 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Current WHO/UNICEF estimates of routine childhood immunization coverage reveal the largest sustained decline in uptake in three decades with pronounced setbacks across Africa. Although the COVID-19 pandemic has induced significant supply and delivery disruptions, the impact of the pandemic on vaccine confidence is less understood. We here examine trends in vaccine confidence across eight sub-Saharan countries between 2020 and 2022 via a total of 17,187 individual interviews, conducted via a multi-stage probability sampling approach and cross-sectional design and evaluated using Bayesian methods. Multilevel regression combined with poststratification weighting using local demographic information yields national and sub-national estimates of vaccine confidence in 2020 and 2022 as well as its socio-demographic associations. We identify declines in perceptions toward the importance of vaccines for children across all eight countries, with mixed trends in perceptions toward vaccine safety and effectiveness. We find that COVID-19 vaccines are perceived to be less important and safe in 2022 than in 2020 in six of the eight countries, with the only increases in COVID-19 vaccine confidence detected in Ivory Coast. There are substantial declines in vaccine confidence in the Democratic Republic of Congo and South Africa, notably in Eastern Cape, KwaZulu-Natal, Limpopo, and Northern Cape (South Africa) and Bandundu, Maniema, Kasaï-Oriental, Kongo-Central, and Sud-Kivu (DRC). While over 60-year-olds in 2022 have higher vaccine confidence in vaccines generally than younger age groups, we do not detect other individual-level socio-demographic associations with vaccine confidence at the sample sizes studied, including sex, age, education, employment status, and religious affiliation. Understanding the role of the COVID-19 pandemic and associated policies on wider vaccine confidence can inform post-COVID vaccination strategies and help rebuild immunization system resilience.
Introduction
The latest World Health Organization (WHO) estimates of national immunization coverage depict worrisome trends. Compared to 2019, six million fewer children received a third-dose diphtheria, tetanus, and pertussis vaccine in 2021, with similar losses for other routine vaccines including those against measles, polio, and human papillomavirus (HPV).Citation1 Globally, few countries have managed to avoid losses in uptake rates of routine childhood immunization uptake, with low- and middle-income countries particularly affected. As countries across Africa have emerged from pandemic restrictions, outbreaks of vaccine-preventable diseases are materializing across multiple settings,Citation2–5 threatening to reverse disease elimination gains made over the past decades. Disruptions in vaccination supply chains, reallocation of limited but already stretched health-care resources to tackle the COVID-19 pandemic, and travel restrictions have played a substantial role in lowering uptake of routine childhood immunizations.Citation6,Citation7 Yet the role of demand-side barriers – such as vaccine confidence – in modulating uptake routine childhood immunizations over the course of the COVID-19 pandemic is not well understood. Although many studies have probed African populations’ attitudes toward COVID-19 vaccines,Citation8–10 we are unable to find evidence of studies tracking perceptions toward vaccines generally over the COVID-19 pandemic in Africa. Without a quantitative understanding of vaccine confidence dynamics, plausibly impacted by the COVID-19 pandemic, its associated policies, or factors associated with the COVID-19 vaccine rollout on vaccine confidence, strategies to address declining uptake rates of childhood immunizations may be misdirected.
In this study, we harness data from sixteen national surveys and over 17,000 individuals across eight countries conducted in 2020 and 2022 to explore national and sub-national trends in and determinants of vaccine confidence. These eight countries are the Democratic Republic of Congo (DRC), Ivory Coast, Kenya, Niger, Nigeria, Senegal, South Africa, and Uganda. Each of these settings is surveyed between October and December 2020Citation10 and again between January and March 2022. In this study, we measure vaccine confidence, defined as perceptions toward vaccines themselves, rather than broader confidence in, for example, the systems and people that deliver vaccines (though we note that vaccine confidence is often defined in this expanded way).Citation11 Thus, we measure perceptions toward the importance, safety, and effectiveness of vaccines, with the former of these two metrics now used in the WHO Behavioural and Social Drivers framework as the major elements of vaccine confidence.Citation12 We do this for both perceptions toward vaccines in general as well as the COVID-19 vaccines specifically. A quantitative understanding the evolution of vaccine confidence via large-scale data collection can shed a light onto vaccination barriers, prompt further discussion and research, and facilitate the design of new public health policies.
