ABSTRACT
It is unclear how the COVID-19 pandemic impacted human papillomavirus (HPV) vaccine uptake and which sociodemographic groups may have been most impacted. We aimed to assess differences in HPV vaccine uptake (initiation and completion) before and during the pandemic in the United States. We conducted a cross-sectional study using data from the 2019 to 2020 National Immunization Surveys – Teen (NIS-Teen), comparing vaccine initiation and completion rates in 2019 vs. 2020, based on confirmed reports by a healthcare provider. Weighted logistic regression analysis estimated odds of vaccine initiation and completion for both adolescent and parental characteristics. There were 18,788 adolescents in 2019 and 20,162 in 2020. There was 3.6% increase in HPV vaccine initiation (71.5% vs. 75.1%) and a 4.4% in completion (54.2% vs. 58.6%) rates from 2019 to 2020. In 2020, Non-Hispanic White teens were significantly less likely to initiate (aOR = 0.62, 95% CI: 0.49, 0.79) and complete (aOR = 0.71, 95% CI: 0.58, 0.86) vaccine uptake compared with non-Hispanic Black teens. Additionally, teens who lived above the poverty line were also less likely to initiate HPV vaccination (aOR = 0.63, 95% CI: 0.49, 0.80) or complete them (aOR = 0.73, 95% CI: 0.60, 0.90), compared to those who lived below the poverty line. During the COVID-19 pandemic in 2020, some historically advantaged socioeconomic groups such as those living above the poverty line were less likely to receive HPV vaccine. The impact of the pandemic on HPV vaccine uptake may transcend traditional access to care factors.
Introduction
There is an estimated 13 million new cases of human papillomavirus (HPV) infection in the United States yearly.Citation1 Its high-risk types (especially HPV 16 and 18) are associated with oropharyngeal and anogenital cancers,Citation2 and oropharyngeal cancer has, in the last decade, surpassed cervical cancer as the leading HPV-associated cancer.Citation3,Citation4 Currently recommended gender-neutral HPV vaccine schedule is a two- or three-dose series based on the age of series initiation.Citation5 Young children who initiate vaccine uptake between 11 and 14 years old are eligible for the two-dose series; at age 15 or older, the three-dose series is recommended.Citation6
HPV vaccination is a national imperative. The Healthy People initiative had the goal of 80% HPV vaccine completion rate among adolescents aged 13–15 y in 2020.Citation7 Data show that in 2020 initiation was at 75%, and only 59% had completed the recommended number of doses.Citation8 Prior to the COVID-19 pandemic, known barriers to HPV vaccination included cost, safety concerns, lack of provider recommendation, and scheduling difficulties.Citation9–11 Additionally, previous studies indicate that HPV vaccine uptake may be influenced by social determinants of health factors, including income and poverty levels, which are also associated with access to care.Citation12,Citation13 Given that the pandemic has had a profound effect on access to health care in general, exacerbated existing health equity concerns and vaccine hesitancy,Citation14–16 and disrupted vaccine delivery, schedule and completion,Citation17,Citation18 it is critical to understand any pandemic-related impacts on the already suboptimal HPV vaccination rate.
In March 2020, the Centers for Disease Control and Prevention (CDC) adopted and mandated a stay-at-home order across the United States as a community mitigation strategy to curb COVID-19 spread.Citation19 This mandate directly contributed to the sharp decline reported in ordering and administering routine vaccines early in the pandemic, compared to 2018 and 2019.Citation20,Citation21 There was a decrease in rate of vaccine doses administered for HPV (24%), Tdap (21.8%) and meningococcus (20.8%), suggesting a decrease in vaccine uptake in general among teens during the COVID pandemic compared to 2019.Citation22 Paradoxically, however, the latest CDC report showed a slight increase in HPV vaccine rates for adolescents aged 13–17 during the first year of the COVID pandemic (2020).Citation8 While the pandemic exposed the impact of socioeconomic and sociodemographic factors on healthcare access, it is unknown whether there were underlying sociodemographic differences in uptake during the pandemic. We hypothesized that the rate of HPV vaccine uptake will decrease disproportionately among racial/ethnic minority groups and individuals with lower socioeconomic status during the pandemic. To test our hypothesis, we assessed differences in provider-reported HPV vaccine uptake in 2019—before the pandemic – compared with that in 2020, the first year of the pandemic.
