ABSTRACT
Vaccines are effective tools to prevent COVID-19-related morbidity. However, coverage is low throughout sub-Saharan Africa. Uptake of public health measures, perceptions of COVID-19 illness and vaccines, and intention to vaccinate were evaluated in 2021–2022 in rural Zambia. Adherence to public health measures, perceptions of COVID-19 risk and severity, and vaccine acceptance increased significantly over time, particularly in December 2021, coinciding with the fourth pandemic wave and relaunch of the national vaccine campaign. Vaccine acceptance was associated with perceptions of vaccine safety and effectiveness, but not disease severity. These findings highlight the importance of strong pandemic response and public communication for increased uptake of mitigatory measures, including vaccine acceptance.
Introduction
To control the spread of SARS-CoV-2 globally, public health measures were implemented in most countries soon after COVID-19 was declared a pandemic in March 2020.Citation1 These measures initially relied on restricting movement, physical distancing, improving hygiene, and masking. The rapid development of safe and effective vaccines by December 2020 was a tremendous achievement and added a key strategy for controlling the pandemic. However, the roll-out of the vaccines has highlighted global inequities in access, with much of the supply going to high-income countries. As of 30 June 2022, 12.1 billion doses of the vaccines have been administered worldwide, with only 539.8 million doses administered in African countries.Citation2 Only 18.5% of the African continent is fully vaccinated compared to >60% in all other regions.Citation2 While supply issues have hampered the roll-out, challenges with vaccine acceptance have also contributed to low uptake. Many factors may contribute to vaccine hesitancy in Africa, including lack of knowledge or confidence in the vaccines, lack of perceived risk of COVID-19, religious beliefs, and mistrust of public health or government institutions due to historical abuses, with rates of hesitancy varying both between and within countries as well as over time.Citation3–5 Monitoring and understanding vaccine acceptance as the pandemic progresses will be critical to improve vaccine uptake and coverage.
This study was conducted to evaluate uptake of public health measures and vaccine acceptance over time in a rural area of southern Zambia, with the hypothesis that uptake of these measures would increase over time. Zambia is located in southern Africa and recorded its first cases of COVID-19 in March 2020.Citation6 Soon afterward, the government imposed public health measures, including screening and quarantine of travelers into Zambia, restrictions on travel for residents and public gatherings, closure of schools, indoor dining and recreational facilities, and mandatory mask wearing in public.Citation7 Easing of restrictions began in a phased manner in April 2020 and continued until September 2020 when most restrictions were fully lifted.Citation7 The COVID-19 vaccine program was launched in April 2021 when vaccines became available for adults 18 years and older through COVAX initiatives, including COVISHIELD (Oxford/AstraZeneca formulation from the Serum Institute of India), Jcovden (Janssen/Johnson & Johnson), and the Sinopharm vaccine.Citation8 However, uptake was low, with only 5% of the eligible population vaccinated by October 2021.Citation9 The program was relaunched that month with the goal of vaccinating 70% of the eligible population.Citation9 Vaccines became available for children 12–17 years of age in December 2021.Citation10 As of 30 June 2022, Zambia reported 325,857 cases and 4,006 deaths,Citation11 and 23.9% of the population was fully vaccinated.Citation2
Methods
Study setting and procedures
Data for this analysis were collected as part of ongoing surveillance conducted at Macha Hospital through the Johns Hopkins Center of Excellence for Influenza Research and Surveillance (JHCEIRS). Macha Hospital is located in a rural area of Southern Province, Zambia, and serves a catchment population of approximately 150,000 individuals, consisting primarily of subsistence farmers. While COVID-19 cases were identified in Zambia beginning in March 2020, the first case in Macha was definitively identified in December 2020.Citation12,Citation13 COVID-19 vaccines became available in Macha in April 2021.
The surveillance methods have been previously described.Citation14 Briefly, surveillance for respiratory infections was initiated in December 2018. All patients attending the outpatient department are screened for influenza-like illness (ILI) and an age-stratified sample of patients with ILI are recruited to participate in the study each week. After obtaining written informed consent, participants are administered a questionnaire to collect information on demographics, household characteristics, current symptoms, and medical history. Questions about COVID-related public health measures were added on 25 January 2021. Participants were asked if they had made changes to their lifestyle or daily activities due to COVID-19 and provided a list of measures. Questions about perceptions of COVID-19 and vaccines and receipt of vaccines were added on 10 May 2021. Participants were presented with a set of statements about COVID-19 risk and severity, COVID-19 vaccine safety and effectiveness, and intention to receive the vaccine. Participants responded on a Likert scale from strongly disagree to strongly agree. For participants who indicated that they did not intend for themselves or their children to be vaccinated, reasons for concern were documented. For participants 0–15 years of age, these questions were answered by their caregiver.