Methods
Data sources
Between October and December 2020, a total of 8,465 individuals were surveyed across the eight study countries, with an additional 8,703 individuals surveyed between January and March 2022. In each wave of data collection, at least 1,000 individuals were surveyed in each country via a cross-sectional design (see Table S1 for further survey information). All surveys were conducted via face-to-face interviews except for Kenya in 2022 which employed a computer-assisted telephone interview design (Table S1). (We note that while both face-to-face and telephone interview designs aim for nationally representative surveys, there may be a survey type bias in Kenya which may be a data collection limitation in this setting.) All face-to-face surveys used a stratified random household probability sampling design that involved: (1) stratification of sub-national regions within each country by first administrative unit; (2) urban and rural stratification within administrative units to ensure sufficient representativeness of hard-to-reach rural communities; (3) selection of primary sampling units (PSUs) using simple random sampling; (4) random selection of households within each PSU; and (5) random selection of individuals within households imposing a quota of 50% male and 50% female. For each face-to-face survey, a sample of about 100 PSUs were selected in each country, with each PSU comprising approximately 10 interviews. Areas within PSUs were selected via probability proportional to size sampling. The study inclusion criteria for all surveys are all citizens aged 18 and over on the day of the survey interview and residents in private households of any type. Any sampled locations with restrictions such as nursing homes, military barracks, etc. were not eligible for study inclusion. All data was collected by ORB International and partners of the Worldwide Independent Network of Market Research (WIN) (www.orb-international.com and www.winmr.com).
Survey items
Seven vaccine confidence items are collected in each time point that relate to individual perceptions around the importance, safety, effectiveness of vaccines generally as well as COVID-19 vaccines specifically (see response variables, ). Each respondent is asked to report their level of agreement to each question on a Likert scale (response variables). Individual data on sex, age, highest education level, religious affiliation, and employment status are also recorded (explanatory variables) as well as the first administrative unit in which the resident resides. These data permit an analysis of the socio-demographic determinants of vaccine confidence as well as an evaluation of how these determinants have shifted between 2020 and 2022. To avoid the loss of missing data in response variables, responses to the vaccine confidence items are recoded to a binary scale, where 1 represents agreement to each survey item (that is, agreement that vaccines are important, safe, and effective) and 0 represents non-agreement including missing data. To avoid the loss of missing data in explanatory data, non-responses are given their own separate category, which is included in the regression analysis. See for all variable information and recodes and Table S2 for a breakdown of respondents across all demographic groups for each country and survey year.
Table 1. Study data. All survey items are shown with possible responses (including recodes, if any) for response and explanatory variables, and baselines used in the multilevel logistic regressions as described in the main text.
Model-based vaccine confidence estimates
A four-level Bayesian multilevel logistic regression model is implemented for each item. The four tiers comprise individuals nested within sub-national regions nested within country and then time (2020 or 2022). The inference goals are threefold: to obtain individual-level probabilities of agreement to each survey item (to be post-stratified, see below); to generate estimates for the strength of association between socio-demographic characteristics and each item; and to derive estimates of the changing strength of association between socio-demographics and vaccine confidence over time. Letting denote whether individual
in sub-national region
in country
at time
either agrees (1) or disagrees (0) with the
th vaccine confidence survey item, then agreement to each item is modeled via a separate four-level Bayesian multilevel logistic regression model
, where
,
, and
, where
is the probability of agreement to question q,
is a matrix of dummy-coded explanatory variables () with baselines incorporated into an intercept, and
is an index corresponding to each column in
. The following prior distributions are specified,
,
,
, where
represents the precision of the normal distribution (that is,
) and the gamma distribution is defined in terms of the shape
and rate
,
. To evaluate whether a socio-demographic determinant has changed in it is association with vaccine confidence over time with respect to a baseline group, the statistic
is used, which is a difference in log-odds ratios for country-level effects between
(2020) and
(2022). If
(
) then the association between an explanatory variable and its respective baseline group has increased (decreased) over time.
The probabilities of agreement for each surveyed individual are reweighted by poststratification weights obtained as the ratio of the proportion of the number of adults in each country belonging to the same age, sex, and administrative region strata to the corresponding proportion in that country’s sample. The expected strata counts for each country are obtained from two data sources that provide sub-national demographic information: the United States census bureau (https://www.census.gov/geographies/mapping-files/time-series/demo/international-programs/subnationalpopulation.html) and City Population (www.citypopulation.de). This post-stratification step provides an additional layer of robustness to the multistage cluster sampling design.
