 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
The effectiveness of motivational interviewing (MI) for reducing vaccine hesitancy (VH) has been demonstrated in Quebec. We conducted a study to evaluate the acquisition of MI skills after MI training via videoconferencing for interns training as general practitioners (GPs) in southeastern France. A vaccination-specific MI training workshop was offered to interns in 2021, consisting of two separate Zoom videoconference sessions. Participants completed the Motivational Interviewing Skills in Immunization questionnaire before and after the training to measure skills acquisition. We used pairwise exact Wilcoxon-Pratt signed rank tests for the analysis. Among 45 GP interns enrolled in the first MI session, 34 (75.6%) attended both sessions and completed the questionnaire at 3 different time points. After the first session, MI knowledge scores improved significantly (+21.1 ± 21.6; P < .0001), as did application of MI skills (+36.8 ± 36.7; P < .0001), and MI practice confidence (+21.2 ± 11.1; P < .0001). The second MI session maintained the skills developed after the first session without further improvement. Participant satisfaction was high. This is the first study in France assessing the impact of a vaccination-specific MI training for GP interns. It shows a substantial improvement in knowledge, application of MI skills, and self-confidence in the practice of MI. GP interns were highly satisfied with the training despite the videoconference format. These promising results will allow the integration of MI training in GP medical curricula in order to prepare future GPs for communication in the field of vaccination.
Introduction
Since the invention of vaccination by Jenner in the 18th century, vaccines have been a source of debate and controversy. Vaccine Hesitancy (VH) is a growing problem worldwide,Citation1–3 and is considered to be among the 10 most pressing global health threats according to the World Health Organization (WHO).Citation4 The WHO “Behavioral and Social Drivers of Vaccinations” working group has proposed the following definition of VH: “Motivational state of being conflicted about, or opposed to, getting vaccinated; including intentions and willingness;Citation5 VH is complex and context-specific, varying across time, place, and vaccines,Citation6 and is influenced by factors such as complacency, convenience, and confidence.Citation7
VH is particularly prominent in France: in 2018, a study conducted among the 28 countries of the European Union showed that France remained one of the countries with the lowest level of confidence in vaccine safety.Citation8 VH is even more notable in southeastern France where vaccine coverage against COVID-19 and HPVCitation9 is lower than the national average and where general practitioners’ (GPs’) uncertainties about some specific vaccines are most pronounced.Citation10
In an infodemic like the one accompanying the COVID-19 pandemic,Citation11,Citation12 vaccine-hesitant people may have various beliefs and concerns about vaccines, especially related to their safety and usefulness.Citation13–16 They may feel a sense of suspicion toward health authorities and find it difficult to make choices about vaccination.Citation17,Citation18
Mandatory vaccination programs in some countries have not always succeeded in restoring confidence in vaccination.Citation19,Citation20
A Cochrane review of qualitative evidence, assessing parents’ views and experiences of communication about routine childhood vaccination, showed that parents require more information than they actually receive and that simple, context-specific facts should be provided in a timely manner by a trusted health worker.Citation21 Healthcare professionals (HCPs) are the individuals whom the general population trusts most to provide them with information on which they can base their decisions about vaccination.Citation22
Interventions based on providing standardized factual information to individuals in addressing VH Citation23,Citation24 have proven ineffective. A recent narrative review found empirical evidence that the use of a presumptive format to recommend vaccines, motivational interviewing, and tailoring information to increase message salience are approaches that can positively affect vaccine acceptance.Citation25 Vaccination-specific motivational interviewing (MI)-based interventions showed promise as potentially helpful approaches for addressing the concerns of vaccine-hesitant individuals and their vaccination decision-making. MI is a patient-centered communication style used to enhance a person’s internal motivation to change by exploring and resolving their own ambivalences toward their behavioral changes.Citation26 A literature review of publications from the past ten years found only four studies on the impact of HCPs’ MI training on vaccine hesitant patientsCitation27–30 (Appendix A). Of these studies, two looked at the effect of motivational interviewing alone and showed an increase in HCPs’ MI competencies, patients intentions to vaccinate, and patients vaccination coverage.
The PromoVac study in Quebec,Citation31–38 in which MI-trained workers provided information on vaccination to parents during postpartum hospitalization in the maternity ward, demonstrates MI’s effectiveness. Various studies have shown that the use of MI-techniques in this setting result in a 12–15% increase in intentions to vaccinate, a 40% decrease in VH scores, and a 6–7% increase in infant vaccination coverage at seven months postpartum. Since 2018, the PromoVac strategy, now named the EMMIE program, has been expanded to all maternity wards in Quebec province as standard practice, with similar efficacy.Citation39 Accordingly, a vaccination-specific MI-training for HCWs was developed and validated,Citation24 as they are key implementers of vaccination policies and the most influential actors of vaccination intention at the individual patient level.
In France, GPs are the cornerstone of mass vaccination of the population. They are regularly confronted with VH among their patients,Citation40,Citation41 especially regarding COVID-19 vaccines; however, they themselves can be hesitant about certain vaccinesCitation42,Citation43 and rarely receive adequate training in addressing it with their patients.Citation41,Citation44 Therefore, it appeared useful to train GPs with a vaccination-specific MI-training. This training was delivered via videoconference, which, in the context of the pandemic, may prove to be an effective alternative to face-to-face training while enabling compliance with health measures. Initial medical education offers the possibility of a greater uptake of this type of training than continuing education of practicing professionals.
In 2021, we organized a vaccination-specific MI training of interns in their final year of general medicine education. The main objective of the present study was to evaluate the acquisition of MI skills through this training. The secondary objectives were to assess students’ satisfaction, in order to improve the training, and to test the feasibility of providing MI training via videoconference to GP interns in France.
