ABSTRACT
Despite the recognized benefits of the COVID-19 vaccination, vaccine hesitancy (VH) remains one of the biggest challenges of the mass vaccination campaign. Most studies investigating VH determinants focused on socio-demographics and direct relationships. In this study, we aimed at: 1) identifying subgroups of people differently affected by the pandemic, in terms of psychological status; 2) investigating the role of psychological status and trust in information as possible mediators of the relationship between individual characteristics and VH. To this purpose, a latent class analysis (LCA) followed by a mediation analysis were carried out on data from a survey conducted in January 2021 on 1011 Italian citizens. LCA identified four different subgroups characterized by a differential psychological impact of the pandemic: the extremely affected (21.1%), the highly affected (49.1%), the moderately affected (21.8%) and the slightly affected (8%). We found that VH decreased with the increase of psychological impact (from 59.3% to 23.9%). In the mediation analysis, past vaccination refusal, age 45-54 years and lower-than-average income, were all indirectly related to higher VH through mistrust in COVID-19 information. Differently, the psychological impact counteracted the greater VH in females, the negative effect of social media among youngest (<35 years) and the negative effect of mistrust in the lower-than-average-income subgroup. Knowledge of psychological profile of hesitant individuals, their level of trust and the sources of information they access, together with their sociodemographic characteristics provides a more comprehensive picture of VH determinants that can be used by public health stakeholders to effectively design and adapt communication campaigns.
Introduction
COVID-19 pandemic has drastically altered people’s lives, as well as multiple aspects of the global, public, and private economy.Citation1–3 National governments adopted several interventions to mitigate the impact of the pandemic, with various levels of effectiveness.Citation4–6 Before the COVID-19 vaccine was available, non-pharmaceutical interventions (e.g., stay-at-home measures, self-isolation and closure of non-essential activities) were largely adopted and helped to contain the spread of the virus, mitigating its impact on the population.Citation7
Regrettably, these non-pharmaceutical interventions, in conjunction with the anxiety instilled by the pandemic, determined highly significant levels of psychological distress in the general population that, in many cases, met the threshold for clinical relevance.Citation8 For instance, a systematic review on the psychological impact of the quarantine on the general European adult population reported a prevalence of anxiety symptoms ranging from 5.5% to 70.4% and a prevalence of psychological distress between 15% and 40%.Citation9
Mass vaccination campaigns proved to be the most effective prevention measures, with both health and economic advantages over non-pharmaceutical interventions.Citation10 Vaccination reduced the overall COVID-19 mortality and number of severe cases (i.e., hospitalizations),Citation11–13 while facilitating the reopening of all of the economic structure and non-essential activities.Citation14 The effectiveness of the mass vaccination has ended in a reduction of the use of non-pharmaceutical containment measures and in alleviating the psychological burden due to the pandemic among vaccine recipients.Citation15,Citation16
Of note, the massive vaccinations campaigns’ positive effects were strictly related to the achievement of coverage rates higher than 70% in a short period of time.Citation17,Citation18 In light of the importance of achieving high coverage rates, it was necessary to rigorously plan and organize mass vaccination campaigns as well as promote vaccine acceptance by the general population.Citation19–21 In this regard, the phenomenon of Vaccine Hesitancy (VH) – described as a “delay in acceptance or refusal of vaccination despite availability of vaccination services” by the SAGE group since 2014Citation22 – posed a major obstacle to the effectiveness of COVID-19 immunization programs.
Even before this pandemic, the World Health Organization (WHO) declared VH as one of the 10 global health threats.Citation23 Over the past few years, there has been a stronger need to fully understand the phenomenon and to find solutions to counter it. In order to monitor and understand the reasons why a considerable number of people do not receive recommended vaccinations, various models have been proposed. In 2015, the SAGE working group described the so-called 3Cs model, in which Confidence, Convenience and Complacency were considered as the main factors of VH.Citation24 Other models (e.g., 4Cs, 5As) and scales (e.g., Global Vaccine Confidence Index Scale and 5Cs antecedents of vaccine acceptance) have been proposed over the years,Citation25–29 emphasizing once again how extremely complex the phenomenon of VH is. In 2022, among the behavioral and social drivers (BeSD) of vaccine uptake, WHO considered aspects such as thinking and feeling, social processes, motivation, and practical issues to be of particular importance. Drivers more pertinent to people’s psychological and attitudinal areas, such as cognitive and emotional responses to vaccine-preventable diseases, vaccine-related experiences, and willingness, were therefore included in the BeSD framework.Citation30
VH for COVID-19 has been much studied during the pandemic, especially in light of the uneven uptake rates achieved globally.Citation31,Citation32 According to a recent review and meta-analysis, the specific uptake and acceptance rates for COVID-19 varied among countries, ranging from 35.9% (34.3–37.5) to 86.9% (81.4–92.5). In addition, some people more prone to hesitancy were identified: females, people aged <60 years old, black individuals, and people with lower education or income.Citation33
Even before the pandemic, VH has often been associated with a lack of trustCitation34,Citation35 emphasizing how trust remained, however, an ‘ill-defined’ and ‘loosely measured concept.’Citation34 The need to further study the relationship between trust and vaccine acceptance became even more clear in light of the conspiracy beliefs that arose during the pandemic.Citation36,Citation37 In addition, according to some recent studies analyzing psychological status, anxiety and COVID-19 related fear have been shown to be associated with higher vaccine acceptance, while self-centeredness and emotional instability were more frequently observed among hesitant people.Citation38,Citation39 These findings underscore that the psychological status is also of utmost importance in understanding VH and uptake.