Methods
Data source and study sample
We used data from the National Immunization Survey−Teen (NIS-Teen) for the years 2019 and 2020. The NIS-Teen is conducted by the CDC’s National Center for Immunization and Respiratory Diseases. It is a yearly, multi-staged, probabilistic cross-sectional sampling of adolescents aged 13–17 y across all 50 states and the District of Columbia, combining random-digit-dial of parents/guardians, and mail-in survey to all vaccination providers. The data is a freely available dataset and is approved for public use by the CDC’s Institutional Review Board. Each participant in the NIS-Teen dataset has a weight assigned to allow estimates from the reported teens to be grouped to attain population estimates that reflect adolescents in the overall population. Weight adjustment is used to account for non-resolution of telephone numbers and screener non-response, interview non-response and for the non-selected teens for households with more than one teen, since only one teen is randomly selected per household for the interview as well as adjustments for provider non-response and other sources of bias.Citation23
Measures
The outcome of interest was HPV vaccine uptake, measured by estimating HPV vaccine initiation and completion. Initiation and completion were assessed with the question “How many HPV shots did [teen name] ever receive?” HPV vaccine initiation was defined as receipt of at least one dose of the vaccine, confirmed by healthcare provider’s questionnaires. Completion was defined as the receipt of at least two doses (if the adolescent received the first dose before age 15) or three doses (if the adolescent was at least 15 years old and the timeframe between the first and second doses was at least 5 months and 4 d).
Independent variables included sociodemographic characteristics of adolescent and parent/guardian, based on prior literature investigating social determinant of health domains related to HPV vaccine uptake.Citation12,Citation13,Citation24 Adolescent characteristics were age in years (13, 14, 15, 16, 17); sex (female, male); race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or non-Hispanic other); geographic region (Northeast, Midwest, South and West); and poverty level (recorded as “above poverty >$75,000” and “below poverty < $75,000,” which is based on the United States’ Census family poverty levels). Parent/guardian characteristics were mother’s age in years (≤34, 35 to 44, or ≥45); mother’s marital status (married or not married); mother’s education (high school or less, some college, or college graduate); number of children <18 y of age living in the household (one, two to three, or four or more) and number of doctor visits (four or more, two to three, one, none). As have been reported in the previous literature, our analyses included parent/guardian characteristics as they are the primary decision makers for their children.Citation25–28
Statistical analyses
We described the characteristics of study sample using proportions. Next, we used weighted multivariable logistic regression models using listwise deletion to estimate associations between adolescent/parent characteristics and the odds of provider-reported initiation and completion of HPV vaccination, stratified by year. Odds ratios and 95% confidence intervals (CI) were reported for all variables. Analyses were weighted to account for the complex survey design used by the NIS-Teen. Statistical tests were two-tailed, and 95% CIs not including the null value were considered statistically significant. All analyses were performed using R version 4.0.2 and SAS version 9.4 (SAS Institute Inc).
Results
We summarized the characteristics of our study sample for 2019 and 2020; distribution of adolescent and parent/guardian characteristics were similar in both years, including age, sex, race/ethnicity, poverty level, provider recommendation status, and mother’s marital status (). In 2020, the prevalence of provider-reported HPV vaccine initiation among teens was 75.1%, which was 3.6% higher than those who initiated HPV vaccine in 2019 (71.5%). There was a rise of 4.4% in HPV vaccine completion from 2019 (54.2%) to 2020 (58.6%).
Table 1. Characteristics of adolescents aged 13–17 y who initiated or completed HPV vaccination for the years 2019 and 2020, National Immunization Survey Teen (NIS-Teen).