In total, seven independent multilevel regressions as described above are fit to the data, one for each of the vaccine confidence response variables in . All model outputs are reported as either a percentage point change (vaccine confidence) or as log odds ratios (socio-demographic determinants) together with a 95% highest posterior density interval (HPDI). Throughout, associations between socio-demographic drivers and confidence items are considered “significant” when the 95% HPDI excludes zero. All analyses are implemented in R version 4.2.2. Bayesian model inference is performed using the RJAGS library which computes posterior distributions via Gibbs sampling.Citation13 All data and code used in this study is freely available at https://osf.io/wbx3h/.
Results
National trends
We report on the largest increases and decreases in vaccine confidence between 2020 and 2022. All raw and model-based estimates of national vaccine confidence levels can be found in Table S3 in the supplementary materials, while sub-national estimates can be found in the supplementary data file.
We find an overall reduction in the percentage of respondents agreeing that vaccines are important for children across all eight countries between 2020 and 2022. The biggest falls in agreement that vaccines are important for children are in DRC (−20·0% points, 95% HPDI, −23·9 to −15·8), Uganda (−14·0, −18·0 to −10·1), and Nigeria (−10·5, −13·6 to −7·5) (). In Nigeria and DRC there are also substantial decreases in confidence in vaccine safety (Nigeria: −8·6, −11·6 to −5·6; DRC: −13·2, −18·0 to −8·7) and effectiveness (Nigeria: −6·2, −9·4 to −3·1; DRC Congo: −17·2, −21·7 to −12·7) perceptions (). Agreement that vaccines are important for people of all ages has decreased in Ivory Coast, Kenya, Nigeria, South Africa, and Uganda, while they have increased in Senegal (). In Ivory Coast, Kenya, and Senegal, vaccine safety perceptions have also improved ().
Figure 1. Declining trends in vaccine confidence across the sub-Saharan countries DRC, Ivory Coast, Kenya, Niger, Nigeria, Senegal, South Africa, and Uganda. The estimated percentage of respondents for each country agreeing that vaccines in general (a) and the COVID-19 vaccine specifically (b) are important, safe, and effective in 2020 and 2022. Percentages are only shown if the 95% highest posterior density interval for the change in agreement over time excludes zero.
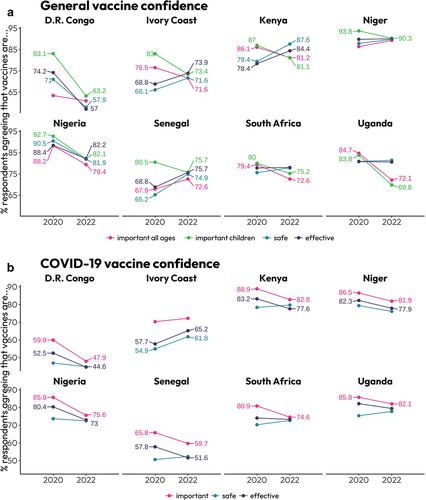
Perceptions around the importance of the COVID-19 vaccine have fallen in all countries, except for Ivory Coast, where no change is detected (). The largest falls in perceptions of the importance of COVID-19 vaccines are in DRC (−12·0, −16·6 to −7·1), Nigeria (−10·2, −13·9 to −6·8) and South Africa (−6·3, −11·3 to −1·1). Compared to 2020, perceptions around the safety of the COVID-19 vaccine have remained consistent in all countries, except Ivory Coast, where confidence in COVID-19 vaccine safety and effectiveness has improved (). However, respondents in DRC, Kenya, Niger, Senegal, and Nigeria currently perceive the COVID-19 vaccine to be less effective compared to 2020 ().
Sub-national trends
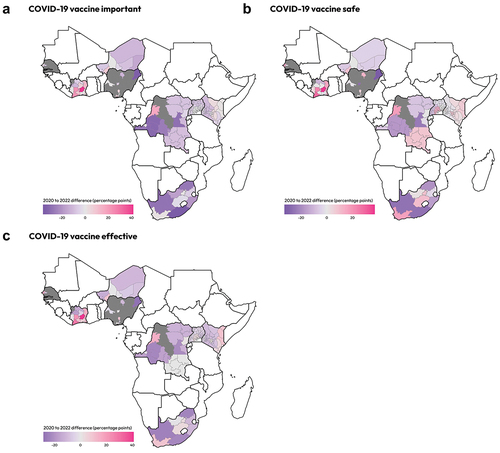
To summarize sub-national changes in vaccine confidence, we list regions with increases or decreases (where the 95% HPDI excludes zero) in vaccine confidence across at least four of the seven survey items. In total, there are 17 sub-national regions with decreases in at least four of the seven survey items. In DRC, there are five regions: Bandundu, Maniema, Kasaï-Oriental, Kongo-Central, and Sud-Kivu. In South Africa there are four: Eastern Cape, KwaZulu-Natal, Limpopo, and Northern Cape. There are three in Nigeria: Borno, Kano, and Federal Capital Territory. In Niger, there are two: Diffa and Zinder. In Ivory Coast, Kenya, and Uganda there are one in each: Savanes, Rift Valley, and Northern Region (respectively) (see ). There are increases in confidence on at least four of the seven survey items in only six sub-national regions: Équateur (D.R. Congo); Bas-Sassandra and Lacs (Ivory Coast); Tahoua (Niger); Dakar (Senegal); and Gauteng (South Africa) ().