In this study, we used data collected in the midst of the pandemic and before the vaccine campaign to investigate the main factors and determinants of VH in Italy, including some of the BeSD drivers. Specifically, we focused on the possible mediating role of trust in information and psychological impact of the pandemic in the relationship between individual characteristics, sources of information and VH. In order to do so, we first characterized subgroups differently affected by the pandemic in terms of psychological status and concerns related to COVID-19 infection using latent class analysis. Then, we used these subgroups to expand a previously developed model, in which the use of different information sources proved to mediate the effect of individual characteristics on VH.Citation40
Materials and methods
Study setting and participants
A cross-sectional online survey was conducted in January 2021 on a representative sample of citizens aged 18–70 living in Emilia-Romagna region, Northern Italy. The age of the respondents was limited to adults under 70 years due to the nature of data collection through an online platform. Moreover, the survey was administered only to Emilia-Romagna residents because Italian regions are responsible and autonomous for the local organization and delivery of health care and the survey aimed at providing information to regional stakeholders. Details on the recruitment method and data collection were described previously.Citation40
Measures
Willingness to get vaccinated against COVID-19 was rated as ‘very likely,’ ‘somewhat likely,’ ‘not sure,’ ‘not in the next two months but would consider it in the future,’ ‘somewhat unlikely,’ ‘very unlikely.’ VH was defined as present when the response to this question spanned ‘not sure’ to ‘very unlikely.’
Five questions measured people’s feelings related to the pandemic. Specifically, participants were asked to indicate how much they were: anxious with the increase in the number of COVID-19 cases, angry for the conflicting information about COVID-19, distressed for not being able to plan life, depressed due to the uncertainty on pandemic evolution and excited for the arrival of a vaccine. The levels of anxiety, anger, depression, distress, and excitement were rated on a Likert scale from one to four (‘not at all,’ ‘a little,’ ‘somewhat,’ ‘very much’). Three items measured concerns about being infected at work, being infected outside working place, and infecting others, and were rated with the same Likert scale of feelings. See supplementary Table S1 for more details.
Moreover, people were asked about how accurate was in their opinion the number of COVID-19 cases officially reported (somewhat accurate, under-reported, over-reported). This question was considered as a proxy of trust in official COVID-19 information and was dichotomized into accurate vs. non-accurate, for ease of interpretation.
Theoretical model
In a previous study, we focused on the effect of information sources as mediators of the relationship between individual characteristics and VH. Individual characteristics included: age, gender, education, family income, presence of comorbidities, past vaccination refusal and perceived risk of infection. The results showed that the use of social media reinforced VH while the use of institutional websites reduced it.Citation40
Based on recently emerged literature stressing the importance of considering people’s psychological status influencing VH,Citation38,Citation39 we hypothesized that both the perceived risk of infection and feelings related to the pandemic were measures of the psychological impact of the COVID-19 pandemic. Specifically, we used the five items measuring feelings and the three items measuring perceived risk to identify subgroups affected differently by the COVID-19 pandemic in terms of psychological consequences.
Similarly, trust in institutions and science has been reported as a determinant of VH.Citation10,Citation35,Citation41,Citation42 Consequently, we used the perceived accuracy of the number of COVID-19 cases officially reported as a proxy measure of trust in official COVID-19 information.
In this perspective, we added the psychological impact together with trust in official COVID-19 information as further possible mediators of the relationship between individual characteristics (e.g., socio-demographic and economic characteristics) and VH. In addition, we hypothesized that the use of different information sources would reflect different levels of trust in COVID-19 information, and both the information sources and trust would affect the psychological status. In summary, we constructed a theoretical model depicting the path from individual non-modifiable factors to VH, passing through modifiable factors, such as behaviors (use of media), beliefs (trust in information) and perceptions (psychological impact of the pandemic) as shown in .
Statistical analysis
This study is a secondary analysis of the survey data; thus, the sample size was not determined for SEM estimation purposes. However, using the rule of thumb proposed by Bentler and Chou that suggests including at least 10 observations per estimated parameter,Citation43 we can conclude that the sample size is sufficient to estimate all the hypothesized associations depicted in .
Eight ordinal variables measuring feelings and concern about infection were used to build a latent-class model to identify subgroups of people differently affected by the pandemic. Latent class analysis (LCA) with maximum likelihood estimation was used and models with two to five classes were estimated. Each model was replicated 10 times to search for a global, and not just a local, maximum of log-likelihood function. The determination of the optimal number of classes was based on interpretability of classes, a sufficient number of cases per class (≥5%, i.e., 50 participants) and three common goodness of fit indices: likelihood ratio test, Bayesian Information criterion (BIC) and entropy. The likelihood ratio test compares the model with k classes and the model with k + 1 classes, and a significant difference indicates a better fit of the more complex model. Lower values of BIC indicate better fit. Entropy is a measure of classification uncertainty and values >0.80 indicate that the latent classes are highly separated.Citation44
Classes (denoting the level of psychological impact of the pandemic) were compared on socio-demographic and behavioral characteristics using Pearson’s χ2 test for categorical variables and ANOVA for continuous variables.