show the regression analysis examining the association between adolescent and parent characteristics, and HPV vaccination uptake. There was no significant association between sex and vaccination completion in 2019; however, in 2020, adolescent males were 18% less likely to complete the HPV vaccine series than were females (aOR = 0.82, 95% CI: 0.73, 0.92). Race/ethnicity was also not significantly associated with vaccination uptake in 2019; however, in 2020, non-Hispanic White adolescents were significantly less likely to initiate (aOR = 0.62, 95% CI: 0.49, 0.79) and complete (aOR = 0.71, 95% CI: 0.58, 0.86) the HPV vaccine series, compared to non-Hispanic Blacks. In 2019, there was no statistically significant difference in HPV vaccine initiation based on poverty level; however, adolescents living above the poverty line were less likely to complete the vaccine series (aOR = 0.72, 95% CI = 0.57, 0.92). In contrast, in 2020, poverty line status was associated with both initiation and completion; adolescents who lived above the poverty line were significantly less likely to initiate (aOR = 0.63, 95% CI: 0.49, 0.80) or complete vaccine series (aOR = 0.73, 95% CI = 0.60, 0.89). Adolescents in the South were less likely to initiate and complete vaccine series compared to those in the Northeast for both 2019 and 2020; the same was true for adolescents without any doctor’s visits the prior 12 months, compared to those who had ≥4 visits.
Figure 1. Factors associated with human papillomavirus vaccine initiation, 2019 and 2020 NIS-Teen.
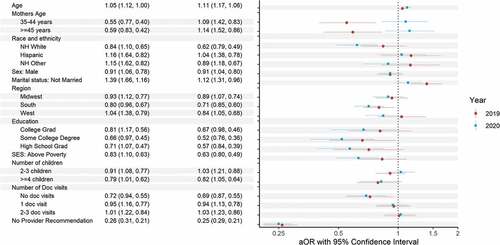
Figure 2. Factors associated with human papillomavirus vaccine completion, 2019 and 2020 NIS-Teen.
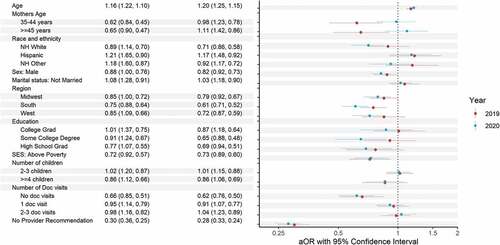
Whereas there were no differences in HPV initiation and completion based on mother’s education status in 2019, in 2020, compared to adolescents with mothers without any high school diploma, those whose mothers who had high school diploma (aOR = 0.57, 95% CI: 0.39, 0.84) or a college degree or higher (aOR = 0.67, 95% CI: 0.46, 0.98) were significantly less likely to initiate HPV vaccine uptake. They were also less likely to complete the series in 2020.
Discussion
The objective of the present study was to examine the difference in sociodemographic and socioeconomic factors affecting HPV vaccine uptake before (year 2019) and during the first year of the COVID pandemic (year 2020). We found that while there was a slight increase in overall initiation and completion rates, certain populations were less likely to initiate and complete the HPV vaccination series in 2020 compared to the prior year. We postulate that the COVID-19 pandemic may have driven some of the sociodemographic and socioeconomic patterns seen in our findings. We hypothesized a priori that rate of HPV vaccine uptake will decrease during the pandemic among individuals of lower sociodemographic status and predicted that factors such as living below poverty would adversely impact access to HPV vaccine in 2020. Strikingly, however, our results showed that historically advantaged socioeconomic groups were less likely to initiate and complete the HPV vaccination series in 2020; a pattern not observed in 2019. We found that non-Hispanic white adolescents were less likely to initiate and complete the series compared with non-Hispanic Black adolescents in 2020, as were adolescents living above the poverty line, compared to those living below the poverty line. Interestingly, both subgroups had no statistically significant difference in vaccination uptake in 2019. Below, we provided some plausible explanations for our findings.
Evidence suggests that during the COVID-19 pandemic, individuals of higher socioeconomic status had greater capacity to socially distance, stay at home and receive health care while at home, due to factors including financial security and telehealth availability.Citation29,Citation30 Unfortunately, some individuals of lower social status and including racial and ethnic minorities, had to continue in-person jobs, use crowded and less socially distant means of transportation, and were less likely to afford or have access to broadband internet or use telehealth services.Citation31 Especially before the availability of the COVID vaccine, about one in every three adults in the United States delayed care for preventive services due to COVID-19 related concerns.Citation32 Also, many parents were concerned about unnecessarily exposing their otherwise healthy children to COVID-19 either from the doctor’s office or other medical facility.Citation33,Citation34 This fear of exposure to COVID-19 may partially explain the spike in utilization of telehealth during the COVID-19 pandemic, especially for routine, preventive and primary care services.Citation35 This deference to telehealth for routine care may have inadvertently impacted HPV vaccination, and since individuals of higher socioeconomic status were more likely to use telehealth,Citation36,Citation37 this might explain the decrease in HPV vaccine uptake seen in this population.