Materials and methods
Participants
A vaccination-specific MI-training workshop was offered at the Marseille and Nice Faculties of Medicine (France) during the academic year of November 2020–November 2021 to GP interns starting their 5th semester, that is, their final year of initial clinical training for internship (after six years of academic medical studies). The MI-training workshop was offered to 70 randomly selected interns. Participation was strictly voluntary but limited to 51 places, so that they could be divided into three training groups of 17 participants at most.
MI-training protocol and curriculum
The MI training curriculum was adapted from a previous vaccination-specific MI training workshop offered to nursing health professionals in Quebec,Citation27 developed by Gagneur et al., who pioneered the PromoVac strategy. This training was associated with the most favorable results in terms of acquisition of skills by the professionals (Appendix A). AG’s team co-adapted this in-person training to a virtual format for French GP interns, with an MI expert (PB), who is a member of the Motivational Interviewing Network of Trainers (MINT). The three days of virtual workshops were conducted by AG and PB.
The vaccination-specific MI training protocol consisted of a workshop spread over three days of meetings with a total of 16 hours of virtual training via Zoom, divided into a 12-hour session divided over two consecutive days in March 2021, followed two months later by a second four-hour session in May 2021, as recommended in the literature for MI training.Citation45 Students were divided into three groups throughout the course. Between the two workshop sessions, the MI expert trainers offered a two-hour coaching session in smaller groups of no more than five participants via Zoom to provide feedback on their MI practice; using, when possible, recordings of their consultations.
The first two-day training session was devoted to discovering the MI philosophy and principles, adapted to VH, and acquiring the five fundamental skills of MI (). The content of this training included MI theory, principles of its adaptation to vaccination, scientific evidence about its effectiveness in reducing VH, and observation of consultations using MI with patients in the maternity ward through filmed interviews. Despite the virtual format, trainees were also able to participate in situational exercises.Citation27
Table 1. The five MI skills.
The two-month interval between the two sessions provided trainees the opportunity to apply and practice their newly acquired MI knowledge and skills in their daily clinical practice with patients. The second half-day training session in May 2021 was devoted to revisiting the MI skills learned during the initial training session, with a supervised group feedback discussion during which participants were invited to share any of the practical challenges encountered with vaccine-hesitant patients, as well as to offer potential techniques to overcome them.
The training material was adapted for the videoconference setting (e.g., trainers had the possibility of breaking trainees into smaller virtual groups with Zoom’s Breakout Rooms feature to facilitate pair-working exercises and role-playing situations).
All examples and situational exercises used in the current training for interns were adapted to target specific vaccines that may be less accepted by the general French population (e.g., the vaccines against COVID-19 and human papillomavirus (HPV) vaccineCitation9).
Training evaluation protocol ()
One week before the first session, a questionnaire was sent to collect participants’ sociodemographic characteristics and their previous experience with training in MI, communication, and vaccination.
We used a pre-/posttest design to assess the effectiveness of the vaccination-specific MI training protocol. This design used the Motivational Interviewing Skills in Immunization (MISI) questionnaire, a validated evaluation tool to assess vaccination-specific MI training (Appendix B).Citation46 Trainees were asked to complete a self-administered online questionnaire at three points in time: before the first training session, immediately after it, and immediately after the second training session. The link to the online pretest questionnaire was sent out by e-mail one week before the training. The MISI requires approximately 15 minutes for completion and assesses three fundamental dimensions of MI learning:Citation47,Citation48 1) acquisition of MI knowledge in multiple-choice questions (6 items); 2) application of MI skills, using first an open-ended situational question, in which the participant must write an MI-consistent dialogue, then a self-report of the frequency of use of MI-compliant and non-MI-compliant behaviors (12 items); and 3) participants’ confidence in applying MI skills in their daily clinical practice (7 items).
In addition, a satisfaction questionnaire was completed at the end of the first training session.
Intercoder reliability for the written open-ended situational item
Coding of the open-ended situational item was blinded to the other coders’ coding and to the pretest or posttest status of the completed questionnaires. First, AG and PB, who previously participated in the development and validation of the MISI questionnaire,Citation46 separately coded the same random selection of questionnaires (15%) (Appendix C). A third, independent evaluator (VG) also coded 15% of the questionnaires. Because intercoder reliability was high, with a mean intraclass correlation coefficient of 0.93, the MINT trainer (PB) coded the remaining questionnaires. The coder identified and scored each MI skill as follows: open-ended question (1 point), reflective listening statement (between 1 and 2 points depending on the complexity level), affirmation statements (1 point) and “elicit-provide-elicit” skill (between 1 and 3 points depending on the completion status). The coder also evaluated the MI-adherence score on a scale from 1 to 5, which assessed the level of MI consistency (closer to 5) or inconsistency (closer to 1) of the participant’s written dialogue.
MISI scoring
The MISI scoring is presented in detail in Appendix D. The total scores obtained for each dimension of the MISI were calculated by summing the responses of the items within that dimension: thus, theoretical totals ranged from 0 to 6 for MI knowledge, from 0 to 12 for MI skills application, and from 7 to 70 for self-confidence in using MI in clinical practice. Each raw total was then linearly transformed to a 0–100 scale, by subtracting from it the observed minimum, dividing the result by the number of items with no missing values, and then multiplying by 100.
For the open-response situational question on the application of MI skills, the total score was calculated by summing the total points attributed for counts of each of the five MI skills and the score for the MI adherence of the participant’s written dialogue. The individual score was not calculated for any dimension of the MISI for which 20% or more of the data for its component items were missing.
