ABSTRACT
The ongoing COVID-19 pandemic highlights that complications and mortality associated with infectious diseases increase with age. Various vaccines are recommended for adults, but coverage rates remain suboptimal. Although co-administration would improve vaccine uptake and timely immunization, this is not routine practice in adults. We review key data on co-administration of vaccines in children and adults to reassure healthcare providers about its safety and advantages. In European countries and the United States, combined tetanus, diphtheria, and acellular pertussis boosters as well as meningococcal and human papillomavirus vaccines are recommended for healthy adolescents and adults of certain ages. Vaccination against influenza (annually), pneumococcal disease, and herpes zoster is recommended for older adults and specific risk groups. While co-administration is well established in children, it is less common in adults. Travelers can also receive multiple co-administered vaccines. Pediatric and travel vaccine co-administration has a well-established positive benefit-risk profile and is an efficient and cost-saving strategy to improve coverage. Healthcare providers could more often recommend and practice vaccine co-administration; this would not risk patient safety and health, would improve protection against vaccine-preventable diseases, and would help comply with national vaccination calendars. Recommending bodies may consider revising vaccination schedules to reduce the number of visits.
Background
The ongoing global coronavirus disease 2019 (COVID-19) pandemic highlights that susceptibility of adults to infectious diseases and associated complications or mortality increase with age. The world’s population is aging; in Europe, the proportion of people aged 65 years and above is forecasted to increase from 20.6% in 2020 to approximately 30% in 2050.Citation1
The COVID-19 pandemic also confirms that vaccination programs are highly effective,Citation2 underscoring that well-implemented vaccination strategies are a crucial determinant in fostering the health and independence of the aging population.Citation3 Currently, several vaccines are available and recommended to European adolescents and adults in certain age groups, such as those against influenza (annually), pneumococcal or meningococcal disease, herpes zoster, diphtheria, tetanus, pertussis, and human papillomavirus, and also against tick-borne encephalitis in endemic regions.Citation4 Other adult vaccines are expected to enter the market in the future, further crowding vaccination calendars. Because the success of vaccination programs is highly dependent on vaccine uptake, strategies to improve coverage are becoming increasingly important.Citation5,Citation6
Although COVID-19 vaccines have only been on the market since late 2020, their coverage was the highest reached across Europe (>70%) in a record time (i.e., one year).Citation7 Despite existing recommendations, such a broad coverage in adults has not been reached in decades for influenza vaccination, not even in risk groups or elderly populations.Citation8 Low vaccination rates in adults are frequently associated with missed opportunities to vaccinate.Citation6,Citation9 Therefore, co-administration of vaccines has a substantial role to play in decreasing the number of consultations and hence missed opportunities, and can increase timeliness of vaccination.Citation10 After an initial observation period of widespread COVID-19 vaccine use in the real-world setting, national and international health authorities have started recommending co-administration of COVID-19 vaccines with vaccines against other diseases based on the limited data available along with general vaccinology principles.Citation11,Citation12 The Advisory Committee on Immunization Practices (ACIP) in the United States was first to issue recommendations for co-administration of COVID-19 vaccines with other vaccines.Citation11 European countries later issued recommendations on co-administration of influenza and COVID-19 vaccines before the influenza season in the Northern Hemisphere.Citation13,Citation14 However, in adults, co-administration of vaccines has not yet become a routine practice, and related recommendations keep evolving. In this non-systematic literature review, we present key data on co-administered vaccines, with the aim of reassuring healthcare providers and thus potentially improving uptake and timely administration of adult vaccines. The cited references were selected by the authors based on their expert opinion and knowledge of the field, as well as from the results of a broad literature search in PubMed using various combinations of the terms “co-administration,” “vaccine,” “adult,” “children,” and “travel.”
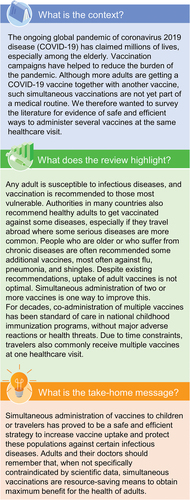
A plain language summary contextualizing the relevance, the results, and the impact of our work is presented in .
