ABSTRACT
Health behavior theories have been effectively used for studying populations’ awareness, attitudes, and beliefs related to COVID-19 preventative behaviors. The aim of this study was to explore the factors associated with the intention to get vaccinated against COVID-19 in the Armenian population using the Health Belief Model (HBM) as a framework. We applied stratified two-stage random sampling to conduct a telephone survey of 3,483 adults in 2021. The multi-domain survey instrument included questions on socio-demographic characteristics, COVID-19-related knowledge, COVID-19 susceptibility, severity and self-efficacy beliefs, sources of information on COVID-19, COVID-19 vaccination practice, and its benefits and barriers. We performed bivariate and hierarchical multivariate regression analysis with the entry of variables in blocks. In total, about 12% of the sample (n = 393) was vaccinated against COVID-19. Of 2,838 unvaccinated participants, about 53% (n = 1516) had an intention to get vaccinated. The final hierarchical logistic regression model containing socio-demographic characteristics, knowledge about COVID-19, and HBM constructs explained 43% of the variance in the intention to get vaccinated against COVID-19. Participants’ age, employment status, average monthly expenditures, perceived threat, benefits, perceived barriers, self-efficacy, and cues to action were significant and independent predictors of the intention to get COVID-19 vaccination. This study confirmed the utility of the HBM in highlighting drivers of an important health-protective behavior in the context of pandemics. Health policy makers, communication specialists, and healthcare providers should particularly stress the effectiveness and safety of the vaccines in their efforts to increase vaccination rates and focus on unemployed and low-income population groups.
Introduction
COVID-19 pandemic
Since the start of the COVID-19 pandemic in 2020, countries around the world have implemented a number of public health and social measures to prevent the spread of SARS-CoV-2 and reduce mortality and morbidity from COVID-19, including personal protective measures, environmental measures, surveillance and response, physical distancing, and international travel restrictions. Combined with medical measures, these efforts assisted in managing the situation to some extent; however, to date, the virus continues to mutate, spread and devastate human lives and the global economy.Citation1,Citation2
As of 15 December 2022, the most recent WHO weekly update report notes that countries around the world have reported over 647 million confirmed cases and over 6.5 million deaths due to COVID-19.Citation3
Vaccines against COVID-19 were developed and distributed globally at an unprecedented speed and represented a fundamental step toward ending the pandemic.Citation4 While countries are adopting various measures in an effort to raise their national immunization rates against COVID-19, to date approximately 66.0% of the global eligible population has been fully vaccinated, while only 34.0% have received booster doses.Citation5
Situation in Armenia
Armenia received a small batch of donated vaccines at the end of 2020, but the larger shipment of the first batch of AstraZeneca vaccine (24,000 doses) procured through the COVAX Facility arrived only on March 28th, 2021.Citation6 As the country only managed to procure a limited number of vaccines during the initial stage, the immunization efforts were also rolled out in stages. In the first stage vaccines were made available to the individuals in the high-risk groups, including healthcare workers, residents and employees of elderly houses, senior citizens at or above the age of 65, and 16–64 years old people with chronic conditions. In the second stage, university lecturers, school teachers, and civil servants were also made eligible.
The vaccination campaign started soon after in mid-April as other vaccine types were shipped to the country, including Sputnik V (Gam-COVID-Vac),Citation7 and vaccines became available to the general public.
Currently, the vaccines administered in Armenia include Sinopharm (BBIBP-CorV), and Pfizer (Comirnaty). The vaccines are available to the public at no cost and can be obtained at primary health care (PHC) facilities in urban and rural areas throughout the country. Based on the booster-shot vaccination plan developed by the Ministry of Health (MoH), the vaccines can be administered as booster shots three to six months post-initial vaccination.Citation8,Citation9 Additionally, Russian Sputnik Light,Citation10 which is being locally produced since December 2021, has been approved to be used as a booster shot only.Citation9,Citation11
As soon as vaccines became available in Armenia, the MoH established a working group, composed of over ten national and international organizations, that has been coordinating the vaccination public awareness campaign. This working group has been able to coordinate the creation of various risk communication tools and materials, including training for healthcare workers, social media campaigns, webinars, and behavioral insight surveys, which allowed for policy to be tailored accordingly. Despite the continuous efforts to vaccinate the majority of its population; as of 8 December 2022, only 45.9% of adults are fully vaccinated, while only 3.7% received a booster shot.Citation12
The initial uptake was particularly slow in the country, and the majority of individuals that have been vaccinated were driven by a policy change that took place in October 2021, which required biweekly COVID-19 PCR testing for unvaccinated employees.Citation13 With PCR tests ranging from $10–30 USD, the nation saw a profound increase in vaccinations. The policy was later modified to mandate weekly testing and restrictions on entering public places for the unvaccinated starting end of January 2022.Citation14 All public restrictions and mandatory measures related to COVID-19 have been lifted in Armenia since 1 May 2022.Citation15 As of 15 December 2022, Armenia has 445,881 confirmed COVID-19 cases and 8,712 deaths.Citation16
This article describes the study conducted in Armenia from May to September 2021 to explore the factors which could explain the adoption of vaccination against COVID-19 in the Armenian population and help to target health communication efforts in the country. As of 30 May 2021, at the beginning of the study, Armenia had more than 192 thousand cases and about 3,500 deaths. The proportion of vaccinated people was 1.1% (received at least one dose) and 0.0% were fully vaccinated.Citation17
