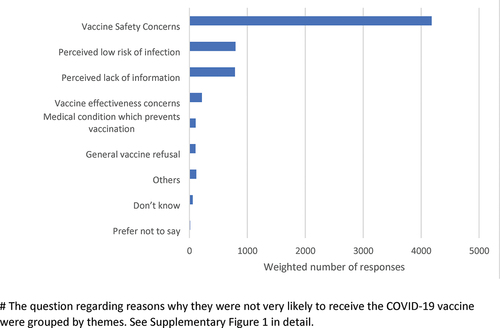
In the weighted logistic regression analysis, predictors identified for lower risk perception about COVID-19 (Table S8) and perceived inadequate information about the vaccine (Table S10) were similar to those for vaccine willingness and vaccine safety confidence (age, gender, Aboriginal people, socioeconomic status, education attainment, employment). However, the COVID-19 vaccine rollout had a significant impact on vaccine safety concerns (Table S6) as the percentage of respondents who had vaccine safety concerns reduced from 35.7% to 30.7% (aOR: 0.80 [95% CI, 0.65–0.98]). In addition, respondents who were not married or did not have a chronic medical illness were more likely to have lower COVID-19 risk perception.
Discussion
Using a large representative sample, we showed that those who were hesitant to receive the vaccine reported concerns with vaccine safety, considering the risk from COVID-19 was low or felt they did not know enough about the vaccine. The study also presented data from the perspective of parents having their child immunized and found a smaller proportion were very likely to consent to their child being vaccinated compared with the adult population.
Although the willingness to vaccinate has been investigated in Australia and other countries,Citation24–27 the questions, responses, and methods varied between studies and results may not be comparable. However, what is common is the trend of willingness to vaccinate against COVID-19 fluctuating over time.Citation14–17,Citation28–30 This study also showed fluctuating support over the 4-month data collection period. This is mirrored by findings in a longitudinal survey reporting 55% of Australians indicated that they would definitely get vaccinated in April 2021 with a lower rate reported in January 2021 and a higher rate reported in August 2020.Citation16 Previous research showed vaccine willingness decreased except for those living in metropolitan Victoria during the period of the Victorian second lockdown, which may imply that vaccine willingness was associated with environmental factors and the degree of threat experienced during the pandemic.Citation14,Citation31 Vaccine attitudes were also compared prior to and after the COVID-19 vaccine rollout. Although vaccine confidence, perceived disease risk, perceived inadequate information and vaccine effectiveness concerns remained unchanged, vaccine willingness increased, and vaccine safety concerns decreased significantly after the rollout. This may be due to people who were hesitant previously becoming more willing to receive the COVID-19 vaccine with less safety concerns, after an increasing number of their family members and friends had received the COVID-19 vaccine without any major side effects. Safety of COVID-19 vaccines and social norms (e.g. more people getting vaccinated) most likely influence individuals’ intentions to receive a COVID-19 vaccine. Similar to survey findings reported in Australia and other developed countries,Citation16 it appears vaccination has been increasingly accepted as a path out of restriction and confinement with interest in being vaccinated varying alongside key pandemic or vaccine-related events.
Social, attitudinal, political, health, and demographic factors associated with willingness to vaccinate with COVID-19 vaccine have been inconsistently reported and varied between studies. Age, gender, a range of socioeconomic factors, identifying as Aboriginal, health literacy, political affiliations, use of traditional media, chronic illness, levels of religiosity, confidence in government or hospitals, supportive attitudes toward migration, perceived disease severity, trust in science, willingness to vaccinate for influenza, experiences of discrimination and remoteness of residence have been reported to be relevant to COVID-19 vaccine willingness.Citation12,Citation13,Citation15,Citation16,Citation24–30,Citation32–36 This study found that females, unemployed people, low educational attainment, people living in lower socioeconomic areas, and younger people were less willing to be vaccinated. There was also a lower proportion of Aboriginal people who were very likely to be vaccinated, but this did not reach traditional levels of significance, likely due to a small sample size. Further, Aboriginal people were less likely to be very confident about vaccine safety and more likely to have perceived insufficient information about the vaccine. Similar to our study, young age has also been reported to be a significant factor related to low vaccine acceptance in other surveys.Citation28,Citation33 In line with the Australian survey conducted in April and August 2020,Citation29 we did not find an association between chronic disease and the willingness to vaccinate. Interestingly, respondents who were married, had chronic illness, and were employed/retired/students/worked without pay were less likely to perceive low risk of disease, which has not been investigated in previous surveys.