Statistical analysis
The analysis of public health measures was restricted to participants enrolled from 25 January 2021 (when questions were added to the questionnaire) to 31 May 2022 (n = 569). The proportion of participants performing each measure was summarized over time. Trends over time were assessed using the Mantel-Haenszel chi-square statistic. Time periods for the analysis were defined by pandemic waves based on the number of cases reported by the World Health Organization (https://covid19.who.int/region/afro/country/zm) (Figure S1).
The analysis of COVID-19 perceptions and vaccine intentions was restricted to participants enrolled from 10 May 2021 (when questions were added to the questionnaire) to 31 May 2022 (n = 461). The proportion of participants strongly agreeing or agreeing to each statement was summarized over time, with time periods defined as previously described. Trends over time were assessed using the Mantel-Haenszel chi-square statistic. Agreement between statements was assessed using the Kappa statistic.
The characteristics of participants intending (strongly agree or agree), no opinion, and not intending (strongly disagree or disagree) to be vaccinated or have their child vaccinated were compared using a chi-square test for categorical variables and a Kruskal-Wallis test for continuous variables. As the proportion of participants intending to be vaccinated increased over time, the analysis was stratified into two periods: Wave 2 to Post-Wave 3 and Wave 4 to Post-Wave 4.
The analysis was conducted using SAS software, Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
This study was approved by the Johns Hopkins Institutional Review Board (IRB00168163), the Macha Research Trust Institutional Review Board (E.2018.02), and the Zambian National Health Research Authority. Adult participants and the parents or legal guardians of pediatric participants provided written informed consent. Children 12–15 years of age provided written assent.
Results
From 25 January 2021 to 31 May 2022, 569 participants were enrolled. The characteristics of participants are provided in Table S1. Adherence to public health measures was 58–90% during Wave 2 and increased significantly over time to 89–100%, with the exception of disinfecting surfaces in the home which was reported by 50% of participants in Wave 2 and decreased over time ().
Figure 1. a) Adherence to public health measures by time perioda (Jan 2021 to May 2022) and b) perceptions of COVID-19 risk, severity, and vaccines by time perioda,b (May 2021 to May 2022) in Macha, Zambia.
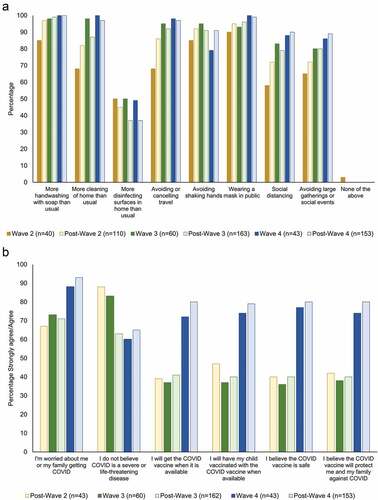
From 10 May 2021 to 31 May 2022, 461 participants were enrolled. Concerns about getting COVID-19 increased significantly over time, from 67% in Post-Wave 2 to 93% in Post-Wave 4 (). Over the same time, perceptions that COVID-19 was not severe or life-threatening decreased significantly, from 88% in Post-Wave 2 to 65% in Post-Wave 4 (). Intentions to get vaccinated and perceptions that the vaccines were safe and effective were low and stable (36–47%) during Post-Wave 2, Wave 3, and Post-Wave 3 (). They then increased significantly to 72–80% during Wave 4 and Post-Wave 4.
Overall, there was strong agreement between intentions to be vaccinated and to have their child vaccinated (Kappa: 0.85) (Table S2). Participants with intentions to be vaccinated or to have their child vaccinated were significantly more likely to believe that the vaccine was safe and effective in all time periods (Table S3). Participants with intentions to receive the vaccine were significantly more likely to have concerns about getting COVID-19 in Wave 2 to Post-Wave 3. Participants with no opinion about intentions to vaccinate were significantly more likely to believe that COVID-19 is not serious or life threatening in Wave 4 to Post-Wave 4. There were no statistically significant differences in the demographic characteristics of participants with and without intentions to vaccinate in any time periods (Table S3).