Health Belief Model
Health behavior theories have been effectively used for studying populations’ awareness, attitudes, and beliefs related to COVID-19 and preventive behaviors. The underlying goal of the application of health behavior theories is to drive behavioral research and the development and evaluation of health interventions aimed at behavior change.Citation18 The Health Belief Model (HBM) was developed in the 1950s to explain the participation of the United States population in public health screening programs.Citation19,Citation20 After its induction, the HBM was extended to study a variety of health-related actions and became one of the most commonly used cognitive models in health behavior research and intervention.Citation21
The HBM postulates that people will take action to prevent, screen for, or control illness if they think they are susceptible to a condition (perceived susceptibility), believe that the condition could have potentially serious consequences (perceived severity), believe that a course of action available to them would help to reduce susceptibility to or severity of the condition (perceived benefits), and believe that the benefits of taking action outweigh the barriers to the action (perceived barriers). The readiness to take action can be influenced by triggers to instigate the action (cues to action). The construct of self-efficacy, defined as “the conviction that one can successfully execute the behavior required to produce the outcomes” was added to the model in 1988.Citation22
The HBM has been widely used in studies that tested the constructs of the model in relation to COVID-19 preventive factors such as mask use, hand washing, maintaining social distance, vaccine acceptance, and others.Citation23–32 Overall, the summarized evidence of the use of HBM in COVID-19-related behavioral research suggests that the model can be effective in identifying modifiable factors that can be targeted for promoting the adoption of protective practices against the novel coronavirus. To our knowledge, no theory-based studies have examined COVID-19-related behaviors in Armenia to date. In the present study, the HBM framework guided the exploration of the perceptions and beliefs about COVID-19 vaccination in a nationwide sample of Armenian adults.
Methods
Study design and setting
We conducted a cross-sectional telephone survey of 3,483 adults (≥18 years old) in the capital Yerevan,Citation33 and 10 marzes (provinces). The survey was one of the components of an extensive study, which was completed in the scope of the USAID-funded “Support to control COVID-19 and other infectious disease outbreaks” project by the Turpanjian College of Health Sciences of the American University of Armenia (AUA/CHS).Citation34
Sampling and recruitment
The research team used stratified two-stage probability proportional to size sampling to select the study participants. The sampling was done through PHC facilities, which cover about 97% of the Armenian population.Citation35 During the first stage, one-third of the PHC facilities in each marz and Yerevan were selected. The random selection of PHC facilities was based on the population size served by each facility. In stage two, the simple random selection of the study participants was performed using a comprehensive national e-health registry of patients (ARMED).Citation36 The list of participants was provided to the trained staff of selected PHC facilities, who recruited the participants via phone calls using standard recruitment scripts prepared by the AUA/CHS researchers. To assure proper representation of all age groups, the participants were recruited from the 18–29, 30–39, 40–49, 50–59, 60–69, and 70+ age groups proportionate to their size in the general population.
To substitute any possible nonresponse or refusal, wrong or missing addresses and other possible errors, the sampling list provided to each facility was six times larger than the needed sample. The participant recruitment continued until the desired sample size was obtained.
Data collection and study tool
The phone survey was embedded in the larger study of COVID-19 seroprevalence. The exclusion criteria for the blood sampling included having a contraindication to venipuncture, being in quarantine or self-isolation for less than 10 days, or being unable to attend the sampling site because of physical disability. At the PHC facility, the AUA/CHS research team administered written informed consent, conducted blood sampling for antibody testing, and obtained the contact numbers of the respondents for the phone survey. There were no additional criteria for the phone survey, and all participants who provided informed consent were contacted by 10 trained interviewers within the first two days after the blood sampling to complete the phone survey. The inclusion criteria for the present study were being unvaccinated and answering to the question about vaccination intention in the survey. The interviews were conducted via electronic tablets using the Alchemer online tool (https://www.alchemer.com/). During the data collection, the phone numbers of participants who completed the phone survey had 1000 AMD ($2 USD) added via an automated system to compensate for their time.
Prior to data collection, the research team pre-tested the entire study protocol, including participant recruitment and inclusion in the study, the blood sampling process, and the phone survey. Based on the hypothesis of the initial project and using the population proportions formulaCitation37 for sample size calculation, the estimated sample size was 3,832.
The Institutional Review Board of the American University of Armenia and WHO ERC/COVID-19 approved the study (#AUA-2021-005; #WHO ERC-CERC.0112)
A multi-domain survey questionnaire captured information on the participants’ socio-demographic characteristics, COVID-19-related knowledge, COVID-19 susceptibility, severity and self-efficacy beliefs, sources of information on COVID-19, COVID-19 vaccination practice, and vaccination benefits and barriers (Supplementary Table S1). The tools from similar studies conducted internationally and in Armenia were identified through an extensive literature search and used for developing the survey questionnaire.Citation24,Citation38–40
Study variables
The intent to get vaccinated for COVID-19 was measured using a single question “When a coronavirus vaccine becomes available to you, how likely is it you will take it?” with four response options ranging from “very likely” to “very unlikely,” which were dichotomized for the regression analysis.
