ABSTRACT
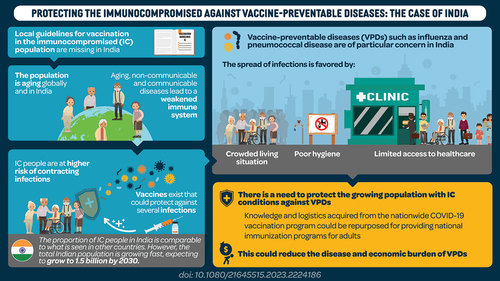
Immunocompromised (IC) populations are at increased risk of vaccine-preventable diseases (VPDs). In India, the concern of VPDs in IC populations is particularly acute due to the prevalence of crowded living situations, poor sanitation and variable access to healthcare services. We present a narrative review of IC-related disease and economic burden, risk of VPDs and vaccination guidelines, based on global and India-specific literature (2000–2022). IC conditions considered were cancer, diabetes mellitus, chronic kidney disease, respiratory disorders, disorders treated with immunosuppressive therapy, and human immune deficiency virus (HIV). The burden of IC populations in India is comparable to the global population, except for cancer and HIV, which have lower prevalence compared with the global average. Regional and socioeconomic inequalities exist in IC prevalence; VPDs add to the burden of IC conditions, especially in lower income strata. Adult vaccination programs could improve health and reduce the economic impact of VPDs in IC populations.
Plain Language Summary
What is the context?
The population is aging, both globally and in India. Older age is associated with a weakened immune system. People with an immunocompromised (IC) status have a higher risk of contracting infections. The combination of these conditions greatly increases risk from infectious disease. A large percentage of infections, referred to as vaccine-preventable diseases (VPDs), could be avoided by vaccination. However, India-specific guidelines for adult immunization are limited and there is a low awareness of these recommendations among healthcare professionals and patients.
What is new?
The proportion of people with IC conditions in India is comparable to that seen in other countries. However, the risk of VPDs, such as influenza and bacterial pneumonia, is of particular concern in India; several factors, such as crowded living situation, poor hygienic conditions, and lack of access to healthcare may favor the spread of infections. The consequences of infections have the greatest impact on families with low income. Furthermore, only few India-specific guidelines exist with recommendations for adult immunization.
What is the impact?
There is a need to protect the growing IC populations against VPDs. The introduction of public healthcare and the experience from the nationwide COVID−19 immunization program in India provide an opportunity to extend adult vaccination programs covering other VPDs. Immunization programs could reduce the economic and disease burden associated with VPDs. Clear national guidelines and communication strategies are required to increase awareness of the benefit of vaccination.
Introduction
Vaccine-preventable diseases (VPDs) impose a substantial burden on patients, their families and the healthcare system. The burden of VPDs is however not uniformly distributed across the population, as infants, older people and people with an immunocompromised (IC) state are at higher risk of infectious diseases and associated complications. Over the past 50 years, IC populations have increased both in high and low- to middle-income countries, including India.Citation1–3 While some IC conditions are due to inherited dysfunctions in the immune system,Citation4 most IC conditions arise secondary to other diseases or associated immunosuppressive therapies.Citation5 The observed rise in IC prevalence can be explained partly by medical advances leading to IC populations living longer, the growing list of clinical indications for immunosuppressive therapies, and a globally aging population, who usually also have reduced immune function.Citation1,Citation3,Citation5–7 Thus, the increase in IC populations may be directly linked with age-related loss of immunocompetence or indirectly through the increased risk of non-communicable diseases (NCDs), such as cancer or diabetes, and some communicable diseases, such as human immunodeficiency virus (HIV) infection.Citation2,Citation5
Impaired host defenses mean that IC adults are at increased risk of VPDs. The morbidity and mortality associated with these infections is also higher among IC adults.Citation8–11 Additionally, the severity and risk of adverse outcomes associated with VPDs are substantially increased in the IC population.Citation2,Citation6,Citation12–14 If the growing population of IC adults are not protected against VPDs, increasing pressure will be put on the Indian health and social systems to meet healthcare demands due to both NCDs and VPDs.Citation15 Despite vaccination being one of the most effective strategies for disease prevention, achieving high vaccination rates among IC adults remains a challenge in developing countries.Citation16–19 The reasons might be multifactorial, including poor infrastructure and access to healthcare services as well as low awareness of adult vaccination guidelines among healthcare professionals and patients.Citation20
While the implications of poor adult vaccination coverage have been discussed in detail for European and North American healthcare systems, there is less discussion in low- and middle-income countries such as India. The situation is particularly difficult in India, where much of the population is subject to crowded living situations, poor diet, lack of access to healthcare and substandard sanitation systems, increasing the risk for spread of infectious disease.Citation21,Citation22 In addition, limited surveillance of VPDs in Indian adults means the burden of disease is likely to be significantly underestimated.Citation23 Therefore, compared with adult IC populations in high-income countries (who are already identified as at risk for VPDs), adults with IC conditions residing in India are likely to be at even greater risk of VPDs.