Importance of adult vaccination
While all adults are at risk of infectious diseases, particular risk groups include pregnant women, persons who are immunocompromised, obese, have chronic respiratory conditions, or are undergoing oncologic treatments, older adults, travelers, sexual minorities, intravenous drug users, alcohol abusers, and smokers.Citation15–25 Vaccine-preventable diseases such as influenza, pneumococcal disease, or herpes zoster have the highest incidence and severity in older adults because of comorbidities and immunosenescence, but younger populations are also susceptible.Citation26–30 Although the true incidence of pertussis in adults is unclear due to underdiagnosis and underreporting, older adults and those with asthma or chronic obstructive pulmonary disease (COPD) are also at increased risk for pertussis and severe outcomes.Citation31–33
Combined tetanus, diphtheria, and acellular pertussis boosters are recommended for healthy adults in several European countries and the United States by national recommending bodies,Citation4,Citation34 and also for patients with COPD by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).Citation35 For patients with COPD, additionally, both the Centers for Disease Control and Prevention (CDC) in the United States and GOLD recommended vaccination against pneumococcal disease, influenza, and herpes zoster.Citation35,Citation36 Younger people may need meningococcal and human papillomavirus vaccines.Citation4,Citation34 Travelers may be recommended or even required to get vaccinated against yellow fever, meningococcal disease, poliomyelitis, hepatitis B and/or A, rabies, typhoid fever, etc., depending on endemicity of these diseases at their destinations.Citation37 Healthcare professionals in travel clinics might administer several vaccines during a single consultation,Citation38,Citation39 often due to the lack of time of travelers for multiple appointments before departure.
Efficiently implemented adult immunization strategies provide an opportunity to maintain functional ability of adults, their families, their communities, and their countries, and hence to improve medical, social, and economic outcomes.Citation6 However, coverage of adult vaccination remains suboptimal and varies highly depending on vaccine, geographic region, or other factors.Citation40,Citation41 Therefore, further efforts from the global community and governments are needed to improve implementation of adult immunization programs.Citation6 Healthcare professionals are the first line of contact with patients, and their contribution is a cornerstone for the implementation of strategies to increase vaccination coverage in adults.Citation42
Principles of vaccine co-administration
Simultaneous administration of two or more vaccines at different injection sites during the same appointment is generally referred to as concomitant or co-administration. It is one of the most efficient approaches to foster vaccination coverage rate, reduce the number of vaccination consultations and thus costs, raise compliance with recommendations, guarantee the timely administration of vaccines according to the recommended age or needs, and to adopt and implement new vaccines.Citation43 Co-administration reduces the number of missed vaccination opportunities,Citation10 which are frequently the cause of low vaccination ratesCitation9 or of incomplete primary vaccination.Citation44 Furthermore, if vaccines were administered separately, transient adverse events would be reported at each visit, and the total cumulative number of transient adverse events would likely be greater than after co-administration of multiple vaccines. Because co-administration is convenient for both patients and healthcare providers, it contributes to the first of the four pillars (Convenience & Easy Access, Patient Communication, Enhanced Vaccination Systems, and Motivation) proposed to convert “vaccine availability” to “vaccination acceptance” throughout life.Citation9,Citation37
Concerns with vaccine co-administration
In Europe, vaccines may be co-administered as indicated in the Summary of Product Characteristics or if no specific contraindications or scientific evidence to discourage simultaneous administration exist.Citation43 However, there are some concerns about potential negative immunological interference and adverse reactions.
In theory, immunologic interference between co-administered vaccines can enhance or impair the immunogenicity of vaccine antigens. In reality, there are very few vaccine combinations and scenarios for which co-administration is contraindicated because of negative immunologic interference. In the United States, such contraindications for currently used vaccines comprise simultaneous administration of the 13-valent pneumococcal conjugate vaccine (PCV13) with the meningococcal diphtheria conjugate vaccine in persons with functional or anatomic asplenia and/or human immunodeficiency virus infection, and PCV13 with the 23-valent pneumococcal polysaccharide vaccine ().Citation45
Table 1. Guidelines of the ACIP in the United States for spacing of live and inactivated vaccines.Citation45.