Figure 2. Subnational estimates of temporal changes in vaccine confidence from 2020 to 2022. Model-based estimates of the sub-national changes in vaccine confidence from 2020 to 2022 given as a difference in percentage points. Estimates are provided for these differences in perceptions toward vaccine importance (a,b), safety (c), and effectiveness (d). Blue colors denote a decrease in confidence since 2020, while pink colors denote an increase. Grey colors signify that no samples were collected in that region in either 2020 or 2022 and so a difference cannot be computed.
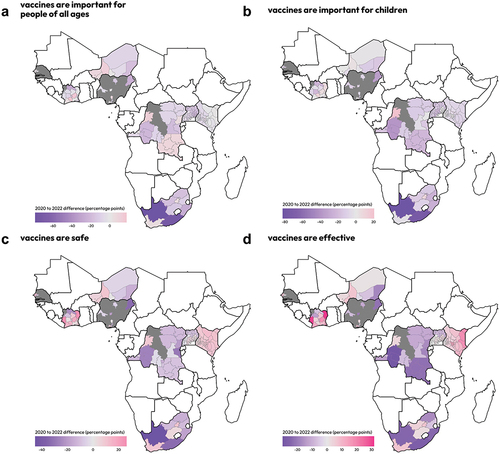
Figure 3. Subnational estimates of temporal changes in COVID-19 vaccine confidence from 2020 to 2022. Model-based estimates of the sub-national changes in COVID-19 vaccine confidence from 2020 to 2022 given as a difference in percentage points. Estimates are provided for these differences in perceptions toward vaccine importance (a), safety (b), and effectiveness (c). Blue colors denote a decrease in confidence since 2020, while pink colors denote an increase. Grey colors signify that no samples were collected in that region in either 2020 or 2022 and so a difference cannot be computed.
Socio-demographic associations
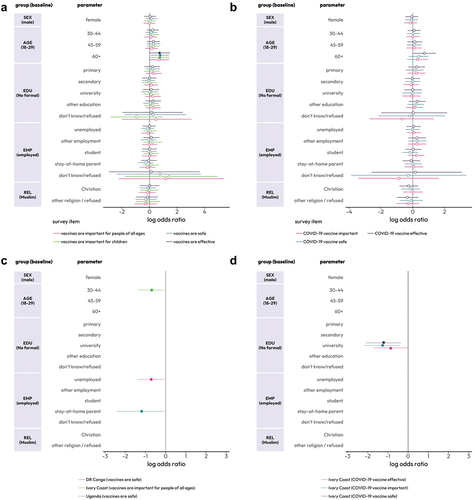
An evaluation of the socio-demographic determinants of vaccine confidence averaged across all countries for all seven items (that is in Methods) reveals that only age in 2022 holds a significant association with vaccine confidence, with over 60s more likely than 18–29-year-olds to agree that vaccines in general are safe, effective, and important for children (). An assessment of the change in socio-demographic determinants of vaccine confidence between 2020 and 2022 in each country reveals that 30–44-year-olds in Ivory Coast have become less confident in the importance of vaccines for people of all ages, while unemployed respondents in DRC and stay-at-home parents in Uganda have become less confident in the safety of vaccines (). University-educated respondents in Ivory Coast have become less confident in the safety, importance, and effectiveness of the COVID-19 vaccine ().
Figure 4. Socio-demographic determinants of vaccine confidence in sub-Saharan Africa. Socio-demographic associations across all countries are shown in (a) and (b) for general and COVID-19 vaccine confidence (respectively) for 2022 data only. (All log-odds ratios in 2020 had 95% highest posterior density intervals – HPDI – that included zero, and these results are not displayed. A filled dot denotes that the 95% HPDI excludes zero.) Changes in socio-demographic associations with vaccine confidence are shown in (c) and (d) where log-odds ratios less (greater) than one signify that the socio-demographic group has become less (more) confident over time with respect to the baseline category: only log-odds ratios whose 95% highest posterior density interval excludes zero are shown. Colours represent country-question combinations and are indicated in the legend below the four plots.