Among the 167 participants who did not intend to be vaccinated or have their child vaccinated, concerns were provided by 161 participants (96%). The primary concern was vaccine safety (). Other top concerns included vaccine side effects and getting COVID-19 from the vaccine.
Figure 2. Reasonsa for not wanting to receive the COVID-19 vaccine in Macha, Zambia.
Self-reported receipt of COVID-19 vaccines was evaluated over time. Between May and November 2021, 41 participants aged 18 to 50 years and 18 participants 51 years and older were enrolled. Only one (2.4%) participant 18 to 50 years and older reported having received a COVID-19 vaccine (Figures S2 and S3). Between December 2021 and May 2022, 29 participants 18 to 50 years of age and 15 participants 51 years of age and older were enrolled. Eleven (38%) participants 18 to 50 years and eight (53%) participants 51 years and older reported having received a vaccine. Between December 2021 and May 2022, 14 participants 12 to 17 years of age were enrolled, and only one (7.1%) reported having received a vaccine. Among the 21 participants receiving a vaccine, three (14%) received COVIDSHIELD and 15 (71%) received Jcovden (three participants did not know which product they received). The median time between self-reported receipt of first dose and enrollment was 2.2 months (range: 0.1, 12.0).
Discussion
In this study, conducted in rural Zambia over one year, adherence to COVID-19 public health measures, perceptions of COVID-19 risk and severity, and COVID-19 vaccine acceptance increased over time.
Intentions to be vaccinated were low at the beginning of the study period (36–47%), consistent with other reports from adults in Zambia around this time.Citation15,Citation16 A study conducted in two districts in Zambia in November 2020, prior to the availability of COVID-19 vaccines, found that 66% of adults planned to receive the vaccine when available, with lower levels of acceptance in the primarily rural (47%) compared to urban (85%) district.Citation15 An online survey available throughout Zambia in April and May 2021 found similarly low acceptance, with only 33% of adults willing to receive the vaccine if made available.Citation16 Comparisons across studies and countries are difficult due to differences in timing, setting, and population, but these findings are consistent with other studies in the region.Citation5,Citation17 A recent review of studies from Africa conducted in late 2020 and early 2021 found a rate of acceptance ranging from 6.9% to 97.9%, with almost a third of studies reporting estimates below 50%.Citation18
Intentions to vaccinate in this study increased significantly up to 80% in December 2021. Other estimates from the region during this time are not currently available for comparison, but these findings are consistent with the upper range of estimates from earlier in the year.Citation18 Increased intentions were supported by increased reports of vaccine receipt among study participants around the same time. This coincided with the emergence of the Omicron variant and fourth pandemic wave as well as the relaunch of the national vaccine campaign. Both factors likely contributed to increased vaccine acceptance, although the contribution of each cannot be evaluated. The onset of the fourth wave and rapid increase in cases may have contributed to increased awareness of COVID-19 in this community, as participants reported an increase in perceived risk and severity of COVID-19 at this same time. Other surveys in Africa, including Zambia, have found that those perceiving a higher risk of infection or severe illness were more willing to be vaccinated.Citation15,Citation17,Citation18 In this study, concerns about getting COVID-19, but not disease severity, were correlated with vaccine acceptance. Relaunching the vaccine campaign may have contributed to vaccine acceptance by increasing knowledge about the vaccines and their benefits. Other programs in the region have found that strong political commitment and leadership, community engagement, and diverse vaccine delivery strategies are critical for a successful program.Citation19
The primary concerns reported by participants were related to the safety and side effects of the vaccine, which is consistent with other studies in the region.Citation17,Citation18,Citation20 Myths and misinformation were also reported by a small proportion of participants, including that the vaccine would alter their DNA, make them infertile, or contain a tracking device. These myths and conspiracy theories have been widely reported and served to increase public suspicion of the vaccines and decrease uptake,Citation18,Citation20,Citation21 including in Zambia. A key goal of the vaccine campaign relaunch was to increase knowledge about COVID-19 and the vaccines and combat misinformation.Citation9
While intentions to vaccinate increased after December 2021, additional gains over time were not observed and approximately 20% of participants throughout the study period in 2022 did not intend to vaccinate. This is consistent with 15–30% of individuals in high-income countries who remain unvaccinated despite widespread availability.Citation22 As the factors contributing to vaccine hesitancy may differ by community and setting, continuing to understand context-specific drivers of vaccine hesitancy will be critical to develop innovative and culturally relevant strategies to enhance existing vaccine campaigns and reach individuals and communities with concerns. Proposed approaches for generating positive health behaviors toward COVID-19 vaccines in sub-Saharan Africa include community empowerment to engage all sectors of society, people-centered strategies to build confidence in vaccines, innovative strategies to promote equitable health education, novel and improved tools to build vaccine literacy, better training for personnel to respond to local needs, and utilizing non-traditional avenues to endorse and facilitate vaccination.Citation23
This study had several limitations. First, the study only included individuals with ILI seeking care at the health facility who may not be representative of all individuals in the community. It is possible that those seeking care may be more aware of COVID-19 and the benefits of vaccination, leading to an overestimation of vaccine acceptance in this community. However, this should have had limited impact on the observed trends over time in perceived risk and vaccine acceptance. Second, uptake of public health measures and perceptions of COVID-19 and vaccines were not available at the start of the pandemic as these questions were added in 2021. However, perceptions about COVID-19 and the vaccines were assessed from the time that vaccines were available in Zambia and can provide insights for the vaccine program. Third, as the study was nested within ongoing surveillance, the analysis of factors associated with vaccine acceptance was limited to those collected in the main survey and important factors may have been missed.
