ABSTRACT
With the advancement of the “internet plus” action plan in China, the electronic information system and the mobile phone applications (APPs) are widely used in the management of expanding national program of immunization (EPI). To estimate the use of childhood vaccination APP to improve migrants’ vaccination knowledge, attitude and practice (KAP), a community trial toward migrant children was carried out in Chongqing, China. Migrant children were divided into two groups, one group was provided with health education and vaccination reminders in manual way and the other group was provided with online health education and vaccination reminders by mobile APP. After seven-month interventions, a total of 196 guardians of migrant children aged 2 months to 2 y participated in the questionnaire survey. There were significant differences between two groups in the awareness of vaccine policy, disposal of adverse reaction and attitude toward vaccination. Few significant differences in vaccination coverage of children ≤12 months between two groups, except 2ndbOPV and 2ndMenA. The timely vaccination rate of children >6 months in the APP group ranged from 37.5% to 68.2%, that was from 0% to 30.5% in the non-APP group (P < .05). Most migrant children above 6 months had vaccination within a month after due day in the APP group, while that was at least 3 months after due day in the non-APP group. The vaccination APP greatly improved migrants’ KAP on vaccination. Continuous and systematic intervention by vaccination APP would play a more critical role in the vaccination behaviors of older migrant children.
Background
Internal migrant population in China has been rising rapidly because of the rapid development of the city. The Chinese Census showed that there were 34.3 million migrant children in 2015.Citation1In 2017 and 2018, China had about 240 million migrants every year.Citation2,Citation3
Vaccination of migrant children is a major potential safety hazard that directly affects vaccination coverage in China.Citation4–8 Apart from failing to ensure the immunity of migrant children against infectious diseases, it poses a certain threat to the health of local children and affects the development and effectiveness of prevention and control of various infectious diseases.Citation9–12
China has been reforming the health system, revising immunization policies, implementing the EPI plan (expanding national program of immunization) to solve the serious vaccination issues of migrants.Citation13–17 Now migrant children in China enjoy the same vaccination services as local resident children.Citation18–20 Although the government has strengthened the active search and invested a large amount of manpower and resources in community management for migrants, the immunization coverage and timely vaccination of migrants were still not ideal.Citation21,Citation22
There were about 270,000 routine vaccination clinics in China, and their EPI management systems were undergoing construction and transformation. The vaccination data (vaccine name, vaccination site/date, etc.) were digitized on line instead of paper. Furthermore, information system of client-side and mobile phone application (APP) would promote management by providing with health knowledge, vaccination appointment services, etc.Citation23 instead of tedious manual registration and notification.
Chongqing, the youngest and the most dynamic municipality in China, attracts a large number of migrants every year, with the floating population accounting for about 20%. In 2019, there were 2.27 million children aged 0–6 y in Chongqing, among which migrant children accounted for 25.3%. Jiulongpo district, one of the largest floating population in Chongqing, has 46.8% of migrant children aged 0–6 y.Citation24,Citation25 Data from a clinic baseline survey of child vaccination rates in JLP district showed that most vaccines had 80%–100% coverage and a very few had 40% coverage among resident children. However, most vaccination rates among migrant children were only from 10% to 50%. In particular, the coverage rate for 2nd JE-L, 4th DPT and 3rd DPT was only 10%.
To assess the use of vaccination APP on promoting migrants’ vaccination behavior, knowledge and attitude, a community trial study on childhood vaccination APP was carried out in Jiulongpo District among migrant children aged 2 months to 2 y old, which lasted for 7 months. It is important to summarize experiences and lessons from immunization management for migrant children, which will provide valuable experiences to other developing countries with large migrant population.
Methods
Study design
From July 1st 2019 to January 31st 2020, a vaccination intervention basing on mobile application was conducted in JLP district of Chongqing to analyze the changes of vaccine knowledge and behaviors among caregivers who took migrant children vaccinated in survey clinics.
Migrant children referred to children whose household registration were in foreign districts and who had lived temporarily with their parents or other caregivers in JLP district. After consulting the child’s registration books and asking the child’s family residence, we identified respondents. The guardians of migrant children aged 2 months to 2 y who had brought children to take inoculations for times were invited to participate in our study by convenience sampling. Nannies were excluded from our study.