Socioeconomic status and choice of health care (telehealth vs. in-person visits) may also partially explain the finding that mothers of adolescents with the least educational level were more likely to have increased HPV vaccine uptake in 2020. This was particularly interesting, given that there was largely no difference in HPV uptake and mother’s education pre-pandemic. It has long been established that there is an association between higher education and income, and that the majority of children in low-income families may have parents without any college education.Citation38 Before and during the first year of the pandemic, there was an established association between education levels, income levels, and use of telehealth visit, especially video telehealth visits.Citation39,Citation40 Possibly, mothers with higher levels of education also had higher incomes, increasing the odds of obeying stay-at-home orders and access to telehealth services during the pandemic as opposed to in-person visits, which is a requirement for HPV vaccine administration.
The present analysis also found that provider recommendation was significantly associated with increased odds of vaccine initiation and completion. This pattern was evident for both initiation and completion before and during the first year of COVID-19 pandemic. Provider recommendation has been reported to be robustly associated with HPV vaccine uptake prior to the pandemic,Citation41,Citation42 and the present analysis found that during the pandemic, it remained the strongest predictor of vaccine uptake of the measured variables. It is important to note that despite health insurance status not being a covariate adjusted for in the present study, the fact that many Southern states have not expanded Medicaid may have impacted HPV vaccine uptake for teens publicly insured both before and during the pandemic.Citation43 Based on a recent report by the Kaiser Family Foundation, there was an increase in Medicaid enrollment during the pandemic, which provided many low-income families with insurance coverage, which might have increased opportunities to receive the HPV vaccine among individuals with low income.Citation44 The decrease in rate of uptake among individuals with zero visits might suggest an overall decrease in the number of individuals seeking routine preventive care, which would diminish the opportunities for clinicians to make vaccine recommendations. This highlights why it remains critical that clinical appointments are seen as opportunities to increase vaccine uptake.Citation45
COVID-19 might have also influenced differences in HPV vaccination completion based on sex. In 2020, males were significantly less likely to complete the HPV vaccine series than were females; while there was no significant association between sex and vaccination completion in 2019. Due to the virus’ association with cervical cancer, HPV research and awareness has historically centered around women,Citation46–48 and the recommendation of the vaccine for males happened 5 y after the vaccine was approved for use in women.Citation47 These factors may feed into the public’s perception of HPV as a “woman’s disease,” which does not require male vaccination.Citation49 We speculate that during COVID-19, the added impetus to stay home and avoid unnecessary appointments might have exacerbated the already low male vaccination rate and dissuaded males from completing their the dose series.
Finally, it is notable that the Southern region had significantly low vaccine initiation and completion compared to the Northeast, which remained consistent both before and during the pandemic. This speaks to an enduring pattern that transcends COVID-19; the South region has historically been associated with vaccine hesitancy and concordantly has an especially low HPV vaccination rate.Citation50 While we cannot ascertain the impact of COVID-19 on our results, we note that both HPV initiation and completion rates in the Southern region decreased from 2019 to 2020. Future studies are needed to establish whether the pandemic exacerbated the already poor vaccination rate in the region.
Public health implications
While there was an increase in HPV vaccination uptake from 2019 to 2020, consistent with increases in prior years, the present study provides evidence of disparity in uptake among sociodemographic groups that are historically advantaged with regard to access to care. Although the HPV vaccine is safe and over 135 million doses have been administered since 2006,Citation16 it is not mandated in the United States, bar a few states.Citation51 Additionally, the HPV vaccine is recommended for 11- to 12-year olds who typically do not make health decisions without their parents/guardians, and this makes parental choice and perception critical to vaccine uptake. While HPV vaccine safety has driven skepticism regarding uptake in the last few years,Citation11 both COVID-19 and COVID-19 vaccines have sparked remarkable skepticism about health care in general in the United States, and there seems to be differences in COVID-19 vaccination based on race and ethnicity.Citation52,Citation53 The decrease in HPV vaccine uptake among White teens and educated individuals during the pandemic seen in this study may be the reflection of the broader vaccine hesitancy that has been seen in the last few years in our society. It follows that a vaccine-skeptical parent when given a choice might be more likely to make the decision to skip HPV vaccine uptake, especially when it is a recommendation rather than a requirement.Citation54,Citation55 As our findings allude to, there may be other behavioral factors that transcend traditional health equity and access issues in the United States that might impact HPV vaccine uptake. This highlights the complex social and behavioral factors associated with vaccine acceptance, beyond the science of vaccine safety and its importance in cancer prevention. It is therefore critical that vaccine uptake interventions focus on these complex issues to be successful.
