ABSTRACT
Vaccine hesitancy during the COVID-19 pandemic continues to be an issue in terms of global efforts to decrease transmission rates. Despite high demand for the vaccines in Nepal, the country still contends with challenges related to vaccine accessibility, equitable vaccine distribution, and vaccine hesitancy. Study objectives were to identify: 1) up-take and intention for use of COVID-19 vaccines, 2) factors associated with vaccine up-take, and 3) trusted communication strategies about COVID-19 and the vaccines. A quantitative survey was implemented in August and September 2021 through an initiative at the Nepali Ministry of Health and Population Department of Health Services, Family Welfare Division. Data were collected from 865 respondents in three provinces (Bagmati, Lumbini, and Province 1). Ordinal multivariate logistic regression was utilized to determine relationships between vaccination status and associated factors. Overall, 62% (537) respondents were fully vaccinated and 18% (159) were partially vaccinated. Those respondents with higher education (p < .001) and higher household income (p < .001) were more likely vaccinated. There were also significant differences in vaccine up-take across the three provinces (p < .001). Respondents who were vaccinated were significantly more likely to perceive vaccines as efficacious in terms of preventing COVID-19 (p = .004) and preventing serious outcomes (p = .010). Among both vaccinated and unvaccinated individuals, there was a high level of trust in information about COVID-19 vaccines provided through local health-care workers [e.g. nurses and physicians]. These results are consistent with other findings within the South Asia region. Targeted advocacy and outreach efforts are needed to support ongoing COVID-19 vaccination campaigns throughout Nepal.
Introduction
A broad range of policy, programmatic, historical, socioeconomic, and behavioral factors affect vaccine acceptance and uptake.Citation1 Three key components of vaccine hesitancy have been defined as ‘convenience’ (e.g., accessibility), ‘complacency’ (e.g., disease risk, importance of vaccines), and confidence (e.g., trust in product, providers, and policymakers, perceived vaccine safety, and efficacy).Citation2,Citation3 Studies of acceptance of COVID-19 vaccines have also utilized behavioral change theories to understand predictors of vaccine up-take.Citation4–6
Although there is evidence that there is higher willingness to receive a COVID-19 vaccine in low- and middle-income countries, there are differences in acceptance rates across social-cultural and economic groups and across and within countries.Citation7 In a systematic review of 11 countries, differences in vaccine acceptance rates also varied across countries by the number of COVID-19 deaths per one million persons.Citation8 COVID-19 vaccine hesitancy studies have been undertaken in South Asia, including in Bangladesh, India, and Pakistan.Citation9–12 However, there remains limited research in Nepal.
Overall, Nepal is a high-coverage country in terms of the National Immunization Program (NIP) with an estimated pentavalent (DTP3HibHepB) up-take of 93% as of 2019.Citation13 However, there are significant variations in routine immunization uptake in different provinces of the country and lower vaccine up-take is associated with maternal low literacy and poverty.Citation14
Since 3 January 2020, there have been over 992,000 confirmed cases of COVID-19 and 11,951 deaths in Nepal. There have been three peak periods of COVID-19 infections. The first peak occurred between September and November 2020, the second peak between April and August 2021, and the third peak occurred in January 2022.Citation15
Existing immunization structures under the authority of the Family Welfare Division at Ministry of Health and Population (MOHP) were harnessed for the COVID-19 vaccine rollout. Nepal deployed COVID-19 vaccines on 27 January 2021 in all seven provinces. Initial implementation focused on health professionals and other frontline workers and adults >60 years. At the time of the survey in August–September 2021, with increasing access to vaccines, the campaign was extended to all adults >18 years. There were no mandatory vaccination policies throughout the campaigns. Six vaccines were approved by the Nepali government prior to the survey including AstraZeneca-University of Oxford, Sinopharm, Bharat Biotech International Limited, Gamaleya Research Institute and Health Ministry of the Russian Federation, Sinovac Research & Development, Ltd., and Janssen Pharmaceutical. In late September, Pfizer-BioNTech and Moderna-NIAID were approved.Citation16 As of August 2022, over 53 million doses of COVID vaccines have been delivered.Citation15
The COVID-19 pandemic seriously impacted health systems at a global level.Citation17 Health systems were overwhelmed caring for COVID-19 patients, national and regional lockdowns decreased access to care, and health systems were shut down for routine services.Citation18,Citation19 Within this context, the introduction of new COVID-19 vaccines has posed challenges in terms of allocation, distribution, introduction, and community uptake. In Nepal, despite high demand for the vaccines and a successful roll-out, challenges continue in relation to vaccine accessibility as well as vaccine hesitancy and uptake.Citation20
The objectives of this paper are to: 1) identify up-take and intention to receive COVID-19 vaccines among 18- to 59-year-old adults including those engaged in prioritized occupations and older adults >60 years living in Kathmandu Valley (Bagmati Province) and rural areas in Eastern (Province 1) and Western (Lumbini Province) Nepal; 2) identify factors associated with COVID-19 vaccine status; and, 3) identify trusted sources of information regarding COVID-19 and COVID-19 vaccines within the study populations.