Interventions
Sample size was calculated based on an assumed awareness rates of 91%,Citation26–30 error margin (two-sided) of ±12%, α of 0.05. The sample was further inflated by approximately 10% to account for potential non-response, which resulted in a final sample size of 246.
We investigated eight vaccination clinics located in JLP district with most floating population. The 8 clinics were divided into the APP group (mobile phone groups) and the non-APP group (traditional education groups) on average by the random number table. The sample size for each group was 123.
In the APP group, we installed a vaccination APP in guardian’s smart phone. Doctors in clinics released vaccination messages to migrant guardians through APP application terminal, including vaccine knowledge, real-time vaccine stocks, disposal of adverse reactions after inoculation, reminder, etc. Meanwhile, guardians could not only make inoculation appointments by APP but timely consult doctors by APP. If children missed the appointments, their guardians would get reminders from APP.
In the non-APP group, guardians received vaccination information as usual. Doctors distributed posters or leaflets about vaccine knowledge and conducted face-to-face consultations for health problems. Doctors made an appointment to the next inoculation by writing down the next vaccination date on children’s vaccination registration book. If children missed inoculation for a few of weeks, doctors would give one reminder call to guardians.
Survey
After seven-month interventions, we administered a questionnaire survey to the guardians whose children had been vaccinated in the eight clinics more than once. The questionnaire was presented in Chinese. According to literature on the vaccine acceptance in China and United States, the contents of our questionnaire included items on demographic information (gender, age, occupation, education background), attitude, knowledge and behavior toward vaccination. Guardian’s knowledge about vaccine policy, dealing with adverse reactions and attitude were also listed in questionnaire. The vaccine policy of 11 routine vaccines was asked in the questionnaire. The vaccination rates of 18 doses of compulsory vaccine for children aged 2 months to 2 y were also investigated () in our study. The coverage rate was calculated by consulting the children’s vaccination record book. Vaccination of children within one month of the scheduled time for vaccination is judged to be timely vaccination. An informed consent was obtained from subject before enrollment. Personal information such as names and phone numbers of all respondents was covered up in questionnaires.
Table 1. Schedule of EPI vaccines from 2016 to 2019 in Chongqing.
Statistical analyses
Guardian’s awareness of vaccine knowledge, simple side reaction post-inoculation treatments, children’s vaccination coverage and children’s timely vaccination after interventions were assessed separately for two groups. Questions about guardian’s vaccine knowledge were collapsed into dichotomous responses (correct/wrong). Response with an option of “I don’t know” was coded as a false answer for the question. Question about attitudes toward vaccination had five options, “strongly agree” and “agree” were coded as positive attitudes, “neither disagree nor agree,” “disagree” and “I don’t know” were coded as negative attitudes. Statistical tests were performed using SPSS 23.0 software. Chi-square test or Fisher’s exact tests were used to determine the difference of groups. P-values less than 0.05 were considered to be significant.
Results
Different interventions between the two groups
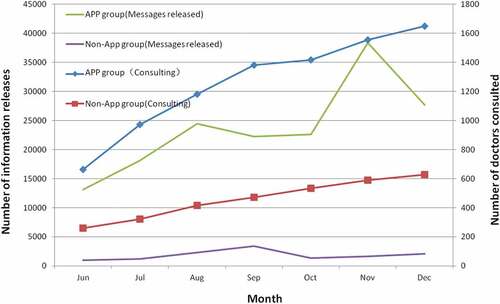
During the interventions, there were 166571 messages released by the vaccination clinics through APP application terminal, which was nearly 13 times as many as the messages released by traditional promotion in non-App group. There were 8819 person-times of consultations by guardians through APP, which was 3223 times of guardians in non-App group ().
Demographic characteristic and vaccine knowledge
We received a total of 196 complete questionnaires with 80% response rate, 90 in non-APP group and 106 in APP group (73.2% vs 86.2%). There was a significant difference in the response rate between two groups (P = .011). A 53.1% of guardians were junior or senior school educated, 84.7% were female, and 37.8% were unemployed. A 46.4% of guardians were aged under 30 y, 26.5% were 30–40 y old, 5.6% were 41–50 y old and 20.4% were above 50 (). Subjects’ demographics were well balanced between two groups in gender, age, education and occupation (P > .05).