By contrast, co-administration in adults is supported by numerous studies that evaluated simultaneous administration of the most widely recommended adult vaccines (i.e., those against influenza, pneumococcal infections, herpes zoster, combined diphtheria and tetanus, and COVID-19 vaccines).Citation46–49 The general principles for timing and spacing of immunobiologics published by the ACIP, including co-administration recommendations for live and inactivated vaccines (),Citation45 could also be adopted more widely in Europe. Except for the few aforementioned specific situations,Citation45 contraindications for co-administration could be the same as those for each vaccine alone. While in the United States the ACIP provides a detailed overview on contraindications for all licensed vaccines,Citation50 in Europe no such comprehensive general guidelines exist.
Safety of vaccine co-administration is detailed in subsequent sections.
Proven co-administration strategies
Throughout the life of an individual, the vaccination schedule is most challenging in infancy and childhood. Co-administration of pediatric vaccines demonstrated an excellent safety and immunogenicity profile, and has consequently become a widely accepted practice worldwide.Citation51 In the United States, the CDC recommends co-administration of routine pediatric vaccines, and supports this recommendation without concerns about immunogenicity and safety.Citation52 Co-administration of pediatric vaccines is also foreseen in immunization schedules across European countries, and infants may simultaneously receive up to four vaccines included in national immunization programs.Citation4 Co-administration of childhood vaccines has been common practice for decades and proved to be an efficient strategy to maintain or even increase vaccine uptake. Despite some regional and sociodemographic differences, the coverage of the vast majority of pediatric vaccines exceeds 90% in both the United States and in Europe.Citation53,Citation54
Fast approaching departure dates impose time constraints on travelers, and co-administration of several (sometimes up to six) required, routine, or recommended vaccines is thus a common practice in travel clinics.Citation38,Citation39 In a large prospective study conducted in healthy German travelers, although the overall frequency of systemic side effects increased with the number of simultaneously administered vaccines (36.7% for two, 40.3% for three, and 50.0% for more than three), the subjective rating by the study participants showed an excellent tolerability of multiple vaccinations before travel.Citation55 Feasibility of co-administration has also been shown in Chinese applicants for a United States immigrant visa, who had to be immunized against diphtheria, tetanus, pertussis, Haemophilus influenzae type b, poliomyelitis, hepatitis B, measles, mumps, rubella, varicella, influenza, and pneumococcal disease.Citation38 Approximately half of the study participants (49.6%) reported side effects, all of which were transient. In Japanese travelers who received up to five simultaneous vaccines against either hepatitis A, hepatitis B, rabies, Japanese encephalitis, diphtheria, tetanus, measles, mumps, and poliomyelitis, the frequency of adverse reactions also increased with the number of simultaneously administered vaccines. However, the overall rate of adverse events was only 26.3%, of which most were transient injection site reactions.Citation39 All three studies concluded that co-administration of multiple vaccines to travelers was well tolerated.Citation38,Citation39,Citation55 Hence, the inconvenience of multiple vaccination visits before travel may outweigh the inconvenience of a slight increase of side effects after simultaneous administration of several vaccines at a single visit.
Conclusions
While simultaneous administration of multiple childhood or travel vaccines during one visit has become the standard of care, co-administration of routine vaccines for adults is only slowly becoming common practice by healthcare providers. Reluctance of routine adult vaccine co-administration with a COVID-19 vaccine can be explained by the initial contraindication for co-administration, which was based on a lack of data in the first months of use of the novel COVID-19 vaccines. Subsequently, recommendations for co-administration of COVID-19 vaccines were issued within a year of licensure; since this practice was implemented, very few risks have been observed and no serious issues emerged. Despite this, reluctance toward co-administration remains considerable and seems to extend even to vaccines with an already established safety profile, for which extensive data on co-administration with other routine vaccines has been accrued. Increasing awareness on the safety of vaccine co-administration may lead to an improvement in compliance to recommendations and ultimately, improved coverage rates for routine adult vaccines.