Materials and methods
Study sites and population
The project utilized a quantitative cross-sectional survey design. Nepal is divided into three north-to-south regions [Mountains, Hills, and Terai (Plains)] and seven provinces. One urban site from Bagmati province (which includes Kathmandu Valley) and two rural sites from Province 1 and Lumbini Provinces were purposefully selected to represent three geographical regions of the country. Approximately 46% of the population lives in the Hills region with 2.5 million persons in Kathmandu Valley.
At the municipal and ward levels, simple random sampling was employed to select study sites. Lists of municipalities and wards within the three study provinces were created and selected using randomly generated numbers. Within Bagmati, four municipalities were randomly selected (Kathmandu, Kirtipur, Lalitpur, and Mahalaxmi). In Province 1, two rural municipalities (Koshi and Gadi) in the Susari District and in Lumbini, two rural municipalities (Bagnaskali and Ripdikot) in the Palpa District were randomly selected. In each municipality, three wards were randomly selected as survey sites for a total of 12 urban and 12 rural wards (see ).
The study population was defined as the targeted populations at the beginning of COVID-19 vaccine introduction (persons >60 years and those in prioritized occupations) and the general population of persons 18–59 years. For prioritized occupations, data collectors went to health facilities and other offices of frontline workers in the selected regions to conduct the survey. For community respondents, households were sequentially selected based on the number of households and sample size for that ward.
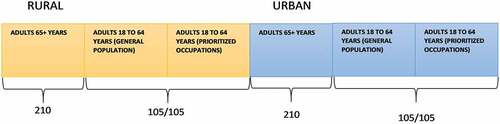
Sample size
The sample size was calculated to enable comparison across urban and rural areas and across populations (18–59 years general population, 18–59 years prioritized occupations, 60+ years). Based on an estimate of 25% hesitancy (prevalence [P]=.25), level of confidence =.99, and precision =.03 for a sample size of 840 ().
Survey development and data collection
The survey was designed based on previous global research on vaccine hesitancy and adapted for specific issues related to adult vaccination, COVID-19, and the sociocultural context of Nepal.Citation2,Citation21,Citation22 The survey consisted of eight sections: 1) respondent demographics and household characteristics; 2) experience with COVID-19; 3) perceived disease vulnerability and severity; 4) general experience with vaccines; 5) information sources and general perceptions of COVID-19 vaccines; 6) COVID-19 vaccine access, up-take/intent to use; 7) COVID-19 vaccine confidence; and, 8) Preferred sources and communication strategies for receiving information about COVID-19 vaccines. The survey was piloted with 25 respondents and minor revisions were made prior to implementation.
Survey data were collected through personal digital assistants (PDAs) using REDCap between 2 August 2021 and 15 September 2021. REDCap is a secure web application for building and managing online surveys and databases.Citation23 Through REDCap, both Nepal- and US-based investigators had immediate access to survey data as it was collected. Surveys were conducted face-to-face in Nepali and data collection took an estimated 30–45 minutes per survey.