Data analysis
Each key dimension of participant MI training was analyzed separately from the others. Scores before and after each training session (1 and 2) were compared in pairs by running exact Wilcoxon-Pratt signed-rank tests. Effect size, reflecting the magnitude of the training session’s effect, was calculated for each dimension, by using the z-score of the signed-rank test as follows: , with n being the number of paired observations.Citation49 Calculating effect size makes it possible to ignore the effects of sample size and score dispersion in considering the strength of the changes: r values between 0 and 0.3 reflect small effect sizes, between 0.3 and 0.5 moderate effect sizes, and between 0.5 and 1 large effect sizes. Analyses were performed with R 4.1.2, and P < .05 indicates statistical significance.
Results
Participants’ characteristics
In all, 45 GP interns registered for and participated in the first (two-day) session of the MI training workshop in March 2021; 64% were women and nearly all (91%) were 25 to 30 years old ( and Appendix E. Some participants had already received training in MI (9%), communications (18%), or vaccination (9%); 38/45 (84%) students participated in the coaching sessions and 35/45 (78%) in the second workshop session. Participant characteristics were not significantly different between interns who attended only the first session and those who attended the entire workshop (Appendix E).
Table 2. Characteristics of participants enrolled for the MI-training.
Effectiveness of the MI training ()
Of the 45 interns enrolled, 43 (96%) and 44 (98%), respectively, completed the MISI before and after the first workshop session. Two months later, all 35 of the interns who participated in the second session completed the MISI afterward. Finally, 34 participants completed the MISI at three points in time. The results are presented for each MISI score in .
Figure 2. Comparison of mean scores of each core aspect of MI training between questionnaires completed before and after the training sessions.
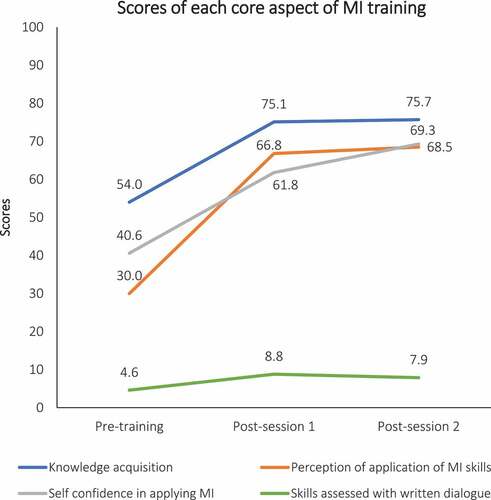
Table 3. Comparison of mean scores of each core aspect of MI training between questionnaires completed before and after the training sessions (exact Wilcoxon-Pratt signed-rank tests).
MI knowledge acquisition
Before the training, the MI knowledge acquisition mean score was 54/100 (±22.2). Comparison of mean scores between questionnaires completed before and after the first session among the 43 participants who completed both of them showed a significant increase in knowledge (+21.1 ± 21.6; P < .0001; ). Compared to the score before the first session, the increase in the MI knowledge acquisition score after the second workshop session (n = 35) was similar (+21.7 ± 17.7; P < .0001) and did not differ significantly from the score observed after the first session ().
Application of MI skills
Before the training, the mean MI application score was 30/100 (±22.7). In comparison with the pre-training questionnaire, the mean score of participants’ self-rated use of MI skills rose significantly after both the first (+36.8 ± 36.7; P < .0001) and second sessions (+38.5 ± 31.9; P < .0001) (). The MI skills score assessed by the written dialogue was 4.6 (±2.8) before session 1 and increased significantly after both sessions 1 and 2 (respectively +4.2 ± 2.9; P < .0001/+3.3 ± 3.2; P < .0001), compared with scores before the workshop ().
Self-confidence in applying MI-related skills
As shown in , participants’ self-confidence in applying MI techniques in clinical practice was 40.6/100 (±10.6) before session 1 and increased after session 1 (+21.2 ± 11.1; P < .0001) and after session 2 (+28.7 ± 25.4; P < .0001), both compared with the corresponding score before the workshop.
Effect sizes of score changes
The effect sizes of all score improvements between pre-session 1 and post-session 1 were large: self-confidence in using MI in clinical practice had the largest effect size (r = 0.87), followed by skills assessed with written dialogue (r = 0.83); it was slightly lower for knowledge acquisition (r = 0.73) and perception of MI-skill application (r = 0.72) (). We found no significant difference between the scores after sessions 1 and 2. The effect size of the score between post-session 2 and post-session 1 for self-confidence in applying MI was moderate (r = 0.31), and it was small for the other dimensions (r ranging from 0.2 to 0.24).
Students’ satisfaction with training
At the end of the two-day session in March 2021, 26/45 (58%) interns completed the satisfaction questionnaire. They reported that they were highly satisfied with the training (they rated it 9.5/10 on average), that it met their expectations (9.5/10); both regarding the MI expert trainers (9.8/10) and the training content (9.3/10). Most (81%) considered the videoconference setting appropriate for the training and did not find that it caused any inconvenience in the management of digital tools. They suggested some improvements: more simulations and practical exercises (i.e. role-playing, work in groups), in-person training, longer and more frequent training sessions, and the possibility for repeat training in the following years (Appendix F).
Discussion
This is the first study in France assessing the impact of a vaccination-specific MI training for GP interns. Our results show a substantial improvement in knowledge acquisition, application of MI skills (perceived and assessed through the written dialogue), and self-confidence in the practice of MI, with a very high level of participant satisfaction. These dimensions are key to both MI learning and training.Citation50 The second MI session helped to maintain the skills developed during the first session but did not further improve them.