In the wake of the recent coronavirus disease 2019 (COVID−19) pandemic, India has an unprecedented opportunity to implement nationwide adult immunization programs leveraging existing COVID−19 infrastructure.Citation24 Political decisiveness is required to utilize the logistics and expertise acquired during the pandemic as long as knowledge and infrastructure are still effective and functional.
In this narrative review, we will discuss the risk of VPDs among IC adults in India and highlight the unmet needs to improve vaccination coverage in this population. In addition, we review existing vaccination policies globally and in India and their potential to alleviate economic and health-related disease burden.
Material and methods
In order to understand the risk of VPDs for IC adults in India, a narrative review was conducted guided by the following questions:
What is the prevalence of IC populations in India and the associated economic burden?
What are the risks and complications of VPDs in IC populations?
What are the recommendations and guidelines available for vaccination of IC populations globally and locally?
A literature search was conducted in two main databases, PubMed and Embase, using keywords and MeSH terms based on the questions above (). Due to the high degree of variation among different IC populations, we have focused our search on the following IC populations: cancer patients, patients taking immunosuppressive treatment (including transplant patients, rheumatological conditions), patients with diabetes, chronic kidney disease or HIV. There were no limits on the VPDs in the search strategy. The search was limited to publications from 2000 to 2022 and excluded the pediatric population, non-human and in vitro studies. Guidelines included were international vaccine recommendations and recommendations from the United States (US) and United Kingdom (UK), which are known to be consulted as reference documents in the conception of local vaccination guidelines in India. Publication with latest data on disease and economic burden were selected with preference given to studies conducted in the US and the UK to substantiate the vaccination guidelines that were selected.
Table 1. Search terms used for literature review.
Results
A total of 94 publications were included in the narrative review, 33 describing disease and economic burden in IC populations (21 specific to India), 35 focusing on the risk of VPDs in IC populations (6 specific to India) and 33 publications presenting vaccination recommendations (7 specific to India). Seven publications were assigned to more than one category.
Disease burden of IC populations
India is projected to be the most populous country in the world very shortly.Citation25 The population of adults aged ≥60 years is growing at a rate three times faster than that of the total Indian population and will account for 19% of the worldwide population by 2050 according to projections.Citation26 This shifting age structure, alongside rapid urbanization, lifestyle transitions, deteriorating diets and pollution, has resulted in a growing burden of immunocompromising NCDs.Citation15,Citation27–29 NCDs have become the primary cause of mortality in India, accounting for 60% of total deaths.Citation24,Citation30 The most prominent NCDs contributing to the overall IC population in India include cancer; disorders treated with immunosuppressive therapy, such as autoimmune diseases and transplant patients; diabetes mellitus (DM) and chronic kidney disease (CKD). Communicable diseases, foremost HIV, add to the overall size of the IC population in India.
Risk factors for NCDs in India have been evaluated in a systematic review: the authors found a significant increase in overweight and obesity among adults during the observation period between 2005 and 2016. Obesity favors the development of cardiac disease and diabetes; on the other hand, alcohol and tobacco consumptions, risk factors for cancer and chronic liver disease, declined.Citation15
Cancer incidence was estimated at 19.3 million new cases worldwide in 2020.Citation31 Globally, 10.0 million deaths were attributed to cancer.Citation31,Citation32 While cancer incidence in India is still markedly lower compared with global average (1,751 vs 3,943 per 100,000 people in India vs globally in 2019Citation9), it is expected to almost double by 2040.Citation33 Based on national registry data, significant heterogeneity in cancer burden in India was demonstrated, with the highest burden observed in the North and Northeast, and with men being proportionally more affected than women.Citation34,Citation35 Cancer contributes substantially to the number of IC adults in India (; ); not only can cancer itself cause a state of immunosuppression, but non-targeted, cytotoxic cancer therapy often compromise the immune system.Citation53
Figure 1. Prevalent cases/100,000 people globally and in India −2019.
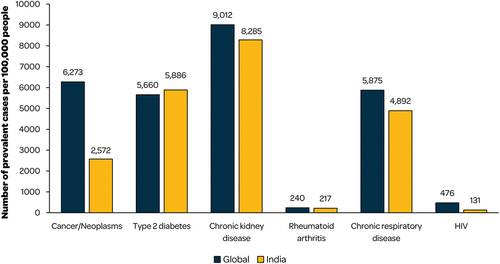
Table 2. Epidemiology and risk of infection in immunocompromised populations in 2019.Citation9.
Similarly, NCDs treated with immunosuppressive therapy increase the risk of infectious disease. Autoimmune disorders, such as rheumatoid disorders, multiple sclerosis (MS), inflammatory bowel disease (IBD), as well as people with asthma and transplant recipients are in general treated with immunosuppressive therapy. Based on a survey conducted at rural and urban centers in India, point estimates for different rheumatoid disorders varied between 0.02% (systematic lupus erythematosus [SLE]) and 4.39% (osteoarthritis), highlighting the substantial burden imposed by these disorders.Citation54 Incidence and clinical manifestation of SLE vary across countries, but some evidence suggests that morbidity and mortality are higher in people with Asian and African ancestry.Citation55 In India, clinical management of rheumatoid disorders is still in its infancy, with only few specialized centers providing care for people with rheumatoid disorders.Citation56 However, with the increased use of immunosuppressive therapy, the concern for infections in general, and tuberculosis in particular, has sharpened, adding to the burden of rheumatoid disorders.Citation56 Organ transplantation is dominated by people with end-stage renal kidney disease, with an estimated 7,500 people undergoing kidney transplant in India, followed by liver, heart and lung transplants.Citation57,Citation58 In addition, number of patients undergoing hematopoietic stem cell transplantation is steadily increasing every year, adding to the population being treated with immunosuppressive therapy.