Discussion
The findings of this study reveal the state of vaccine confidence at national and sub-national levels across eight countries in sub-Saharan Africa. To our knowledge, this is the first multi-country study examining temporal trends in vaccine confidence at sub-national levels across the sub-Sahara. Our study reveals broad declines in perceptions toward the importance of vaccines, with perceptions toward the importance of vaccines for children falling across all eight countries studied. There were notable falls in confidence in DRC and Nigeria, especially with regard to perceptions of vaccine safety and effectiveness. At a sub-national level, there were notable vaccine confidence falls in Bandundu, Maniema, Kasaï-Oriental, Kongo-Central, and Sud-Kivu (DRC) and Eastern Cape, KwaZulu-Natal, Limpopo, and Northern Cape (South Africa).
A recent study by Lazarus and colleagues explored trends in vaccine acceptance across 23 countries between 2010 and 2021, and found decreases in intent to accept a COVID-19 among South African and Nigerian respondents between 2020 and June 2021, consistent with the findings of this study.Citation14 A multi-country COVID-19 vaccine acceptance study conducted in 2021 in sub-Saharan settings by Anjorin and colleagues found high rates of vaccine hesitancy in DRC with only 47% of respondents indicating that they might accept a COVID-19 vaccine, with South Africa, Nigeria, and Kenya reporting lower rates of hesitancy.Citation15 Another multi-country COVID-19 acceptance study in sub-Saharan Africa by Kanyanda and colleagues found relatively high rates of COVID-19 vaccine acceptance in Nigeria in 2021,Citation9 aligning with the earlier wave of data collection in this study. High rates of COVID-19 vaccine hesitancy have also been found among medical students in Uganda.Citation15
Recent reviews of COVID-19 vaccine hesitancy across Africa have found consistent themes emerge around the drivers of low acceptance that include vaccine safety concerns,Citation8,Citation16–18 low-risk perception,Citation8,Citation16,Citation18 as well as distrust of pharmaceutical companies and exposure to misinformation.Citation8 Males and individuals with higher education levels are also found to be consistent predictors of lower vaccine hesitancy,Citation14,Citation16,Citation17,Citation19 results that are not consistent with our findings. These discrepancies may be due to the differing measurement instruments surrounding vaccine hesitancy or confidence, variable rates of hesitancy over time, or the national scope of our surveys in contrast to highly region- or group-specific surveys, for example studies that investigated health-care workers,Citation20–22 rural communities,Citation18 or other small qualitative samples.Citation23,Citation24 Many studies do find that younger age groups are more hesitant and less willing to accept COVID-19 vaccination than older adults, consistent with our findings.Citation25–27
A review into the determinants of COVID-19 vaccine acceptance in South Africa by Cooper and colleagues found a range of factors associated with acceptance, including urbanicity, with individuals in more rural regions less likely to accept the vaccine.Citation28 An expert opinion by the authors concludes that “COVID-19 has substantially increased vaccine concerns and potential hesitancy predispositions in South Africa,” which strongly aligns with our findings.Citation28 A separate study in Limpopo found that the presence of visits by traditional healers was more common in COVID-19 unvaccinated than vaccinated.Citation29 Our findings add to this literature base: the largest falls in vaccine confidence in South Africa appear to be in predominantly rural provinces, including Limpopo, Eastern Cape, and Kwazulu Natal. Confidence losses in these regions should be carefully monitored, especially as they may translate to childhood immunizations which – currently – appear to be relatively homogeneous across South Africa.Citation30 While COVID-19 vaccine confidence appears higher in urban areas in South Africa, the reverse seems to be true in Senegal where evidence suggests vaccine refusal is higher in large cities.Citation31 As only two sub-national regions of Senegal are considered in this study, evaluating whether refusal is higher in urban areas has not been possible.
An examination of temporal trends in COVID-19 vaccine confidence in Nigeria by Sato found that COVID-19 vaccine hesitancy had increased between 2020 and 2021 in line with this study. In Kenya, however, a recent study by Rego and colleaguesCitation32 found that COVID-19 vaccine refusal – as measured via the question “would you agree to be vaccinated if the vaccine was available at no cost” – decreased from 24% to 9% between February and October 2021, which is perhaps contrary to the findings of our study, as we find a decrease in COVID-19 vaccine confidence, although our second wave was conducted in 2022. Despite possible decreases in perceptions toward the importance and effectiveness of the COVID-19 in Kenya, perceptions toward the safety and effectiveness of vaccines in general have increased.