Table 2. Demographic sociology information of migrant children.
Overall, less than 50% of guardians clearly knew the vaccine classification policy, with 15.6% in the non-APP group and 44.3% in the APP group, respectively (P = .000). A 95.9% of guardians knew that children should be kept for 30 minutes after vaccination, with 99.1% in the APP group and 92.2% in the non-APP group (P = .016). A 62.8% and 48.47% of guardians knew how to correctly treat fever and redness, respectively. Totally, 90.8% of guardians had a positive attitude toward vaccination, which was significantly different between non-APP group (84.4%) and APP group (96.2%) (P = .004) ().
Table 3. Guardian’s knowledge and attitude about vaccination.
Vaccination uptake
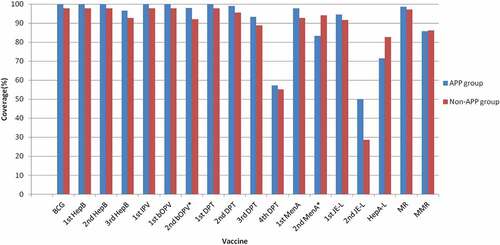
Most vaccination rates were above 90% among children under 9 months, which were slightly higher than children over 9 months (). There was no significant difference in vaccination coverage between APP group and non-APP group except for 2ndbOPV and 2ndMenA.
To further understand the vaccination behavior of migrant children, we compared the distribution of inoculation interval in two groups. Because child under six months was vaccinated intensively, we selectively analyzed the vaccination behavior of child above 6 months in two groups (1st MenA, MR, 1st JE-L, 2nd MenA, 4th DPT, MMR, 2nd JE-L, HepA-L). The result shew the distribution of inoculation interval was significantly different between two groups (P < .05) except for 4th DPT and HepA-L. Most migrant children above 6 months in the APP group got vaccinations on time, often within a month of their appointment. While the children in the non-APP group mostly delayed vaccination, often three months or more after the scheduled date (), especially MR, 2nd MenA, MMR and 2nd JE-L.
Table 4. Timely vaccination coverage of migrant children.
Table 5. The distribution of vaccination delay in migrant children.
Discussion
In this study, we found the long-term caregivers of migrant children had some common characteristics, young, poorly educated and jobless. Their limited social circle led to few accesses to new health information, and their health knowledge mainly from doctors.Citation31–34 Doctors are the key factor influencing the public’s believe on immunization and behavior of vaccination.Citation35–37 In fact, there is not enough time for clinic doctors to introduce vaccine knowledge in detail one by one. Usually, clinics with a large floating population see 100 to 200 children a day in Chongqing. Therefore, the usage of APP has become an important tool for vaccination clinics to carry out education, which can not only spread vaccination knowledge through medical staffs but also save manpower.
On the other hand, 20.4% of the caregivers were above 50 y old, who had difficulty in using the mobile phone APP. So clinics should seize the opportunity of parental first registration in clinic to introduce the vaccination APP and then let parents teach caregivers how to continuously use the APP.
Comparing the amount of information released by clinics and the frequencies of consultation in two groups, we found there were more opportunities for parents or caregivers to communicate with doctors in App group than that in non-APP group. It is suggested that migrant parents were in great demand for vaccination knowledge, and the traditional interventions could not meet parents’ needs. Moreover, the accessibility of education by doctor face-to-face was poorer than that by APP, which was more convenient and more timely.
Overall, the guardian’s awareness rate of vaccine knowledge was very low in non-APP group. Although they held a positive attitude toward vaccination, children in non-APP group still show poorer compliance in timely vaccination than children in APP group, which was the same as the studies in India and Rwanda.Citation38,Citation39APP group had more positive attitudes toward vaccination, which was affected by their better awareness about immunization and vaccine.Citation40–44 Mobile APP has built a flexible channel for doctors to deliver health information to parents. It also provides a good communication platform for timely updating information and releasing vaccination reminders, which is not limited by parental visiting time or the information loss. Therefore, migrants in APP group got more flexible chances to receive health education than non-APP group, which improved guardians’ positive attitude toward vaccination.