COVID-19 knowledge was measured with five questions with three answer options: “Agree,” “Disagree,” and “Don’t know.” COVID-19 knowledge score (ranging from zero to five) was calculated by summing up the responses to all the questions and later converted into a knowledge percent score. The susceptibility was assessed by asking respondents how susceptible they consider themselves to infection with COVID-19 with four response options ranging from “very susceptible” to “not at all susceptible.” Perceived severity was measured by asking the respondents how severe they think contracting COVID-19 would be for them with four response options ranging from “very severe” to “not at all severe.” Participants were asked whether the COVID-19 vaccine could give them COVID-19 disease and whether they are likely to experience side effects from COVID-19 vaccination. The answer options for both ranged from “strongly agree” to “strongly disagree” and were combined to receive the overall COVID-19 vaccination barriers score. The study participants were asked to assess on a scale from one (“Never”) to seven (“Very often”), how often they used eight different sources of information about COVID-19 (i.e., TV, social media, radio, etc., with the mean score of frequency of use of these sources for obtaining information on COVID-19 serving as a proxy variable for cues to action construct in the HBM. Socio-demographic characteristics of participants measured in the survey included place of residence (urban/rural), gender (male/female), age (continuous), education level (categorical), employment status (categorical), and average monthly expenditures (categorical).
Data management and analysis
The Statistical Package for Social Sciences (SPSS) version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp) was used for data analysis. The SPSS file was downloaded from the Alchemer platform.Citation41 Relationship between intent to get vaccinated and the set of independent variables and covariates were examined by bivariate analyses (T-tests and Chi-squared test). We performed hierarchical multivariable regression analysis with the entry of variables in blocks based on theory to measure the incremental variance accounted for by each predictor set. Socio-demographic variables and knowledge score were entered in the first and second steps. The third block included perceived susceptibility, severity, benefits, and barriers. Cues to action score was entered in the fourth step. Cox & Snell R-squared and Nagelkerke R-squared were used to assess the variability in the outcome explained by the models.
Results
Out of 3,727 people who underwent blood sampling for the antibody testing 3,483 (93.5%) were contacted for the phone survey About 12% (n = 393) of the respondents in the sample received the COVID-19 vaccine, of which about 50% received two doses. The study analysis was conducted using the sample of those 2,838 respondents, who were unvaccinated and answered a question about vaccination intention.
Females constituted about 71.7% of the sample (). The mean age was 49.1 (SD = 14.95). About 68% of the study participants reported some vocational (12–13 years) or university degree education, and approximately half of them were employed. One fifth of the respondents reported monthly family expenditures of less than 100,000 AMD ($226 USD), while the majority had expenditures of 101,000 AMD to 400,000 AMD ($228–900 USD).
Table 1. Socio-demographic characteristics of the respondents.
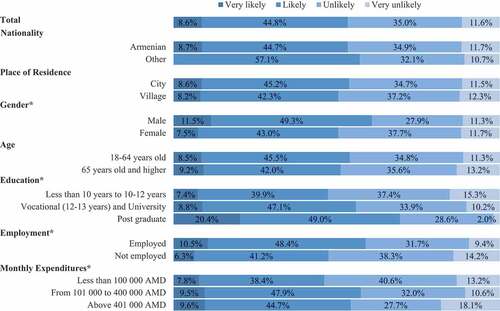
Out of 2,838 unvaccinated participants, about 53% (n = 1,516) were likely or very likely to get vaccinated. The intent to get vaccinated was significantly different among male and female participants, across the education levels, among employed and unemployed respondents, and by monthly expenditure levels ().
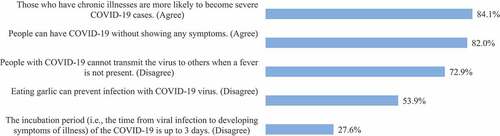
The vast majority of the respondents knew that COVID-19 might be asymptomatic (82.0%) and that people with chronic illnesses are more likely to have a severe case of COVID-19 (84.1%). About 70% of the respondents knew that COVID-19 can be transmitted even if the person does not have a fever. However, about half of the respondents did not know that eating garlic cannot prevent infection with COVID-19. Also, only about one third of the respondents disagreed with the statement that COVID-19 incubation period is up to 3 days. The mean knowledge score and knowledge percent score were 3.2 out of 5 (SD = 1.19) and 64.1%, respectively (). The knowledge score of the respondents intending to get vaccinated was significantly higher than the knowledge score of those without the intent (3.3 vs 3.1, p < .001).
About 70% of the respondents thought that they were very susceptible or susceptible to COVID-19 (). The susceptibility belief score was significantly different among those who intended and those who did not intend to get the vaccine (1.9 vs 1.7, respectively). However, only one third of the respondents perceived COVID-19 as a very severe or severe disease.
Table 2. COVID-19 susceptibility and severity, vaccine benefits, barriers, self-efficacy, cues to action and intent to get vaccinated.
About 66% of the participants strongly agreed or agreed that the COVID-19 vaccine protects from severe disease and death from COVID-19 (). This percentage was substantially higher among the respondents with intent to get the vaccine (72%) as compared with those without intent (28.0%). More than half of the participants thought that COVID-19 vaccination could give them COVID-19 disease and about 90% of the respondents thought that they are likely to experience side effects from the vaccine (). COVID-19 vaccination barriers score significantly differed among the respondents that had the intent (3.4) and those who did not have the intent (3.8) to get vaccinated. Overall, only 45.5% of the respondents thought that it would be very easy for them to get vaccinated against COVID-19 with a four times lower proportion among those with no intent (16.6%) compared to those who intended to get vaccinated (71.5%).