The high-income Western lifestyle, characterized by poor nutritional choices and sedentary habits, has spread globally as income has risen, leading to an increase in obesity, type 2 diabetes (T2D) and cardiovascular diseases. In India, obesity affects more than 135 million individuals according to serial national surveys, but prevalence rates highly depend on age, gender, urban vs rural setting, socioeconomic status and geographical location.Citation30 Obesity is higher in women compared with men and higher in urban than rural settings: 22.5%, 45.6% and 57.4% of rural, urban low-class and urban middle-class women were considered obese, respectively.Citation30 Interestingly, Asian Indians tend to have more abdominal fat compared with Caucasians, increasing the detrimental effect of excess body weight on metabolic syndrome and cardiovascular risk factors. As a consequence, India is seeing a rise in its T2D population from ~69 million to an estimated 140 million in 2040.Citation30 Diabetes is also a major risk factor for chronic kidney disease (CKD), which is expected to increase in prevalence.Citation59 Malnutrition, poor sanitation and nephrotoxins are additional risk factors for CKD in India. However, the true burden of CKD is ill described in the absence of a national registry and the scarcity of centers dedicated to patients with renal disease.Citation60 Obesity, metabolic syndrome, T2D and CKD can all have deleterious effects on the immune system and account for a large number of IC adults in India ().Citation8,Citation61 Optimal disease control often improves a patient’s immune function; however, in India many cannot afford suitable treatment.Citation5,Citation60
Among communicable diseases, HIV is of particular concern, as the virus attacks CD4+ T cells, which are crucial for the proper functioning of the immune system.Citation5 Globally, approximately 38 million people live with HIV and in 2021, there were an estimated 1.5 million new HIV cases.Citation5,Citation62,Citation63
An estimated 2.14 million people are living with HIV in India, representing the third largest HIV population of any country worldwide.Citation64 While a slight downward trend in HIV incidence was observed in recent years, large variations were observed between districts, with incidence positively correlating with population size, density, urbanization and at-risk populations.Citation64–66 At the same time, prevalence is plateauing or increasing, likely due to improved clinical management leading to an increase in life expectancy.Citation67 The highest burden in terms of HIV prevalence was observed in the Northeast, particularly in the states of Mizoram, Nagaland and Manipur, all with prevalence >1% compared with the national prevalence of 0.22% in the adult population.Citation65,Citation68
Prevalence estimates (cases per 100,000 people) for different IC conditions are on a par with global estimates, except for cancer and HIV (). Together, the increase in NCDs and HIV infection along with the large and aging Indian population give rise to high levels of immunosuppression and thus aggravate susceptibility to infection in adults.
Economic burden of IC populations
The continuous increase in IC populations is a global problem, but India is more economically constricted when it comes to dealing with the health issues compared with high-income countries.Citation69 Only 1.5% of the overall global domestic product (GDP) is dedicated to public healthcare, while the total of public and private investments amounts to 4% of overall GDP.Citation69 Furthermore, healthcare policies in India are complex, as they need to deal with regional and social disparities, inequalities in access to healthcare and a large diversity in health-related problems originating both from infectious diseases and NCDs.Citation70
Despite some progress being made in the inauguration of healthcare programs, public health improvement has not advanced in India as in some other countries with similar GDP.Citation70 This could be due to competing interests on the political agenda, such as building infrastructure to improve sanitation and access to drinking water. Another possible reason lies in the deeply rooted Indian tradition that views personal care as a responsibility of family and kinship. Only a small proportion of the population has health insurance.Citation30 A large proportion of healthcare expenditure is paid out of pocket, often pushing people with IC conditions and their families into financial crisis and debt.Citation69,Citation71,Citation72 With the introduction in 2018 of the Ayushman Bharat Yojana health insurance scheme for Indian’s economically disadvantaged population, it is hoped that the financial strain imposed on families will be reduced with the goal of improving healthcare access for the most vulnerable and poor.Citation73
In India, annual direct and indirect costs for diabetes care were estimated at US$ 31.9 billion in 2010 and this economic burden is predicted to rise to nearly US$ 150 billion in 2030.Citation30 People with T2D from the low-income strata are estimated to spend 25% to 35% of their annual income on diabetes care.Citation30 In case of complications and hospitalizations, these costs can increase several-fold. Another aspect to consider is that Indians often develop metabolic syndrome and T2D at a younger age compared with Caucasians.Citation30 Increased T2D-related morbidity and mortality occur during peak years of their productive life and have profound effects not only on their personal finances and those of their families but also on the individual’s contribution to national economic growth.