Motivational interviewing training for general health care practitioners has been studied over the past 15 years, mainly outside the field of vaccination. In 2011, a literature reviewCitation45 found ten studies published between 1999 and 2009 with a median training time for participants of nine hours. Study quality varied considerably (only four of the studies used the design with the highest validity (level 5 of the Maryland Scale of Scientific Methods: MSSMCitation51 which describes five levels of designs ranked in terms of their ability to handle threats to internal validity). MI training generated positive outcomes overall (basic MI skills, MI spirit, ability to recognize and reinforce change, and rolling with resistance) and had a significant effect on many aspects of participants’ daily practice. Other studies have shown an increase in medical students’ skills due to MI training. A randomized controlled trial at Lausanne Medical School in 2012Citation52 showed an increase of MI performance after an eight-hour MI training workshop. Recently, in 2020, a systematic reviewCitation53 suggested that the implementation of MI curricula in medical schools is feasible and effective, and that it would allow students to achieve beginner levels of proficiency. All of these results support the inclusion of MI in initial medical education curricula. In the specific context of vaccine hesitancy, only four studies were found on MI training for Health Care ProfessionalCitation27–30 (Appendix A).
The results of our study can be compared with those of the study by Gagneur et al. among 34 nurses in Quebec in 2016–2017,Citation27 which was based on a very similar vaccination-specific MI training protocol and the same evaluation tool (MISI). Our results are in line with this study, which was carried out in-person by the same team. The protocol slightly differed from ours with one seven-hour training session over one day and then, three months later, an additional half-day session of four hours. The results showed, after the first session, an improvement in knowledge acquisition (+55%), perceived application of MI skills (+7%), as well as in their application assessed through a written dialogue (+113%), and in self-confidence in MI practice (+8%).Citation27 On this last dimension, however, the increase was less marked than in our study (+53%), which may be explained by the fact that the first training session for interns in France lasted two days (only one day for nurses), which allowed more time to be devoted to MI skill exercises. The results of our study among GP interns in France thus complement and reinforce those of Gagneur et al. among nurses in Quebec.Citation27
The literature points out that MI competencies tend to diminish quickly over time when not applied:Citation54 this is why two sessions are usually recommended, and interns were offered a second session two months after the first training workshop. The second training session was also used to improve knowledge and skills. We did not observe such an improvement in our study, but the scores in post-session 1 — and thus the skills acquired in session 1 — were maintained. Supervised coaching sessions conducted at one month after the first training by PB indicated a lack of opportunities for some interns to use their newly acquired MI skills with vaccine-hesitant patients, and lack of time and/or some difficulties in taking their first steps with patients, which may explain our results. In the study by Gagneur et al. among nurses, differences between post-day 1 and post-day 2 were not marked; but they found a 27% improvement in the perception of MI skill application between the posttests. The participants, who were vaccination nurses working in public health clinics and thus among those performing the vast majority of vaccinations in the province of Quebec, had the opportunity to practice MI after the first training session. This suggests that MI training for GP interns in France should take place when they are present in an internship in a family practice, which is now the rule in France, for at least two semesters, at the end of their internship.
Other studies using MI showed positive results despite shorter training periods than in our study. A brief four-hour MI training program targeting vaccine hesitancy increased MI competency among rheumatology physicians and promoted behavioral change among patients.Citation29 The five MI competencies were evaluated at baseline and post-training with a standardized patient using the Motivational Interviewing Treatment Integrity [MITI] scale. MITI scores increased in this study; however, it involved only seven participants. 71% (n = 5) achieved thresholds of clinical competency post-training. Autonomy/support and empathy competencies reached expected thresholds. Evocation and collaboration competencies improved but without reaching competency thresholds, and direction did not improve. Another communication training in Denver in 2018Citation28 proved to significantly increase HPV vaccine series initiation and completion among adolescent patients. In total, 16 practices and 43,132 patients participated in this trial. The communication training consisted of two and a half hours of communication training (webinar and in-person sessions) on using a presumptive vaccine recommendation as defined by Opel et al,Citation55 followed by motivational interviewing if parents were resistant to vaccination. But the intervention also included four other components: an HPV fact sheet library to create customized information sheets relevant to each practice’s patient population, a tailored parent education website, a set of HPV-related disease images and an HPV vaccine decision aid. It is important to note that skills acquisition was not evaluated specifically regarding MI in this intervention, and that HCPs reported that communication training and the fact sheets were the most useful aspect of intervention components.
As in our study, others have found significant student satisfaction with online education. An online format has proven to be a highly adaptable and acceptable educational tool.Citation56 However, as expressed by the interns in our study, they expect more in-person training and role-playing. Training could therefore be developed that combines face-to-face role-playing and e-learning/webinar sessions.
Our results show that teaching MI is applicable and adaptable to different types of HCPs, in initial training (our study) or continuing education (Quebec study), in face-to-face or distance learning, and in different cultural contexts. Initial training has the advantage over continuing medical education of providing the opportunity to train all members of future cohorts of HCPs at a time when MI skill acquisition is a priori easier – a key element in being able to scale up such a program.
Limitations
The results of this study should be interpreted cautiously, in view of several limitations. Our training was offered on a voluntary basis, and participants may therefore have been more motivated to learn MI than the average trainee. MI is an approach requiring interpersonal skills such as empathy and listening.Citation26 These behavioral skills are not present in everyone equally, are not always encouraged in the initial medical curriculum, and can be more or less difficult to acquire.
Using videoconference for MI training might limit feedback, exchanges, and especially the possibility of role-playing, all of which are important in the acquisition of MI skills.Citation26 During the post-training satisfaction questionnaire, several interns (7/26) reported the need for more practice time with role-playing to become better prepared for practice during consultations.
