ABSTRACT
A substantial burden of high-risk human papillomavirus (HPV) infections and HPV-related cancers can be mitigated by vaccination. The current study aimed to investigate the willingness of female students at the University of Kuwait to get HPV vaccination and its possible association with general vaccine conspiracy beliefs (VCBs). This cross-sectional survey study was conducted during September–November 2022 using a validated VCB scale as the survey instrument. The final sample comprised 611 respondents with a median age of 22 y and a majority of Arab ethnicity (n = 600, 98.2%). Only 360 respondents (56.9%) heard of HPV before participation and these students showed an above-average level of HPV knowledge (mean knowledge score of 12.7 ± 2.6 out of 16 as the maximum score), of whom only 33 self-reported HPV vaccine uptake (9.2%). The willingness to accept free-of-charge HPV vaccination was seen among 69.8% of the participants, with 20.1% who were hesitant and 10.1% who were resistant. The acceptance of HPV vaccination if payment is required was 23.1%. Reasons for HPV vaccine hesitancy/resistance included complacency to the HPV disease risks, lack of confidence in HPV vaccination, and inconvenience. The embrace of VCBs was associated with significantly higher odds of HPV vaccine hesitancy/resistance. The current study showed the detrimental impact of endorsing vaccine conspiracy beliefs manifested in lower intention to get HPV vaccination among female university students in Kuwait. This should be considered in vaccine promotion efforts aiming to reduce the burden of HPV cancers.
Introduction
The morbidity and mortality from human papillomavirus (HPV)-related cancers remain substantial worldwide.Citation1 In particular, infection by high-risk HPV types (e.g., HPV-16, HPV-18, among others) is associated with cervical, oropharyngeal, and anogenital cancers.Citation2–4 Additionally, HPV is considered the most common causative agent of sexually transmitted infections (STIs).Citation1 A major problem of HPV infection is the large fraction of asymptomatic cases that remain unrecognized sustaining the forward transmission of the virus.Citation5,Citation6
The tropism of HPV is in the squamous epithelium of mucous membranes, including the cervix.Citation7 The main documented route of HPV transmission is sexual practices, although non-sexual routes of transmission have also been reported.Citation8,Citation9 The molecular basis of HPV carcinogenesis is well described, with the integration of viral DNA into the host genome, leading to genomic instability, subsequently favoring transforming genetic events and progression to malignancy.Citation10 Strategies to prevent HPV-related cancers include vaccination against high-risk types and screening programs for early detection and treatment of precancerous lesions.Citation11
Vaccination for girls represents an evidence-based, cost-effective intervention measure to reduce the burden of HPV-related cervical cancer (CC) as advocated by the World Health Organization (WHO).Citation12 If the WHO 90–70–90 targets (90% fully vaccinated girls by age 15 y, 70% of females undergoing CC screening by high-performance test at 35 and 45 y of age, and treatment for 90% of women identified with cervical disease) are achieved by the year 2030, this strategy would prevent more than 62 million CC-related deaths by the year 2120.Citation12,Citation13
So far, three vaccine types have been approved to prevent infection by HPV types commonly implicated in CC.Citation14 Currently, HPV vaccination is recommended for girls at 11 y through to 26 y given as a two-dose vaccine, with lower benefits among older females as a result of the higher chance of HPV exposure that comes with advancing in age.Citation15,Citation16 The current evidence points to high safety and efficacy profiles of the currently approved HPV vaccines, despite the need for further comprehensive long-term studies.Citation17–19
In Kuwait, among other Middle Eastern countries, the burden of HPV-related disease is relatively low.Citation20,Citation21 This can explain the low perceived risk of HPV-related disease in the region.Citation22 Complacency toward the disease partly explains the low intentions to get vaccinated, which was previously shown in the context of HPV vaccination.Citation22–24 However, there is sufficient evidence indicating that the burden of HPV-related cancers represents a public health issue warranting intervention.Citation25
The challenges to the efforts aiming to reduce the burden of HPV-related disease in the Middle East include a lack of awareness, low HPV vaccine uptake, and unwillingness to get vaccinated.Citation22,Citation24,Citation26–29 These issues were manifested in earlier studies in the Middle East, where the discussion of STIs can be viewed as a taboo subject.Citation30,Citation31 An additional issue impeding HPV vaccination in Middle Eastern countries is the affordability of the vaccine in terms of cost. Even in Kuwait, a high-income country, the vaccine is not part of the routine immunization program and the two-dose HPV vaccine costs about 150 Kuwaiti dinars (KWD, about 490 US dollars).Citation25,Citation32 Thus, unwillingness to pay for the vaccine can be a major constraint driving HPV vaccination hesitancy/resistance.Citation22,Citation33 Furthermore, an issue that came to light following the coronavirus disease 2019 (COVID-19) pandemic, is the embrace of conspiratorial ideas regarding vaccination which was widely prevalent in the Middle East, even among educated study groups (e.g., health professionals).Citation34–36 Misinformation as the main driving factor behind the negative attitude to vaccination was recently shown in the context of HPV vaccination.Citation37
Therefore, the current study aimed to evaluate the willingness of female university students in Kuwait to get HPV vaccination. Additionally, the study objectives included the evaluation of the factors associated with hesitancy/resistance to get HPV vaccination. Moreover, the study intended to evaluate the overall embrace of vaccine conspiracy beliefs among female students at various colleges studying at Kuwait University.