Television was the most frequently used source of information about COVID-19 in our sample with a mean score of 4.6, followed by social media (4.2), friends and relatives (4.1), and health care providers (3.6). The mean composite score of frequency of use of different sources was 3.0 (SD = 1.02), with substantially higher use among those with the intent to get vaccinated (3.2 vs 2.8).
describes the results of hierarchical multivariate logistic regression predicting the intent to receive a COVID-19 vaccine. Sociodemographic characteristics and COVID-19 knowledge explained only 6% of the variance in the intent to get vaccinated against COVID-19. Adding Block 3 with the HBM constructs of perceived threat, benefits and barriers increased the Nagelkerke R Square to 0.419. The final model including socio-demographic characteristics, knowledge score, and all HBM constructs, including cues to action, explained 43% of the variance.
Table 3. Hierarchical multivariate logistic regression predicting COVID-19 vaccination intent*.
In the final model, age, employment status, average monthly expenditures, perceived benefits, perceived barriers, perceived threat, self-efficacy, and cues to action were significantly associated with the intent to get the vaccine. The odds of COVID-19 vaccination intent were about 50% higher among employed participants compared to unemployed participants (OR = 1.47, 95% CI: 1.10–1.97, p = .009) and 59% higher among participants with average monthly expenditures from 101,100 to 400,000 AMD compared to participants with average monthly expenditures less than 100,000 AMD (OR = 1.59, 95% CI: 1.11–2.27, p = .011). A one-year increase in age increased the odds of vaccination intention by 1% (OR = 1.01, 95% CI: 1.00–1.02, p = .035). With a one-unit increase in the perceived threat score, the odds of intent to get vaccinated increased by 16% (OR = 1.16, 95%CI: 1.03–1.30, p = .017) in the adjusted analysis. The odds of COVID-19 vaccination intent were substantially higher among those participants who believed in the protective effect of the COVID-19 vaccine as compared with those who did not (OR = 3.31, 95% CI: 2.44–4.47, p = .000). The odds of vaccination intent were almost six times higher among those participants who believed that it would be very easy for them to get vaccinated (OR = 5.87, 95%CI: 4.38–7.86, p = .000] as opposed to those who thought it would be difficult. An increase in the mean score of cues to action was associated with 1.39 times higher odds of COVID-19 vaccination intent (OR = 1.39, 95% CI: 1.21–1.60, p = .000). Meanwhile, a higher score of barriers to vaccination was associated with substantially lower odds of COVID-19 vaccination intention (OR = 0.63, 95% CI: 0.53–0.74, p = .000).
Discussion
The purpose of this study was to explore factors explaining COVID-19 vaccination uptake in Armenia using HBM constructs. The final hierarchical logistic regression model containing socio-demographic factors, knowledge about COVID-19, and HBM constructs explained 44% of the variance in the intent to get vaccinated against COVID-19. Participants’ age, employment status, average monthly expenditures, perceived threat, benefits, perceived barriers, self-efficacy for COVID-19 vaccine, and cues to action were significant and independent predictors of the intent to get vaccinated.
Our nationwide survey found that between May to September 2021, out of 2,838 unvaccinated participants only about 53% (n = 1516) had the intent to get vaccinated. A similar rate (57.5%) was observed in Germany from February to April 2021.Citation42 Another cross-sectional survey conducted between January and March 2021 showed that 90.4% of the participants from 17 countries were likely or extremely likely to receive the COVID-19 vaccine; however, the proportions substantially differed between countries, ranging from 96.4% in Australia to 65.4% in Japan. In Iran, a neighboring country, about 70% of the participants had the intent to receive the vaccine.Citation43 These drastic differences between countries are difficult to interpret given that our survey and other surveys of this type are snapshots taken at a certain point in time in very different and changing contexts.Citation42,Citation43 Dynamic variations influenced by the phases of the outbreak, the availability of vaccines, and the stages of national vaccine rollouts are expected. For example, a scoping review on COVID-19 vaccine acceptance showed that globally the acceptance rate fluctuated notably between March 2020 (86%), July 2020 (54%), and September 2020 (72%).Citation44
In our study, the adjusted odds of COVID-19 vaccination intent were about 50% higher among employed participants. Similarly, in the US, COVID-19 vaccine acceptance was shown to be negatively associated with unemployment.Citation45 Although this survey was completed before the Armenia’s Government mandate was adopted, requiring biweekly COVID-19 PCR testing for unvaccinated employees, it is possible that employed participants expected this policy change based on the experience of other countries and/or had to conform to heightened social expectations to get vaccinated and overt or covert pressure from the employers and colleagues that unemployed individuals could avoid.Citation46 In addition, employed individuals might have had better sources of information about vaccines and had more of a chance to receive a vaccine through organized vaccination drives that the MoH was conducting for a number of large institutions and offices in Yerevan and the regions in that time period.