Evaluation of the application of the MI skills was limited to a written response in the form of an MI-consistent dialogue and participants’ perception of their ability to apply these skills. This is a user-friendly and inexpensive method compared to others that use audio and video recordings, but participant scores for MI skill application, as measured by those two methods, are not necessarily representative of how medical interns would perform MI in a real-life setting with a vaccine-hesitant patient. Nonetheless, results from long-term evaluations of vaccination counselors in the Quebec EMMIE program showed that counselors’ scores were better after six months of practice than post-session 2, demonstrating the sensitivity of the methods used to measure skill improvement (personal data).
There is also a possibility of bias with self-administered online questionnaires due to their variable timing: some participants completed the MISI several days after the sessions and might have sought information from other sources in addition to the MI training we dispensed to answer the questions; however, their number was limited.
The attrition between the two training sessions was moderate (22%): the effectiveness of the MI training might have been slightly overestimated because the students who participated in the second session could have been those who were more enthusiastic about the training and thus more receptive to an enhancement of their MI skills. The comparison of MISI scores (post-session 1) between the ten interns who stopped their training after the first session and the 35 who continued to the end, did not show any significant difference. The data nonetheless show a trend toward lower MISI scores among the ten students who stopped the training (Appendix E).
Conclusion and perspectives
This is the first study in France assessing the impact of a vaccination-specific MI training for GP interns. We found a very significant and positive impact, and demonstrate the feasibility of such an educational training. Participating interns also expressed their high satisfaction with the training and were in favor of continuing the integration of MI training into their courses, in order to promote the acquisition of skills by future general practitioners during initial education.
MI in vaccination shows promise as an approach HCPs could use to establish a dialogue with vaccine-hesitant patients, avoid stigma and polarization, and build/rebuild confidence in vaccination. Our results suggest the ability of MI training for GP interns applied to vaccination to improve MI skills, as least as assessed via the MISI. Moreover, our results show the feasibility of using videoconferencing for this type of training, an important finding at the time of a health crisis that disrupted education. Further research is needed to assess the impact of such training in reducing patients’ VH and improving their vaccine uptake. Moreover, before generalizing MI training in medical curricula, efforts should be devoted to optimizing both the time necessary to train interns and its timing within their academic studies, as well as the most optimal way of providing them with post-training supervision and support. This last aspect is all the more important since MI mastery comes with practice, and difficulties may be encountered in practicing MI particularly at earlier stages of education.
Finally, further research is warranted to compare and/or combine MI with other approaches. Because VH intensity and vaccine concerns vary between patients, personalized approaches are required to address their concerns. MI is, by essence, such an approach, but it also requires that HCPs be equipped to address a variety of vaccine concerns, including knowing how to debunk myths and false information with their patients.
Abbreviations
| GP | = | General practitioner |
| HCP | = | Healthcare professionals |
| HPV | = | Human papillomavirus |
| MI | = | Motivational interviewing |
| MINT | = | Motivational Interviewing Network of Trainers |
| MISI | = | Motivational interviewing skills in immunization |
| SD | = | Standard deviation |
| VH | = | Vaccine hesitancy |
| WHO | = | World Health Organization |
Acknowledgements
We thank the medical interns who participated in this study, Gwenaelle Maradan and Cyril Bérenger for their invaluable help in data collection management and Amanda Garrison for her precise and rigorous proofreading.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Carcelen AC, Prosperi C, Mutembo S, Chongwe G, Mwansa FD, Ndubani P, Simulundu E, Chilumba I, Thuma P, Truelove SA , et al. COVID-19 vaccine hesitancy in Zambia: a glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub-Saharan Africa. Hum Vaccin Immunother. 2022;(Dec 31);18(1):1–14.
- Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013 Aug;9(8):1755–1762. doi:10.4161/hv.25085. Epub 2013 Jun 6.PMID: 23744504 Free PMC article. Review.
- Santhanes D, Wong CP, Yap YY, San SP, Chaiyakunapruk N, Khan TM. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): A scoping review. Hum Vaccin Immunother. 2018;14(1):124–133. doi:10.1080/21645515.2017.1381811.
- World Health Organization. Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- Shapiro GK, Kaufman J, Brewer NT, et al. A critical review of measures of childhood vaccine confidence. Curr Opin Immunol. 2021;71:34–45.
- Zhou M, Qu S, Zhao L, Campy KS, Wang S. Parental perceptions of human papillomavirus vaccination in central China: The moderating role of socioeconomic factors. Hum Vaccin Immunother. 2019;15(7–8):1688–1696. doi:10.1080/21645515.2018.1547605.
- MacDonald NE. SAGE working group on vaccine hesitancy vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–4164. doi:10.1016/j.vaccine.2015.04.036. Epub 2015 Apr 17.
- Larson H, de Figueiredo A, Karafllakis E and Rawal M. European commission report. State of vaccine confidence in the EU 2018. Luxemb Publ Off Eur Union: 2018. © Eur Union 2018 httpseceuropaeuhealthsystemfiles2018-112018vaccineconfidenceen0pdf
- Géodes. Santé Publique France. 2021 Sep 23. https://geodes.santepubliquefrance.fr/#c=indicator&i=vacsi12.couv_complet&s=2021-09-23&t=a01&view=map2
- Collange F, Zaytseva A, Pulcini C, Bocquier A, Verger P. Unexplained variations in general practitioners’ perceptions and practices regarding vaccination in France. Eur J Public Health. 2018;(Aug 6). doi:10.1093/eurpubcky146.
- Ginossar T, Cruickshank IJ, Zheleva E, Sulskis J, Berger-Wolf T. Cross-Platform spread: vaccine-related content, sources, and conspiracy theories in YouTube videos shared in early twitter COVID-19 conversations. Hum Vaccin Immunother. 2022;18(1):1–13.