In conclusion, our study paints a worrying picture of declining vaccine confidence trends across many sub-national regions in sub-Saharan Africa, notably in DRC where confidence losses are particularly large. While sub-national estimates and modeling of local vaccination rates exist across Africa,Citation30,Citation33,Citation34 there is limited evidence of routinely collected vaccine confidence data across Africa at national or sub-national levels. While Sato,Citation35 Rego et al.,Citation32 and Lazarus et al.Citation14 have collected temporal data on COVID-19 trends, we currently lack a thorough investigation of whether losses in confidence in COVID-19 vaccines will translate to other immunization programs. As there is precedent for vaccine confidence losses in one vaccine to trigger confidence losses in others,Citation36 the losses in confidence in COVID-19 vaccines found in this study may be a cause for concern with respect to childhood immunizations, especially if the losses witnessed are related to institutional distrust, a key factor associated with uptake of routine immunizations for children.Citation37 Early warning signals of confidence losses – such as those detected in this study – can provide time to respond, in case of other epidemics, pandemics, or other emerging crises. Confidence monitoring at sub-national resolutions can also provide clearer signals to the regions and groups facing confidence losses and can better prepare policymakers and stakeholders for potential losses in vaccine uptake. Regional losses in confidence – such as those established in this study – can translate to an increased clustering of non-vaccinated individuals, which may pose challenges for herd immunity goals.Citation38
Author contributions
Conceptualization: AdF, ET, RT, HJL
Methodology: AdF
Investigation: AdF
Visualization: AdF
Funding acquisition: ET, RT, HJL
Project administration: AdF, ET, RT, HJL
Writing – original draft: AdF
Writing – review & editing: AdF, ET, RT, HJL
Ethical statement
All data used in this study were collected by ORB International funded by Africa CDC following local laws and ethical best practices. Local fieldwork teams obtained informed consent prior to data collection and no personally identifiable data were recorded by the fieldwork teams. Africa CDC own the data. All data used in this study are freely available in the public domain at https://orb-international.com/african-perceptions-on-covid-19-vaccines/.
Supplemental Material
Download MS Excel (127 KB)Supplemental Material
Download PDF (245.3 KB)Disclosure statement
Within the last two years, HJL was involved in collaborative grants with GlaxoSmithKline, Merck and Johnson & Johnson. HJL has also received other support for participating in Merck meetings and GlaxoSmithKline advisory round tables. Within the last two years, AdF has been funded by the Merck Investigator Studies Program and has performed consultancy work for Pfizer Inc.
Data availability statement
All data and code used in this study is freely available at https://osf.io/wbx3h/. Raw data is also freely available in the public domain at https://orb-international.com/african-perceptions-on-covid-19-vaccines/.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2213117.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- World Health Organization. Progress and challenges with achieving universal immunization coverage: technical document [Internet]. 2022 [accessed 2022 Sept 15]. https://www.who.int/publications/m/item/progress-and-challenges.
- Roberts L. Africa battles out-of-control polio outbreaks. Science. 2022;375(6585):1–9. doi:10.1126/science.adb1920.
- CDC. Measles in Africa [Internet]. 2022 [accessed 2022 Nov 23]. https://wwwnc.cdc.gov/travel/notices/watch/measles-africa.
- Berjaoui C, Tabassum S, Sabuncu Ö, Al Tarawneh YJ, Naeem A, El Khoury C, Bacha IT, Wellington J, Uwishema O. Measles outbreak in Zimbabwe: an urgent rising concern. Ann Med Surg. 2022;82:82. doi:10.1016/j.amsu.2022.104613.
- WHO Africa. Vaccine-preventable disease outbreaks on the rise in Africa [Internet]. 2022 [accessed 2022 Nov 23]. https://www.afro.who.int/news/vaccine-preventable-disease-outbreaks-rise-africa.
- Causey K, Fullman N, Sorensen RJD, Galles NC, Zheng P, Aravkin A, Danovaro-Holliday MC, Martinez-Piedra R, Sodha SV, Velandia-González MP, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398(10299):522–34. doi:10.1016/S0140-6736(21)01337-4.