The same holds true for HIV. In a household survey conducted in people diagnosed with HIV in India, HIV prevalence was highest in individuals 25–35 years old, representing people in the active labor force.Citation71 Twenty percent (20%) of HIV+ men and 10% percent of HIV+ women lost their employment. However, approximately 30% of women who were unemployed prior to HIV diagnosis, started working after diagnosis, which might reflect their obligation to cope with healthcare expenditures. Individual responses showed that patients who lost their jobs, also lost their savings and had to sell their possessions and take on debt to cover medical bills.Citation71
Burden of VPDs in IC populations
VPDs in adults impose a substantial burden to patients and the healthcare system, especially in the absence of life-course immunization programs.Citation74 Several studies have shown that infectious diseases lead to higher average costs per episode in patients with IC conditions compared with the general population.Citation36,Citation75,Citation76 In a retrospective healthcare database study conducted in the US, invasive pneumococcal disease (IPD) led to costs of $58.5 million per 100,000 patient years in people at high risk, including individuals with IC conditions and HIV, which were 23.4-fold higher compared with the general population.Citation74,Citation76 Incremental costs in the IC populations are driven by a higher probability of severe disease and complications, more frequent and longer hospitalization and need for additional specialized care ().Citation37,Citation74 In general, the risk of VPDs and the associated morbidity and mortality are high among IC adults ().Citation8–11
In a retrospective database study, conducted in the US, the risk of all-cause pneumonia and IPD was respectively 3.6 and 4.6-fold higher in IC populations compared with the general population.Citation36 In an English cohort study, the overall incidence of herpes zoster (HZ) in IC adults was 7.77/1000 person-years compared with 6.21/1000 person-years in immunocompetent adults.Citation77 This study also reported that older IC adults (≥80 years) had an almost five-fold greater risk of developing postherpetic neuralgia (PHN) compared with younger IC adults (18–49 years); PHN is a significant complication of HZ infection, associated with persistent pain and significant reduction in quality of life.Citation77 HZ epidemiology is similar in Asia with a lifetime risk of approximating 30% and a rising trend, most likely due to an aging population and increased use of immunosuppressive drugs.Citation38 Invasive meningococcal disease (IMD) has been reported in India both in endemic and epidemic settings, such as in mass gatherings during Haj pilgrimage.Citation78,Citation79 While Neisseria meningitidis is responsible for only approximately 1.9% of bacterial meningitis in all age groups confounded, the true burden of IMD in India is probably underestimated due to incomplete reporting.Citation80 In a French case–control study, the risk of IMD-related hospitalization was up to 39-fold higher in patients with primary immunodeficiency, and up to five-fold higher in people with chronic medical conditions.Citation43
In cancer patients, bacterial pneumonia is the most common infection. Cancer patients have a 40 to 50-fold increased risk of IPD compared with healthy adults.Citation81 Pneumonia frequently leads to hospitalization and need for mechanical ventilation.Citation40,Citation41 In a prospective study conducted in cancer patients admitted to the hospital with pneumonia, 81% required mechanical ventilation and 75% presented with septic shock.Citation41 Mortality rates were 45.8% in people admitted to the ICU and 64.9% in patients admitted to the general ward.Citation41 Cancer patients are also at increased risk of influenza and HZ and associated complications (e.g., PHN).Citation81
Adults with diabetes are six times more likely to be hospitalized during an influenza episode and are almost three times more likely to die of pneumonia complications compared with those who do not have diabetes.Citation46 In a multicenter, observational cohort study, diabetes was found to be an independent factor for mortality in patients with IPD (hazard ratio: 1.91; 95% confidence intervals: 1.23–3.03; p = .006).Citation47 In addition, higher hepatitis B infection rates were observed among people with diabetes compared with nondiabetic people.Citation45
CKD is a risk factor for influenza-related hospitalization, especially in people with glomerular filtration rates <30 mL/min/1.73 m2.Citation48 A study in India examined the proportion of risk factors in patients with IPD. Among 233 patients with invasive pneumococcal disease, 151 (62%) had at least one risk factor for pneumococcal infection, with the most common ones being CKD (n = 37), malignant disease (n = 31), diabetes (n = 27) and immunosuppressive treatment (n = 32).Citation82
People with HIV are at increased risk of severe disease from both hepatitis A (HAV) and B (HBV) infection.Citation51,Citation83,Citation85 HBV co-infection in patients with HIV results in higher rates of chronicity and occult HBV (HBV-DNA positivity in the absence of the hepatitis B surface antigen) increased end-stage liver disease, higher mortality from liver complications and decreased response to treatment.Citation51 This co-infection is particularly concerning in India, where prevalence of HIV-HBV co-infection is 8.3%.Citation51 The risk of bacterial and viral respiratory tract infections, as well as IMD is higher in people with HIV compared with the general population.Citation74,Citation84 HIV-positive individuals are at higher risk of developing serious influenza-related complications when they contract influenza, especially those who have a very low CD4+ cell count (indicating a highly suppressed immune system) or those who are not taking antiretrovirals.Citation37,Citation85,Citation86 Similarly, in a retrospective study, HIV patients with IMD were 5.3-times more likely to have CD4+ counts <0.2 × 109 cells/L than those without IMD.Citation84 In India, the adherence to antiretrovirals is low, as many people cannot access suitable clinics; in 2021, only 65% of Indians living with HIV were receiving treatment.Citation87 As a result, many people with HIV in India may be at high risk of severe influenza-related complications.