- Nihal Durmaz & Engin Hengirmen . The dramatic increase in anti-vaccine discourses during the COVID-19 pandemic: A social network analysis of twitter. Hum Vaccin Immunother. 2022;(Dec 31);18(1):2025008. doi:10.1080/21645515.2021.2025008.
- Larson HJ, Gakidou E, Murray CJL. The vaccine-hesitant moment. NEJM. 2022;387(1):58–65. doi:10.1056/NEJMra2106441.
- Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel). 2020 Dec 30;9(1):16. doi:10.3390/vaccines9010016.
- Cascini F, Pantovic A, Al-Ajlouni Y, Failla G, Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. EClinicalMedicine. 2021 Oct;40:101113. doi:10.1016/j.eclinm.2021.101113.
- Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021 Apr 8;39(15):2024–2034. doi:10.1016/j.vaccine.2021.02.005.
- Ward JK, Gauna F, Gagneux-Brunon A, Botelho-Nevers E, Cracowski JL, Khouri C, Launay O, Verger P, Peretti-Watel P. The French health pass holds lessons for mandatory COVID-19 vaccination. Nat Med. 2022 Jan 12; 28(2):232–235. doi:10.1038/s41591-021-01661-7. Online Ahead Print.
- Chi Tam C, Qiao S, Li X. Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Psychol Health Med. 2022 Jan;27(1):150–161. doi:10.1080/13548506.2021.1983185.
- Gualano MR, Olivero E, Voglino G, Corezzi M, Rossello P, Vicentini C, Bert F, Siliquini R. Knowledge, attitudes and beliefs towards compulsory vaccination: a systematic review. Hum Vaccin Immunother. 2019;15(4):918–931. doi:10.1080/21645515.2018.1564437.
- Mignot A, Le Maréchal M, Guimier L, Epaulard O. Mandatory vaccination in France: perception by outpatients and self-evaluation of its impact on their vaccine confidence. Hum Vaccin Immunother. 2021 Nov 2;17(11):4529–4534. doi:10.1080/21645515.2021.1949952.
- Ames HM, Glenton C, Lewin S. Parents’ and informal caregivers’ views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database Syst Rev. 2017;2017(4). doi:10.1002/14651858.CD011787.pub2.
- Oude Engberink A, Carbonnel F, Lognos B, Million E, Vallart M, Gagnon S, Bourrel G. Comprendre la décision vaccinale des parents pour mieux accompagner leurs choix : étude qualitative phénoménologique auprès des parents français. Can J Public Health Rev Can Santé Publique. 20158;106(8):E527–E532. doi:10.17269/CJPH.106.5078. November December.
- Dubé È, Gagnon D, MacDonald NE. SAGE working group on vaccine hesitancy. strategies intended to address vaccine hesitancy: review of published reviews. Vaccine. 2015;33(34):4191–4203. doi:10.1016/j.vaccine.2015.04.041.
- Fokoun C. Strategies implemented to address vaccine hesitancy in France: a review article. Hum Vaccin Immunother. 2018 Jul 3;14(7):1580–1590. doi:10.1080/21645515.2018.1458807.
- Limaye RJ, Opel DJ, Dempsey A, Ellingson M, Spina C, Omer SB, Dudley MZ, Salmon DA, Leary SO. Communicating with vaccine-hesitant parents: a narrative review. Acad Pediatr May-Jun. 2021;21(4S):S24–S29. doi:10.1016/j.acap.2021.01.018.
- Rollnick S, Miller WR, Butler CC. Motivation interviewing in health care: helping patients change behavior. New York: The Guilford Press; 2008.
- Gagneur A, Bergeron J, Gosselin V, Farrands A, Baron G. A complementary approach to the vaccination promotion continuum: an immunization-specific motivational-interview training for nurses. Vaccine. 2019;37(20):2748–2756. doi:10.1016/j.vaccine.2019.03.076.
- Dempsey AF, Pyrznawoski J, Lockhart S, Barnard J, Campagna EJ, Garrett K, Allison Fisher LMD, O’Leary ST, O’Leary ST. Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: a cluster randomized clinical trial. JAMA Pediatr. 2018 May 7;172(5):e180016. doi:10.1001/jamapediatrics.2018.0016.
- Labbé S, Colmegna I, Valerio V, Gosselin Boucher V, Peláez S, Dragomir AI, Laurin C, Hazel EM, Bacon SL, Lavoie KL. Training physicians in motivational communication to address influenza vaccine hesitation: a proof-of-concept study. Vaccines. 2022;10(2):143. doi:10.3390/vaccines10020143.
- Wermers R, Ostroski T, Hagler D. Health care provider use of motivational interviewing to address vaccine hesitancy in college students. J Am Assoc Nurse Pract. 2021 Jan 1;33(1):86–93. doi:10.1097/JXX.0000000000000281.
- Gagneur A, Lemaître T, Gosselin V, Farrands A, Carrier N, Petit G, Valiquette L, De Wals P. A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health. 2018;18(1):11. doi:10.1186/s12889-018-5724-y.
- Gagneur A, Petit G, Valiquette L, De Wals P. 2013. An innovative promotion of vaccination in maternity ward can improve childhood vaccination coverage. governmental report of the promovac study in the eastern townships. Univ Sherbrooke Cent Hosp Univ. Libr Arch Can ISBN 978-2-9813830-0-6 Print Version 978-2-9813830-1-3 PDF Version 112 P.
- Lemaitre T, Carrier N, Farrands A, Gosselin V, Petit G, Gagneur A. Impact of a vaccination promotion intervention using motivational interviewing techniques on long-term vaccine coverage: the PromoVac strategy. Hum Vaccin Immunother. 2019;15(3):732–739. doi:10.1080/21645515.2018.1549451.