Having separate appointments, whether they are requested by patients or offered by healthcare providers for each vaccine, is detrimental for vaccination coverage among adults and may lead to increased use of resources. Co-administration of routine childhood vaccines and adult vaccines to travelers has proved to be a safe and efficient strategy to improve coverage and protect these populations against vaccine-preventable diseases for which they are at risk. The success of these strategies may increase confidence of healthcare providers in routine adult vaccine co-administration, which might be of significant added value once integrated into regular practices to ensure compliance with recommendations. This is especially important considering the recent licensure of new pneumococcal conjugate vaccines and potential future licensure of respiratory syncytial virus vaccines, which will make adult vaccination calendars even more challenging.
Authors’ contributions
LB-J wrote the first draft of the manuscript. All authors reviewed the drafts critically and provided invaluable feedback for the development of the present manuscript. All authors approved the final submitted version.
Acknowledgments
The authors thank the Akkodis Belgium platform, on behalf of GSK, for editorial assistance and manuscript coordination. Alpár Pöllnitz provided medical writing support, and Camille Turlure coordinated the manuscript development and provided editorial support.
Disclosure statement
PB discloses support by GSK for participation in advisory boards, formative events, and Data Safety Monitoring Board or Advisory Board for Shigella vaccine. RS discloses support (grants, consulting fees, support for attending meetings and/or travel, payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing, educational events, participation on Data Safety Monitoring Boards or Advisory Boards) from Bavarian Nordic, Emergent BioSolutions, GSK, Merck, Pfizer, Sanofi Pasteur, Takeda, Valneva, outside of the submitted work. RS is president of the International Society of Travel Medicine Foundation. JS discloses consulting fees from AstraZeneca, Bavarian Nordic, GSK, Sanofi Pasteur, Pfizer, Johnson & Johnson, MSD, BioNTech, Seqirus, Takeda; payment or honoraria for lectures, presentations, speaker bureaus, manuscript writing, or educational events from GSK, Sanofi Pasteur, Pfizer, Johnson & Johnson, MSD, BioNTech, Seqirus, Takeda; support for attending meetings and/or travel from Sanofi Pasteur and holding shares from Valneva, outside of the submitted work. LB-J was an employee of GSK at the time of the study. IP and MZ are employees of GSK and hold GSK shares. PVD reports grants obtained by the University of Antwerp from GSK, Pfizer, Sanofi, Merck, Takeda, Baxter, CanSino China, Themis, Osivax, Johnson & Johnson, Abbott, The Bill & Melinda Gates Foundation, PATH, Flemish Government, and European Union, and participation to Janssen Vaccines and Virometrix Data Safety Monitoring Boards, outside of the submitted work. Neither of the authors declares non-financial relationships and activities.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Additional information
Funding
References
- Eurostat. Population structure and ageing. 2021 [accessed 2021 Dec 7]. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#Slightly_more_than_three_persons_of_working_age_for_every_person_aged_65_or_over.
- Harder T, Koch J, Vygen-Bonnet S, Külper-Schiek W, Pilic A, Reda S, Scholz S, Wichmann O. Efficacy and effectiveness of COVID-19 vaccines against SARS-CoV-2 infection: interim results of a living systematic review, 1 January to 14 May 2021. Euro Surveill. 2021;26(28):2100563. doi:10.2807/1560-7917.es.2021.26.28.2100563.
- Doherty TM, Connolly MP, Del Giudice G, Flamaing J, Goronzy JJ, Grubeck-Loebenstein B, Lambert PH, Maggi S, McElhaney JE, Nagai H, et al. Vaccination programs for older adults in an era of demographic change. Eur Geriatr Med. 2018;9(3):289–6. doi:10.1007/s41999-018-0040-8.
- ECDC. Vaccine schedules in all countries in the EU/EEA. 2021 [accessed 2021 Dec 7]. https://vaccine-schedule.ecdc.europa.eu/.
- Bonanni P, Bonaccorsi G, Lorini C, Santomauro F, Tiscione E, Boccalini S, Bechini A. Focusing on the implementation of 21st century vaccines for adults. Vaccine. 2018;36(36):5358–65. doi:10.1016/j.vaccine.2017.07.100.
- Privor-Dumm LA, Poland GA, Barratt J, Durrheim DN, Deloria Knoll M, Vasudevan P, Jit M, Bonvehí PE, Bonanni P. A global agenda for older adult immunization in the COVID-19 era: a roadmap for action. Vaccine. 2021;39(37):5240–50. doi:10.1016/j.vaccine.2020.06.082.