A recent report suggested that in India, 95% of deaths due to VPDs occur in adults,Citation88 however, India-specific data regarding burden of VPDs in IC populations remain limited. As vaccines are one of the most cost-effective health interventions available, the implementation of successful adult immunization programs is imperative, particularly for the most vulnerable adult populations.Citation17,Citation18,Citation46,Citation88
Vaccination in IC population
Vaccination among IC adults can reduce the incidence and severity of VPDs, as well as rate of VPD-related complications, subsequently limiting the socioeconomic burden and contributing to healthy aging.Citation74,Citation89 A systematic review assessing the cost-effectiveness of numerous adult vaccinations between 1980 and 2016 reported a favorable cost-effectiveness profile for most adult vaccinations when compared with no vaccinations. Cost savings and cost-effectiveness ratios of ≤$50,000 per quality-adjusted life years were reported for the influenza and pneumococcal vaccinations.Citation90 Several developed countries, including Australia, Germany and the UK have life-long immunization programs in place. Increased adult vaccination was shown to reduce the risk of hospitalization, hospitalization lengths and mortality.Citation74
Yet, adult vaccination in India is an overlooked and poorly communicated issue, leaving a large population of IC adults vulnerable to infection.Citation23 There are only few India-specific guidelines providing recommendations for adult immunization schedule that focus on IC populations.Citation88,Citation91,Citation92 Therefore, consultation of recommendations issued for other regions and countries is useful in order to gain a complete picture of immunization schedules for IC populations. Available vaccination guidelines vary between countries but agree on the need for specific prevention strategies for at-risk populations including people with IC conditions (). Whenever possible, vaccines should be administered prior to immunosuppression or administration should be delayed until immune recovery.Citation81 This is particularly relevant to individuals due to start immunosuppressive treatment when it is advised that inactivated vaccines should be given at least 2 weeks before the start of treatment onset.Citation93 In cancer patients not immunized prior to therapy, vaccination should occur at least 3 months after discontinuation of immunosuppressive therapy.Citation113
Table 3. Recommendations for vaccinations in adults with immunocompromising conditions provided by various guidelines across the world.Citation2,Citation12,Citation91–93,Citation94–112.
Even though vaccine effectiveness may be lower in IC patients compared with the general population, vaccination may still confer protection and reduce morbidity and mortality of VPD.Citation81 The immune response in severely immunocompromised individuals upon vaccination may be insufficient; re-immunization of individuals with inadequate immune response or vaccination of family members for indirect protection needs to be considered in these individuals.Citation2,Citation114 In cancer patients, the immunogenic response may vary widely, depending on the type of cancer, chemotherapeutic agents and underlying humoral response.Citation40 In general, most guidelines do not recommend the use of live attenuated vaccines (LAVs) in IC adults; however, in some patients who are not severely IC, LAVs may be considered ().Citation115 In India, there is a lack of comprehensive and nationally adopted vaccination guidelines for IC adults.Citation23 When vaccination guidelines do exist, they are often based on information issued by Western countries (e.g., US, UK), which does not always apply to the Indian population, which presents with different epidemiology and risk factors for VPDs.Citation23,Citation38
Discussion
IC populations in India are predicted to increase over the next decades due to a demographic shift toward older population, rapid urbanization combined with poor living standards and pollution.Citation15,Citation70 This shift is occurring at a faster pace than that observed in Western countries, which leaves little time for adaptation to new healthcare and socioeconomic challenges.Citation3
IC conditions combined with an increased risk of VPDs impose a high burden on patients and their families, as well as the healthcare sector. The burden of IC is not distributed uniformly in India. Some geographic regions and socio-economic strata have significantly higher prevalence rates compared with others. For example, cancer and HIV prevalence were highest in North and Northeast regions. In addition, low-income households bear a proportionally higher economic burden due to IC conditions compared with the middle- and high-income classes. Most of the disease burden due to IC conditions occur when people are in their peak working and earning years, thus affecting productivity and economic development.Citation116 Preventative measures, such as immunization programs, could reduce the burden of illness in IC adults, thereby minimizing the impact on working hours and the economy.
Mass immunization programs are effective strategies to lower the disease and economic burden of VPDs both at the individual level and from a health-economic perspective. Despite undoubted benefits of adult immunization, vaccination coverage remains suboptimal even in high-income countries. For example, the World Health Organization (WHO) target for influenza vaccination coverage was 75% among elderly populations by 2010 in Europe. This target was achieved by only one country (the Netherlands).Citation117 In the US, VPDs in adults still incur costs of $27 billion annually.Citation74 Barriers to vaccination include limited healthcare encounters, lack of specific recommendations and limited awareness of health benefits conferred by vaccination. An additional challenge in vaccinating people with IC conditions concerns the varying levels of altered immunocompetence. Individuals with a severe immunocompromised status may have an inadequate immunogenic response to vaccines; the level of altered immunocompetence should be determined prior to vaccination by the physician, rendering vaccination strategies even more complex.Citation2 In India, substantial economic inequalities and personal beliefs represent additional roadblocks to the deployment of effective adult immunization programs.