- Gagneur A, Gosselin V, Dubé E. Motivational interviewing: a promising tool to address vaccine hesitancy. Vaccine 2018 34 44 6553–6555. doi: 10.1016/jvaccine201710049.
- Gagneur A. Motivational interviewing: a powerful tool to address vaccine hesitancy. Can Commun Rep. 2020;46(04):93–97. doi:10.14745/ccdr.v46i04a06.
- Gagneur A, Lemaître T, Gosselin V, Farrands A, Carrier N, Petit G, Valiquette L, De Wals P. Promoting vaccination at birth using motivational interviewing techniques improves vaccine intention: the PromoVac strategy. J Infect Ther. 2018:65379. doi:10.4172/2332-0877.1000379.
- Gagneur A, Battista MC, Boucher FD, Tapiero B, Quach C, De Wals P, Lemaître T, Farrands A, Boulianne N, Sauvageau C, et al. Promoting vaccination in maternity wards – motivational interview technique reduces hesitancy and enhances intention to vaccinate, results from a multicentre non-controlled pre- and post-intervention RCT-nested study, Quebec, March 2014 to February 2015. Euro Surveill. 2019;24(36):1800641. doi:10.2807/1560-7917.ES.2019.24.36.1800641.
- Gagneur A, Quach C, Boucher FD, Tapiero B, De Wals P, Farrands A, Lemaitre T, Boulianne N, Sauvageau C, Ouakki M, et al. Promoting vaccination in the province of Québec: the PromoVaQ randomized controlled trial protocol. BMC Public Health. 2019;19(1):160. doi:10.1186/s12889-019-6468-z.
- Gagneur A. 2019. Increasing immunization coverage by strengthening the decision-making process of parents through motivational interviewing intervention in maternity wards: the EMMIE program. Abstract.
- Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, Verger P. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk–benefit balance. Euro Surveill. 2018;23(17). Apr231717-00816. doi:10.2807/1560-7917.ES.2018.23.17.17-00816.
- Kernéis S, Jacquet C, Bannay A, May T, Launay O, Verger P, Pulcini C. Vaccine education of medical students: a nationwide cross-sectional survey. Am J Prev Med. Pii S0749-37971730020-X. doi:10.1016/j.amepre.2017.01.014.
- Verger P, Scronias D, Dauby N, Awoenam Adedzi K, Gobert C, Bergeat M, Gagneur A, Dubé E. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020 Euro Surveill. Euro Surveillance : Bulletin Europeen Sur Les Maladies Transmissibles = European Communicable Disease Bulletin. 2021 Jan;26(3):2002047. doi:10.2807/1560-7917.ES.2021.26.3.2002047.
- Verger P, Botelho-Nevers E, Garrison A, Gagnon D, Gagneur A, Gagneux-Brunon A, Dubé E. Vaccine hesitancy in health-care providers in Western countries: a narrative review. Expert Rev Vaccines. 2022 Mar 22;0(0):1–19.
- Lepiller Q, Bouiller K, Slekovec C, Millot D, Mazué N, Pourchet V, Balice R, Garrien-Maire F, Simon E, Wintenberger V, et al. Perceptions of French healthcare students of vaccines and the impact of conducting an intervention in health promotion. Vaccine. 2020 Oct 7;38(43):6794–6799. doi:10.1016/j.vaccine.2020.08.036.
- Söderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns. 2011;84(1):16–26. doi:10.1016/j.pec.2010.06.025.
- Gagneur A, Gosselin V, Bergeron J, Farrands A, Baron G. Development of motivational interviewing skills in immunization (MISI): a questionnaire to assess MI learning, knowledge and skills for vaccination promotion. Hum Vaccin Immunother. 2019;15 (10): 1–7. doi:10.1080/21645515.2019.1586030.
- Madson MB, Loignon AC, Lane C. Training in motivational interviewing: a systematic review. J Subst Abuse Treat. 2009;36(1):101–109. doi:10.1016/j.jsat.2008.05.005.
- Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs: the four levels. San Franc (CA) Berrett-Koehler; 2006. https://www%20AspresolvercomaspresolveraspBIZP2341903
- Tomczak M, Tomczak E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014;1(21):19–25.
- Baer JS, Rosengren DB, Dunn CW, Wells EA, Ogle RL, Hartzler B An evaluation of workshop training in motivational interviewing for addiction and mental health clinicians. Drug Alcohol Depend. 2004;73:99–106.
- Wells K, Littell JH. Study quality assessment in systematic reviews of research on intervention effects. Res Soc Work Prac. 2009;19(1):52–62. doi:10.1177/1049731508317278.
- Daeppen J-B, Fortini C, Bertholet N, Bonvin R, Berney A, Michaud P-A, Layat C, Gaume J. Training medical students to conduct motivational interviewing: A randomized controlled trial patient education and counseling. 2012 June;87(3):313–318. doi:10.1016/j.pec.2011.12.005.
- Kaltman S, Tankersley A. Teaching motivational interviewing to medical students: a systematic review academic medicine. Acad Med. 2020 mars;95(3):458–469(12). doi:10.1097/ACM.0000000000003011.
- Walters ST, Matson SA, Baer JS, Ziedonis DM. Effectiveness of workshop training for psychosocial addiction treatments: a systematic review. J Subst Abuse Treat. 2005;29(4):283–293. doi:10.1016/j.jsat.2005.08.006.
- Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Salas HS, DeVere V, Zhou C, Robinson JD. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037–1046. doi:10.1542/peds.2013-2037.