The marginally significant association of increasing age with intent to get vaccinated found in this study is in agreement with the international literature.Citation26,Citation28 Several authors assume that this could be explained by heightened perceptions of vulnerability to diseases and their consequences among older people.Citation42,Citation47–49 However, in our study this association was independent of perceived susceptibility and severity constructs explored as part of the HBM, which highlights the need to investigate other variables not explored in the scope of this analysis, possibly conveyed by age (i.e. social or emotional predictors of intention).Citation23
The odds of COVID-19 vaccination uptake were 59% higher among the participants with medium monthly expenditures (101,000 AMD-400,000 AMD) as compared with the odds among those reporting monthly expenditures below 100,000 AMD. Similar findings were reported in the global survey conducted across nine low-middle income countries, where high income was associated with greater vaccine acceptance.Citation50 The relationship between socio-economic status and various health-related behaviors has been well-demonstrated in the literature,Citation51 and several explanations have been proposed for this phenomenon, which could help understand the influence of the socio-economic status on the intent to get vaccinated above and beyond the constructs of the HBM explored in our study. For example, some researchers argue that less affluent members of society might believe that they have less to gain in terms of longevity from protective behaviors and have a lower capability for choosing and following the course of action that would extend their lives.Citation51–53 Others suggest that more affluent groups might adopt healthy behaviors as a primary source of their social identification.Citation51,Citation52 Irrespectively of the underlying mechanisms, our findings imply that future interventions toward increasing intent to get vaccinated and promoting the actual practice should target financially disadvantaged population groups.
While it is assumed that knowledge influences preventive behaviors indirectly via HBM constructs,Citation21 exploring its possible independent effects could be important in the context of infectious disease pandemic, where concerns about the well-being of others (not captured in our study) might influence behavior beyond perceived personal threat variables. In our analysis, knowledge score was not independently associated with the intention to get vaccinated in the final adjusted model. It should be noted that in the HBM, the scope of knowledge that could influence behavioral outcomes, is not delineated.Citation21 We assessed basic COVID-19 knowledge that was not related to vaccination.
Socio-demographic variables and knowledge explained only 6% of the variance in the hierarchical logistic regression, while the HBM constructs, including perceived benefits, barriers, self-efficacy and cues to action were strongly associated with vaccine uptake intent and added 37% to the explained variance.
In accordance with the tenets of the HBM, the odds of vaccine uptake intent in the adjusted analysis were substantially higher among those participants who believed in the protective effects of the vaccines against severe disease and death. Similar to our finding, the perceived benefits construct was a significant predictor for vaccination intention in IsraelCitation26 ChinaCitation54 Saudi Arabia,Citation55 Malaysia,Citation31 and Russia.Citation56 Greater perceived effectiveness of the vaccine was found to be one of the most important factors influencing vaccination intent in a nationally representative cross-sectional survey conducted in the UK,Citation24 and the only factor from the HBM that was associated with vaccination intention in the US.Citation57 Perceived vaccine effectiveness along with perceived safety and side-effects were the strongest predictors of vaccination intention according to several systematic reviews of the literature on potential factors influencing COVID-19 vaccine acceptance and hesitancy conducted in 2021.Citation58,Citation59 In our study as well, perceived barriers (including safety and side effects) were negatively associated with the intent to get the COVID-19 vaccine in the adjusted analysis.
While the evidence about the relative utility of different HBM constructs in explaining vaccination behavior is not conclusive, a systematic review of the research that used the Health Belief Model (HBM) as a theoretical basis to examine the influence of beliefs on health-related behaviors found that these two constructs have the most consistent association with the behaviors across various settings,Citation60–62 which is supported by our analysis.
A vast majority of the study participants (about 70%) believed that they are susceptible to COVID-19, while only one third of the respondents thought that contracting COVID-19 would be severe or very severe for them. In the multivariable analysis, the perceived threat score was a significant predictor for the vaccination intent in agreement with the HBM model.Citation21 However, separate constructs of perceived susceptibility and severity were not significantly associated with intention, which contradicts several studies where the association was confirmed.Citation31,Citation63 It is possible that in the context of COVID-19 preventive behaviors, individuals are motivated by the perceived threat for important others rather than beliefs about personal susceptibility and severity, which form the core of the HBM model.Citation23 Future research should investigate whether expanding the model constructs and assessing concern for others along with individual risk perceptions can increase the HBM’s suitability for predicting behaviors related to infectious disease prevention.
Many authors have argued that susceptibility and severity should be combined into the perceived threat construct; however, no conclusive evidence exists on whether the multiplicative or summative approach should be utilized and the construct is operationalized differently by different researchers.Citation21 In HBM, the relationship between two variables is not specified.Citation21 We tested the model with the multiplicative variable of perceived threat as well but failed to detect significant association, which implies that a summative score might be a better predictor of intention.
Cues to action construct (mean score of frequency of use of different sources of information on COVID-19) was another significant predictor of vaccination uptake in our adjusted analyses. Our findings suggest that disseminating adequate and evidence-based information through television and social media could increase the acceptance and actual uptake of the COVID-19 vaccines. However, since we did not ask direct questions about receiving vaccination-promoting cues due to time and resource limitations related to questionnaire administration, we assume that this association may only partially reflect the actual contribution of the original cues to action construct of the HBM to the vaccination intent.