The vaccination rate of children decreased with the increase of age and dose. It is reported that the vaccination coverage was <50% for the first dose in migrant children aged 0–4 y and <25% for the second dose in Greece.Citation45 Children ≤2 y should receive 18 doses of routine EPI vaccines in China.Citation18 Our study also show the vaccination rate of the first dose was higher than that of subsequent ones in both two groups, which were inversely related to age. So, it is suggested that we should focus on the vaccination of older children and multiple doses of the vaccine. After the APP intervention, 11 doses of vaccine coverage rate were above 95% for migrant children aged 0–8 months, which was higher than the data of other provinces in China without APP interventions,Citation46–49 5 doses of routine vaccines coverage were from 80% to 95%, and the last 2 doses (4th DPT and 2nd JE-l) of routine vaccines were about 50%, which were separately injected at 18 months and 24 months. In the non-APP group, only eight doses of vaccine coverage were above 95%, which were mostly for 0–5 months children. And the coverage of 2nd JE-l was lowest to 28.6% in the non-APP group. Totally, the vaccine coverages of 3rd polio vaccine, 2nd MenA and 2nd JE-l were significantly different between two groups. Children aged 0–8 months in the App group finished the vaccination schedule better than children in the non-APP group. The usage of APP can effectively improve the vaccination compliance of migrant children.
According to Chinese vaccination schedule, the number of injection decreases after 6 months of age. The visiting time of guardian’s going to clinics turns more sparse with age, which influences guardian’s chance to learn knowledge from doctors. We found it was significantly different of children’s vaccination interval among the children ≤12 months between two groups. Children ≤12 months in the APP group usually timely vaccinated within one month of the scheduled time, which reduced the risk of diseases infection. It was possible owing to the appointment reminder of mobile APP. While there were no differences of the distributions of vaccination interval in 4th DPT, 2nd JE-L and HepA-L between two groups. It might be that children over nine months were vaccinated at least six months from last vaccination, so the seven-month interventions involved in the study might not work. These results suggest that vaccination APP with the function of reminder, information delivery and consultation can indeed improve the vaccination compliance of migrant children, but the interventions should last for a long-term more than the interval between the two doses.
This study also has some limitations. Firstly, the childhood vaccination APP intervention lasted only seven months. Although we found obvious improvements on knowledge, attitude and behavior of migrant children under 12 months, few differences in timely vaccination among children aged above 12 months were observed. In addition, it was a current situation survey, not all the respondents had received a complete seven-month intervention. Secondly, during the intervention period, subjects might be influenced by vaccine knowledge released by other public channels, such as Internet, television and so on. Thirdly, the response rate of the questionnaire survey was 80%. This was related to the fact that the respondents were partly over 50 y old, and their questionnaire cooperation was not high. However, the results positively support continuous use of childhood vaccination APP among migrants.
Conclusion
Vaccination clinics integrating vaccination information system and vaccination APP can easily realize health education, vaccination reminder, online appointment, information exchange and so on. The usage of vaccination APP increases timely vaccination rate and optimizes the service efficiency compared to the traditional way, especially it is good for managers to manage migrants timely and accessibly. Crucially, APP intervention needs to be sustained a long time period so that timely vaccination rate among migrant children can eventually improve.
Ethical approval
All procedures involving human in this study were granted by the Ethical Committee of Chongqing CDC. Written informed consent was obtained from the legal guardians of the children before enrollment.
Abbreviations
APPApplication of mobile phone;
EPIExpanding national program of immunization
HepBHepatitis B vaccine
BCGBacille Calmette-Guérin vaccine
IPVInactivated polio vaccine
bOPVBivalent polio attenuated live vaccine
DTaPDiphtheria-tetanus-acellular pertussis vaccine
MRCombined measles and rubella vaccine
MMRMeasles, Rubella and Mumps Combined Vaccine
JE-LJapanese encephalitis attenuated live vaccine vaccine
MenAEpidemic cerebrospinal meningitis group A polysaccharide vaccine
HepA-LLive attenuated hepatitis A
Acknowledgments
We thank the staffs in the eight vaccination clinics in Jiulongpo district for conducting volunteer enrollment and questionnaire collection.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- UNICEF. Figure 10.3 number of migrant children, by province, 2015[EB/OL]. [ accessed 2022 Apr 15]. https://www.unicef.cn/en/figure-103-number-migrant-children-province-2015.