Methods
Study design
The current online survey study was based on a cross-sectional design to survey female students enrolled at Kuwait University (KU), which is the oldest and the largest public university in the country with more than 38,000 students enrolled in 16 different colleges.Citation38 The survey instrument was based on the previously published validated tools including the vaccine conspiracy belief scale (VCBS) validated by Shapiro et al.Citation22,Citation26,Citation27,Citation39 The survey tool was uploaded into Google Forms in both Arabic and English languages simultaneously. Then, survey distribution was based on the snowball convenience-based approach starting from the first author and her contacts asking for further distribution of the survey link via the following social media and instant messaging services: Facebook, Twitter, Instagram, LinkedIn, Messenger, and WhatsApp. Participation was voluntary, and anonymous and no incentives were offered to the potential participants.
Survey instrument
The survey instrument was briefly divided into six sections as follows: First, an introductory section with a mandatory e-consent item. Second, the sociodemographic information section inquired about age, nationality, ethnicity, current educational level, college, and monthly income of the household. Third, a section on HPV knowledge started with an introductory question “Have you heard of HPV prior to this survey?,” with “yes” or “no” as possible responses. For those who answered “no,” the survey was directed to the VCBS section. For the students who answered “yes,” eight HPV knowledge questions adopted from a previous study followed, with yes, no, and I do not know as the possible responses.Citation22 The eight items formed the HPV knowledge score (HPV K-score) based on the following scoring: for correct responses a score of 2 was given, while I do not know and incorrect responses were given the scores of 1 and zero, respectively, yielding a range for HPV K-score of zero–16. Fourth, a section assessing the intention to get HPV vaccination, the previous history of HPV vaccine uptake and sources of information about HPV followed. The exact phrasing of the item assessing the intention to get HPV vaccination was “Are you willing to get HPV vaccine if provided for free?,” with yes vs. maybe vs. no as the possible responses. The students who answered “yes” comprised the HPV vaccine acceptance group, while those who answered “maybe” and “no” comprised the vaccine hesitant and vaccine-resistant groups, respectively. Finally, the vaccine conspiracy beliefs were assessed using seven items on a 7-point Likert scale (strongly disagree, disagree, somewhat disagree, neutral, somewhat agree, agree, and strongly agree).Citation39 Higher VCBS scores indicated a higher embrace of vaccine conspiracies.Citation22,Citation34,Citation39 To rule out careless responses, an attention question was asked by the end of the survey, where the participants were asked to write down a number shown in an attached figure. The complete survey instrument is provided in (Supplementary File 1).
Ethical approval
The current study was approved by the Health Sciences Center Ethical Committee at Kuwait University (reference number: VDR/EC-4016, granted on 27 April 2022). Electronic informed consent was obtained from all participants, which was mandatory for the completion of the survey.
Statistical analysis
Statistical analysis was conducted using IBM SPSS Statistics for Windows (Version 26.0, IBM Corp). Descriptive statistics included the measurements of mean, median, standard deviation (SD) and interquartile range (IQR). Normality of distribution for scale variables (HPV K-score, VCBS), was assessed using Kolmogorov–Smirnov normality test (K–S). Univariate analyses were conducted based on the chi-squared (χ2), Mann–Whitney U (M–W), and Kruskal–Wallis (K–W) tests. Logistic regression multivariate analyses were done to evaluate the associations between different study variables as follows: Age was dichotomized into two categories based on the median age in the study sample, which was 22 y. The HPV K-score was dichotomized based on the mean value of the participants who have heard of HPV prior to the study into two categories: HPV K-score ≤12 (lower HPV knowledge) vs. HPV K-score >12 (higher HPV knowledge). The VCBS score was dichotomized into two categories based on the mean VCBS in the whole study sample: VCBS <28 indicating a lower embrace of vaccine conspiracies vs. VCBS ≥28 indicating higher embrace of vaccine conspiracies. The level of statistical significance was considered for p < .050.
Results
A total of 652 responses were retrieved during 18 September 2022–9 November 2022. The number of respondents who did not agree to participate in the study was 33 (5.1%), with an additional eight responses that were excluded as careless responses based on incorrect responses to the attention item (1.2%). Thus, the final study sample comprised a total of 611 respondents (93.7%).
Study sample characteristics
The final study sample consisted of 611 respondents. A summary of the study sample characteristics is shown in ().
Table 1. Study sample characteristics (N = 611).
The respondents belonged to 15 different colleges with the highest number affiliated with the College of Engineering and Petroleum (n = 94, 15.4%), Medicine (n = 87, 14.2%), Education (n = 67, 11.0%), Pharmacy (n = 61, 10.0%), Allied Health Sciences (n = 56, 9.2%), Science (n = 42, 6.9%), Social Sciences (n = 39, 6.4%), Law (n = 33, 5.4%), Arts (n = 32, 5.2%), Business Administration (n = 31, 5.1%), Life Sciences (n = 23, 3.8%), Public Health (n = 14, 2.3%), Architecture (n = 12, 2.0%), Dentistry (n = 10, 1.6%), and Sharia and Islamic Studies (n = 10, 1.6%).
Knowledge of HPV prior to participation
In the whole study sample, only 55.3% of the respondents indicated that they have heard of HPV prior to participation (n = 338). Older age, postgraduate education, affiliation with health colleges, and higher monthly income were significantly associated with a higher percentage of knowledge of HPV prior to participation ().
Table 2. Association between study variables and knowledge of HPV prior to participation.