In all, 11% of respondents were not at all confident about vaccine safety and 46% were somewhat confident with only one third being very confident. Vaccine safety concerns were also the top reason why respondents did not choose “very likely” to get vaccinated. Other studies have also shown that vaccine safety may be the most important concern respondents had about COVID-19 vaccine and one of the main reasons for hesitancy of the vaccine.Citation28,Citation33
Around 48% of parents or caregivers indicated that they were very likely to get their children vaccinated in this study. Similar results were reported in Japan and the UK with a higher percentage of respondent’s willingness to get COVID-19 vaccination for themselves than for their children.Citation19,Citation20 One of the main concerns for parents has been the potential side effects of the COVID-19 vaccine.Citation19,Citation20 Previous research has found vaccine acceptance is influenced by vaccine efficacy and perceptions of disease risk. Prior to the Delta and Omicron strain outbreaks, children were reported to have a lower susceptibility to COVID-19. Parents might more often balance the risks and benefits to their child when making a vaccination decision, rather than considering the benefits to communities and society.Citation37 The COVID-19 vaccination program has been extended to all children aged five and over. Monitoring parental willingness would be warranted to modify current vaccination strategies to improve the vaccine coverage rates in children.
This study found little evidence of an increase in any generalized aversion to vaccines,Citation28 with very few vaccine hesitant respondents indicating that they did not believe in vaccinations.
This study has some strengths and limitations. The survey was administered in a representative sample with a large sample size, although it was undertaken in a state with low level of COVID-19 disease. Weighting was applied to the analyses to compensate for the selection of specific observations with oversampling, non-responses, and other types of bias. This is a cross-sectional, and not a longitudinal or repeated survey study. Comparisons between different respondents over time should be interpreted with caution.
The overall effectiveness of the vaccine rollout will depend on the widespread community trust of COVID-19 vaccines. Despite enormous efforts to deliver the COVID-19 vaccine rollout, governments, health professionals, and COVID-19 vaccination providers may need to address vaccine safety concerns by providing evidence-based information, and enhancing vaccine safety messaging in Indigenous languages and languages other than English for migrants, refugees, and other limited-English-proficient populations. Our study also highlights the need for vaccination campaigns targeting healthy populations with young age, female gender, unemployment, and low education and/or socioeconomic level, as well as culturally appropriate information for Aboriginal and Torres Strait Islander people. Future research on a large longitudinal or repeated survey sample is paramount to monitor vaccine willingness, and adjust communication strategies developed for immunization providers and health professionals.
Abbreviations
ABS Australian Bureau of Statistics
COB Country of Birth
SAPHS South Australian Population Health Survey
SEIFA Socio-Economic Index For Areas
Author’s contribution
Conceptualization: H. M., B. W., R. N., K. D, and B. K.; methodology: H. M., B. W., R. N., K. D, and B. K.; formal analysis, B. W. and B. K.; data curation: R. N., K. D, and B. K.; writing-original draft preparation: B. W.; writing-review and editing: H. M., B. W., R. N., K. D, and B. K.
Ethical approval statement
This survey was approved by the Department for Health and Wellbeing Human Research Ethics Committee (HREC/18/SAH/11/AM04).
Supplementary Data
Download MS Word (77.9 KB)Disclosure statement
H. M. is an investigator on vaccine trials sponsored by the GSK group of companies, Pfizer, Sanofi, and Merck. H. M.’s and B. W.’s institution receives funding for investigator-led studies from industry, including Pfizer and Sanofi Pasteur; H. M. and B. W. receive no personal payments from the industry. All other authors report no potential conflicts of interest.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2079345
Additional information
Funding
References
- McIntosh K, Hirsch MS, Bloom A COVID-19: epidemiology, virology, and prevention. Wolters Kluwer, UpToDate; 2022 Mar 1 [accessed 2022 Apr 19]. https://www.uptodate.com/contents/covid-19-epidemiology-virology-and-prevention
- AIHW. 2021. The first year of COVID-19 in Australia: direct and indirect health effects. Cat. no. PHE 287. Canberra:AIHW.