- ECDC. COVID-19 vaccine tracker. 2021 [accessed 2021 Dec 7]. https://qap.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab.
- Rizzo C, Rezza G, Ricciardi W. Strategies in recommending influenza vaccination in Europe and US. Hum Vaccin Immunother. 2018;14(3):693–8. doi:10.1080/21645515.2017.1367463.
- Lin CJ, Nowalk MP, Pavlik VN, Brown AE, Zhang S, Raviotta JM, Moehling KK, Hawk M, Ricci EM, Middleton DB, et al. Using the 4 pillars™ practice transformation program to increase adult influenza vaccination and reduce missed opportunities in a randomized cluster trial. BMC Infect Dis. 2016;16(1):623. doi:10.1186/s12879-016-1940-1.
- WHO. Increasing RI coverage by reducing missed opportunities for vaccination. [accessed 2022 Aug 23]. https://cdn.who.int/media/docs/default-source/immunization/mov/who-mov-materials-2pager-l3.pdf?sfvrsn=dfdbba0_6.
- CDC. Interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Coadministration of COVID-19 vaccines with other vaccines. 2021 [accessed 2021 Dec 7]. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html#Coadministration.
- WHO. Coadministration of seasonal inactivated influenza and COVID-19 vaccines: interim guidance. 2021 [accessed 2021 Dec 7]. https://apps.who.int/iris/rest/bitstreams/1382850/retrieve.
- Koch J, Wichmann O, Mertens T. STIKO-Empfehlung zur Koadministration von COVID-19-Impfstoffen und anderen Totimpfstoffen und die dazugehörige wissenschaftliche Begründung. Epid Bull. 2021;39:42–5 doi:10.25646/9044.
- Hoge Gezondheidsraad . Gelijktijdige toediening van vaccins tegen COVID-19 met andere vaccins (simultane vaccinatie). [Co-administration of vaccines against COVID-19 with other vaccines (simultaneous vaccination)]. 2021 [accessed 2021 Dec 7]. https://www.health.belgium.be/sites/default/files/uploads/fields/fpshealth_theme_file/20211006_hgr-9675_simultane_vaccinatie_covid19_vweb.pdf.
- Karlsson EA, Beck MA. The burden of obesity on infectious disease. Exp Biol Med. 2010;235(12):1412–24. doi:10.1258/ebm.2010.010227.
- Sappenfield E, Jamieson DJ, Kourtis AP. Pregnancy and susceptibility to infectious diseases. Infect Dis Obstet Gynecol. 2013;2013:752852. doi:10.1155/2013/752852.
- McGrath B, Broadhurst M, Roman C. Infectious disease considerations in immunocompromised patients. JAAPA. 2020;33(9):16–25. doi:10.1097/01.JAA.0000694948.01963.f4.
- Lange P. Chronic obstructive pulmonary disease and risk of infection. Pneumonol Alergol Pol. 2009;77(3):284–8. doi:10.5603/ARM.27817.
- Bender BS. Infectious disease risk in the elderly. Immunol Allergy Clin North Am. 2003;23(1):57–64, vi. doi:10.1016/s0889-8561(02)00078-4.
- Vento S, Cainelli F. Infections in patients with cancer undergoing chemotherapy: aetiology, prevention, and treatment. Lancet Oncol. 2003;4(10):595–604. doi:10.1016/s1470-2045(03)01218-x.
- Chen LH, Blair BM. Infectious risks of traveling abroad. Microbiol Spectr. 2015;3(4). doi:10.1128/microbiolspec.IOL5-0005-2015.
- Levitt A, Mermin J, Jones CM, See I, Butler JC. Infectious diseases and injection drug use: public health burden and response. J Infect Dis. 2020;222(Supplement_5):S213–7. doi:10.1093/infdis/jiaa432.
- Vaisrub S. Homosexuality—a risk factor in infectious disease. JAMA. 1977;238(13):1402. doi:10.1001/jama.1977.03280140080031.
- Jiang C, Chen Q, Xie M. Smoking increases the risk of infectious diseases: a narrative review. Tob Induc Dis. 2020;18:60. doi:10.18332/tid/123845.