HPV knowledge among the respondents who have heard of the virus before participation
The overall level of HPV knowledge among the participants who have heard of HPV prior to the study was non-normally distributed (p < .001, K–S), with moderate skewness of −0.531 indicating a relatively high level of HPV knowledge ().
Figure 1. Human papillomavirus (HPV) knowledge among the participants who have heard of HPV prior to the study.
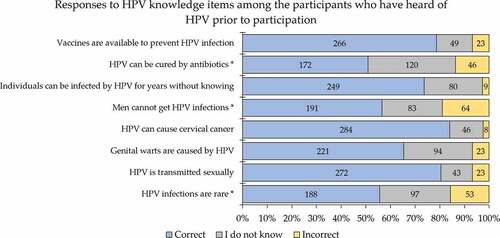
Per item, correct responses ranged from 50.9% to 84.0%, with correct knowledge that vaccination is available to prevent HPV infection observed among 78.7% of the participants who heard of HPV prior to participation ().
Figure 2. Human papillomavirus (HPV) knowledge per item among the participants who have heard of HPV prior to the study.
By dividing the HPV-K score into two categories (lower for HPV K-scores ≤12 and higher for HPV K-scores >12), better HPV knowledge was seen among students in health colleges followed by students in scientific colleges and students in humanities colleges ().
Table 3. HPV knowledge association with study variables.
History of HPV vaccine uptake among the study participants
Among the students who have heard of HPV prior to participation, only 30 indicated the previous uptake of HPV vaccination (8.9%). Higher vaccine uptake was associated with older age (11.5% among those aged 22 y or older vs. 4.2% among the students younger than 22 y, ).
Table 4. History of human papillomavirus (HPV) vaccine uptake among participants who have heard of HPV prior to participation.
The intention to get HPV vaccination if provided freely and if payment is needed
The overall willingness to accept HPV vaccination if provided freely was expressed by 236 participants who have heard of HPV prior to participation (69.8%), with 68 participants who were hesitant (20.1%) and 34 participants who were resistant (10.1%). The acceptance for HPV vaccination was associated with older age, postgraduate educational level, and affiliation with health colleges ()
Table 5. The intention to get human papillomavirus (HPV) vaccination if provided freely and if payment is required divided by different study variables.
The willingness to pay for the vaccine was reported only by 78 participants (23.1%), compared to 134 who were hesitant (39.6%) and 126 participants who were resistant to pay for the vaccine (37.3%). Willingness to pay for HPV vaccination was associated with a higher monthly income of the household ().
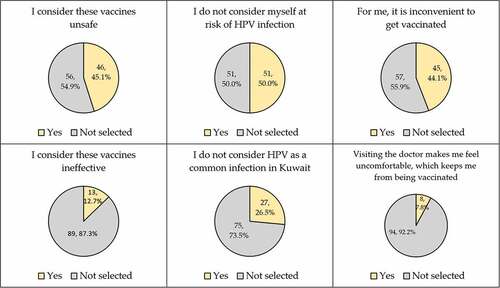
The reasons for HPV vaccine hesitancy/resistance were mostly linked to the complacency and lack of confidence items followed by the constraints’ items ().
The embrace of vaccine conspiracy beliefs among the participating students
The mean value for VCBS in the whole study sample was 28.2 ± 11.7 (median: 28.0, IQR: 18.0–38.0). Higher VCBS was seen among students younger than 22 y (mean VCBS: 29.3 ± 11.1 vs. 27.3 ± 12.0, p = .027, M–W), undergraduate students (mean VCBS: 28.7 ± 11.4 vs. 26.2 ± 12.5, p = .032, M–W), students affiliated to humanities’ colleges compared to those affiliated to scientific and health schools, respectively (mean VCBS: 33.4 ± 10.6 vs. 29.5 ± 10.5 vs. 22.4 ± 10.8, p < .001, K–W), lower monthly income (mean VCBS: 30.2 ± 11.4 vs. 27.1 ± 11.7,p = .001, M–W), and among participants who did not hear of HPV prior to participation (mean VCBS: 31.5 ± 10.1 vs. 25.5 ± 12.2, p < .001, M–W), while nationality, and ethnicity did not show statistically significant differences.
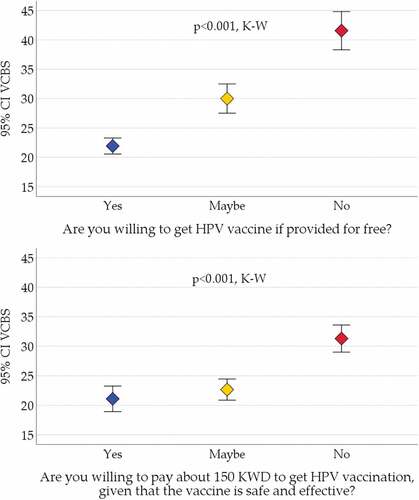
Higher VCBS was also noticed among the participants who were resistant to HPV vaccination (unwilling to get free HPV vaccination and unwilling to pay for HPV vaccination) compared to hesitancy and acceptance groups (p < .001 for the two comparisons, K–W, ).
Figure 4. The association between acceptance of HPV vaccination and vaccine conspiracy beliefs.
Multivariate analysis for the factors associated with higher HPV vaccine acceptance
Multivariate analysis using multinomial logistic regression with age, educational level and college as the covariates revealed that the embrace of conspiracy beliefs was significantly correlated with HPV vaccine resistance and hesitancy (), while higher level of HPV knowledge and postgraduate education were associated with vaccine acceptance compared to the hesitancy group ().