Data management and analysis
Data cleaning includes creation of variables for scales and use of descriptive statistics to screen for missing cases, outliers, and normality of distributions. Ordinal multivariate logistic regression was performed to determine the relationships between vaccination status (fully, partial, unvaccinated) and demographic and exposure variables. Analysis also focused on descriptive statistics and bivariate analysis to identify significant differences which indicate potential associations and relationships across independent variables. Bivariate analysis included Pearson’s chi-square and independent t-tests and ANOVA (continuous variables). Pairwise comparisons were made using chi-square test with a Benjamini Hochberg multiple comparisons adjustment. The statistical significance is set at p < .05. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS 25 (IBM Corp, Armonk, NY, USA).
Ethical approval
This study was reviewed and approved by the Nepal Health Research Council, Kathmandu, Nepal (protocol number 385/2021 P). All participants signed a consent form prior to completing the survey.
Results
Demographics
A total of 865 surveys were collected. Overall, 50.5% (n = 437) of respondents were male. Mean age was 50.3 years (SD 18.0) with a range from 18 to 90 years. Fifty percent (n = 432) of respondents lived in Bagmati Province [urban], 25.1% (n = 217) in Province 1 [rural], and 24.9% (n = 215) in Lumbini [rural]. Bivariate analysis indicates differences across study sites by gender (p = .02), education (p < .001), employment status (p < .001), and monthly household income (p < .001). In Lumbini Province there were significantly more female respondents than in Bagmati or Province 1. In Lumbini and Province 1, there were more respondents with no formal schooling compared to Bagmati Province and there were more respondents with university/professional education in Bagmati Province compared to the two rural sites. More respondents reported full-time employment in Bagmati Province than Lumbini or Province 1 and there were more unemployed/retired respondents in Lumbini compared to Province 1. In terms of monthly household income, Bagmati respondents reported higher income than respondents in both Lumbini and Province 1 ().
Table 1. Pairwise comparisons for significant demographic variables.
Demographics and COVID-19 vaccination status
Overall, 62% (537) of respondents reported being fully vaccinated, 18% (159) were partially vaccinated [received one dose of a two-dose vaccine] and 20% (168) were unvaccinated. Among those who were not vaccinated, 71% (118) said that they would get the vaccine as soon as possible. Among the remaining unvaccinated respondents, 13% (22) were undecided, 12% (20) would probably not take the vaccine, and 4% (7) stated they would delay one to 2 months before receiving the vaccine.
There was no difference in terms of vaccination status [fully vaccinated, partially vaccinated, unvaccinated] by gender (p = .17) or by employment status (p = .14). Respondents fully/partially vaccinated (51.8 years, SD 17.47) were older than those unvaccinated (44.1 years, SD 19.10) [p = .001]. There were also significant differences in vaccination status by education, province, and household income. Respondents with primary (52.3%, 81) [p < .001] or secondary school (57.8%, 115) [p < .001] education were more than 2 times less likely to be fully vaccinated than respondents with university or professional degrees (81.4%, 171). Compared to respondents in Lumbini Province (63.0%, 136), Province One respondents (33.2%, 72) [p < .001] were less likely to be fully vaccinated (63.0%, 136) and Bagmati respondents were more likely to be fully vaccinated (76.3%, 329) [p = .011]. Respondents with a household income of less than 15,000 Nepali Rubee (NPR)/month (33.3%, 31) [<0.001] were 3 times less likely to be fully vaccinated than respondents with incomes over 45,000 NPR/month (75.8%, 184) and those with incomes 15,000 to 30,000 NPR/month (48.6%, 136) [p = .001] were 2 times less likely to be fully vaccinated than the highest income group ().
Table 2. Demographic characteristics and vaccine status.