Strengths and limitations
This study was not without limitations. First, the data procured were only from 2019 to 2020; while this could describe differences between the 2 y of the study, further investigation would be necessary to assess whether the findings represent changes in previously enduring patterns (such as before 2019 and in the latter part of the COVID-19 pandemic). Second, the cross-sectional nature of our data did not allow us to assess for causation, so our results only describe associations based on two time periods. Third, our study included data for only the first year of the pandemic, and that this may not be enough to reflect the true effect of the COVID pandemic on HPV vaccine uptake among the different sociodemographic groups. Further studies examining future time frames will shed important light on whether the pandemic at large impacted HPV vaccine uptake long term. Fourth, it is important to note that routine HPV vaccination is recommended for 11- and 12-year olds and could start as early as 9 years old, whereas data used for this study were for teens aged 13–17 y, a catch-up age group. Thus, our findings may not be generalizable to HPV vaccine uptake in general and are not necessarily representative of 11- to 12-year olds across the United States who are routinely offered the vaccine based on recommendations. Fifth, since the study examined both initiation and completion, there would likely be spillover for completion in 2020 for those who started the vaccine series in latter 2019, before the pandemic.
Notwithstanding these limitations, the present study sheds light on COVID-19 as a potential barrier to HPV vaccination. The understanding of how the pandemic has affected HPV vaccination could aid providers in the selection of particularly at-risk populations to target when encouraging vaccine compliance. Overcoming the obstacles impeding HPV vaccination uptake will in the long-term impact HPV-associated cancers, so it is critical to continue encouraging vaccine uptake.
Conclusion
The present analysis suggests that while HPV vaccine uptake continued to increase during the first year of the COVID-19 pandemic in 2020, historically advantaged sociodemographic groups, including non-Hispanic white individuals and individuals living above the poverty line, had significantly decreased odds for HPV vaccine uptake. As these groups typically have better healthcare access, additional insight is needed to understand whether the sociodemographic differences in uptake seen in this study were driven by parental choice or other factors unexplained by our study.
Disclosure statement
Dr Osazuwa-Peters is a scientific advisor to Navigating Cancer.
Additional information
Funding
References
- Kreisel KM, Spicknall IH, Gargano JW, Lewis FMT, Lewis RM, Markowitz LE, Roberts H, Johnson AS, Song R, St Cyr SB. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transm Dis. 2021;48(4):208–8. doi:10.1097/OLQ.0000000000001355.
- Dunne EF, Markowitz LE, Saraiya M, Stokley S, Middleman A, Unger ER, Williams A, Iskander J. CDC grand rounds: reducing the burden of HPV-associated cancer and disease. MMWR Morb Mortal Wkly Rep. 2014;63:69.
- Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus–associated cancers—United States, 1999–2015. Morb Mort Wkly Rep. 2018;67(33):918. doi:10.15585/mmwr.mm6733a2.
- Osazuwa-Peters N, Graboyes EM, Khariwala SS. Expanding Indications for the human papillomavirus vaccine: one small step for the prevention of head and neck cancer, but one giant leap remains. JAMA Otolaryngol Head Neck Surg. 2020 Dec 1;146(12):1099–101. doi:10.1001/jamaoto.2020.4068.
- McLendon L, Puckett J, Green C, James J, Head KJ, Yun Lee H, Young Pierce J, Beasley M, Daniel CL. Factors associated with HPV vaccination initiation among United States college students. Hum Vaccines Immunother. 2021;17(4):1033–43. doi:10.1080/21645515.2020.1847583.
- Centers for Disease Control and Prevention. HPV vaccine. [accessed 2021 Jan 27]. https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html#::text=Children%20ages%2011%E2%80%9312%20years,doses%2C%20given%20over%206%20months.