Table 6. Multinomial logistic regression analysis for the possible factors associated with HPV vaccine acceptance compared to vaccine hesitancy and resistance.
Sources of HPV information
The most common source of HPV information as reported by the participants who have heard of HPV prior to participation was university courses (n = 149, 44.1%), followed by social media platforms (n = 137, 40.5%), and internet websites (n = 131, 38.8%). The source of HPV information was linked with HPV vaccine acceptance, with the highest acceptance level seen among those who depended on university courses (78.5%), followed by those who depended on healthcare providers’ information (77.7%), while the lowest percentage of HPV vaccine acceptance was seen among those who depended on television/radio/newspapers (54.5%), internet websites (58.0%), and social media platforms (67.2%, ).
Figure 5. The sources of information regarding HPV as reported by the participants who have heard of HPV prior to participation.
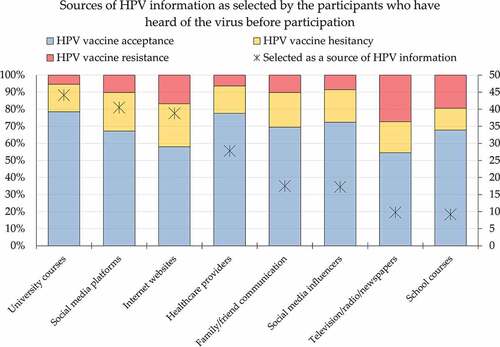
The reliance on university courses as a source of HPV information was associated with higher intention to get HPV vaccination (117/149 (78.5%) vs. 119/189 (63.0%), p = .002, χ2 test). On the contrary, the following were associated with lower intention to get HPV vaccination: the dependence on internet websites (76/131 (58.0%) vs. 160/207 (77.3%), p < .001, χ2 test), and the dependence on television/radio/newspapers (18/33 (54.5%) vs. 218/305 (71.5%), p = .044, χ2 test).
Discussion
The main findings of the current study indicated the detrimental effect of endorsing vaccine conspiracy beliefs which were manifested in HPV vaccine hesitancy/resistance among female university students in Kuwait. Additionally, the results of the current study revealed a very low percentage of HPV vaccine uptake among university students in the Middle Eastern country, as self-reported by the participants.
The current study demonstrated a history of HPV vaccine uptake at a level of 9% among female university students studying at the largest public university in the country, and who knew about the virus before participation.Citation38 The very low level of HPV vaccine coverage resonates with the results of previous studies that were conducted in the Middle East.Citation22,Citation40–42 For example, a recent study that was conducted in Kuwait among female school teachers demonstrated that only 26 participants were vaccinated against HPV representing 16% of the participants who were aware of HPV vaccine availability.Citation29 The self-reported history of HPV vaccine uptake was also very low at a level of 4% in a recent study among female university students studying at health schools in Jordan.Citation22 A recent study among medical students in Lebanon showed a vaccination rate of 16%, with an alarmingly low level of HPV knowledge.Citation43 Possible explanation for the very low coverage of HPV vaccination in this study among other studies from the Middle East is the conservative culture and low level of recommendation by health professionals besides the unawareness regarding vaccine availability.Citation42,Citation44–46
Another important finding was the low level of awareness regarding HPV. Specifically, 45% of the participants have not heard of HPV before participation. Additionally, variable gaps in HPV knowledge were found among the participants who have heard of HPV before participation including aspects related to disease treatment, HPV infection occurrence among males, the possibility of asymptomatic HPV infections, and awareness regarding vaccine availability. Consistent with our findings, several recent studies suggested unawareness regarding several aspects of HPV-related disease in the Middle East region.Citation22,Citation26–28,Citation47
Considering the sexual transmission of high-risk HPV types that are associated with cervical among other genital and oropharyngeal cancers, coupled with cultural and religious barriers prevailing in the Middle East, the preventive efforts aiming to reduce the burden of HPV-related cancers can be challenging in the region.Citation48,Citation49 The socio-cultural and religious issues should be meticulously considered for the successful implementation of HPV vaccination in the region similar to other world regions.Citation49,Citation50
Another important finding of the current study is the relatively considerable percentage of participants who were either hesitant (20%) or resistant (10%) to HPV vaccination if provided free-of-charge. The intention to get HPV vaccination dropped from about 70% for free vaccination to only 23% if payment for the vaccine was required. This can be a major barrier to the successful implementation of HPV vaccination in Kuwait considering the cost of the vaccine. Similarly, a recent study among female university students in Jordan highlighted the issue of vaccine affordability in the decision to get vaccinated.Citation22 Understandably, a higher willingness to pay for the vaccine was observed among participants with a higher monthly income. A recent systematic review from the Middle East showed that HPV vaccine acceptance would be high if the cost issues could be rectified.Citation51
The role of sociodemographic variables should be considered in the strategic planning of vaccine implementation, which was shown in univariate analysis in this study where older age and postgraduate education were associated with higher intention to get vaccinated against HPV. The role of sociodemographic factors as determinants of willingness to get vaccinated has been demonstrated previously regarding HPV vaccination among other vaccines.Citation22,Citation34,Citation52,Citation53
The intention to get HPV vaccination was reported at variable rates in different countries and depending on the population of interest. For example, a recent study among young Greek adults showed a rate of willingness to get HPV vaccination of 66%, with vaccine coverage of 52%.Citation54 On the other hand, a recent study that was conducted in 2022 among female university students in China showed much higher rate of intention to get HPV vaccination (90%).Citation52 Another recent study among male medical students in Saudi Arabia showed an acceptance rate of 49% for HPV vaccination.Citation47 The acceptance of HPV vaccination was much higher among adult women in the United Arab Emirates (UAE) at 80%.Citation55