Finally, the level of psychological impact of the pandemic was used as a mediator in a structural equation modeling analysis. The mediation model depicted in was initially estimated and simplified through backward stepwise selection. Goodness of fit to the data of the final mediation model was assessed using the χ2, CFI, TLI, AGFI, RMSEA and SRMR indices.Citation45–48 Results were reported as standardized regression coefficients (std b) to allow comparison of effects; direct, indirect, and total effects (β) were estimated.
All statistical analyses were conducted using R statistical software 4.0.5 (R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/). LCA was performed using poLCA package,Citation49 while the mediation model was estimated using the sem package.Citation50
Results
Characteristics of the sample
The study population had a mean age of 46.9 ± 11.5 years, 55% were female, 36.5% had a university degree and 71.3% were employed. TV was the mostly used source of information about the pandemic (71.9%), while social media were the least used source (18.9%). Comorbidities related to the risk of severe COVID-19 disease were reported by 28.4% of the sample and 9.2% had a diagnosis of COVID-19; 158 (15.6%) reported to have refused a vaccination in the past and 314 (31.1%) reported to be hesitant toward the COVID-19 vaccine. See supplementary table S2 for more details.
Psychological impact of the pandemic: latent class analysis
The goodness of fit indices for 2 up to 5 classes models are shown in supplementary table S3. There was no concordance between the various goodness of fit indices in the suggested optimal number of classes, with entropy indicating the 2-class model, BIC indicating the 4-class model and the likelihood ratio test indicating the 5-class model. Because the addition of a 5th class resulted in a less interpretable classification as compared to the 4-class solution (see Supplementary Figure S1), we retained the 4-class model as the best for distinguishing subgroups of people differently affected, from a psychological point of view, by the COVID-19 pandemic.
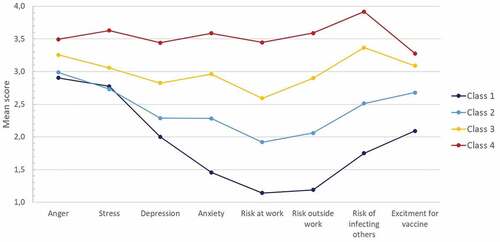
shows the mean scores of the indicators used to define the classes. Classes were ordered with respect to indicators mean values from the one with the lowest to the one with the highest values. Class 1 was the smallest and included 81 people (8.0%). Based on the lowest mean values for most of indicators, this subgroup was denominated as slightly affected by the COVID-19 pandemic. On average, people in this subgroup were somewhat angry and distressed, less depressed, less worried to infect other people and not so much excited for the vaccine arrival; moreover, they had almost no anxiety and no concern about being infected. Class 2 comprised 21.8% of sample and was characterized by people somewhat angry and stressed as class 1 but more excited for vaccine arrival and more worried to infect others. People in this class were also a little worried to be infected, somewhat anxious and depressed. This subgroup was denominated moderately affected by the COVID-19 pandemic. Class 3 included around half of sample (49.1%) and was characterized by a mean value of all the indicators around 3, thus it was denominated highly affected by the COVID-19 pandemic. Finally, class 4 included 21.1% of sample reporting the highest mean values for all the indicators from a minimum of 3.3 for excitement about the arrival of a vaccine up to 3.9 for concern about infecting other people. This subgroup was denominated the extremely affected by the COVID-19 pandemic.
Characteristics and VH of people with a different psychological impact of the pandemic
A higher psychological impact of the pandemic was associated with a lower VH (p < .001, ). In particular, the proportion of hesitant people ranged from 23.9% in class 4 (Extremely affected) to 26.4% in class 3 (Highly affected), 38% in class 2 (Moderately affected), up to 59.3% in class 1 (Slightly affected).
Table 1. Comparison between classes with respect to socio-demographic and other characteristics.
The four classes were significantly different also for socio-demographics and other characteristics as shown in . People in class 1 (Slightly affected) reported a lower use of TV for informing themselves, a lower trust in COVID-19 information, and more frequently a previous vaccination refusal, as compared to the other three classes. Class 2 (Moderately affected) was instead the wealthiest including the lowest proportion of people with a lower-than-average-income (25.8%) and the highest proportion of people with higher-than-average-income (13.6%), it was characterized by a higher proportion of employed people and a lower proportion of people experiencing income reduction due to the pandemic. As compared to the other two classes, class 3 (Highly affected) and class 4 (Extremely affected) had a lower mean age, comprised a significantly higher proportion of females and a higher proportion of people consulting institutional websites ().
Mediation model to predict VH
shows the final mediation model. Four mediators of the relationship between individual characteristics and VH where identified, i.e., social media use, institutional websites use, trust in COVID-19 information and psychological impact of the pandemic. Specifically, a higher psychological pandemic impact was associated with a reduced VH (std b = −0.188, p < .001). The use of institutional websites and trust in official COVID-19 information were both directly and indirectly related to lower VH through a higher psychological impact, while social media use was only directly related to higher VH. No significant association was found between the use of social media or institutional websites and trust in official COVID-19 information.
Figure 3. Estimated mediation model including factors predicting vaccination hesitancy. The red line denotes a positive effect, and the blue line denotes a negative effect. The numbers represent standardized regression coefficients.