In summary, this study demonstrated how adherence to COVID-19 public health measures, perceptions of COVID-19 risk and severity, and COVID-19 vaccine acceptance have changed over time in rural Zambia as both the pandemic and response have evolved. The findings highlight the importance of providing accurate and trustworthy information about COVID-19 and vaccines and having strong national and regional pandemic response strategies to increase vaccine demand.
Supplemental Material
Download MS Word (129.8 KB)Acknowledgements
We thank the study team and participants for their contributions to the study. We also thank the staff at Macha Hospital for their support and assistance in conducting the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Under the Research Health Act, the Government of Zambia does not allow public access to data collected in Zambia. All investigators interested in the data are required to submit a written request to the Ministry of Health. Contact Dr. Catherine Sutcliffe ([email protected]) to coordinate the request.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2153538.
Additional information
Funding
References
- WHO. Timeline: WHO’s COVID-19 response. [accessed 2021 Jun 15]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#event-71.
- ONE Africa. Data dive: the astoundingly unequal vaccine rollout. [accessed 2022 Jul 1]. https://www.one.org/africa/issues/covid-19-tracker/explore-covid-response/.
- Mutombo PN, Fallah MP, Munodawafa D, Kabel A, Houeto D, Goronga T, Mweemba O, Balance G, Onya H, Kamba RS, et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob Health. 2022;10(3):e320–6. doi:10.1016/S2214-109X(21)00563-5.
- Dzinamarira T, Nachipo B, Phiri B, Musuka G. COVID-19 vaccine roll-out in South Africa and Zimbabwe: urgent need to address community preparedness, fears and hesitancy. Vaccines (Basel). 2021;9(3):250. doi:10.3390/vaccines9030250.
- Sallam M, Al-Sanafi M, Sallam M. A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. 2022;15:21–45. doi:10.2147/JMDH.S347669.
- Simulundu E, Mupeta F, Chanda-Kapata P, Saasa N, Changula K, Muleya W, Chitanga S, Mwanza M, Simusika P, Chambaro H, et al. First COVID-19 case in Zambia — Comparative phylogenomic analyses of SARS-CoV-2 detected in African countries. Int J Infect Dis. 2021;102:455–59. doi:10.1016/j.ijid.2020.09.1480.
- ZNPHI. Situation reports | coronavirus disease 2019 (COVID-19) SITREPS. [accessed 2021 Jun 15]. http://znphi.co.zm/news/situation-reports-new-coronavirus-covid-19-sitreps/.
- WHO Regional Office for Africa. Zambia launches the COVID-19 vaccination (16 April 2021). [accessed 2022 Jul 1]. https://www.afro.who.int/news/zambia-launches-covid-19-vaccination.
- deVere Zambia. Zambia relaunches coronavirus vaccine campaign. [accessed 2022 July 1]. https://devere-zambia.co.zm/news/zambia-relaunches-coronavirus-vaccine-campaign
- Reuters. Zambia to introduce COVID-19 booster jabs next week. [accessed 2022 Jul 1]. https://www.reuters.com/world/africa/zambia-introduce-covid-19-booster-jabs-next-week-2021-12-23/.