It has been reported that socioeconomic status is strongly correlated with vaccination status; in the richest areas of India, the vaccination coverage is indeed two times higher compared with the poorest areas.Citation118,Citation119 India’s universal immunization program covers eleven vaccines, but these are mainly for children and pregnant women.Citation120 Therefore, IC adults in India have to pay for their vaccinations themselves, which places a huge additional financial burden on the Indian population for whom the cost of IC treatment is already high; This acts as a significant barrier to the acceptance of vaccines.Citation121 A lack of education about the role of vaccination and concerns about vaccine efficacy and potential side effects are additional factors contributing to the poor rates of adult vaccination.Citation16,Citation122 In India, one survey reported that 68% of adults were not aware of the vaccines recommended for them and 38% of adults perceived immunization as being for children only.Citation23,Citation123
Cultural and religious factors also pose a barrier to vaccination among IC adults in India. Western biomedicine and indigenous medicine co-exist and adherence to either of these is distributed along a wide spectrum. Within some communities, there is little acceptance of Western medicine, including vaccinations.Citation124 However, if vaccine education is delivered in a culturally responsive and sensitive way, there is still the possibility to reach people in these communities. An excellent example of this was the involvement of religious leaders in garnering support for the polio vaccination, which contributed to India being declared polio-free in 2014 by the WHO.Citation124,Citation125 The COVID−19 pandemic has highlighted the urgent need to increase the coverage of adult vaccinations, particularly for the IC adult population. The success of the national COVID−19 immunization campaign could be harnessed to improve access to other adult vaccinations using existing infrastructure and expertise. Effective information campaigns, use of existing infrastructure from the universal immunization program and the development of a digital platform to register and book vaccination slots led to India having one of the highest Covid-19 vaccination coverage.Citation126
There are several limitations to this study. India-specific prevalence and incidence data of IC conditions are limited in the absence of nationwide disease-specific registries. Apart from HIV, for which nationwide screening programs have been instituted, IC conditions are likely underreported.Citation39 Data regarding risk factors and the economic burden of VPDs in IC populations in India are scarce and most of the information reported in this review are from studies carried out in North America and Europe. While some of the findings can be reasonably assumed to translate to the Indian context, others might not, due to epidemiological, genetic and socioeconomic differences. Further studies are needed to assess the economic impact of VPDs in a wider range of IC populations in India and to assess the benefit of adult vaccination programs.
Conclusion
IC populations in India pose an increasing challenge for the healthcare and social welfare system. Vaccines are one of the most cost-effective health interventions available and the implementation of successful adult immunization programs is imperative, particularly for the most vulnerable adult populations. A rapidly growing older population, inequalities in healthcare access and the absence of a public immunization program targeting the adult population complicate the task of providing nationwide immunization against VPDs. Following the COVID−19 pandemic, India has an unprecedented opportunity to leverage the infrastructure put in place for the COVID−19 vaccination campaign to provide nationwide immunization coverage against other VPDs.
Author contributions
All authors participated in the design or implementation or analysis, interpretation of the study, and the development of this manuscript. All authors had full access to the data and gave final approval before submission.
All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The work described was carried out in accordance with the recommendations of the International Committee of Medical Journal Editors for conduct, reporting, editing, and publication of scholarly work in medical journals.
Acknowledgments
The authors thank Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK. Katrin Spiegel, on behalf of GSK, provided medical writing support.
Disclosure statement
Peter San Martin is employed by GSK. Mark Doherty and Yashpal Chugh are employed by and hold shares in GSK. Peter San Martin, Yashpal Chugh and Mark Doherty declare no other financial and non-financial relationships and activities. Ashok Vaid and Neha Rastogi, declare no financial and non-financial relationships and activities and no conflicts of interest.
Data availability statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Additional information
Funding
References
- Memoli MJ, Athota R, Reed S, Czajkowski L, Bristol T, Proudfoot K, Hagey R, Voell J, Fiorentino C, Ademposi A, et al. The natural history of influenza infection in the severely immunocompromised vs nonimmunocompromised hosts. Clin Infect Dis. 2013;58(2):214–15. doi:10.1093/cid/cit725.
- Centers for Disease Control and Prevention. Altered Immunocompetence. Office of the associate director for communication, digital media branch, division of public affairs; 2018 Jun 26 [accessed 2021 Jan 20]. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/immunocompetence.html. Published 2020.
- National Institutes of Health. Why population aging matters: a global perspective. National Institute on Aging (Publication No. 07–6134). [accessed 2022 Feb 17]. https://www.nia.nih.gov/sites/default/files/2017-06/WPAM.pdf. Published 2007.
- McCusker C, Upton J, Warrington R. Primary immunodeficiency. Allergy Asthma Clin Immunol. 2018;14(Suppl 2):61. doi:10.1186/s13223-018-0290-5.