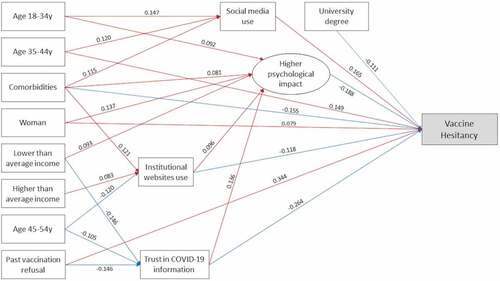
As to socio-demographic variables, compared to the older age class (≥55 years), age 35-44y was directly and indirectly associated with higher VH through a higher social media use, age 45-54y was indirectly associated with higher VH through a lower use of institutional websites and a lower trust in COVID-19 information, while age 18-34y was associated with a higher use of social media but also higher psychological impact resulting in a null total effect on VH (β = 0.007, p = .645). Similarly, female gender was directly associated with higher VH but also associated with a higher psychological impact resulting in a negative indirect effect and in a non-significant total effect on VH (β = 0.053, p = .187). As compared to on-average income, lower-than-average income was associated with a lower trust in COVID-19 information but also with a higher psychological impact of the pandemic, resulting in a non-significant total effect on VH (β = 0.021, p = .154); on the contrary, higher-than-average income was indirectly associated with lower VH through higher use of institutional websites. The association between higher education and lower VH was only direct.
Comorbid conditions were directly related to lower VH but also indirectly associated through several mediators. Indeed, comorbid conditions were related to higher psychological impact, higher institutional websites use, but also higher social media use resulting in a non-significant indirect effect.
Finally, past vaccination refusal was directly related to higher VH, but also indirectly related to VH through a lower trust in COVID-19 information.
Details on direct, indirect and total effects on VH are reported in supplementary Table S4. Fit indices indicated a good fit to the data: χ2(df = 30) = 30.2, p = .457; RMSEA = 0.002 (95% CI: 0.000–0.024); SRMR = 0.024; TLI = 0.999; CFI = 0.998; AGFI = 0.922.
Discussion
Psychological impact of the pandemic
In this paper, we identified different subgroups of the general population during the acute phase of COVID-19 pandemic, based on psychological status and risk perception. Findings from LCA indicate four different groups characterized by a gradual increase in the level of the psychological impact, namely: the extremely affected, the highly affected, the moderately affected and the slightly affected by the pandemic. Other studies have investigated the COVID-9 pandemic impact in terms of concerns and anxietyCitation51 or perceived risk and preventive behavior.Citation52,Citation53 Similarly, to our study, they used the LCA and found an increasing level of COVID-19 impact among different classes, for example Horn and colleaguesCitation52 identified three subgroups: the least, the more and the most affected by the COVID-19 pandemic. However, these studies were conducted on specific sub-groups, university students,Citation51 older adultsCitation52 and social media usersCitation53 while our study concerns the general population.
The extremely and the highly affected subgroups included 70% of participants and were characterized by a higher frequency of females, younger mean age and lower income as compared to the slightly and the moderately affected subgroups. Other studies reported an association between female gender and increased psychological distress caused by the pandemic.Citation51,Citation52,Citation54,Citation55 This result may be related to higher fear and anxiety responses of women related to a perceived higher vulnerability along with an increased risk of developing post-traumatic symptoms as compared to men.Citation55–58 Similarly, the association between young age, low-income and greater psychological impact of the pandemic is consistent with evidence from other studies.Citation9–Citation59–61 Both these associations may be explained by the greater consequences of lockdown and restriction measures among these subgroups. For instance, university students were the first experiencing the effect on daily life caused by restriction measures such as online learning and social and sports activities forced interruption. In addition, people with low economic sources are more likely to live in smaller houses with limited space for privacy that could have amplified the mental health consequences of lockdown and restriction measures. Finally, it cannot be ignored the impact that the pandemic has had on temporary and lower-wage workers who have lost or have been at risk of losing their jobs to a greater extent than others.
In our study, we found a significant decrease in VH with the increase of psychological distress and perceived risk. This result can be explained by the fact that the pandemic phase at that time mostly affected respondents’ lives, thus many people were likely to see vaccination as a self-protective measure as well as an act of social responsibility with beneficial effects for all rather than just oneself. Indeed, the pandemic brought to light the interdependencies between people and countries, hence people have become more aware that the achievement of their personal goals depends, now more than ever, on the choices made by other society members.Citation62 However, as reported in another study, the correlation between vaccine acceptance and psychological distress should not be exploited to promote vaccine acceptance by stoking fears, stress, and anxiety in the general population.Citation38 Rather, it is likely that the extremely and highly affected subgroups are more sensitive to community issues, while less affected people may be characterized by a more self-centered attitude and perception of the consequences of the pandemic. Indeed, we also found that the slightly affected subgroup was characterized by a significantly lower proportion of people trusting the official COVID-19 information, that is, a lower proportion of people perceiving the real burden of COVID-19 pandemic. This result was confirmed in the mediation model, where trust in official COVID-19 information was both directly and indirectly related through a higher psychological impact with a lower VH.
The mediating role of trust in information sources and psychological impact of the pandemic on vaccine hesitancy
As compared to the mediation model reported previously,Citation40 the positive effect of obtaining information through institutional sources and the negative effect of social media use on vaccine acceptance were confirmed, although these relationships were not mediated by trust in official COVID-19 information as initially hypothesized. The absence of an association between sources of information and trust in COVID-19 information could be related to the fact that the official number of cases reported was the same across different information sources, thus trust depends more on personal attitudes rather than the type of channel used. On the other hand, relying on institutional sources was indirectly associated with lower vaccine hesitancy through a higher psychological impact. Evidence from the literature suggests an association between the use of healthcare sources and higher perceived risk.Citation39 These findings indicate that people who frequently consult institutional sources may be more aware of the importance of vaccination in counteracting the pandemic.