Personal experiences and impact of COVID-19 and vaccination status
Respondents were asked a series of questions regarding their experiences with COVID-19 and the impact of the pandemic on their lives. Respondents in the urban province (Bagmati) reported more experiences with COVID-19 than residents in the two rural provinces (Lumbini and Province 1). However, nearly 40% of Bagmati and Lumbini participants reported personally knowing someone who died from COVID. Across all three provinces, greatest impact related to job loss and decrease in income, inability to see family and friends, and feelings of sadness, depression, and anxiety. () In terms of vaccination status, those individuals who reported having been tested for COVID-19 were less likely to be partially/unvaccinated (OR 0.54 [0.35–0.82, p = .004]). In terms of the impact of COVID-19, those that lost their job and/or experienced a decrease in income were more than two times as likely to be partially/unvaccinated (OR 2.02 [1.39–2.93, p < .001]). Those that reported feelings of sadness, depression, and/or anxiety during the pandemic were less likely to be partially/unvaccinated (0.59 [0.41–0.86, p = .006]) ().
Table 3. COVID-19 experiences and impact by provinces.
Table 4. Experience and impact of COVID-19 by vaccination status.
Perceptions of COVID-19 vulnerability and severity
On a four-point scale, participants were asked about perceptions of personal vulnerability and disease severity related to COVID-19 and four other infectious diseases, which are endemic in Nepal (typhoid fever, cholera, influenza, and dengue fever). Overall, COVID-19 was perceived as significantly more severe and participants reported perceiving that they or household members were more likely to contract COVID-19 compared to other diseases. () However, there was no relationship between vaccination status and either perceptions of vulnerability (OR 0.73 [0.47–1.12]/p = .147) or severity (OR 1.00 [0.25–4.06]/p = .446).
Table 5. Perceptions of vulnerability and severity for COVID-19 compared to dengue fever, typhoid fever, cholera, and influenza.
Vaccine confidence and vaccination status
Vaccination confidence includes a broad range of factors including positive and negative perceptions of the characteristics, benefits, and risk of the product (vaccine), trust in pharmaceutical companies that produce vaccines, trust in government agencies that approve and implement vaccination programs, and trust in the health system and healthcare providers.Citation24 In terms of perceptions regarding COVID-19 vaccines, those respondents who agreed that COVID-19 vaccines would decrease risk for getting COVID-19 (p = .004) or decrease risk of a serious case of COVID-19 (p = .010) were significantly less likely to be partially/unvaccinated. () Alternatively, those respondents who were concerned the vaccine could have a negative effect on babies in the future were more likely to be partially/unvaccinated (p = .021) ().
Table 6. Positive perceptions about COVID-19 vaccines and vaccination status.
Table 7. Negative perceptions about COVID-19 vaccines and vaccination status.
Respondents indicated greatest confidence in local health-care workers (e.g., nurses and physicians) as trusted sources for information about COVID-19 vaccines. Female Community Health Volunteers (FCHVs) were significantly more trusted in Lumbini than in either Bagmati or Province 1. In addition, across the three study sites there were significant differences in levels of trust in pharmacists/medical shop owners, representatives of district and local health services, pharmaceutical companies, and experts and scientists. () Those respondents who reported trust in health-care workers were less likely to be partially/unvaccinated (OR 0.13 [0.03–0.05]/p = .01). There were no significant differences in relation to vaccination status and trust for the other groups.
Table 8. Trusted sources for information about COVID-19 vaccines (‘trust a lot’) by province.
Perceptions of COVID-19 vaccines among healthcare workers
Health-care workers were one of the first groups of vaccine recipients in Nepal. Overall, 88.9% (176/198) of healthcare workers were fully vaccinated, (8.6%, 16) were partially vaccinated, and 2.5% (n = 5) were unvaccinated. A vast majority of health-care workers agreed that use of the vaccine would decrease risk of contracting COVID (91.9%/n = 182) and decrease risk of serious COVID (e.g., hospitalization) (94.9%/186). However, health-care workers did report concerns about the vaccine in terms of side effects, the risk of getting COVID-19 from the vaccine, and concerns about the development, production, and vaccine trials ().
Table 9. COVID-19 vaccine perceptions among health-care workers.