The issues cited by the participants who were hesitant/resistant to HPV vaccination in this study included the relatively high level of complacency toward HPV-related disease. In the Arab countries of the Middle East, a notion is present among the general public that views STIs as an uncommon issue. This view lacks credible evidence due to the primitive nature of research addressing STIs in the region.Citation56 Recent studies have shown the relevance of conducting STI research in the region, and in the context of HPV for example, recent studies from Kuwait demonstrated the circulation of high-risk HPV types not covered in the bivalent HPV vaccine highlighting the role of epidemiologic domestic studies to guide a successful immunization campaign.Citation57,Citation58
Besides complacency toward the disease, the lack of confidence particularly in relation to HPV vaccine safety was reported by the hesitant/resistant participants in this study. This was also demonstrated in the previous Jordanian study, and it emphasizes the value of demonstrating the safety of the vaccine and its health benefits in the prevention of CC development.Citation22,Citation59 The issue of perceived susceptibility in relation to HPV vaccine uptake rates has been highlighted in a systematic review involving studies from the United States, Australia, and China.Citation60 Stressing on vaccine safety and recommendation by health providers were shown to enhance HPV vaccine acceptability in the UAE study.Citation55
A major finding of the current study was the significant correlation between the embrace of vaccine conspiracies and HPV vaccine hesitancy/resistance. Supporting this finding and highlighting the negative impact of conspiracies on health behavior, recent studies in the context of different vaccines have shown the prominence of this issue. For example, a previous study conducted among the general Arab public (mainly in Jordan and Kuwait) has shown a very high level of coronavirus disease 2019 (COVID-19) vaccine hesitancy correlated with vaccine hesitancy.Citation34 Similarly, a recent study among health professionals in Kuwait showed a similar finding.Citation35 Of note, vaccine conspiracies were significantly associated with lower uptake of influenza vaccine among healthcare workers in Jordan.Citation61 In the context of HPV vaccination, and consistent with our findings, a recent study among female university students in Jordan showed that the endorsement of vaccine conspiracy beliefs was associated with higher odds of HPV vaccine rejection.Citation22
Since the source of information regarding HPV was linked with the intentions to get vaccinated against HPV, health education particularly through university courses appears of high importance.Citation22 This was reflected in our results where lower HPV knowledge was associated with HPV vaccination hesitancy. This issue is of particular relevance for the students in the humanities colleges where the students are less likely to be exposed to health education and this was manifested in lower HPV knowledge among this group in the current study. Additionally, the reliance on internet websites was linked with lower intentions to get HPV vaccination highlighting the role of sources of information on the decision to get vaccinated.
The current study suffered from inevitable limitations including the cross-sectional design which should be considered in the interpretation of the results since vaccine hesitancy/rejection is a time- and context-specific phenomenon.Citation62 Additionally, the history of HPV vaccine uptake was self-reported with the absence of evidence of getting the vaccine among the participants. Furthermore, the current study albeit involving students in the largest public university in Kuwait, might not be totally representative of female university students in the country. Finally, convenience sampling provides the advantage of expedited results; however, this sampling method is prone to suffer from the issue of selection bias.
To conclude, our findings demonstrated the potential harmful impact of vaccine conspiracies that were linked with HPV vaccine hesitancy/rejection among female university students in Kuwait. Issue to be considered in the vaccine promotion efforts include (1) improving the level of HPV awareness and knowledge which can reduce the complacency to the disease risks: (2) the provision of introducing HPV vaccination free-of-charge as demonstrated by the disparity between vaccine acceptance rates for free vaccination compared to willingness to pay for the vaccine; (3) efforts should be made to lower the constraints of vaccination to make it aconvenient experience; (4) the focus on vaccine safety and efficacy besides the potential benefits of the vaccine should be highlighted to emphasize the vaccine role in cancer prevention; and (5) importantly, addressing the issues of vaccine conspiracies which appear widely prevalent in the Middle East, and stressing on accurate delivery of information regarding vaccination through reliable sources.
Author contributions
Conceptualization: Mariam Alsanafi and Malik Sallam
Methodology: Mariam Alsanafi, Nesreen A. Salim, and Malik Sallam
Software: Malik Sallam
Validation: Mariam Alsanafi, Nesreen A. Salim, and Malik Sallam
Formal analysis: Malik Sallam
Investigation: Mariam Alsanafi, Nesreen A. Salim, and Malik Sallam
Resources: Malik Sallam
Data Curation: Mariam Alsanafi, Nesreen A. Salim, and Malik Sallam
Writing – Original Draft: Malik Sallam
Writing – Review & Editing: Mariam Alsanafi, Nesreen A. Salim, and Malik Sallam
Visualization: Malik Sallam
Supervision: Malik Sallam
Project administration: Mariam Alsanafi and Malik Sallam
Supplementary Material
Download PDF (782 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available on request from the corresponding author (Malik Sallam).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2194772
Additional information
Funding
References
- Kombe Kombe AJ, Li B, Zahid A, Mengist HM, Bounda GA, Zhou Y, Jin T. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Public Health. 2020;8:552028. doi:10.3389/fpubh.2020.552028.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: gLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–10. doi:10.3322/caac.21660.