As to individual characteristics (i.e., socio-demographics, comorbidities and past vaccination refusal), all the effects on VH, direct and indirect through the use of information sources, found in the previous mediation model were confirmed.Citation40 In this study, in addition, we found a significant direct and positive effect of woman on VH and other indirect effects through trust in official COVID-19 information and psychological pandemic impact. Specifically, past vaccination refusal, age 45–54 years and lower-than-average income, were all indirectly related to higher VH through a lower trust in COVID-19 official information. These results, are in line with literature reporting that trust in information, in informative sources and in institution is a crucial mediator in determining willingness to accept vaccine.Citation62–65 Mistrust of official information may be indicative of a conspiracy mind-set perceiving evidence that vaccines are helpful as misleading and covering up evidence that vaccines are harmful.Citation65 Conspiracy theories and mistrust have greater appeal on younger-age and low-income population as also demonstrated by others.Citation66–69
Finally, being psychologically involved with the pandemic counteracted the greater VH in females, the negative effect of social media use in the subgroup of young adult (<35 years) and the negative effect of lower trust associated with the lower-than-average-income subgroup. As a result, the total effect of female gender, young age and low-than-average-income on VH was not statistically significant. The findings of this study underscore the importance of emphasizing the prosocial benefits of vaccination when promoting it, as well as implementing targeted communication campaigns to specific subgroups like females that are known to be at higher risk of vaccine refusal.Citation70,Citation71
Study limitations
These findings should be interpreted in light of several limitations. First, due to the cross-sectional study design, the causal relationship between variables cannot be determined. Secondly, these data were collected during the early weeks of the vaccination campaign in Italy. At this time, only healthcare personnel were vaccinated. Therefore, the willingness to be vaccinated, as well as the level of perceived risk and psychological distress, may have changed in the subsequent weeks. This is because both VH and pandemic perception are dynamic processes. On the other hand, data collected before the vaccination campaign provide insight that can help prepare for future emergencies or viruses that may require mass vaccination. Third, despite the fact that the sample is representative, the results cannot be generalized to the overall Italian population for two reasons: the sample was limited to adults up to 70 years and the survey was administered in a specific geographical area (Emilia-Romagna region in Northern Italy). Fourth, variables included as feelings indicators are not validated measures of the underlying constructs (anxiety, anger, stress, depression, excitement). Similarly, the same critiques apply to the indicators of perceived risk. Nevertheless, the corresponding questions were ad-hoc formulated for the COVID-19 pandemic context and were similar to those used in other studies.Citation52,Citation72,Citation73
Conclusions
Getting vaccinated against COVID-19 is an individual choice, but individual choices have population-level effects that could challenge efforts to control the pandemic, which is why studying the factors that lead to VH is crucial. Many of the determinants already known in the scientific literature were confirmed, but the strength of our study lies in linking them together in a model that considered existing validated frameworks and focusing on the psychological impact of the pandemic and trust in information.
Being psychologically affected by the pandemic means being aware of one’s responsibility to act against its consequences. Accepting vaccination could thus be an effective way not only to take care of oneself but also of the community.
Knowledge of the socio-demographic and psychological profiles of hesitant individuals, together with knowledge of the sources of information they access and their level of trust, provides important information for public health stakeholders to effectively design and adapt communication campaigns. As reducing VH is an important public health priority, interventions aimed at building trust, such as community-based public education, could be developed in order to improve understanding of the individual and social benefits of vaccination.
Supplementary Materials
Download PDF (431.5 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2157622.
Additional information
Funding
References
- Hiscott J, Alexandridi M, Muscolini M, Tassone E, Palermo E, Soultsioti M, Zevini A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020 Jun;53:1–9 . Epub 2020 May 28. PMID: 32487439; PMCID: PMC7254014. doi:10.1016/j.cytogfr.2020.05.010.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 Mar 14;395(10227):912–20. Epub 2020 Feb 26. PMID: 32112714; PMCID: PMC7158942. doi:10.1016/S0140-6736(20)30460-8.
- Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the Coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020 Jun 23;11:1540. PMID: 32655463; PMCID: PMC7325630.Ro. doi:10.3389/fpsyg.2020.01540.
- Perra N. Non-pharmaceutical interventions during the COVID-19 pandemic: a review. Phys Rep. 2021;913:1–52. doi:10.1016/j.physrep.2021.02.001.
- Nguyen LKN, Howick S, McLafferty D, Anderson GH, Pravinkumar SJ, Van Der Meer R, Megiddo I. Evaluating intervention strategies in controlling coronavirus disease 2019 (COVID-19) spread in care homes: an agent-based model [published correction appears in Infect Control Hosp Epidemiol. 2022 May;43(5):685]. Infect Control Hosp Epidemiol. 2021;42(9):1060–70. doi:10.1017/ice.2020.1369.
- Samanlioglu F, Kaya BE. Evaluation of the COVID-19 pandemic intervention strategies with Hesitant F-AHP. J Healthc Eng. 2020 Aug 20;2020:8835258. PMID: 32850105; PMCID: PMC7441437. doi:10.1155/2020/8835258.
- Reno C, Sanmarchi F, Stoto MA, Fantini MP, Lenzi J, Golinelli D. The impact of health policies and vaccine rollout on the COVID-19 pandemic waves in Italy. Health Policy Technol. 2022 Jun;11(2):100604. Epub 2022 Feb 15. PMID: 35186670; PMCID: PMC8843325. doi:10.1016/j.hlpt.2022.100604.