- Cates JR, Diehl SJ, Fuemmeler BF, North SW, Chung RJ, Forcina Hill J, Coyne-Beasley T. Toward optimal communication about HPV vaccination for preteens and their parents: evaluation of an online training for pediatric and family medicine health care providers. J Public Health Manag Pract. 2020 Mar/Apr;26(2):159–167. doi:10.1097/PHH.0000000000001022.
Appendix Appendix A.
Review of literature about motivational interviewing training for health care professional
Appendix B:
The MISI (Motivational Interviewing Skills in Immunization) questionnaire
Date : _____________
Caractéristiques du répondant
Sexe du répondant : ◽ H ◽ F
Année de naissance du répondant:
1.Sélectionnez les 3 facteurs déterminants dans le changement de comportement d’une personne selon l’entretien motivationnel.
◽ (Veuillez choisir au moins une réponse)
◽ La confiance en ses capacités de changer
◽ La pression pour changer
◽ L’importance accordée au changement
◽ Les récompenses et les plaisirs anticipés
◽ Être prêt au changement
2.Quels sont les savoir-faire essentiels utilisés en entretien motivationnel ?
(Veuillez choisir une réponse)
◽ Conseils, directives, reflets, questions ouvertes, résumés
◽ Questions ouvertes, valorizations, reflets, résumés, partager de l’information
◽ Questions ouvertes, conseils, reflets, informations, résumés
◽ Questions ouvertes, reflets, valorizations, conseils, informations
3.Selon les principes de l’entretien motivationnel, laquelle de ces attitudes préconisez-vous devant une personne hésitante ?
(Veuillez choisir une réponse)
◽ Donner des conseils sur les recommandations vaccinales
◽ Encourager le parent dans sa réflexion même s’il ne fera pas vacciner son enfant
◽ Expliquer les risques de la non-vaccination
◽ Argumenter en faveur des avantages de la vaccination
4.En respectant l’esprit de l’entretien motivationnel, quelle serait la meilleure réponse au propos suivant : « Il y a de plus en plus de vaccins. Donner tous ces vaccins en même temps à un bébé si jeune, ce n’est pas possible pour moi » ?
(Veuillez choisir une réponse)
◽ Pourtant, ce sont les recommandations du calendrier de vaccination
◽ C’est pour vous éviter de revenir plusieurs fois, ainsi c’est plus facile pour vous
◽ Vous êtes effrayé à l’idée de donner autant de vaccins à votre nourrisson
◽ C’est difficile pour vous mais c’est la seule façon de bien protéger votre bébé
5.Quelles sont les 4 attitudes composant l’esprit de l’entretien motivationnel?
(Veuillez choisir une réponse)
◽ Expertise, conseil, directivité, empathie
◽ Partenariat, évocation, non-jugement, altruisme
Empathie, sincérité, enthousiasme, accompagnement
◽ Jugement, conseils, dynamisme, ouverture
6.Quelle serait la meilleure réponse au propos suivant : « Pourquoi ma fille de 9 ans devrait-elle recevoir le vaccin contre le VPH? Elle n’a même pas encore de relation sexuelle. »
(Veuillez choisir une réponse)
◽ Parce qu’il est recommandé de recevoir le vaccin à cet âge, il est plus efficace lorsque la personne n’est pas déjà infectée. C’est donc préférable de recevoir le vaccin avant d’avoir des relations sexuelles. Qu’en pensez-vous?
◽ Vous vous demandez pourquoi le vaccin est recommandé aussi jeune. Je vais vous donner de l’information concernant l’âge d’administration du vaccin et vous allez comprendre.
◽ Selon vous, quelles pourraient être les raisons pour que le vaccin soit recommandé à cet âge?
◽ Si le vaccin est inscrit au calendrier vaccinal, c’est qu’il est sûr et efficace. Inutile de vous inquiéter, ce sont les recommandations du calendrier de vaccination. Il est donné au meilleur moment pour la santé de votre fille, cela va lui éviter d’être infectée.
7.Dans la mise en situation, imaginez et écrivez de façon précise et concrètele dialogue que vous pourriez mettre en place avec votre client en utilisant les savoir-faire de l’entretien motivationnel (entre 10 et 15 lignes). Exemple :
Moi : « … »
Parent :
« … »
Moi : « … »
Mise en situation : Vous êtes vaccinateur. Vous recevez Nathalie pour la vaccination HPV de sa fille Mathilde. Elle vous exprime qu’elle ne souhaite pas que celle-ci reçoive le vaccin car elle a entendu des informations sur des risques de mort subite après ce vaccin. Que lui répondez-vous?
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
9.Pour chacun des énoncés suivants, indiquez sur l’échelle de 1 à 10 la valeur qui reflète le mieux votre perception en ce qui a trait à l’entretien motivationnel.
1) À combien situez-vous votre niveau de confiance à poursuivre la pratique de l’entretien motivationnel dans votre contexte professionnel ?
2) À quel point est-ce facile pour vous d’échanger avec un client plutôt fermé à certains vaccins ou à la vaccination en général ?
3) À quel point vous sentez-vous confiant(e) de pouvoir écouter avec empathie un patient fermé à la vaccination?
4) À quel point vous sentez-vous confiant(e) de plutôt poser des questions ouvertes ?
5) À quel point vous sentez-vous confiant(e) de pouvoir refléter la réalité du parent ?
6) À quel point vous sentez-vous confiant(e) de pouvoir influencer la discussion vers le changement ?
7) À quel point vous sentez-vous outillé(e) pour mener un entretien motivationnel en immunisation?
Nous vous remercions de votre précieuse collaboration, soyez assurées de la confidentialité des données recueillies.
Appendix C:
Intercoder reliability for the written open-ended situational item
Appendix D:
Scoring the MISI
“Don’t know” answers and refusals were considered as missing values.