The odds of intention to get the COVID-19 vaccine were five times higher among the participants who believed that it would be very easy for them to receive COVID-19 vaccine as compared with those who were not that confident. Greater perceived ease of vaccination explained COVID-19 vaccination intent in the UKCitation24,Citation64 and other countriesCitation26,Citation65 and was found important in the earlier research investigating the uptake of vaccines against H1N1.Citation66
Study strengths
This study used a large nationwide probability sample to explore COVID-19-related beliefs and vaccination intent, therefore our findings are essentially generalizable to the Armenian population. There are few studies exploring health-related behaviors in Armenia or in other post-Soviet countries using value-expectancy theoretical frameworks. The need for assessing the effectiveness of the HBM in different social, economic and cultural contexts has been amply stressed in the literature, and therefore this study is an important addition to the international body of evidence on this topic. We applied a full range of relevant constructs described by the HBM in a multivariable analysis of the predictors of vaccination uptake and utilized a hierarchical regression approach, which allowed quantifying the unique contribution of the HBM constructs to the variance in the vaccination intent.
Study limitations
We would like to recognize several study limitations. First, we aimed to explore the influence of HBM constructs on COVID-19 vaccination intent; hence, we did not consider the impact of normative influences on behavior,Citation67 which were found to be important predictors of COVID-19 vaccination intent in other studies.Citation26,Citation68 Logistical and time considerations forced us to assess several HBM constructs with one or two direct questions. Moreover, although it is recommended to use validated scales to obtain more accurate measures of health beliefs,Citation21 the questionnaire employed in this study was not validated.
The results should be interpreted with caution because we explored the reported intent of vaccination uptake, which may or may not translate into actual behavior. In addition, the current situation with COVID-19 in Armenia is quite different from the 2021 conditions, when this study was conducted. COVID-19-related beliefs might be time-sensitive and fluctuate along with changes in morbidity and mortality and the evolution of corresponding policies and interventions.
Conclusions
An improved understanding of factors influencing vaccination uptake can help tailor health communication messages and facilitate positive behavior change in Armenia. This study evidenced the utility of HBM in highlighting drivers of important health-protective behavior in the context of the pandemic. Health policymakers, communication specialists, and healthcare providers should particularly stress the effectiveness and safety of vaccines in their efforts to increase vaccination rates. The focus on unemployed and low-income population groups is warranted.
Disclaimer
“This study is made possible by the generous support of the American People through the United States Agency for International Development (USAID). The contents of this paper are the sole responsibility of the American University of Armenia Fund and do not necessarily reflect the views of USAID or the United States Government.”
Supplemental Material
Download PDF (202.2 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2165383.
Additional information
Funding
References
- World Health Organization. Considerations for implementing and adjusting public health and social measures in the context of COVID-19. 2021.
- James KJ, Martin AW, Andres BS, Rebecca MN. Global economic effects of COVID-19. Economics. [Published online 2020 Nov].
- Weekly epidemiological update on COVID-19 - 21 September 2022. [accessed 2022 Sep 22]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—21-september-2022.
- Li Y, Tenchov R, Smoot J, Liu C, Watkins S, Zhou Q. A comprehensive review of the global efforts on COVID-19 Vaccine Development. ACS Cent Sci. 2021;7(4):512. doi:10.1021/ACSCENTSCI.1C00120.
- WHO Coronavirus (COVID-19) Dashboard. WHO Coronavirus (COVID-19) dashboard with vaccination data. [accessed 2022 Sep 9]. https://covid19.who.int/.
- The European Union and UN Armenia welcome the arrival of COVID-19 vaccines to Armenia through the COVAX facility. [accessed 2022 Sep 9]. https://www.unicef.org/armenia/en/press-releases/european-union-and-un-armenia-welcome-arrival-covid-19-vaccines-armenia-through.
- Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, Kovyrshina AV, Lubenets NL, Grousova DM, Erokhova AS, et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia. Lancet. 2021;397:(10275):671–11. doi:10.1016/S0140-6736(21)00234-8.
- Vaccines available in Armenia - Covid. [accessed 2022 Jun 16]. https://covid.ncdc.am/en/vaccines-available-in-armenia.
- Booster shot - Covid. [accessed 2022 Jun 16]. https://covid.ncdc.am/en/booster.
- Dolzhikova IV, Gushchin VA, Shcheblyakov DV, Tsybin, A. N., Shchetinin, A. M., Pochtovyi, A. A, … & Gintsburg, A. L. One-shot immunization with Sputnik Light (the first component of Sputnik V vaccine) is effective against SARS-CoV-2 Delta variant: efficacy data on the use of the vaccine in civil circulation in Moscow. medRxiv. Published online Oct 2021. doi:10.1101/2021.10.08.21264715.
- Armenian company starts production of Russian Sputnik Light Covid-19 vaccines. [accessed 2022 Jun 16]. http://arka.am/en/news/society/armenian_company_starts_production_of_russian_sputnik_light_covid_19_vaccines/.
- National Centre for Disease Control. Covid-19 vaccination satistics. [accessed 2022 Sep 22]. https://covid.ncdc.am/en/statistics#daily_tab.
- The Government of the Republic of Armenia. Covid-19 regulation to take effect from October 1 will be equally applicable for persons holding public offices. [accessed 2022 Jun 8]. https://www.gov.am/en/news/item/9977/.