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001.
- Bonati M, Campi R, Segre G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: a systematic review of the evidence. Epidemiol Psychiatr Sci. 2022 Apr 27;31:e27. PMID: 35475479; PMCID: PMC9069583. doi:10.1017/S2045796022000051.
- Steinert JI, Sternberg H, Prince H, Fasolo B, Galizzi MM, Büthe T, Veltri GA. COVID-19 vaccine hesitancy in eight European countries: prevalence, determinants, and heterogeneity. Sci Adv. 2022 Apr 29;8(17):eabm9825. Epub 2022 Apr 27. PMID: 35476432; PMCID: PMC9045608. doi:10.1126/sciadv.abm9825.
- Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022 Jan;114:252–60 . Epub 2021 Nov 17. PMID: 34800687; PMCID: PMC8595975. doi:10.1016/j.ijid.2021.11.009.
- Mohammed I, Nauman A, Paul P, Ganesan S, Chen K-H, Jalil SMS, Jaouni SH, Kawas H, Khan WA, Vattoth AL, et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Hum Vaccin Immunother. 2022;18(1):2027160. doi:10.1080/21645515.2022.2027160.
- Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022;22(9):1293–302. doi:10.1016/S1473-3099(22)00320-6.
- Deb P, Furceri D, Jimenez D, Kothari S, Ostry JD, Tawk N. The effects of COVID-19 vaccines on economic activity. Swiss J Econ Stat. 2022;158(1):3. doi:10.1186/s41937-021-00082-0.
- Zheng YB, Sun J, Liu L, Zhao Y-M, Yan W, Yuan K, Su S-Z, Lu Z-A, Huang Y-T, Liu L, et al. COVID-19 vaccine-related psychological stress among general public in China. Front Psychiatry. 2021 Dec 7;12:774504. Published 2021 Dec 7. doi:10.3389/fpsyt.2021.774504
- Nguyen M. The psychological benefits of COVID-19 vaccination. Adv Public Health. 2021;2021:9, Article ID 1718800. doi:10.1155/2021/1718800.
- World Health Organization. Achieving 70% COVID-19 immunization coverage by Mid-2022. [accessed 2022 Sep 2]. https://www.who.int/news/item/23-12-2021-achieving-70-covid-19-immunization-coverage-by-mid-2022.
- Paetzold J, Kimpel J, Bates K, Hummer M, Krammer F, von Laer D, Winner H. Impacts of rapid mass vaccination against SARS-CoV2 in an early variant of concern hotspot. Nat Commun. 2022;13(1):612. doi:10.1038/s41467-022-28233-8.
- Niazi SK. Making COVID-19 mRNA vaccines accessible: challenges resolved. Expert Rev Vaccines. 2022 Jun 17;21(9):1–14. Epub ahead of print. PMID: 35695469. doi:10.1080/14760584.2022.2089121.
- Marinus R, Mofid S, Mpandzou M, Kühler TC. Rolling reviews during COVID-19: the European Union experience in a global context. Clin Ther. 2022 Mar;44(3):352–63. Epub 2022 Jan 10. PMID: 35123802; PMCID: PMC8743449. doi:10.1016/j.clinthera.2022.01.001.
- Lee SK, Sun J, Jang S, Connelly S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022;12(1):13681. doi:10.1038/s41598-022-17430-6.
- Strategic Advisory Group of Experts on Immunization. Report of the SAGE working group on vaccine hesitancy. 2014 Nov 12 [accessed 2022 Sep 2]. https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf.
- World Health Organization. Ten Threats to global health in 2019. [accessed 2022 Sep 2] https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–64. Epub 2015 Apr 17. PMID: 25896383. doi:10.1016/j.vaccine.2015.04.036.
- Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. 2015;2(1):61–73. doi:10.1177/2372732215600716.
- Thomson A, Robinson K, Vallée-Tourangeau G. The 5as: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016 Feb 17;34(8):1018–24. Epub 2015 Dec 7. PMID: 26672676. doi:10.1016/j.vaccine.2015.11.065.
- Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016 Oct;12:295–301. Epub 2016 Sep 13. PMID: 27658738; PMCID: PMC5078590. doi:10.1016/j.ebiom.2016.08.042.
- Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Bo ̈hm R, Angelillo IF. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE. 2018;13(12):e0208601. doi:10.1371/journal.pone.0208601.
- World Health Organization. Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022. Weekly epidemiological record. Vol. 97. 2022 May 20 [accessed 2022 Sep 2]. https://www.who.int/publications/i/item/who-wer9720-209-224.
- World Health Organization. Behavioural and social drivers of vaccination: tools and practical guidance for achieving high uptake. Geneva. 2022 [accessed 2022 Sep 2]. https://apps.who.int/iris/bitstream/handle/10665/354459/9789240049680-eng.pdf?sequence=1&isAllowed=y.
- Salomoni MG, Di Valerio Z, Gabrielli E, Montalti M, Tedesco D, Guaraldi F, Gori D. Hesitant or not hesitant? A systematic review on global COVID-19 vaccine acceptance in different populations. Vaccines (Basel). 2021 Aug 6;9(8):873. PMID: 34452000; PMCID: PMC8402447. doi:10.3390/vaccines9080873.
- Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, Giattino C, Rodés-Guirao L. A global database of COVID-19 vaccinations. Nature Human Behav. 2021;5(7): 947–5. doi:10.1038/s41562-021-01122-8.