- Zhao M, Wu Q, Hao Y, Hu J, Gao Y, Zhou S, Han L. Global, regional, and national burden of cervical cancer for 195 countries and territories, 2007–2017: findings from the global burden of disease study 2017. BMC Womens Health. 2021;21:419. doi:10.1186/s12905-021-01571-3.
- Boda D, Docea AO, Calina D, Ilie MA, Caruntu C, Zurac S, Neagu M, Constantin C, Branisteanu D, Voiculescu V, et al. Human papilloma virus: apprehending the link with carcinogenesis and unveiling new research avenues (Review). Int J Oncol. 2018;52:637–55. doi:10.3892/ijo.2018.4256.
- Gravitt PE, Winer RL. Natural history of HPV infection across the lifespan: role of Viral Latency. Viruses. 2017;9:267. doi:10.3390/v9100267.
- Christensen ND. HPV disease transmission protection and control. Microb Cell. 2016;3:476–90. doi:10.15698/mic2016.09.530.
- Egawa N, Egawa K, Griffin H, Doorbar J. Human papillomaviruses; epithelial tropisms, and the development of Neoplasia. Viruses. 2015;7:3863–90. doi:10.3390/v7072802.
- Petca A, Borislavschi A, Zvanca ME, Petca RC, Sandru F, Dumitrascu MC. Non-sexual HPV transmission and role of vaccination for a better future (review). Exp Ther Med. 2020;20:186. doi:10.3892/etm.2020.9316.
- Panatto D, Amicizia D, Trucchi C, Casabona F, Lai PL, Bonanni P, Boccalini S, Bechini A, Tiscione E, Zotti CM, et al. Sexual behaviour and risk factors for the acquisition of human papillomavirus infections in young people in Italy: suggestions for future vaccination policies. BMC Public Health. 2012;12:623. doi:10.1186/1471-2458-12-623.
- Lehoux M, D’abramo CM, Archambault J. Molecular mechanisms of human papillomavirus-induced carcinogenesis. Public Health Genomics. 2009;12:268–80. doi:10.1159/000214918.
- Chan CK, Aimagambetova G, Ukybassova T, Kongrtay K, Azizan A. Human papillomavirus infection and cervical cancer: epidemiology, screening, and vaccination-review of current perspectives. J Oncol. 2019;2019:3257939. doi:10.1155/2019/3257939.
- World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. [accessed 2023 Feb 9]. https://www.who.int/publications/i/item/9789240014107.
- Canfell K, Kim JJ, Brisson M, Keane A, Simms KT, Caruana M, Burger EA, Martin D, Nguyen DTN, Bénard É, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395:591–603. doi:10.1016/s0140-6736(20)30157-4.
- Wang R, Pan W, Jin L, Huang W, Li Y, Wu D, Gao C, Ma D, Liao S. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 2020;471:88–102. doi:10.1016/j.canlet.2019.11.039.
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68:698–702. doi:10.15585/mmwr.mm6832a3.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405–8. doi:10.15585/mmwr.mm6549a5.
- Soliman M, Oredein O, Dass CR. Update on safety and efficacy of HPV vaccines: focus on gardasil. Int J Mol Cell Med. 2021;10:101–13. doi:10.22088/ijmcm.Bums.10.2.101.
- Arbyn M, Xu L. Efficacy and safety of prophylactic HPV vaccines. A Cochrane review of randomized trials. Expert Rev Vaccines. 2018;17:1085–91. doi:10.1080/14760584.2018.1548282.
- Porras C, Tsang SH, Herrero R, Guillén D, Darragh TM, Stoler MH, Hildesheim A, Wagner S, Boland J, Lowy DR, et al. Efficacy of the bivalent HPV vaccine against HPV 16/18-associated precancer: long-term follow-up results from the Costa Rica vaccine trial. Lancet Oncol. 2020;21:1643–52. doi:10.1016/s1470-2045(20)30524-6.
- Al-Awadhi R, Chehadeh W, Kapila K. Prevalence of human papillomavirus among women with normal cervical cytology in Kuwait. J Med Virol. 2011;83:453–60. doi:10.1002/jmv.21981.
- Al-Awadhi R, Chehadeh W, Jaragh M, Al-Shaheen A, Sharma P, Kapila K. Distribution of human papillomavirus among women with abnormal cervical cytology in Kuwait. Diagn Cytopathol. 2013;41:107–14. doi:10.1002/dc.21778.
- Sallam M, Al-Mahzoum K, Eid H, Assaf AM, Abdaljaleel M, Al-Abbadi M, Mahafzah A. Attitude towards HPV vaccination and the intention to get vaccinated among female university students in health schools in Jordan. Vaccines (Basel). 2021;9:1432. doi:10.3390/vaccines9121432.
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–9. doi:10.1016/j.vaccine.2014.01.081.
- Bencherit D, Kidar R, Otmani S, Sallam M, Samara K, Barqawi HJ, Lounis M. Knowledge and awareness of Algerian students about cervical cancer, HPV and HPV vaccines: a cross-sectional study. Vaccines (Basel). 2022;10:1420. doi:10.3390/vaccines10091420.
- Fernandes Q, Allouch S, Gupta I, Elmakaty I, Elzawawi KE, Amarah A, Al-Thawadi H, Al-Farsi H, Vranic S, Al Moustafa A-E. Human papillomaviruses-related cancers: an update on the presence and prevention strategies in the Middle East and North African regions. Pathogens. 2022;11:1380. doi:10.3390/pathogens11111380.