- US Department of Health and Human Services. Healthy people 2020 topics & objectives: immunization and infectious diseases. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Williams CL, Fredua B, McNamara LA, Stokley S, Singleton JA. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — United States, 2020. MMWR Morb Mortal Wkly Rep. 2021 Sep 3;70(35):1183–90. doi:10.15585/mmwr.mm7035a1.
- Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: a systematic review. Prev Med. 2014 Jan;58:22–32. doi:10.1016/j.ypmed.2013.10.009.
- Downs LS Jr, Scarinci I, Einstein MH, Collins Y, Flowers L. Overcoming the barriers to HPV vaccination in high-risk populations in the US. Gynecol Oncol. 2010 Jun;117(3):486–90. doi:10.1016/j.ygyno.2010.02.011.
- Sonawane K, Lin YY, Damgacioglu H, Zhu Y, Fernandez ME, Montealegre JR, Cazaban CG, Li R, Lairson DR, Lin Y, et al. Trends in human papillomavirus vaccine safety concerns and adverse event reporting in the United States. JAMA Netw Open. 2021 Sep 1;4(9):e2124502. doi:10.1001/jamanetworkopen.2021.24502.
- Maness SB, Thompson EL. Social determinants of human papillomavirus vaccine uptake: an assessment of publicly available data. Public Health Rep. 2019 May/Jun;134(3):264–73. doi:10.1177/0033354919838219.
- Thompson EL, Rosen BL, Maness SB. Social determinants of health and human papillomavirus vaccination among young adults, national health interview survey 2016. J Community Health. 2019 Feb;44(1):149–58. doi:10.1007/s10900-018-0565-2.
- Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020 Jun 23;323(24):2466–67. doi:10.1001/jama.2020.8598.
- Menon DU, Belcher HME. COVID-19 pandemic health disparities and pediatric health care-the promise of telehealth. JAMA Pediatr. 2021 Apr 1;175(4):345–46. doi:10.1001/jamapediatrics.2020.5097.
- Osazuwa-Peters N, Rohde RL, Adjei Boakye E. HPV vaccination is safe-you don’t have to whisper it. JAMA Netw Open. 2021 Sep 1;4(9):e2125124. doi:10.1001/jamanetworkopen.2021.25124.
- Gilkey MB, Bednarczyk RA, Gerend MA, Kornides ML, Perkins RB, Saslow D, Sienko J, Zimet GD, Brewer NT. Getting human papillomavirus vaccination back on track: protecting our national investment in human papillomavirus vaccination in the COVID-19 era. J Adolesc Health. 2020 Nov;67(5):633–34. doi:10.1016/j.jadohealth.2020.08.013.
- Toh ZQ, Russell FM, Garland SM, Mulholland EK, Patton G, Licciardi PV. Human papillomavirus vaccination after COVID-19. JNCI Cancer Spectr. 2021 Apr;5(2):kab011. doi:10.1093/jncics/pkab011.
- Moreland A, Herlihy C, Tynan MA, Sunshine G, McCord RF, Hilton C, Poovey J, Werner AK, Jones CD, Fulmer EB, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement — United States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020 Sep 4;69(35):1198–203. doi:10.15585/mmwr.mm6935a2.
- Santoli JM, Lindley MC, DeSilva MB, Kharbanda EO, Daley MF, Galloway L, Gee J, Glover M, Herring B, Kang Y, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020 May 15;69(19):591–93. doi:10.15585/mmwr.mm6919e2.
- Patel Murthy B, Zell E, Kirtland K, Jones-Jack N, Harris L, Sprague C, Schultz J, Le Q, Bramer CA, Kuramoto S, et al. Impact of the COVID-19 pandemic on administration of selected routine childhood and adolescent vaccinations — 10 U.S. jurisdictions, March–September 2020. MMWR Morb Mortal Wkly Rep. 2021 Jun 11;70(23):840–45. doi:10.15585/mmwr.mm7023a2.
- Saxena K, Marden JR, Carias C, Bhatti A, Patterson-Lomba O, Gomez-Lievano A, Yao L, Chen Y-T. Impact of the COVID-19 pandemic on adolescent vaccinations: projected time to reverse deficits in routine adolescent vaccination in the United States. Curr Med Res Opin. 2021 Dec;37(12):2077–87. doi:10.1080/03007995.2021.1981842.