- Regarding the new restrictions. The Ministry of Health of Armenia. [accessed 2022 Jun 16]. https://www.moh.am/#1/4736.
- The RA Government. The Prime Minister of the Republic of Armenia.
- Armenia: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data WHO coronavirus (COVID-19) dashboard with vaccination data. [accessed 2022 Sep 22]. https://covid19.who.int/region/euro/country/am.
- Coronavirus Pandemic (COVID-19). Our World in data. [accessed 2022 Oct 10]. https://ourworldindata.org/coronavirus.
- Noar SM, Zimmerman RS. Health behavior theory and cumulative knowledge regarding health behaviors: are we moving in the right direction? Health Educ Res. 2005;20(3):275–90. doi:10.1093/HER/CYG113.
- Rosenstock IM. Historical origins of the health belief model. 1974;2(4):328–35. doi:10.1177/109019817400200403.
- Hochbaum GM. Public participation in medical screening programs; a socio-psychological study. (Book, 1958) [WorldCat.Org]. Vol. 572. Washington (DC): U.S. Government Printing Office; 1958.
- Glanz K, Rimmer BK, VK. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco (CA): HJohn Wiley and Sons, Inc; 2008.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1(4):139–61. doi:10.1016/0146-6402(78)90002-4.
- Guidry JPD, O’Donnell NH, Austin LL, Coman IA, Adams J, PB P. Stay socially distant and wash your hands: using the health belief model to determine intent for COVID-19 preventive behaviors at the beginning of the pandemic. Heal Educ Behav. 2021;48(4):424–33. doi:10.1177/10901981211019920.
- Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, Rubin GJ, Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17(6):1612–21. doi:10.1080/21645515.2020.1846397.
- Magnan RE, Gibson LP, Bryan AD. Cognitive and affective risk beliefs and their association with protective health behavior in response to the novel health threat of COVID-19. J Behav Med. 2021;44(3):285–95. doi:10.1007/s10865-021-00202-4.
- Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):804. doi:10.1186/s12889-021-10816-7.
- Matthews VS, Stough-hunter A, Marazita JM. Attitudes towards social distancing in response to COVID-19. Public Health Nurs. 2021;38(6):1019–29. doi:10.1111/phn.12954.
- Shewasinad Yehualashet S, Asefa KK, Mekonnen AG, Gemeda BN, Shiferaw WS, Aynalem YA, Bilchut AH, Derseh BT, Mekuria AD, Mekonnen WN, et al. Predictors of adherence to COVID-19 prevention measure among communities in North Shoa Zone, Ethiopia based on health belief model: a cross-sectional study. Thet Wai K, ed. PLoS One. 2021;16(1):e0246006. doi:10.1371/journal.pone.0246006.
- Tong KK, Chen JH, Yu EW, Wu AMS. Adherence to COVID-19 precautionary measures: applying the health belief model and generalised social beliefs to a probability community sample. Appl Psychol Heal Well-Being. 2020;12(4):1205–23. doi:10.1111/aphw.12230.
- Bressington DT, Cheung TCC, Lam SC, Suen LKP, Fong TKH, Ho HSW, Xiang Y-T. Association between depression, health beliefs, and face mask use during the COVID-19 pandemic. Front Psychiatry. 2020;11:11. doi:10.3389/fpsyt.2020.571179.
- Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. doi:10.1080/21645515.2020.1790279.
- Moussaoui LS, Ofosu ND, Desrichard O. Social psychological correlates of protective behaviours in the COVID-19 outbreak: evidence and recommendations from a nationally representative sample. Appl Psychol Heal Well-Being. 2020;12(4):1183–204. doi:10.1111/aphw.12235.
- The Demographic Handbook of Armenia, 2019 Statistical committee of the Republic of Armenia. [accessed 2022 Jun 13]. https://armstat.am/en/?nid=82&id=2225.
- AUA Center for Health Services Research and Development. Support to control COVID-19 and other infectious disease outbreaks. [accessed 2022 Sep 30]. https://chsr.aua.am/support-to-control-covid-19-and-other-infectious-disease-outbreaks-a-three-year-project-in-partnership-with-the-ministry-of-health-government-of-armenia/.
- Andreasyan D, Bazarchyan A, Matevosyan M, Mirzoyan L, Muradyan G, Simonyan A, Simonyan S. «Health and health care» yearbook Republic of Armenia. Yerevan, Armenia: National Institute of Health Named After Academician S. Avdalbekyan; 2020.
- National electronic healthcare operator CJSC. [accessed 2022 Jun 16]. https://corporate.armed.am/en/about-us.
- Wayne WD. Biostatistics: a foundation for analysis in the Health Sciences. 10th ed. Hoboken (NJ): Wiley; 2013.
- Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Heal Surveill. 2020;6(2):e19161. doi:10.2196/19161.
- Parsons Leigh J, Fiest K, Brundin-Mather R, Plotnikoff K, Soo A, Sypes EE, Whalen-Browne L, Ahmed SB, Burns KEA, Fox-Robichaud A. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: self-reported beliefs, knowledge, and behaviors. Tu WJ, ed. PLoS One. 2020;15(10):e0241259. doi:10.1371/journal.pone.0241259.
- WHO Regional Office for Europe. Survey tool and guidance. Rapid, simple, flexible behavioural insights on COVID-19. Copenhagen, Denmark: WHO Regional Office for Europe; 2020.