- Sallam M, Al-Fraihat E, Dababseh D, Yaseen A, Taim D, Zabadi S, Hamdan AA, Hassona Y, Mahafzah A, Şahin GÖ. Dental students’ awareness and attitudes toward HPV-related oral cancer: a cross sectional study at the university of Jordan. BMC Oral Health. 2019;19:171. doi:10.1186/s12903-019-0864-8.
- Sallam M, Dababseh D, Yaseen A, Al-Haidar A, Ettarras H, Jaafreh D, Hasan H, Al‐salahat K, Al‐fraihat E, Hassona Y, et al. Lack of knowledge regarding HPV and its relation to oropharyngeal cancer among medical students. Cancer Rep (Hoboken). 2022;5:e1517. doi:10.1002/cnr2.1517.
- Alsous MM, Ali AA, Al-Azzam SI, Abdel Jalil MH, Al-Obaidi HJ, Al-Abbadi EI, Hussain ZK, Jirjees FJ. Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities. Sci Rep. 2021;11:786. doi:10.1038/s41598-020-80834-9.
- Rezqalla J, Alshatti M, Ibraheem A, Omar D, Houda AF, AlHaqqan S, AlGhurair S, Akhtar S. Human papillomavirus (HPV): unawareness of the causal role of HPV infection in cervical cancer, HPV vaccine availability, and HPV vaccine uptake among female school teachers in a Middle Eastern country. J Infect Public Health. 2021;14:661–7. doi:10.1016/j.jiph.2021.01.015.
- Albanghali MA, Othman BA. A cross-sectional study on the knowledge of sexually transmitted diseases among young adults living in Al Bahah, Saudi Arabia. Int J Environ Res Public Health. 2020;17:1872. doi:10.3390/ijerph17061872.
- Horanieh N, Macdowall W, Wellings K. How should school-based sex education be provided for adolescents in Saudi Arabia? Views of stakeholders. Sex Educ. 2021;21:645–59. doi:10.1080/14681811.2020.1843424.
- Bruni L, Albero G, Serrano B, Mena M, Collado J, Gómez D, Muñoz, J, Bosch, F, de Sanjosé, S. Human Papillomavirus and Related Diseases in Kuwait. Summary Report. [accessed 2023 Feb 9]. https://hpvcentre.net/statistics/reports/KWT.pdf.
- Milondzo T, Meyer JC, Dochez C, Burnett RJ. Human papillomavirus vaccine hesitancy highly evident among caregivers of girls attending South African private schools. Vaccines (Basel). 2022;10:503. doi:10.3390/vaccines10040503.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines (Basel). 2021;9:42. doi:10.3390/vaccines9010042.
- Al-Sanafi M, Sallam M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: a cross-sectional study using the 5C and vaccine conspiracy beliefs scales. Vaccines (Basel). 2021;9:701. doi:10.3390/vaccines9070701.
- Alsanafi M, Al-Mahzoum K, Sallam M. Monkeypox knowledge and confidence in diagnosis and management with evaluation of emerging virus infection conspiracies among health professionals in Kuwait. Pathogens. 2022;11:994. doi:10.3390/pathogens11090994.
- Milondzo T, Meyer JC, Dochez C, Burnett RJ. Misinformation drives low human papillomavirus vaccination coverage in South African girls attending private schools. Front Public Health. 2021;9:598625. doi:10.3389/fpubh.2021.598625.
- Kuwait University. About Kuwait University. [accessed 2023 Feb 9]. http://kuweb.ku.edu.kw/ku/ar/AboutUniversity/AboutKU/AboutUSKU/index.htm.
- Shapiro GK, Holding A, Perez S, Amsel R, Rosberger Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016;2:167–72. doi:10.1016/j.pvr.2016.09.001.
- Dany M, Chidiac A, Nassar AH. Human papillomavirus vaccination: assessing knowledge, attitudes, and intentions of college female students in Lebanon, a developing country. Vaccine. 2015;33:1001–7. doi:10.1016/j.vaccine.2015.01.009.
- Abou El-Ola MJ, Rajab MA, Abdallah DI, Fawaz IA, Awad LS, Tamim HM, Ibrahim A, Mugharbil A, Moghnieh R. Low rate of human papillomavirus vaccination among schoolgirls in Lebanon: barriers to vaccination with a focus on mothers’ knowledge about available vaccines. Ther Clin Risk Manag. 2018;14:617–26. doi:10.2147/tcrm.S152737.
- Al Shdefat S, Al Awar S, Osman N, Khair H, Sallam G, Maki S. Identification level of awareness and knowledge of Emirati men about HPV. J Healthc Eng. 2022;2022:5340064. doi:10.1155/2022/5340064.
- Haddad SF, Kerbage A, Eid R, Kourie HR. Awareness about the human papillomavirus (HPV) and HPV vaccine among medical students in Lebanon. J Med Virol. 2022;94:2796–801. doi:10.1002/jmv.27509.
- Abi Jaoude J, Khair D, Dagher H, Saad H, Cherfan P, Kaafarani MA, Jamaluddine Z, Ghattas H. Factors associated with human papilloma virus (HPV) vaccine recommendation by physicians in Lebanon, a cross-sectional study. Vaccine. 2018;36:7562–7. doi:10.1016/j.vaccine.2018.10.065.