- Chriscaden K Impact of COVID-19 on people’s livelihoods, their health and our food systems. Joint statement by ILO, FAO, IFAD and WHO. WHO; 2020 Oct 13 [accessed 2022 Apr 19]. https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people%27s-livelihoods-their-health-and-our-food-systems
- Viana J, van Dorp CH, Nunes A, Gomes MC, van Boven M, Kretzschmar ME, Veldhoen M, Rozhnova G. Controlling the pandemic during the SARS-CoV-2 vaccination rollout. Nat Commun. 2021 Jun 16;12(1):1. doi:10.1038/s41467-021-23938-8.
- Yamey G, Schaferhoff M, Hatchett R, Pate M, Zhao F, McDade KK. Ensuring global access to COVID-19 vaccines. Lancet. 2020 May 2;395(10234):1405–9. doi:10.1016/S0140-6736(20)30763-7.
- WHO. Weekly epidemiological update on COVID-19 - 27 April 2022. Emergency Situational Updates (Edition 89). WHO; 2022 April 27 [accessed 2022 April 28]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—27-april-2022
- WHO. The Omicron variant: sorting fact from myth. WHO; 2022 Jan 19 [acessed 2022 Apr 19]. https://www.euro.who.int/en/health-topics/health-emergencies/pages/news/news/2022/01/the-omicron-variant-sorting-fact-from-myth
- COVID Live. South Australia daily confirmed cases: COVID LIVE. 2022 April 19 [accessed 2022 April 19]. https://covidlive.com.au/sa
- McBryde ES, Meehan MT, Sziklay J, et al. Vaccination is Australia’s most important COVID-19 public health action, even though herd immunity is unlikely. medRxiv; 2021 [accessed 2022 April 19]. doi:10.1101/2021.07.16.21260642.
- Australian Government Department of Health. COVID-19 vaccine rollout update – 18 April 2022. Commonwealth of Australia, Department of Health; 2022 Apr 18 [accessed 2022 Apr 19]. https://www.health.gov.au/resources/publications/covid-19-vaccine-rollout-update-18-april-2022
- Australian Government Department of Health. ATAGI statement on the Omicron variant and timing of COVID-19 booster vaccination. Commonwealth of Australia, Department of Health; 2021 Dec 24 [accessed 2021 Dec 29]. https://www.health.gov.au/news/atagi-statement-on-the-omicron-variant-and-the-timing-of-covid-19-booster-vaccination
- Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ, Ayre J, Batcup C, Copp T, Cornell S, Dakin T. Sydney Health Literacy Lab-COVID-group. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(3):318–19. doi:10.1016/S1473-3099(20)30559-4.
- Seale H, Heywood AE, Leask J, Sheel M, Durrheim DN, Bolsewicz K, Kaur R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021 Jan 28;21(1):120. doi:10.1186/s12879-021-05833-1.
- To QG, Stanton R, Khalesi S, Williams SL, Alley SJ, Thwaite TL, Fenning AS, Vandelanotte C. Willingness to vaccinate against COVID-19 declines in Australia, except in lockdown areas. Vaccines (Basel). 2021 May 10;9(5):479. doi:10.3390/vaccines9050479.
- Biddle N, Edwards B, Gray M, Sollis K. Change in vaccine willingness in Australia: August 2020 to January 2021. medRxiv; 2021 [accessed 2022 Apr 19]. doi:10.1101/2021.02.17.21251957.
- Biddle N, Edwards B, Gray M, Sollis K. Vaccine willingness and concerns in Australia: August 2020 to April 2021. ANU Centre for Social Research and Methods; 2021 [accessed 2022 Apr 19]. https://csrm.cass.anu.edu.au/research/publications/vaccine-willingness-and-concerns-australia-august-2020-april-2021-1
- Biddle N, Edwards B, Gray M, Sollis K Determinants of COVID-19 vaccination and views of parents about vaccination of children in Australia: August 2021. ANU Centre for Social Research and Methods. 2021 [accessed 2022 Apr 19]. https://csrm.cass.anu.edu.au/research/publications/determinants-covid-19-vaccination-and-views-parents-about-vaccination-children
- Rhodes A, Hoq M, Measey MA, Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(5):e110. doi:10.1016/S1473-3099(20)30724-6.
- Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020 Nov 17;38(49):7789–98. doi:10.1016/j.vaccine.2020.10.027.
- Yoda T, Katsuyama H. Parents’ hesitation about getting their children vaccinated against COVID-19 in Japan. Hum Vaccin Immunother. 2021 Dec 2;17(12):4993–98. doi:10.1080/21645515.2021.1981087.
- The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed. AAPOR; 2016.
- Australian Bureau of Statistics. 2033.0.55.001- Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. Australian Bureau of Statistics; 2018 Mar 27 [accessed 2021 Aug 3]. https://www.abs.gov.au/ausstats/[email protected]/Lookup/by%20Subject/2033.0.55.001 2016 Main%20Features FAQs%20-%20SEIFA%202016 4
- Australian Bureau of Statistics. 1200.0.55.004- Country of Birth Standard, 2012, Version 1.0. Australian Bureau of Statistics; 2012 Sep 26 [accessed 2021 August 3]. https://www.abs.gov.au/ausstats/[email protected]/Lookup/1200.0.55.004main+features42012,%20Version%201.0
- Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel). 2020 Dec 30;9(1):16. doi:10.3390/vaccines9010016.
- Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines (Basel). 2021 Sep 24;9(10):1071. doi:10.3390/vaccines9101071.
- Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021 Apr 8;39(15):2024–34. doi:10.1016/j.vaccine.2021.02.005.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021 Feb 16;9(2):160. doi:10.3390/vaccines9020160.
- Smith DT, Attwell K, Evers U. Support for a COVID-19 vaccine mandate in the face of safety concerns and political affiliations: an Australian study. Politics. 2021:026339572110090. doi:10.1177/02633957211009066.
- Alley SJ, Stanton R, Browne M, To QG, Khalesi S, Williams SL, Thwaite TL, Fenning AS, Vandelanotte C. As the pandemic progresses, how does willingness to vaccinate against COVID-19 evolve? Int J Environ Res Public Health. 2021 Jan 19;18(2):797. doi:10.3390/ijerph18020797.
- Attwell K, Lake J, Sneddon J, Gerrans P, Blyth C, Lee J, Samy AM. Converting the maybes: crucial for a successful COVID-19 vaccination strategy. PLoS One. 2021 Jan 20;16(1):e0245907. doi:10.1371/journal.pone.0245907.
- Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011 Sep 2;29(38):6472–84. doi:10.1016/j.vaccine.2011.06.107.
- Davis SR, Ampon RD, Poulos LM, Marks GB, Toelle BG, Reddel HK. Willingness to receive vaccination against COVID-19: results from a large nationally representative Australian population survey. medRxiv; 2021 [accessed 2022 Apr 19]. doi:10.1101/2021.07.22.21260551.
- Dodd RH, Pickles K, Cvejic E, Cornell S, Isautier JMJ, Copp T, Nickel B, Bonner C, Batcup C, Muscat DM, et al. Perceived public health threat a key factor for willingness to get the COVID-19 vaccine in Australia. Vaccine. 2022 Apr 14;40(17):2484–90. doi:10.1016/j.vaccine.2021.08.007.
- Edwards B, Biddle N, Gray M, Sollis K, Di Gennaro F. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS One. 2021 Mar 24;16(3):e0248892. doi:10.1371/journal.pone.0248892.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021 ;27(2):225–28. doi:10.1038/s41591-020-1124-9.
- Trent M, Seale H, Chughtai AA, Salmon D, MacIntyre CR. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: a comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine. 2022 Apr 14;40(17):2498–505. doi:10.1016/j.vaccine.2021.06.048.
- Paterson P, Chantler T, Larson HJ. Reasons for non-vaccination: parental vaccine hesitancy and the childhood influenza vaccination school pilot programme in England. Vaccine. 2018 Aug 28;36(36):5397–401. doi:10.1016/j.vaccine.2017.08.016.