Discussion
A range of factors have been identified at a global level affecting up-take of COVID-19 vaccines. In a review of global studies, these factors include gender, age, education, occupation, trust in authorities, vulnerability, and vaccine efficacy and safety.Citation25 In our study, higher education and higher monthly household income were associated with vaccine up-take, as well as, COVID-19 socio-economic impact and experience, vaccine safety and efficacy, and trust in health-care workers. Other regional studies in Bangladesh, India, and Pakistan have also found differences in vaccine acceptance by education and income, as well as vaccine efficacy. Within the region, other studies have also indicated differences in acceptance by gender, age, perceived personal risk, and vaccine production country of origin.Citation9–12
In Nepal, there were variations by the study site for vaccine acceptance including significant differences between the two rural sites. Differences in COVID-19 acceptance by geopolitical and socio-economic regions was similarly reported in a study in Bangladesh.Citation9 These differences highlight the need for in-country studies within and across regions to identify both generalized and specific factors contributing to vaccine acceptance. Variations by regions also require that outreach and communication efforts need to focus on different messaging in different areas of the country and not rely on “all-in-one” messaging for the entire country. This is in keeping with consistent widescale findings regarding COVID-19 messaging in general and for vaccines.Citation26
Over 50% of the total respondents reported feelings of depression, anxiety, and sadness during the pandemic with the highest rate in the urban site (63.3%). Literature suggests that concurrent with the pandemic, there is a mental health crisis both in terms of care for those who are diagnosed and identification of emerging mental health challenges across demographic groups and populations.Citation27, Citation28–30 In addition, over 65% of the respondents reported loss of job or decrease in income. These respondents were less likely to be fully vaccinated. On the other hand, those reporting feelings of depression, anxiety, and sadness were more likely to be fully vaccinated. At a global level, more research is needed to increase our understanding of the impact of complex socio-economic and psychosocial factors on families and communities during the pandemic and how these factors might contribute to engagement in preventive practices including vaccine up-take.Citation31
In terms of vaccine hesitancy and complacency, severity, and vulnerability have been shown to contribute to decision-making about the use of vaccines.Citation32 In this study, there was no difference in perceptions about COVID-19 in terms of personal risk or disease severity between vaccination groups. This may be related to the overall high scores regarding perceptions of COVID-19 vulnerability and severity which suggests a general high level of concern among respondents about the disease.
Those who reported having been tested were more likely to be vaccinated. One interpretation of these data is that personal exposure (and therefore perceived risks) may affect vaccination acceptance. Alternatively, those who go for testing may be more concerned about disease spread and prevention and therefore more likely to be vaccinated.
Respondents who were vaccinated had more positive perceptions of COVID-19 vaccines in relation to vaccine effectiveness both in terms of preventing COVID-19 and decreasing risk for serious COVID (e.g., hospitalization). Those who perceived that the vaccine could have an effect on babies born in the future were more likely to be unvaccinated. Concerns about fertility and/or potential impact on future pregnancies are often associated with vaccine hesitancy. In the case of the COVID-19 vaccines, multiple factors have contributed to these concerns including the relatively short period of time for vaccine development, exclusion of pregnant women in early trials, and the persistent and rapid dissemination of information/misinformation through social media.Citation33–35 However, specific concerns about fertility and other negative perceptions including risk of contracting COVID from the vaccine, rapid vaccine development, and country of origin for vaccines and trials were not significantly related to vaccination status.
Health-care workers can also be vaccine hesitant.Citation36,Citation37 In a 23 country study, approximately 15% of health-care workers were hesitant regarding use of COVID-19 vaccines.Citation38 Reasons cited include vaccine safety and efficacy, and distrust in vaccine science. In Nepal, less than 3% of health-care workers respondents were unvaccinated. However, negative perceptions of vaccine risks were reported by health-care workers including those who were vaccinated. In Nepal, the overall trust in local health-care workers can provide one approach that will ensure that specific barriers in different areas are addressed. Because of this level of trust, it is imperative that health-care workers are trained and have up-to-date information available to share with their patients and in their communities.Citation39 This could support a two-tiered approach in which local health-care providers receive training and training materials that they can use within their clinics and communities.