- Wang Q, Hu S, Du F, Zang S, Xing Y, Qu Z, Zhang X, Lin L, Hou Z. Mapping global acceptance and uptake of COVID-19 vaccination: a systematic review and meta-analysis. Commun Med. 2022;2(1):113. doi:10.1038/s43856-022-00177-6.
- Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, Paterson P. Measuring trust in vaccination: a systematic review. Human Vaccines Immunotherapeutics. 2018 July 3;14(7):1599–609. doi:10.1080/21645515.2018.1459252.
- Goldenberg MJ. Vaccine hesitancy: public trust, expertise, and the war on science. Pittsburgh, PA: University of Pittsburgh Press; 2021.
- Pivetti M, Melotti G, Bonomo M, Hakoköngäs E. Conspiracy beliefs and acceptance of COVID-vaccine: an exploratory study in Italy. Soc Sci. 2021;10(3):108. doi:https://doi.org/10.3390/socsci10030108.
- Anakpo G, Mishi S. Hesitancy of COVID-19 vaccines: rapid systematic review of the measurement, predictors, and preventive strategies. Human Vaccines Immunotherapeutics. 2022;18(5):5. doi:10.1080/21645515.2022.2074716.
- Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. 2021 Aug;97:107724 . Epub 2021 Apr 27. PMID: 33951558; PMCID: PMC8078903. doi:10.1016/j.intimp.2021.107724.
- Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021 Jan 4;12(1):29. PMID: 33397962; PMCID: PMC7782692. doi:10.1038/s41467-020-20226-9.
- Reno C, Maietti E, Di Valerio Z, Montalti M, Fantini MP, Gori D. Vaccine hesitancy towards COVID-19 vaccination: investigating the role of information sources through a mediation analysis. Infect Dis Rep. 2021 Aug 12;13(3):712–23. PMID: 34449654; PMCID: PMC8395997. doi:10.3390/idr13030066.
- Zarbo C, Candini V, Ferrari C, D’Addazio M, Calamandrei G, Starace F, Caserotti M, Gavaruzzi T, Lotto L, Tasso A, et al. COVID-19 vaccine hesitancy in Italy: predictors of acceptance, fence sitting and refusal of the COVID-19 vaccination. Front Public Health. 2022;10:873098. Published 2022 Apr 29. doi:10.3389/fpubh.2022.873098.
- Sturgis P, Brunton-Smith I, Jackson J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. 2021;5(11):1528–34. doi:10.1038/s41562-021-01115-7.
- Bentler PM, Chou CH. Practical issues in structural modeling. Sociological Methods Res. 1987;16(1):78–117. doi:10.1177/0049124187016001004.
- Tein JY, Coxe S, Cham H. Statistical power to detect the correct number of classes in latent profile analysis. Struct Equ Modeling. 2013 Oct 1;20(4):640–57. PMID: 24489457; PMCID: PMC3904803. doi:10.1080/10705511.2013.824781.
- Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;422(107):238–46, 423. doi:10.1037/0033-2909.107.2.238.
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor 424 analysis. Psychometrika. 1973;38(1):1–10. doi:10.1007/BF02291170 425.
- Steiger JH, Lind J. Statistically-based tests for the number of common factors. 426 Paper presented at the Annual Spring Meeting of the Psychometric Society; 1980; Iowa City, 427
- Li‐tze H, Peter MB. Cutoff criteria for fit indexes in covariance structure 428 analysis: conventional criteria versus new alternatives, structural equation modeling: a 429. Multidisciplinary J. 1999;6(1):1–55. doi:10.1080/10705519909540118.
- Linzer DA, Lewis JB. poLCA: an R package for polytomous variable latent class analysis. J Stat Softw. 2011;42(10):1–29. doi:10.18637/jss.v042.i10.
- Fox J. Structural equation modeling with the sem package in R. Struct Equ Model. 2006;13(3):465–86. doi:10.1207/s15328007sem1303_7.
- Dratva J, Zysset A, Schlatter N, von Wyl A, Huber M, Volken T. Swiss university students’ risk perception and general anxiety during the COVID-19 pandemic. Int J Environ Res Public Health. 2020 Oct 13;17(20):7433. PMID: 33066008; PMCID: PMC7599649. doi:10.3390/ijerph17207433.
- Horn V, Semmler M, Schweppe C. Older people in Germany during the COVID-19 pandemic: the least, the more, and the most affected. J Popul Ageing. 2021 Dec 13:1–22. Epub ahead of print. PMID: 34925638; PMCID: PMC8666192. doi:10.1007/s12062-021-09352-4.
- Wang PW, Chen YL, Chang YP, Wu CF, Lu WH, Yen CF. Sources of COVID-19-related information in people with various levels of risk perception and preventive behaviors in Taiwan: a latent profile analysis. Int J Environ Res Public Health. 2021;18(4):2091. Published 2021 Feb 21. doi:10.3390/ijerph18042091.
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020 Mar 6;33(2):e100213. Erratum in: Gen Psychiatr. 2020 Apr 27;33(2):e100213corr1. PMID: 32215365; PMCID: PMC7061893. doi:10.1136/gpsych-2020-100213.
- Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020 May 2;17(9):3165. PMID: 32370116; PMCID: PMC7246819. doi:10.3390/ijerph17093165.
- Dalla C, Antoniou K, Drossopoulou G, Xagoraris M, Kokras N, Sfikakis A, Papadopoulou-Daifoti Z. Chronic mild stress impact: are females more vulnerable? Neuroscience. 2005;135(3):703–14. doi:10.1016/j.neuroscience.2005.06.068.