- Shet A, Carr K, Danovaro-Holliday CM, Sodha SV, Prosperi C, Wunderlich J, Wonodi C, Reynolds HW, Mizra I, Gacic-Dobo M, et al. Impact of the SARS-CoV-2 pandemic on routine immunization services: evidence of disruption and recovery from 169 countries and territories. SSRN Electron J. 2021. doi:10.2139/ssrn.3850009.
- Ackah BB, Woo M, Stallwood L, Fazal ZA, Okpani A, Ukah UV, Adu P. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Heal Res Policy. 2022;7(1):1–20. doi:10.1186/s41256-022-00255-1.
- Kanyanda S, Markhof Y, Wollburg P, Zezza A. Acceptance of COVID-19 vaccines in sub-Saharan Africa: evidence from six national phone surveys. BMJ Open. 2021;11(12):e055159. doi:10.1136/bmjopen-2021-055159.
- Africa CDC. COVID 19 vaccine perceptions: a 15 country study [Internet]. 2021 [accessed 2022 Oct 25]. https://africacdc.org/download/covid-19-vaccine-perceptions-a-15-country-study/.
- Shapiro GK, Kaufman J, Brewer NT, Wiley K, Menning L, Leask J, Abad N, Betsch C, Bura V, Correa G, et al. A critical review of measures of childhood vaccine confidence. Curr Opin Immunol. 2021;71:34–45. doi:10.1016/j.coi.2021.04.002.
- World Health Organization. Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022. Wkly Epidemiol Rec. 2022;97:209–24.
- Plummer M. rjags: Bayesian graphical models using MCMC. R Packag. version 3–132016. 2023.
- Lazarus JV, Wyka K, White TM, Picchio CA, Rabin K, Ratzan SC, Parsons Leigh J, Hu J, El-Mohandes A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. 2022;13(1). doi:10.1038/s41467-022-31441-x.
- Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, Agira D, Wamala NK, Asiimwe A, Matovu D, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. 2021;49(1). doi:10.1186/s41182-021-00331-1.
- Gudayu TW, Mengistie HT. COVID-19 vaccine acceptance in sub-Saharan African countries: a systematic review and meta-analysis. Heliyon. 2023;9(2):e13037. doi:10.1016/j.heliyon.2023.e13037.
- Alemayehu A, Demissie A, Yusuf M, Gemechu Lencha A, Oljira L. Covid-19 vaccine acceptance and determinant factors among general public in East Africa: a systematic review and meta-analysis. Heal Serv Res Manag Epidemiol. 2022;9:233339282211062. doi:10.1177/23333928221106269.
- Davis TP, Yimam AK, Kalam MA, Tolossa AD, Kanwagi R, Bauler S, Kulathungam L, Larson H. Behavioural determinants of COVID-19-vaccine acceptance in rural areas of six lower-and middle-income countries. Vaccines. 2022;10(2):214. doi:10.3390/vaccines10020214.
- Larson HJ, MC GE, Murray CJL. The vaccine hesitant moment. N Engl J Med. 2022;87(1):58–65. doi:10.1056/NEJMra2106441.
- Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, Lora Mwimba B, Cikomola Mwana Bene A, Mukamba Musenga E. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic republic of the Congo. pragmatic Obs Res. 2020;Volume 11:103–9. doi:10.2147/POR.S271096.
- Adejumo OA, Ogundele OA, Madubuko CR, Oluwafemi RO, Okoye OC, Okonkwo KC, Owolade SS, Junaid OA, Lawal OM, Enikuomehin AC, et al. Perceptions of the COVID-19 vaccine and willingness to receive vaccination among health workers in Nigeria. Osong Public Heal Res Perspect. 2021;12(4):236–43. doi:10.24171/j.phrp.2021.0023.
- Adeniyi OV, Stead D, Singata-Madliki M, Batting J, Wright M, Jelliman E, Abrahams S, Parrish A. Acceptance of COVID-19 vaccine among the healthcare workers in the eastern cape, South Africa: a cross sectional study. Vaccines. 2021;9(6):666. doi:10.3390/vaccines9060666.
- Tibbels NJ, Dosso A, Fordham C, Benie W, Brou JA, Kamara D, Hendrickson ZM, Naugle DA. “On the last day of the last month, I will go”: a qualitative exploration of COVID-19 vaccine confidence among Ivoirian adults. Vaccine. 2022;40(13):2028–35. doi:10.1016/j.vaccine.2022.02.032.