COVID-19 vaccination campaigns continue to be an essential component of disease prevention at a global level. Based on the differences contributing to vaccine hesitancy by demographics, experiences, and perceptions, public health communications must pursue a range of strategies to increase public confidence in available COVID-19 vaccines.Citation40 COVID-19 vaccine hesitancy remains an issue in Nepal and there is a need for ongoing efforts to communicate about the disease and vaccines, including boosters and vaccination of children and adolescents. However, these campaigns need to be locally focused on factors affecting vaccine up-take in diverse communities throughout Nepal and globally.Citation41
There are limitations to this study. First, the study is cross-sectional and so assumptions cannot be made about direction or causality. The study was initiated in July 2021 and approved by the national ethics council in time for data to be collected in August and September 2021. The situation with COVID-19 in terms of prevalence, vaccine accessibility, vaccine policies concerning eligible recipients, and other prevention strategies change quickly. The oversampling of older adults may skew the results as these demographic groups were initially targeted for receipt of the vaccine. Due to funding restrictions, we were only able to conduct surveys in three provinces. However, the study team calculated a sample size which allowed data analysis by residency (urban/rural), province, and demographic groups. There was only one item to measure feelings of sadness and anxiety. Validated scales for depression or anxiety were not included in the survey and therefore may limit comparability with other studies of COVID-19 and mental health.
Acknowledgements
This study was funded through the Global Health Initiative, Henry Ford Health, Detroit MI. We would like to thank all of our partner organizations and individuals involved in the design, implementation, and analysis for this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Adrien P, Francois J, Parke D, Bebekoski T, Boncy PJ, Corvil S, Existe A, Jacques R, Joseph G, Kaljee LM, et al. Establishing and utilizing strategic partnerships for vaccine-preventable diseases: best practices in Haiti. Infect Dis Clin Pract. 2018;26(5):252–9. doi:10.1097/IPC.0000000000000644.
- Larson HJ, Schulz WS, Tucker JD, Smith DM. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 2015;7. doi:10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4.
- Pach A, Tabbusam G, Khan MI, Suhag Z, Hussain I, Hussain E, Mumtaz U, Haq IU, Tahir R, Mirani A, et al. Formative research and development of an evidence-based communication strategy: the introduction of Vi typhoid fever vaccine among school-aged children in Karachi, Pakistan. J Health Commun. 2013;18(3):306–24. doi:10.1080/10810730.2012.727958. PMID: 23330632.
- Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. doi:10.1080/21645515.2020.1790279.
- Fan CW, Chen IH, Ko NY, Yen CF, Lin C, Griffiths MD, Pakpour AH. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):3413–20. doi:10.1080/21645515.2021.1933687.
- Huang PC, Hung CH, Kuo YJ, Chen YP, Ahorsu DK, Yen CF, Lin C, Griffiths MD, Pakpour AH. Expanding protection motivation theory to explain willingness of COVID-19 vaccination uptake among Taiwanese university students. Vaccines. 2021;9:1046. doi:10.3390/vaccines9091046.
- Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385–94. doi:10.1038/s41591-021-01454-y. PMID: 34272499; PMCID: PMC8363502.
- Kukreti S, Rifai A, Padmalatha S, Lin CY, Yu T, Ko WC, Chen PL, Strong C, Ko NY. Willingness to obtain COVID-19 vaccination among the general population – a systematic review and meta-analysis. J Glob Health. 2022;12:05006.
- Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, Hossain MA, Mamun AA. COVID-19 vaccine hesitancy among the adult population in Bangladesh: a nationwide cross-sectional survey. PLoS One. 2021;16(12):e0260821. doi:10.1371/journal.pone.0260821. PMID: 34882726; PMCID: PMC8659424.
- Ali M, Hossain A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ Open. 2021;11(8):e050303. doi:10.1136/bmjopen-2021-050303. PMID: 34429316; PMCID: PMC8387740.
- Chandani S, Jani D, Sahu PK, Kataria U, Suryawanshi S, Khubchandani J, Thorat S, Chitlange S, Sharma D. COVID-19 vaccination hesitancy in India: state of the nation and priorities for research. Brain Behav Immun Health. 2021;18:100375. doi:10.1016/j.bbih.2021.100375. PMID: 34693366; PMCID: PMC8523306.