- Chinen J, Shearer WT. Secondary immunodeficiencies, including HIV infection. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S195–S203. doi:10.1016/j.jaci.2009.08.040.
- Doherty TM, Connolly MP, Del Giudice G, Flamaing J, Goronzy JJ, Grubeck-Loebenstein B, Lambert P-H, Maggi S, McElhaney JE, Nagai H, et al. Vaccination programs for older adults in an era of demographic change. Eur Geriatr Med. 2018;9(3):289–300. doi:10.1007/s41999-018-0040-8.
- Harpaz R, Dahl R, Dooling K. The prevalence of immunocompromised adults: United States, 2013. JAMA. 2016;316(23):2547–8. doi:10.1001/jama.2016.16477.
- Menon GR, Singh L, Sharma P, Yadav P, Sharma S, Kalaskar S, Singh H, Adinarayanan S, Joshua V, Kulothungan V. National burden estimates of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability data. Lancet Glob Health. 2019;7(12):e1675–e84. doi:10.1016/S2214-109X(19)30451-6.
- Institute for Health Metrics and Evaluation. GBD compare, Viz hub. IHME. [ accessed 2021 May 10]. https://vizhub.healthdata.org/gbd-compare/. Published 2019.
- Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. doi:10.1016/S0140-6736(18)32203-7.
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. doi:10.1016/S0140-6736(18)32279-7.
- Health and Safety Executive. Immunisations of immunocompromised persons. HSE National Immunisation Office. [accessed 2022 Feb 17]. https://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/chapter3.pdf. Published 2020.
- Ljungman P. Vaccination of immunocompromised patients. Clin Microbiol Infect. 2012;18(Suppl 5):93–9. doi:10.1111/j.1469-0691.2012.03971.x.
- Chen L, Han X, Li Y, Zhang C, Xing X. The severity and risk factors for mortality in immunocompromised adult patients hospitalized with influenza-related pneumonia. Ann Clin Microbiol Antimicrob. 2021;20(1):55. doi:10.1186/s12941-021-00462-7.
- Nethan S, Sinha D, Mehrotra R. Non communicable disease risk factors and their trends in India. Asian Pac J Cancer Prev. 2017;18(7):2005–10. doi:10.22034/APJCP.2017.18.7.2005.
- Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff T. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–6. doi:10.2471/BLT.07.040089.
- Doherty M, Schmidt-Ott R, Santos JI, Stanberry LR, Hofstetter AM, Rosenthal SL, Cunningham AL. Vaccination of special populations: protecting the vulnerable. Vaccine. 2016;34(52):6681–90. doi:10.1016/j.vaccine.2016.11.015.
- Philip RK, Attwell K, Breuer T, Di Pasquale A, Lopalco PL. Life-course immunization as a gateway to health. Expert Rev Vaccines. 2018;17(10):851–64. doi:10.1080/14760584.2018.1527690.
- Williams WW, Lu PJ, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al. Surveillance of vaccination coverage among adult populations - United States, 2014. Morb Mortal Wkly Rep Surveill Summ (Washington, DC: 2002). 2016;65(1):1–36. doi:10.15585/mmwr.ss6501a1.
- Perroud JM, Soldano S, Avancena ALV, Wagner A. Adult vaccination uptake strategies in low- and middle-income countries: a systematic review. Vaccine. 2022;40(36):5313–21. doi:10.1016/j.vaccine.2022.07.054.
- Bishwajit G, Ide S, Ghosh S. Social determinants of infectious diseases in South Asia. Int Sch Res Notices. 2014;2014:135243. doi:10.1155/2014/135243.
- Dandona L, Dandona R, Kumar GA, Shukla D, Paul VK, Balakrishnan K, Prabhakaran D, Tandon N, Salvi S, Dash A. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–60. doi:10.1016/S0140-6736(17)32804-0.
- Dash R, Agrawal A, Nagvekar V, Lele J, Di Pasquale A, Kolhapure S, Parikh R. Towards adult vaccination in India: a narrative literature review. Hum Vaccin Immunother. 2020;16(4):991–1001. doi:10.1080/21645515.2019.1682842.
- Vora A, Di Pasquale A, Kolhapure S, Agrawal A, Agrawal S. The need for vaccination in adults with chronic (noncommunicable) diseases in India - lessons from around the world. Hum Vaccin Immunother. 2022;18(5):2052544. doi:10.1080/21645515.2022.2052544.
- United Nations. UN DESA policy brief No. 153: India overtakes China as the world’s most populous country. [accessed 2023 May 1]. https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-no-153-india-overtakes-china-as-the-worlds-most-populous-country/. Published 2023.
- Agarwal A, Lubet A, Mitgang E, Mohanty S, Bloom DE. Population aging in India: facts, issues, and options. In: Population change and impacts in Asia and the Pacific. Singapore: Springer; 2020. p. 289–311. doi:10.1007/978-981-10-0230-4_13.
- Upadhyay RP. An overview of the burden of non-communicable diseases in India. Iran J Public Health. 2012;41(3):1–8. https://pubmed.ncbi.nlm.nih.gov/23113144. Published 2012 Mar 31.