- Center for Disease Control and Prevention. National Immunization Surveys (NIS). [ accessed 2022 Jul 28]. https://www.cdc.gov/vaccines/imz-managers/nis/about.html.
- Mansfield LN, Chung RJ, Silva SG, Merwin EI, Gonzalez-Guarda RM. Social determinants of human papillomavirus vaccine series completion among U.S. adolescents: a mixed-methods study. SSM - Popul Health. 2022 Jun;18:101082. doi:10.1016/j.ssmph.2022.101082.
- Landis K, Bednarczyk RA, Gaydos LM. Correlates of HPV vaccine initiation and provider recommendation among male adolescents, 2014 NIS-Teen. Vaccine. 2018 Jun 7;36(24):3498–504. doi:10.1016/j.vaccine.2018.04.075.
- Choi Y, Eworuke E, Segal R. What explains the different rates of human papillomavirus vaccination among adolescent males and females in the United States? Papillomavirus Res. 2016 Dec;2:46–51. doi:10.1016/j.pvr.2016.02.001.
- Williams CL, Walker TY, Elam-Evans LD, Yankey D, Fredua B, Saraiya M, Stokley S. Factors associated with not receiving HPV vaccine among adolescents by metropolitan statistical area status, United States, National Immunization Survey–Teen, 2016–2017. Hum Vaccines Immunother. 2020 Mar 3;16(3):562–72. doi:10.1080/21645515.2019.1670036.
- Hirth JM, Fuchs EL, Chang M, Fernandez ME, Berenson AB. Variations in reason for intention not to vaccinate across time, region, and by race/ethnicity, NIS-Teen (2008–2016). Vaccine. 2019 Jan 21;37(4):595–601. doi:10.1016/j.vaccine.2018.12.017.
- Huang X, Lu J, Gao S, Wang S, Liu Z, Wei H. Staying at home is a privilege: evidence from fine-grained mobile phone location data in the United States during the COVID-19 pandemic. Ann Am Assoc Geogr. 2022;112(1):286–305. doi:10.1080/24694452.2021.1904819.
- Dasgupta N, Funk M, Lazard A, White B, Marshall S. Quantifying the social distancing privilege gap: a longitudinal study of smartphone movement. medRxiv. Published Online 2020 May;8:2020.05.
- Chiou L, Tucker C. Social distancing, internet access and inequality. 2020.
- Czeisler M, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, et al. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020 Sep 11;69(36):1250–57. doi:10.15585/mmwr.mm6936a4.
- Davis AL, Sunderji A, Marneni SR, Seiler M, Hall JE, Cotanda CP, Klein EJ, Brown JC, Gelernter R, Griffiths MA, et al. Caregiver-reported delay in presentation to pediatric emergency departments for fear of contracting COVID-19: a multi-national cross-sectional study. CJEM. 2021 Nov;23(6):778–86. doi:10.1007/s43678-021-00174-z.
- Nicholson E, McDonnell T, Conlon C, Barrett M, Cummins F, Hensey C, McAuliffe E. Parental hesitancy and concerns around accessing paediatric unscheduled healthcare during COVID-19: a cross-sectional survey. Int J Environ Res Public Health. 2020 Dec 11;17(24):9264. doi:10.3390/ijerph17249264.
- Adams K Telehealth usage primarily driven by fear of COVID-19 transmission, survey finds. [ accessed 2022 Oct 16]. https://www.beckershospitalreview.com/telehealth/telehealth-usage-primarily-driven-by-fear-of-covid-19-transmission-survey-finds.html.
- Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol–Head Neck Surg. 2021 Mar 1;147(3):287–95. doi:10.1001/jamaoto.2020.5161.
- Katz AJ, Haynes K, Du S, Barron J, Kubik R, Chen RC. Evaluation of telemedicine use among us patients with newly diagnosed cancer by socioeconomic status. JAMA Oncol. 2022 Jan 1;8(1):161–63. doi:10.1001/jamaoncol.2021.5784.
- Douglas-Hall A, Chau MM. Parents’ low education leads to low income, despite full-time employment. 2007.