- Morojele NK, Shenoi SV, Shuper PA, Braithwaite RS, Rehm J. Alcohol use and the risk of communicable diseases. Nutrients. 2021;13(10):3317. doi:10.3390/nu13103317.
- Vousden N, Bunch K, Knight M, UKOSS Influenza Co-Investigators Group. Incidence, risk factors and impact of seasonal influenza in pregnancy: a national cohort study. PLoS One. 2021;16(1):e0244986. doi:10.1371/journal.pone.0244986.
- Torres A, Blasi F, Dartois N, Akova M. Which individuals are at increased risk of pneumococcal disease and why? Impact of COPD, asthma, smoking, diabetes, and/or chronic heart disease on community-acquired pneumonia and invasive pneumococcal disease. Thorax. 2015;70(10):984–9. doi:10.1136/thoraxjnl-2015-206780.
- Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833. doi:10.1136/bmjopen-2014-004833.
- Cromer D, van Hoek AJ, Jit M, Edmunds WJ, Fleming D, Miller E. The burden of influenza in England by age and clinical risk group: a statistical analysis to inform vaccine policy. J Infect. 2014;68(4):363–71. doi:10.1016/j.jinf.2013.11.013.
- Nasreen S, Wang J, Kwong JC, Crowcroft NS, Sadarangani M, Wilson SE, McGeer A, Kellner JD, Quach C, Morris SK, et al. Population-based incidence of invasive pneumococcal disease in children and adults in Ontario and British Columbia, 2002–2018: a Canadian Immunization Research Network (CIRN) study. Vaccine. 2021;39(52):7545–53. doi:10.1016/j.vaccine.2021.11.032.
- Jenkins VA, Savic M, Kandeil W. Pertussis in high-risk groups: an overview of the past quarter-century. Hum Vaccin Immunother. 2020;16(11):2609–17. doi:10.1080/21645515.2020.1738168.
- Kandeil W, Atanasov P, Avramioti D, Fu J, Demarteau N, Li X. The burden of pertussis in older adults: what is the role of vaccination? A systematic literature review. Expert Rev Vaccines. 2019;18(5):439–55. doi:10.1080/14760584.2019.1588727.
- Aris E, Harrington L, Bhavsar A, Simeone JC, Ramond A, Papi A, Vogelmeier CF, Meszaros K, Lambrelli D, Mukherjee P. Burden of pertussis in COPD: a retrospective database study in England. COPD. 2021;18(2):157–69. doi:10.1080/15412555.2021.1899155.
- CDC. Adult immunization schedule: recommendations for ages 19 years or older, United States. 2022 [accessed 2022 Aug 23]. https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html.
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for prevention, diagnosis and management of chronic obstructive lung disease: 2022 report. 2021 [accessed 2021 Dec 7]. https://goldcopd.org/wp-content/uploads/2021/12/GOLD-REPORT-2022-v1.1-22Nov2021_WMV.pdf.
- CDC. Lung disease including asthma and adult vaccination. [accessed 2021 Dec 7]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/lung-disease.html.
- Philip RK, Attwell K, Breuer T, Di Pasquale A, Lopalco PL. Life-course immunization as a gateway to health. Expert Rev Vaccines. 2018;17(10):851–64. doi:10.1080/14760584.2018.1527690.
- Hua L, Hongtao H, Shunqin W, Jinping G, Jiandong C, Zhaoliang L, Xinwen F. Simultaneous vaccination of Chinese applicants for a United States immigrant visa. Travel Med Infect Dis. 2008;6(3):130–6. doi:10.1016/j.tmaid.2008.03.004.
- Mizuno Y, Kano S, Urashima M, Genka I, Kanagawa S, Kudo K. Simultaneous vaccination in Japanese travelers. Travel Med Infect Dis. 2007;5(2):85–9. doi:10.1016/j.tmaid.2006.09.001.
- Lu PJ, Hung MC, Srivastav A, Grohskopf LA, Kobayashi M, Harris AM, Dooling KL, Markowitz LE, Rodriguez-Lainz A, Williams WW. Surveillance of vaccination coverage among adult populations-United States, 2018. MMWR Surveill Summ. 2021;70(3):1–26. doi:10.15585/mmwr.ss7003a1.