- Verma R, Balhara YP, Gupta CS. Gender differences in stress response: role of developmental and biological determinants. Ind Psychiatry J. 2011 Jan;20(1):4–10. PMID: 22969173; PMCID: PMC3425245. doi:10.4103/0972-6748.98407.
- Sandanger I, Nygård JF, Sørensen T, Moum T. Is women’s mental health more susceptible than men’s to the influence of surrounding stress? Soc Psychiatry Psychiatr Epidemiol. 2004;39(3):177–84. doi:10.1007/s00127-004-0728-6.
- Beck F, Léger D, Fressard L, Peretti-Watel P, Verger P, Group C. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2021 Feb;30(1):e13119. Epub 2020 Jun 28. PMID: 32596936; PMCID: PMC7361195. doi:10.1111/jsr.13119.
- Prati G. Mental health and its psychosocial predictors during national quarantine in Italy against the coronavirus disease 2019 (COVID-19). Anxiety Stress Coping. 2021 Mar;34(2):145–56. Epub 2020 Dec 22. PMID: 33350343. doi:10.1080/10615806.2020.1861253.
- Santana CLA, Manfrinato CV, Souza PRP, Marino A, Condé VF, Stedefeldt E, Tomita LY, Do Carmo Franco M. Psychological distress, low-income, and socio-economic vulnerability in the COVID-19 pandemic. Public Health. 2021 Oct;199:42–45. Epub 2021 Aug 27. PMID: 34537575; PMCID: PMC8390360. doi:10.1016/j.puhe.2021.08.016.
- Falcone R, Ansani A, Colì E, Marini M, Sapienza A, Castelfranchi C, Paglieri F. Trusting COVID-19 vaccines as individual and social goal. Sci Rep. 2022 Jun 8;12(1):9470. PMID: 35676518; PMCID: PMC9176163. doi:10.1038/s41598-022-13675-3.
- Siegrist M. Trust and risk perception: a critical review of the literature. Risk Analysis. 2021 Mar;41(3):480–90. PMID:31046144. doi:10.1111/risa.13325.
- Gilles I, Le Pogam MA, Perriraz M, Bangerter A, Green EGT, Staerklé C, Krings F, Wagner-Egger P, Peytremann-Bridevaux I. Trust in institutions and the COVID-19 threat: a cross-sectional study on the public perception of official recommendations and of othering in Switzerland. Int J Public Health. 2022 Jan 10;66:1604223. PMID: 35095384; PMCID: PMC8790817. doi:10.3389/ijph.2021.1604223.
- Caserotti M, Gavaruzzi T, Girardi P, Tasso A, Buizza C, Candini V, Zarbo C, Chiarotti F, Brescianini S, Calamandrei G, et al. Who is likely to vacillate in their COVID-19 vaccination decision? Free-riding intention and post-positive reluctance. Prev Med. 2022 Jan;154:106885 . Epub 2021 Nov 12. PMID: 34774880; PMCID: PMC8585567. doi:10.1016/j.ypmed.2021.106885.
- Hornsey MJ. Reasons why people may refuse COVID-19 vaccination (and what can be done about it). World Psychiatry. 2022 Jun;21(2):217–18. PMID: 35524590; PMCID: PMC9077616. doi:10.1002/wps.20990.
- Lee JJ, Kang KA, Wang MP, Zhao SZ, Wong JYH, O’Connor S, Yang SC, Shin S. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J Med Internet Res. 2020 Nov 13;22(11):e22205. PMID: 33048825; PMCID: PMC7669362. doi:10.2196/22205.
- Duplaga M. The determinants of conspiracy beliefs related to the COVID-19 pandemic in a nationally representative sample of internet users. Int J Environ Res Public Health. 2020;17(21):7818. doi:10.3390/ijerph17217818.
- Gabriel Salvador Casara B, Suitner C, Jetten J. The impact of economic inequality on conspiracy beliefs. J Exp Soc Psychol. 2022;98:104245. doi:10.1016/j.jesp.2021.104245.
- Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–21. doi:10.1016/S2468-2667(21)00012-8.
- Montalti M, Di Valerio Z, Rallo F, Squillace L, Costantino C, Tomasello F, Mauro GL, Stillo M, Perrone P, Resi D, et al. Attitudes toward the SARS-CoV-2 and influenza vaccination in the metropolitan cities of Bologna and Palermo, Italy. Vaccines. 2021;9(10):1200. doi:10.3390/vaccines9101200.
- Savoia E, Harriman NW, Piltch-Loeb R, Bonetti M, Toffolutti V, Testa MA. Exploring the association between misinformation endorsement, opinions on the government response, risk perception, and COVID-19 vaccine hesitancy in the US, Canada, and Italy. Vaccines (Basel). 2022 Apr 23;10(5):671. PMID: 35632427; PMCID: PMC9147457. doi:10.3390/vaccines10050671.
- Chen YL, Lin YJ, Chang YP, Chou WJ, Yen CF. Differences in sources of information, risk perception, and cognitive appraisals between people with various latent classes of motivation to get vaccinated against COVID-19 and previous seasonal influenza vaccination: Facebook survey study with latent profile analysis in Taiwan. Vaccines (Basel). 2021 Oct 19;9(10):1203. PMID: 34696311; PMCID: PMC8538554. doi:10.3390/vaccines9101203.