- Fischer SH, Ray KN, Mehrotra A, Bloom EL, Uscher-Pines L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw Open. 2020 Oct 1;3(10):e2022302. doi:10.1001/jamanetworkopen.2020.22302.
- Karimi M, Lee EC, Couture SJ, Gonzales A, Grigorescu V, Smith SR, De Lew N, Sommers BD. National Survey Trends in Telehealth Use in 2021: Disparities in Utilization and Audio vs. Video Services. [ accessed 2022 Sept 15]. https://aspe.hhs.gov/reports/hps-analysis-telehealth-use-2021
- Nasserie T, Bendavid E. Systematic identification and replication of factors associated with human papillomavirus vaccine initiation among adolescents in the United States using an environment-wide association study approach. Sex Transm Infect. 2022 May;98(3):203–09. doi:10.1136/sextrans-2021-054976.
- Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: a meta-analysis and systematic review. Prev Med. 2021 Jul;148:106554. doi:10.1016/j.ypmed.2021.106554.
- Kaiser Family Foundation. Status of State Medicaid expansion decisions: interactive map. [ accessed 2022 Oct 16]. www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.
- Corallo BM, Sophia analysis of recent national trends in Medicaid and CHIP enrollment. [ accessed 2022 Oct 16]. https://www.kff.org/coronavirus-covid-19/issue-brief/analysis-of-recent-national-trends-in-medicaid-and-chip-enrollment/.
- Vadaparampil ST, Kahn JA, Salmon D, Lee J-H, Quinn GP, Roetzheim R, Bruder K, Malo TL, Proveaux T, Zhao X, et al. Missed clinical opportunities: provider recommendations for HPV vaccination for 11–12 year old girls are limited. Vaccine. 2011 Nov 3;29(47):8634–41. doi:10.1016/j.vaccine.2011.09.006.
- Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Human Vaccines Immunother. 2017 Nov 2;13(11):2713–22. doi:10.1080/21645515.2017.1363133.
- Osazuwa-Peters N, Adjei Boakye E, Mohammed KA, Tobo BB, Geneus CJ, Schootman M. Not just a woman’s business! Understanding men and women’s knowledge of HPV, the HPV vaccine, and HPV-associated cancers. Prev Med. 2017 Jun;99:299–304. doi:10.1016/j.ypmed.2017.03.014.
- Dunne EF, Nielson CM, Stone KM, Markowitz LE, Giuliano AR. Prevalence of HPV infection among men: a systematic review of the literature. J Infect Dis. 2006 Oct 15;194(8):1044–57. doi:10.1086/507432.
- Daley EM, Vamos CA, Zimet GD, Rosberger Z, Thompson EL, Merrell L. The feminization of HPV: reversing gender biases in US human papillomavirus vaccine policy. Am J Public Health. 2016 Jun;106(6):983–84. doi:10.2105/ajph.2016.303122.
- Maples JM, Zite NB, Oyedeji O, Chamberlin SM, Mastronardi AM, Gregory S, Gatwood JD, Hohmeier KC, Booker ME, Perry JD, et al. Availability of the HPV vaccine in regional pharmacies and provider perceptions regarding HPV vaccination in the pharmacy setting. Vaccines. 2022 Feb 24;10(3):351. doi:10.3390/vaccines10030351.
- Osazuwa-Peters N. Human papillomavirus (HPV), HPV-associated oropharyngeal cancer, and HPV vaccine in the United States–do we need a broader vaccine policy? Vaccine. 2013 Nov 12;31(47):5500–05. doi:10.1016/j.vaccine.2013.09.031.
- Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. 2020 Jun 23;323(24):2458–59. doi:10.1001/jama.2020.8711.
- Fridman A, Gershon R, Gneezy A, Capraro V. COVID-19 and vaccine hesitancy: a longitudinal study. PloS One. 2021;16(4):e0250123. doi:10.1371/journal.pone.0250123.
- Dubé È, Ward JK, Verger P, MacDonald NE. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Ann Rev Public Health. 2021 Apr 1;42(1):175–91. doi:10.1146/annurev-publhealth-090419-102240.
- Majee W, Anakwe A, Onyeaka K, Harvey IS. The past is so present: understanding COVID-19 vaccine hesitancy among African American adults using qualitative data. J Racial Ethn Health Disparities. 2022 Feb 19;1–13. doi:10.1007/s40615-022-01236-3.