- Abi Jaoude J, Saad H, Farha L, Dagher H, Khair D, Kaafarani MA, Jamaluddine Z, Cherfan P. Barriers, attitudes and clinical approach of Lebanese physicians towards HPV vaccination; a cross- sectional study. Asian Pac J Cancer Prev. 2019;20:3181–7. doi:10.31557/apjcp.2019.20.10.3181.
- Hamdi S. The impact of teachings on sexuality in Islam on HPV vaccine acceptability in the Middle East and North Africa region. J Epidemiol Glob Health. 2018;7(Suppl S1):S17–s22. doi:10.1016/j.jegh.2018.02.003.
- Farsi NJ, Baharoon AH, Jiffri AE, Marzouki HZ, Merdad MA, Merdad LA. Human papillomavirus knowledge and vaccine acceptability among male medical students in Saudi Arabia. Hum Vaccin Immunother. 2021;17:1968–74. doi:10.1080/21645515.2020.1856597.
- Obeid DA, Almatrrouk SA, Alfageeh MB, Al-Ahdal MNA, Alhamlan FS. Human papillomavirus epidemiology in populations with normal or abnormal cervical cytology or cervical cancer in the Middle East and North Africa: a systematic review and meta-analysis. J Infect Public Health. 2020;13:1304–13. doi:10.1016/j.jiph.2020.06.012.
- Dochez C, Al Awaidy S, Mohsni E, Fahmy K, Bouskraoui M. Strengthening national teams of experts to support HPV vaccine introduction in Eastern Mediterranean countries: lessons learnt and recommendations from an international workshop. Vaccine. 2020;38:1114–19. doi:10.1016/j.vaccine.2019.11.027.
- Abdullahi LH, Hussey GD, Wiysonge CS, Kagina BM. Lessons learnt during the national introduction of human papillomavirus (HPV) vaccination programmes in 6 African countries: stakeholders’ perspectives. S Afr Med J. 2020;110:525–31. doi:10.7196/SAMJ.2020.v110i6.14332.
- Gamaoun R. Knowledge, awareness and acceptability of anti-HPV vaccine in the Arab states of the Middle East and North Africa region: a systematic review. East Mediterr Health J. 2018;24:538–48. doi:10.26719/2018.24.6.538.
- Huang Y, Chen C, Wang L, Wu H, Chen T, Zhang L. HPV vaccine hesitancy and influencing factors among university students in China: a cross-sectional survey based on the 3cs model. Int J Environ Res Public Health. 2022;19:14025. doi:10.3390/ijerph192114025.
- Van Boetzelaer E, Daae A, Winje BA, Vestrheim DF, Steens A, Stefanoff P. Sociodemographic determinants of catch-up HPV vaccination completion between 2016-2019 in Norway. Hum Vaccin Immunother. 2022;18:1976035. doi:10.1080/21645515.2021.1976035.
- Sidiropoulou M, Gerogianni G, Kourti FE, Pappa D, Zartaloudi A, Koutelekos I, Dousis E, Margari N, Mangoulia P, Ferentinou E, et al. Perceptions, knowledge and attitudes among young adults about prevention of HPV infection and immunization. Healthcare (Basel). 2022;10:1721. doi:10.3390/healthcare10091721.
- Ortashi O, Raheel H, Shalal M. Acceptability of human papilloma virus vaccination among women in the United Arab Emirates. Asian Pac J Cancer Prev. 2014;15:2007–11. doi:10.7314/apjcp.2014.15.5.2007.
- Abu-Raddad LJ, Ghanem KG, Feizzadeh A, Setayesh H, Calleja JM, Riedner G. HIV and other sexually transmitted infection research in the Middle East and North Africa: promising progress? Sex Transm Infect. 2013;89(Suppl S3):iii1–4. doi:10.1136/sextrans-2013-051373.
- Mallik MK, Alramadhan B, Dashti H, Al-Shaheen A, Al Juwaiser A, Das DK, George SS, Kapila K. Human papillomaviruses other than 16, 18 and 45 are the major high risk HPV genotypes amongst women with abnormal cervical smear cytology residing in Kuwait: implications for future vaccination strategies. Diagn Cytopathol. 2018;46:1036–9. doi:10.1002/dc.24035.
- Kapila K, Balakrishnan M, Ali RH, Al-Juwaiser A, George SS, Mallik MK. Interpreting a diagnosis of atypical squamous cells of undetermined significance in cervical cytology and its association with human papillomavirus: a retrospective analysis of 180 cases in Kuwait. Sultan Qaboos Univ Med J. 2020;20:e318–23. doi:10.18295/squmj.2020.20.04.007.
- World Health Organization. Human papillomavirus vaccines: wHO position paper, October 2014-recommendations. Vaccine. 2015;33:4383–4. doi:10.1016/j.vaccine.2014.12.002.
- Barnard M, Cole AC, Ward L, Gravlee E, Cole ML, Compretta C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: a systematic literature review. Prev Med Rep. 2019;14:100884. doi:10.1016/j.pmedr.2019.100884.
- Sallam M, Ghazy RM, Al-Salahat K, Al-Mahzoum K, AlHadidi NM, Eid H, Kareem N, Al-Ajlouni E, Batarseh R, Ababneh NA, et al. The role of psychological factors and vaccine conspiracy beliefs in influenza vaccine hesitancy and uptake among Jordanian healthcare workers during the COVID-19 pandemic. Vaccines (Basel). 2022;10:1355. doi:10.3390/vaccines10081355.
- Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015;7. doi:10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289.