- Chukwuocha UM, Emerole CO, Iwuoha GN, Dozie UW, Njoku PU, Akanazu CO, Eteike PO, Hemingway C. Stakeholders’ hopes and concerns about the COVID-19 vaccines in Southeastern Nigeria: a qualitative study. BMC Public Health. 2022;22(1). doi:10.1186/s12889-022-12754-4.
- Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. infect Drug Resist. 2021;Volume 14:2015–25. doi:10.2147/IDR.S312116.
- Anjorin AAA, Odetokun IA, Abioye AI, Elnadi H, Umoren MV, Damaris BF, Eyedo J, Umar HI, Nyandwi JB, Abdalla MM, et al. Will Africans take COVID-19 vaccination? PLoS One. 2021;16(12):e0260575. doi:10.1371/journal.pone.0260575.
- Bongomin F, Olum R, Andia-Biraro I, Nakwagala FN, Hassan KH, Nassozi DR, Kaddumukasa M, Byakika-Kibwika P, Kiguli S, Kirenga BJ. COVID-19 vaccine acceptance among high-risk populations in Uganda. Ther Adv Infect Dis. 2021;8:204993612110243. doi:10.1177/20499361211024376.
- Cooper S, van Rooyen H, Wiysonge CS. COVID-19 vaccine hesitancy in South Africa: how can we maximize uptake of COVID-19 vaccines? Expert Rev Vaccines. 2021;20(8):921–33. doi:10.1080/14760584.2021.1949291.
- Mbombi MO, Muthelo L, Mphekgwane P, Dhau I, Tlouyamma J, Nemuramba R, Mashaba RG, Mothapo K, Maimela E. Prevalence of COVID-19 vaccine hesitancy in a rural setting: a case study of DIMAMO health and demographic surveillance site, Limpopo province of South Africa. J Respir. 2022;2(2):101–10. doi:10.3390/jor2020008.
- Mosser JF, Gagne-Maynard W, Rao PC, Osgood-Zimmerman A, Fullman N, Graetz N, Burstein R, Updike RL, Liu PY, Ray SE, et al. Mapping diphtheria-pertussis-tetanus vaccine coverage in Africa, 2000–2016: a spatial and temporal modelling study. Lancet. 2019;393(10183):1843–55. doi:10.1016/S0140-6736(19)30226-0.
- Ba MF, Faye A, Kane B, Diallo AI, Junot A, Gaye I, Bonnet E, Ridde V. Factors associated with COVID-19 vaccine hesitancy in Senegal: a mixed study. Hum Vaccines Immunother. 2022;18(5). doi:10.1080/21645515.2022.2060020.
- Rego RTT, Kenney B, Ngugi A, Espira L, Orwa J, Siwo G, Sefa C, Shah J, Weinheimer-Haus E, Delius A, et al. COVID-19 vaccination refusal trends in Kenya over 2021. SSRN Electron J. 2022. doi:10.2139/ssrn.4138298.
- Utazi CE, Thorley J, Alegana VA, Ferrari MJ, Takahashi S, Metcalf CJE, Lessler J, Tatem AJ. High resolution age-structured mapping of childhood vaccination coverage in low and middle income countries. Vaccine. 2018;36(12):1583–91. doi:10.1016/j.vaccine.2018.02.020.
- Galles NC, Liu PY, Updike RL, Fullman N, Nguyen J, Rolfe S, Sbarra AN, Schipp MF, Marks A, Abady GG, et al. Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: a systematic analysis for the global burden of disease study 2020, release 1. Lancet. 2021;398(10299):503–21. doi:10.1016/S0140-6736(21)00984-3.
- Sato R. Vaccine hesitancy against COVID-19 vaccine over time in Nigeria. Vaccine. 2023;41(17):41. doi:10.1016/j.vaccine.2023.03.029.
- Larson HJ, Hartigan-Go K, de Figueiredo A. Regarding response by Dans et. al. to our article, “ Vaccine confidence plummets in the Philippines following dengue vaccine scare: why it matters to pandemic preparedness.”. Hum Vaccines Immunother. 2019;15(3):630. doi:10.1080/21645515.2018.1556079.
- Stoop N, Hirvonen K, Maystadt JF. Institutional mistrust and child vaccination coverage in Africa. BMJ Glob Health. 2021;6(4):e004595. doi:10.1136/bmjgh-2020-004595.
- Salathé M, Bonhoeffer S. The effect of opinion clustering on disease outbreaks. J R Soc Interface. 2008;5(29):1505–8. doi:10.1098/rsif.2008.0271.