- Garbinsky D, Hunter S, La EM, Poston S, Hogea C. State-level variations and factors associated with adult vaccination coverage: a multilevel modeling approach. Pharmacoecon Open. 2021;5(3):411–23. doi:10.1007/s41669-021-00262-x.
- de Gomensoro E, Del Giudice G, Doherty TM. Challenges in adult vaccination. Ann Med. 2018;50(3):181–92. doi:10.1080/07853890.2017.1417632.
- Bonanni P, Boccalini S, Bechini A, Varone O, Matteo G, Sandri F, Gabutti G. Co-administration of vaccines: a focus on tetravalent Measles-Mumps-Rubella-Varicella (MMRV) and meningococcal C conjugate vaccines. Hum Vaccin Immunother. 2020;16(6):1313–21. doi:10.1080/21645515.2019.1688032.
- Turner N, Grant C, Goodyear-Smith F, Petousis-Harris H. Seize the moments: missed opportunities to immunize at the family practice level. Fam Pract. 2009;26(4):275–8. doi:10.1093/fampra/cmp028.
- CDC. Timing and spacing of immunobiologics. General best practice guidelines for immunization: best practices guidance of the Advisory Committee on Immunization Practices (ACIP). 2021 [accessed 2021 Dec 7]. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/timing.html.
- Frenck RW Jr., Gurtman A, Rubino J, Smith W, van Cleeff M, Jayawardene D, Giardina PC, Emini EA, Gruber WC, Scott DA, et al. Randomized, controlled trial of a 13-valent pneumococcal conjugate vaccine administered concomitantly with an influenza vaccine in healthy adults. Clin Vaccine Immunol. 2012;19(8):1296–303. doi:10.1128/cvi.00176-12.
- Song JY, Cheong HJ, Tsai TF, Chang HA, Choi MJ, Jeon JH, Kang SH, Jeong EJ, Noh JY, Kim WJ. Immunogenicity and safety of concomitant MF59-adjuvanted influenza vaccine and 23-valent pneumococcal polysaccharide vaccine administration in older adults. Vaccine. 2015;33(36):4647–52. doi:10.1016/j.vaccine.2015.05.003.
- Domnich A, Grassi R, Fallani E, Ciccone R, Bruzzone B, Panatto D, Ferrari A, Salvatore M, Cambiaggi M, Vasco A, et al. Acceptance of COVID-19 and influenza vaccine co-administration: insights from a representative Italian survey. J Pers Med. 2022;12(2):139. doi:10.3390/jpm12020139.
- CDC. Administering shingrix. [accessed 2021 Dec 7]. https://www.cdc.gov/vaccines/vpd/shingles/hcp/shingrix/administering-vaccine.html.
- CDC. Contraindications and precautions. General best practice guidelines for immunization: best practices guidance of the Advisory Committee on Immunization Practices (ACIP). 2021 [accessed 2021 Dec 7]. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html.
- Bauwens J, Saenz LH, Reusser A, Künzli N, Bonhoeffer J. Safety of co-administration versus separate administration of the same vaccines in children: a systematic literature review. Vaccines. 2019;8(1):12. doi:10.3390/vaccines8010012.
- CDC. Multiple vaccinations at once. 2021 [accessed 2021 Dec 7]. https://www.cdc.gov/vaccinesafety/concerns/multiple-vaccines-immunity.html.
- Hill HA, Yankey D, Elam-Evans LD, Singleton JA, Pingali SC, Santibanez TA. Vaccination coverage by age 24 months among children born in 2016 and 2017 - national immunization survey-child, United States, 2017–2019. MMWR Morb Mortal Wkly Rep. 2020;69(42):1505–11. doi:10.15585/mmwr.mm6942a1.
- Bechini A, Boccalini S, Ninci A, Zanobini P, Sartor G, Bonaccorsi G, Grazzini M, Bonanni P. Childhood vaccination coverage in Europe: impact of different public health policies. Expert Rev Vaccines. 2019;18(7):693–701. doi:10.1080/14760584.2019.1639502.
- Börner N, Mühlberger N, Jelinek T. Tolerability of multiple vaccinations in travel medicine. J Travel Med. 2003;10(2):112–16. doi:10.2310/7060.2003.31690.