- ZNPHI and Ministry of Health. Zambia COVID-19 dashboard. [accessed 2022 Jul 1]. https://nsdi-mlnr.maps.arcgis.com/apps/dashboards/c08c4cce115244f7ba472a458e1483f7.
- Hamahuwa M, Sinywimaanzi P, Muleka M, Munachoonga P, Matakala HK, Morales J, Fenstermacher, KZJ, Rothman, RE, Pekosz, A, Monze, M, et al. Influenza, RSV and SARS-CoV-2 surveillance in rural Zambia from 2019-2021. Presented at: American Society for Tropical Medicine and Hygiene Annual Meeting; 2022 Oct 30 - Nov 3; Seattle (WA).
- Sinywimaanzi P, Sianyinda M, Hamahuwa M, Munachoonga P, Muleka M, Morales J, Fenstermacher, KZJ, Monze, M, Rothman, RE, Pekosz, A, et al. Clinical outcomes among individuals infected with SARS-CoV-2 in rural Zambia: a longitudinal study. Presented at: American Society for Tropical Medicine and Hygiene Annual Meeting; 2022 Oct 30 - Nov 3; Seattle (WA).
- Loevinsohn G, Hamahuwa M, Sinywimaanzi P, Fenstermacher KZJ, Shaw-Saliba K, Pekosz A, Monze M, Rothman RE, Simulundu E, Thuma PE, et al. Facility-based surveillance for influenza and respiratory syncytial virus in rural Zambia. BMC Infect Dis. 2021;21(1):986. doi:10.1186/s12879-021-06677-5.
- Carcelen AC, Prosperi C, Mutembo S, Chongwe G, Mwansa FD, Ndubani P, Simulundu E, Chilumba I, Musukwa G, Thuma P, et al. COVID-19 vaccine hesitancy in Zambia: a glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub-Saharan Africa. Hum Vaccin Immunother. 2022;18(1):1–6. doi:10.1080/21645515.2021.1948784.
- Mudenda S, Hikaambo CN, Daka V, Chileshe M, Mfune RL, Kampamba M, Kasanga M, Phiri M, Mufwambi W, Banda M, et al. Prevalence and factors associated with COVID-19 vaccine acceptance in Zambia: a web-based cross-sectional study. Pan Afr Med J. 2022;41:112. doi:10.11604/pamj.2022.41.112.31219.
- Anjorin AA, Odetokun IA, Abioye AI, Elnadi H, Umoren MV, Damaris BF, Eyedo J, Umar HI, Nyandwi JB, Abdalla MM, et al. Will Africans take COVID-19 vaccination? PLoS One. 2021;16(12):e0260575. doi:10.1371/journal.pone.0260575.
- Ackah BBB, Woo M, Stallwood L, Fazal ZA, Okpani A, Ukah UV, Adu PA. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Health Res Policy. 2022;7(1):21. doi:10.1186/s41256-022-00255-1.
- WHO Regional Office for Africa. Africa’s COVID-19 vaccine uptake increases by 15% (17 March 2022); [accessed 2022 Jul 13]. https://www.afro.who.int/news/africas-covid-19-vaccine-uptake-increases-15.
- Ahiakpa JK, Cosmas NT, Anyiam FE, Enalume KO, Lawan I, Gabriel IB, Oforka CL, Dahir HG, Fausat ST, Nwobodo MA, et al. COVID-19 vaccines uptake: public knowledge, awareness, perception and acceptance among adult Africans. PLoS One. 2022;17(6):e0268230. doi:10.1371/journal.pone.0268230.
- Murewanhema G, Musuka G, Mukwenha S, Chingombe I, Mapingure MP, Dzinamarira T. Hesitancy, ignorance or uncertainty? The need for effective communication strategies as Zimbabwe’s uptake of COVID-19 vaccine booster doses remains poor. Public Health Pract (Oxf). 2022;3:100244. doi:10.1016/j.puhip.2022.100244.
- Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, et al. Coronavirus (COVID-19) vaccinations. [accessed 2022 Nov 7]. https://ourworldindata.org/covid-vaccinations.
- Ajeigbe O, Arage G, Besong M, Chacha W, Desai R, Doegah P, Hamoonga TE, Hussein H, Matchado A, Mbotwe-Sibanda S, et al. Culturally relevant COVID-19 vaccine acceptance strategies in sub-Saharan Africa. Lancet Glob Health. 2022;10(8):e1090–1. doi:10.1016/S2214-109X(22)00251-0.