- Tahir MJ, Saqlain M, Tariq W, Waheed S, Tan SHS, Nasir SI, Ullah I, Ahmed A. Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health. 2021;21(1):1759. doi:10.1186/s12889-021-11814-5. PMID: 34565351; PMCID: PMC8474768.
- World Health Organization. Regional Office for South-East Asia. Nepal factsheet 2020: expanded programme on Immunization (EPI). World Health Organization. Regional Office for South-East Asia; 2020 [accessed 2022 Aug 3]. https://apps.who.int/iris/handle/10665/336761.
- Acharya K, Paudel YR, Dharel D. The trend of full vaccination coverage in infants and inequalities by wealth quintile and maternal education: analysis from four recent demographic and health surveys in Nepal. BMC Public Health. 2019 Dec 12;19(1):1673. doi:10.1186/s12889-019-7995-3. PMID: 31830944; PMCID: PMC6909493.
- World Health Organization. COVID-19 dashboard: Nepal; 2022. [accessed 2022 Aug 12]. Nepal: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data
- Gaire A, Panthee B, Basyal D, Paudel A, Panthee S. COVID-19 vaccine acceptance: a case study from Nepal. COVID. 2022;2(8):1014–25. doi:10.3390/covid2080075.
- Polašek O, Wazny K, Adeloye D, Song P, Chan KY, Bojude DA, Ali S, Bastien S, Becerra-Posada F, Borrescio-Higa F, et al. Research priorities to reduce the impact of COVID-19 in low- and middle-income countries. J Glob Health. 2022;15(12):09003. doi:10.7189/jogh.12.09003. PMID: 35475006; PMCID: PMC9010705.
- Suwantika AA, Boersma C, Postma MJ. The potential impact of COVID-19 pandemic on the immunization performance in Indonesia. Expert Rev Vaccines. 2020;19(8):687–90. doi:10.1080/14760584.2020.1800461. PMID: 32758031.
- United Nations Children’s Fund (UNICEF). Impact of COVID-19 on vaccine supplies. UNICEF Supply Division; 2021 [accessed 2022 Aug 16].
- Bhattarai S, Dhungana J. A million-dose success for Nepal: insights from Nepal’s national vaccine deployment plan against COVID-19. J Travel Med. 2021;28(4):taab027. doi:10.1093/jtm/taab027. PMID: 33668060; PMCID: PMC7989250.
- Kaljee LM, Pham V, Son ND, Hoa NT, Thiem VD, Canh DG, Thoa le TK, Ali M, Ochiai RL, Danovaro-Holliday MC, et al. Trial participation and vaccine desirability for Vi polysaccharide typhoid fever vaccine in Hue City, Viet Nam. Trop Med Int Health. 2007;12(1):25–36. doi:10.1111/j.1365-3156.2006.01751.x. PMID: 17207145.
- Kar SK, Pach A, Sah B, Kerketta AS, Patnaik B, Mogasale V, Kim YH, Rath SB, Shin S, Khuntia HK, et al. Uptake during an oral cholera vaccine pilot demonstration program, Odisha, India. Hum Vaccin Immunother. 2014;10(10):2834–42. doi:10.4161/21645515.2014.971655. PMID: 25483631; PMCID: PMC5443101.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi:10.1016/j.jbi.2008.08.010. PMID: 18929686; PMCID: PMC2700030.
- Ahorsu DK, Lin CY, Yahaghai R, Alimoradi Z, Broström A, Griffiths MD, Pakpour AH. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum Vaccin Immunother. 2022;18(1):e1993689. doi:10.1080/21645515.2021.1993689.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;13(9):698111. doi:10.3389/fpubh.2021.698111. PMID: 34485229; PMCID: PMC8414566.
- Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, Al-Haidar A, Yaseen A, Ababneh NA, Assaf A, et al. A. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. doi:10.3390/ijerph18052407. PMID: 33804558; PMCID: PMC7967761.
- Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;23(9):636. doi:10.12688/f1000research.24457.1. PMID: 33093946; PMCID: PMC7549174.
- Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. 2021;18(5):2470. doi:10.3390/ijerph18052470. PMID: 33802278; PMCID: PMC7967607.