- Jizhe N. China statistical yearbook 2019[M]. West San Huan South Road, Fengtai District, Beijing: National Bureau of Statistics; 2019.
- Commission G O O N. Summary of “China’s migrant population development report 2018”[EB/OL]. [ accessed 2022 Apr 15]. http://www.nhc.gov.cn/wjw/xwdt/201812/a32a43b225a740c4bff8f2168b0e9688.shtml.
- Hu Y, Chen Y, Liang H, Wang Y. Analysis of the effects of individual- and community- level predictors on migrant children’s primary immunization in Yiwu city, east China[J]. Hum Vaccin Immunother. 2018;14(9):2239–8. doi:10.1080/21645515.2018.1467684.
- Lin S, Jing Z, Howard N. Associations of elements of parental social integration with migrant children’s vaccination: an epidemiological analysis of national survey data in China[J]. Vaccines (Basel). 2021;9(8 884).
- Wang J. Current situation and intervention strategies of KAP vaccination for guardians of migrant children aged 2-4 years old[J]. J Dis Monit Control. 2020;14:94–96.
- Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J, Zhang B. Does introducing an immunization package of services for migrant children improve the coverage, service quality and understanding? An evidence from an intervention study among 1548 migrant children in eastern China[J]. BMC Public Health. 2015;15(1):664. doi:10.1186/s12889-015-1998-5.
- Lv H, Zheng H, Li J. Effect evaluation of immunization program intervention mode for floating children in Foshan,Nanhai[J]. South China J Prev Med. 2021;47(7):902–05.
- Honghong C, Liping Z, Hualin S. Epidemiological characteristics of measles outbreaks in international schools in Minhang district, Shanghai, 2019 [J]. Dis Surveill. 2021;36(7):734–38.
- Li Z, Pei YR, Liang ZZ. Study on the immunization coverage rate and its influential factors among floating children in Chengdu[J]. Modern Prev Med. 2016;43:1405–08.
- Armitage AJ, Heys M, Lut I, Hardelid P. Health outcomes in international migrant children: protocol for a systematic review[J]. BMJ Open. 2021;11(5):e41173. doi:10.1136/bmjopen-2020-041173.
- Fahrni O, Posfay-Barbe KM, Wagner N. Immunization against hepatitis A in migrant children: three vaccination strategies, a retrospective study[J]. Pediatr Infect Dis J. 2020;39(2):164–69. doi:10.1097/INF.0000000000002526.
- Hu Y, Li Q, Chen E, Chen Y, Qi X. Determinants of childhood immunization uptake among socio-economically disadvantaged migrants in East China[J]. Int J Environ Res Public Health. 2013;10(7):2845–56. doi:10.3390/ijerph10072845.
- Kusuma YS, Kaushal S, Sundari AB, Babu BV. Access to childhood immunisation services and its determinants among recent and settled migrants in Delhi, India[J]. Public Health. 2018;158:135–43. doi:10.1016/j.puhe.2018.03.006.
- Han K, Zheng H, Huang Z, Qiu Q, Zeng H, Chen B, Xu J. Vaccination coverage and its determinants among migrant children in Guangdong, China[J]. BMC Public Health. 2014;14(1):203. doi:10.1186/1471-2458-14-203.
- Sun M, Ma R, Zeng Y, Luo F, Zhang J, Hou W. Immunization status and risk factors of migrant children in densely populated areas of Beijing, China[J]. Vaccine. 2010;28(5):1264–74. doi:10.1016/j.vaccine.2009.11.015.
- Fang H, Yang L, Zhang H, Li C, Wen L, Sun L, Hanson K, Meng Q. Strengthening health system to improve immunization for migrants in China[J]. Int J Equity Health. 2017;16(1):19. doi:10.1186/s12939-016-0504-8.
- National C G O O. Notice on issuing the standard for vaccination work[S]; 2016.
- Peng Z, Qiao S, Ming SX, Quan, LJ, Min, ZY, et al. Immunization status of migrant children aged 0 to 7 years[J]. Modern Prev Med. 2017;44(15):2765–67.