- Enterprise online survey software & tools - alchemer. [accessed 2022 Jun 16]. https://www.alchemer.com/.
- Umakanthan S, Lawrence S. Predictors of COVID-19 vaccine hesitancy in Germany: a cross-sectional, population-based study. Postgrad Med J. 2022;98(1164):756–64. Published online Feb 2022:postgradmedj-2021-141365. doi:10.1136/postgradmedj-2021-141365.
- Wong LP, Alias H, Danaee M, Ahmed J, Lachyan A, Cai CZ, Lin Y, Hu Z, Tan SY, Lu Y, et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: a global survey of 17 countries. Infect Dis Poverty. 2021;10:(1):122. doi:10.1186/s40249-021-00900-w.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;9:9. doi:10.3389/fpubh.2021.698111.
- Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. E Clin Med. 2020;26:100495. doi:10.1016/j.eclinm.2020.100495.
- Belle N, Cantarelli P. Nudging public employees through descriptive social norms in healthcare organizations. Public Adm Rev. 2021;81(4):589–98. doi:10.1111/puar.13353.
- Malesza M, Wittmann E. Acceptance and intake of COVID-19 vaccines among older Germans. J Clin Med. 2021;10(7):1388. doi:10.3390/JCM10071388.
- Banik R, Islam MS, Pranta MUR, Rahman QM, Rahman M, Pardhan S, Driscoll R, Hossain S, Sikder MT. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infect Dis. 2021;21:(1). doi:10.1186/S12879-021-06406-Y.
- Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002. doi:10.1016/J.VACCINE.2020.09.041.
- Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, Hasan MT, Sessou P, Ditekemena JD, Amodan BO, Hosseinipour MC, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. 2021;9:(5):515. doi:10.3390/vaccines9050515.
- Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36(1):349–70. doi:10.1146/annurev.soc.012809.102529.
- Cockerham W. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. 2005;46(1):51–67. doi:10.1177/002214650504600105.
- Lawlor DA, Frankel S, Shaw M, Ebrahim S, Smith GD. Smoking and Ill health: does lay epidemiology explain the failure of smoking cessation programs among deprived populations? Am J Public Health. 2003;93(2):266–70. doi:10.2105/AJPH.93.2.266.
- Yu Y, Lau JTF, She R, Chen X, Li L, Li L, Chen X. Prevalence and associated factors of intention of COVID-19 vaccination among healthcare workers in China: application of the health belief model. Hum Vaccin Immunother. 2021;17(9):2894–902. doi:10.1080/21645515.2021.1909327.
- Mahmud I, Kabir R, Rahman MA, Alradie-Mohamed A, Vinnakota D, Al-Mohaimeed A. The health belief model predicts intention to receive the COVID-19 vaccine in Saudi Arabia: results from a cross-sectional survey. Vaccines. 2021;9(8):864. doi:10.3390/vaccines9080864.
- Tran VD, Pak TV, Gribkova EI, Galkina GA, Loskutova EE, Dorofeeva VV, Dewey RS, Nguyen KT, Pham DT. Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia. Pharm Pract (Granada). 2021;19(1):2276. doi:10.18549/PharmPract.2021.1.2276.
- Rabin C, Dutra S. Predicting engagement in behaviors to reduce the spread of COVID-19: the roles of the health belief model and political party affiliation. Psychol Health Med. 2022;27(2):379–88. doi:10.1080/13548506.2021.1921229.
- Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review. Delcea C, ed. PLoS One. 2022;17(3):e0265496. doi:10.1371/journal.pone.0265496.
- Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2020;9(1):16. doi:10.3390/vaccines9010016.
- Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi:10.1177/109019818401100101.
- Limbu YB, Gautam RK, Pham L. The health belief model applied to COVID-19 vaccine hesitancy: a systematic review. Vaccines. 2022;10(6):973. doi:10.3390/vaccines10060973.
- Sulat JS, Prabandari YS, Sanusi R, Hapsari ED, Santoso B. The validity of health belief model variables in predicting behavioral change. Health Educ. 2018;118(6):499–512. doi:10.1108/HE-05-2018-0027.
- Wong MCS, Wong ELY, Huang J, Cheung AWL, Law K, Chong MKC, Ng RWY, Lai CKC, Boon SS, Lau JTF, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39:(7):1148–56. doi:10.1016/j.vaccine.2020.12.083.
- Griffin B, Conner M, Norman P. Applying an extended protection motivation theory to predict Covid-19 vaccination intentions and uptake in 50–64 year olds in the UK. Soc Sci Med. 2022;298:114819. doi:10.1016/j.socscimed.2022.114819.
- Eberhardt J, Ling J. Predicting COVID-19 vaccination intention using protection motivation theory and conspiracy beliefs. Vaccine. 2021;39(42):6269–75. doi:10.1016/j.vaccine.2021.09.010.
- Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566–76. doi:10.1080/10410236.2013.873363.
- Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. Taylor and Francis; 2010. doi:10.4324/9780203838020.
- Lueck JA, Spiers A. Which beliefs predict intention to get vaccinated against COVID-19? A mixed-methods reasoned action approach applied to health communication. J Health Commun. 2020;25(10):790–98. doi:10.1080/10810730.2020.1865488.