- Lindert J, Jakubauskiene M, Bilsen J. The COVID-19 disaster and mental health-assessing, responding and recovering. Eur J Public Health. 2021;31(Suppl 4):iv31–35. doi:10.1093/eurpub/ckab153. PMID: 34751367; PMCID: PMC8576295.
- Witteveen D, Velthorst E. Economic hardship and mental health complaints during COVID-19. Proc Natl Acad Sci U S A. 2020 3; 117(44):27277–84. doi: 10.1073/pnas.2009609117. PMID: 33046648; PMCID: PMC7959574.
- Kong KL, Chu S, Giles ML. Factors influencing the uptake of influenza vaccine vary among different groups in the hard-to-reach population. Aust N Z J Public Health. 2020;44(2):163–68. doi:10.1111/1753-6405.12964. Epub 2020 Feb 26. PMID: 32101355.
- Pacella-LaBarbara ML, Park YL, Patterson PD, Doshi A, Guyette MK, Wong AH, Chang BP, Suffoletto BP. COVID-19 vaccine uptake and intent among emergency healthcare workers: a cross-sectional survey. J Occup Environ Med. 2021;63(10):852–56. doi:10.1097/JOM.0000000000002298. PMID: 34138823; PMCID: PMC8478093.
- Diaz P, Reddy P, Ramasahayam R, Kuchakulla M, Ramasamy R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following emergency use authorization. Andrologia. 2021 Oct;53(9):e14156. doi:10.1111/and.14156.
- Hsu AL, Johnson T, Phillips L, Nelson TB. Sources of vaccine hesitancy: pregnancy, infertility, minority concerns, and general skepticism. Open Forum Infect Dis. 2021 Aug 18;9(3):ofab433. doi:10.1093/ofid/ofab433
- Botwe BO, Antwi WK, Adusei JA, Mayeden RN, Akudjedu TN, Sule SD. COVID-19 vaccine hesitancy concerns: findings from a Ghana clinical radiography workforce survey. Radiography (Lond). 2022 May;28(2):537–44. doi:10.1016/j.radi.2021.09.015.
- Kotecha IS, Vasavada DA, Kumar P, Nerli LM, Tiwari DS, Parmar DV. Knowledge, attitude, and belief of health-care workers toward COVID-19 vaccine at a tertiary care center in India. Asian Journal of Social Health and Behavior. 2022;5:63–67. doi:10.4103/shb.shb_20_21.
- Kukreti S, Lu MY, Lin YH, Strong C, Lin CY, Ko NY, Chen PL, Ko WC. Willingness of Taiwan’s healthcare workers and outpatients to vaccinate against COVID-19 during a period without community outbreaks. Vaccines (Basel). 2021 Mar 12;9(3):246. doi:10.3390/vaccines9030246
- Leigh JP, Moss SJ, White TM, Picchio CA, Rabin KH, Ratzan SC, Wyka K, El-Mohandes A, Lazarus JV. Factors affecting COVID-19 vaccine hesitancy among healthcare providers in 23 countries. Vaccine. 2022;40(31):4081–89. doi:10.1016/j.vaccine.2022.04.097.
- Al-Ashwal FY, Kubas M, Zawiah M, Bitar AN, Mukred Saeed R, Sulaiman SAS, Khan AH, Ghadzi SMS. Healthcare workers’ knowledge, preparedness, counselling practices, and perceived barriers to confront COVID-19: a cross-sectional study from a war-torn country, Yemen. PLoS One. 2020;15(12):e0243962. doi:10.1371/journal.pone.0243962.
- Hudson A, Montelpare WJ. Predictors of vaccine hesitancy: implications for COVID-19 public health messaging. Int J Environ Res Public Health. 2021;18(15):8054. doi:10.3390/ijerph18158054.
- James EK, Bokemper SE, Gerber AS, Omer SB, Huber GA. Persuasive messaging to increase COVID-19 vaccine uptake intentions. Vaccine. 2021;39(49):7158–65. doi:10.1016/j.vaccine.2021.10.039. PMID: 34774363; PMCID: PMC8531257.