- Chunxi D, Yuhua S, Jinxin L, Ding, CX, Shen, YH, Lu, JX, Huang, J, et al. Evaluation on the effect of immunization program management for migrant children in Jiashan[J]. Chin J Public Health. 2014;30(8):1106–07.
- Wilson K, Atkinson K, Deeks S. Opportunities for utilizing new technologies to increase vaccine confidence[J]. Expert Rev Vaccines. 2014;13(8):969–77. doi:10.1586/14760584.2014.928208.
- Larson HJ. Negotiating vaccine acceptance in an era of reluctance[J]. Hum Vaccin Immunother. 2013;9(8):1779–81. doi:10.4161/hv.25932.
- Shicheng G, Xiaobo C, Yuqin Z. Construction and application of the integrated immunization program information management based on a cloud platform in Jiangxi province[J]. Chin J Vaccines Immun. 2022;28(1):110–14.
- Chongqing Municipal Bureau Of Statistics. 2021. NBS survey office in Chongqing. Chongqing statistical yearbook 2020[M]. West San Huan South Road, Fengtai District, Beijing: China Statistics Press.
- Jiulongpo,Chongqing Bureau of Statistics. The seventh national population census communique of Jiulongpo, Chongqing[EB/OL]. [2021 Nov 17]. http://cqjlp.gov.cn/bmjz/qzfbm_97119/qtjj_97732/zwgk_97124/fdzdgknr_97126/tjxx/202111/t20211117_9988238.html.
- Rencong Y, Ge Z, Sha L. Analysis on immunization awareness and service needs among two-child parents in Guangxi Zhuang autonomous region[J]. Chin J Health Educ. 2018;34(7):629–32.
- Xiao Y, Hong-quan Z, Xian Z. Comparison analysis of the awareness, attitudes, behavior of guardians of migrant children and local children to vaccination[J]. Modern Prev Med. 2016;43(22):4076–80.
- Li-juan B, Jin-hua N, Hai-ying Q. Investigation on immunization of children vaccination program in border areas of Chongzuo city[J]. Modern Prev Med. 2017;44:819–22.
- Yanmei W, Wen C, Ke Z. Survey on satisfaction rate of vaccination service and awareness rate of vaccination knowledge among parents in Chengdu[J]. Chongqing Med. 2014;43(24):3210–11.
- Hongyun Q, Huisi Z, Yongmei K. Survey on knowledge-attitude-practice of immunization among parents of children from Linxia Hu autonomous prefecture of Gansu Province[J]. Chin J Health Educ. 2015;31(4):362–66.
- Stefanoff P, Mamelund SE, Robinson M, Netterlid E, Tuells J, Bergsaker MAR, Heijbel H, Yarwood J. Tracking parental attitudes on vaccination across European countries: the vaccine safety, attitudes, training and communication project (VACSATC)[J]. Vaccine. 2010;28(35):5731–37. doi:10.1016/j.vaccine.2010.06.009.
- Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey[J]. Pediatrics. 2011;127 Suppl 1(Supplement_1):S92–S99. doi:10.1542/peds.2010-1722N.
- Alawneh I, Saymeh A, Yasin A, Alawneh M, Al-Tatari H. Vaccines attitudes, concerns, and information sources reported by parents of young children among north Palestinian parents[J]. Adv Prev Med. 2020;2020:8028172. doi:10.1155/2020/8028172.
- Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey[J]. Pediatrics. 2000;106(5):1097–102. doi:10.1542/peds.106.5.1097.
- Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers the role of information[J]. Am J Prev Med. 2005;29(2):105–12. doi:10.1016/j.amepre.2005.04.010.
- Healy CM, Montesinos DP, Middleman AB. Parent and provider perspectives on immunization: are providers overestimating parental concerns?[J]. Vaccine. 2014;32(5):579–84. doi:10.1016/j.vaccine.2013.11.076.
- Campbell H, Edwards A, Letley L, Bedford H, Ramsay M, Yarwood J. Changing attitudes to childhood immunisation in English parents[J]. Vaccine. 2017;35(22):2979–85. doi:10.1016/j.vaccine.2017.03.089.
- Modi D, Dholakia N, Gopalan R, Venkatraman S, Dave K, Shah S, Desai G, Qazi SA, Sinha A, Pandey RM. mHealth intervention “ImTeCHO” to improve delivery of maternal, neonatal, and child care services-A cluster-randomized trial in tribal areas of Gujarat, India[J]. PLoS Med. 2019;16(10):e1002939. doi:10.1371/journal.pmed.1002939.
- Hategeka C, Ruton H, Law MR. Effect of a community health worker mHealth monitoring system on uptake of maternal and newborn health services in Rwanda[J]. Glob Health Res Policy. 2019;4(1):8. doi:10.1186/s41256-019-0098-y.
- Mergler MJ, Omer SB, Pan WK, Navar-Boggan AM, Orenstein W, Marcuse EK, Taylor J, deHart MP, Carter TC, Damico A, et al. Association of vaccine-related attitudes and beliefs between parents and health care providers[J]. Vaccine. 2013;31(41):4591–95. doi:10.1016/j.vaccine.2013.07.039.
- Kazi AM, Ahsan N, Mughis W, Jamal S, Allana R, Raza M, Muneer S, Mughal MAK, Kaleemuddin H, Sameen F, et al. Usability and acceptability of a mobile app for behavior change and to improve immunization coverage among children in Pakistan: a mixed-methods study[J]. Int J Environ Res Public Health. 2021;18(18):9527. doi:10.3390/ijerph18189527.
- Kazi AM, Ahsan N, Khan A, Jamal S, Kalimuddin H, Ghulamhussain N, Wajidali Z, Muqeet A, Zaidi F, Subzlani M, et al. Personalized text messages and automated calls for improving vaccine coverage among children in Pakistan: protocol for a community-based cluster randomized clinical trial[J]. JMIR Res Protoc. 2019;8(5):e12851. doi:10.2196/12851.
- Gibson DG, Kagucia EW, Ochieng B, Hariharan N, Obor D, Moulton LH, Winch PJ, Levine OS, Odhiambo F, O’Brien KL, et al. The mobile solutions for immunization (M-SIMU) trial: a protocol for a cluster randomized controlled trial that assesses the impact of mobile phone delivered reminders and travel subsidies to improve childhood immunization coverage rates and timeliness in Western Kenya[J]. JMIR Res Protoc. 2016;5(2):e72. doi:10.2196/resprot.5030.
- Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V. Mobile phone messaging reminders for attendance at healthcare appointments[J]. Cochrane Database Syst Rev. 2013;(12):D7458.
- Mellou K, Silvestros C, Saranti-Papasaranti E, Koustenis A, Pavlopoulou ID, Georgakopoulou T, Botsi C, Terzidis A. Increasing childhood vaccination coverage of the refugee and migrant population in Greece through the European programme PHILOS, April 2017 to April 2018[J]. Euro Surveill. 2019;24(27). doi:10.2807/1560-7917.ES.2019.24.27.1800326.
- Lin SY, Zhang SY, Chantler T, Sun FY, Zou J-T, Cheng -J-J, Chen Y-Q, Sun M, Howard N. Vaccination coverage determinants in low uptake areas of China: a qualitative study of provider perspectives in Sichuan, Guangdong, and Henan Provinces[J]. Hum Vaccin Immunother. 2022;18(1):2030623. doi:10.1080/21645515.2022.2030623.
- Gong D, Jiang Q, Chantler T, Sun FY, Zou J, Cheng J, Chen Y, Li C, Sun M, Howard N. Health system barriers and facilitators to delivering additional vaccines through the national immunisation programme in China: a qualitative study of provider and service-user perspectives[J]. Vaccines. 2021;9(5):476. doi:10.3390/vaccines9050476.
- Ni ZL, Tan XD, Shao HY, WANG Y. Immunisation status and determinants of left-behind children aged 12-72 months in central China[J]. Epidemiol Infect. 2017;145(9):1763–72. doi:10.1017/S0950268817000589.
- Chen L, Wang W, Du X, Rao X, van Velthoven MH, Yang R, Zhang L, Koepsell JC, Li Y, Wu Q, et al. Effectiveness of a smart phone app on improving immunization of children in rural Sichuan Province, China: study protocol for a paired cluster randomized controlled trial[J]. BMC Public Health. 2014;14(1):262. doi:10.1186/1471-2458-14-262.