- Institute for Health Metrics and Evaluation. Comprehensive health study in India finds rise of non-communicable diseases. Seattle (WA). [accessed 2021 Apr 19]. http://www.healthdata.org/news-release/comprehensive-health-study-india-finds-rise-non-communicable-diseases#:~:text=Injuries%20increased%20from%209%25%20of,disorders%2C%20and%20chronic%20kidney%20disease. Published 2017.
- Pandey A, Brauer M, Cropper ML, Balakrishnan K, Mathur P, Dey S, Turkgulu B, Kumar GA, Khare M, Beig G. Health and economic impact of air pollution in the states of India: the Global Burden of Disease Study 2019. Lancet Planet Health. 2021;5(1):e25–e38. doi:10.1016/S2542-5196(20)30298-9.
- Shrivastava U, Misra A, Mohan V, Unnikrishnan R, Bachani D. Obesity, diabetes and cardiovascular diseases in India: public health challenges. Curr Diabetes Rev. 2017;13(1):65–80. doi:10.2174/1573399812666160805153328.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. doi:10.3322/caac.21660.
- Global Burden of Disease Cancer C, Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD, Henrikson HJ, Lu D, Pennini A, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022;8(3):420–44. doi:10.1001/jamaoncol.2021.6987.
- Smith RD, Mallath MK. History of the growing burden of cancer in India: from antiquity to the 21st century. J Glob Oncol. 2019;5(5):1–15. doi:10.1200/jgo.19.00048.
- Kulothungan V, Sathishkumar K, Leburu S, Ramamoorthy T, Stephen S, Basavarajappa D, Tomy N, Mohan R, Menon GR, Mathur P. Burden of cancers in India - estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22(1):527. doi:10.1186/s12885-022-09578-1.
- Mathur P, Sathishkumar K, Chaturvedi M, Das P, Sudarshan K, Santhappan S, Nallasamy V, John A, Narasimhan S, Roselind F, et al. Cancer statistics, 2020: report from National Cancer Registry Programme, India. JCO Glob Oncol. 2020;6(6):1063–75. doi:10.1200/GO.20.00122.
- Zhang D, Petigara T, Yang X. Clinical and economic burden of pneumococcal disease in US adults aged 19-64 years with chronic or immunocompromising diseases: an observational database study. BMC Infect Dis. 2018;18(1):436. doi:10.1186/s12879-018-3326-z.
- Harish M, Ruhatiya RS. Influenza H1N1 infection in immunocompromised host: a concise review. Lung India. 2019;36(4):330–6. doi:10.4103/lungindia.lungindia_464_18.
- Chen L-K, Arai H, Chen L-Y, Chou M-Y, Djauzi S, Dong B, Kojima T, Kwon KT, Leong HN, Leung EMF, et al. Looking back to move forward: a twenty-year audit of herpes zoster in Asia-Pacific. BMC Infect Dis. 2017;17(1):213. doi:10.1186/s12879-017-2198-y.
- Patki A, Vora A, Parikh R, Kolhapure S, Agrawal A, Dash R. Herpes zoster in outpatient departments of healthcare centers in India: a review of literature. Hum Vaccin Immunother. 2021;17(11):4155–62. doi:10.1080/21645515.2021.1968737.
- Wong JL, Evans SE. Bacterial pneumonia in patients with cancer: novel risk factors and management. Clin Chest Med. 2017;38(2):263–77. doi:10.1016/j.ccm.2016.12.005.
- Rabello LS, Silva JR, Azevedo LC, Souza I, Torres VB, Rosolem MM, Lisboa T, Soares M, Salluh JI. Clinical outcomes and microbiological characteristics of severe pneumonia in cancer patients: a prospective cohort study. PLoS One. 2015;10(3):e0120544. doi:10.1371/journal.pone.0120544.
- Chemaly RF, Vigil KJ, Saad M, Vilar-Compte D, Cornejo-Juarez P, Perez-Jimenez C, Mubarak S, Salhab M, Jiang Y, Granwehr B, et al. A multicenter study of pandemic influenza a (H1N1) infection in patients with solid tumors in 3 countries. Cancer. 2012;118(18):4627–33. doi:10.1002/cncr.27447.
- Taha M-K, Weil-Olivier C, Bouée S, Emery C, Nachbaur G, Pribil C, Loncle-Provot V. Risk factors for invasive meningococcal disease: a retrospective analysis of the French national public health insurance database. Hum Vaccin Immunother. 2021;17(6):1858–66. doi:10.1080/21645515.2020.1849518.
- Guzek A, Berghoff AS, Jasinska J, Garner-Spitzer E, Wagner A, Stiasny K, Holzmann H, Kundi M, Zielinski C, Wiedermann U. Reduced seroprevalence against vaccine preventable diseases (VPDs) in adult patients with cancer: necessity of routine vaccination as part of the therapeutic concept. Ann Oncol. 2020;31(2):319–21. doi:10.1016/j.annonc.2019.11.005.
- Zhang X, Zhu X, Ji Y, Li H, Hou F, Xiao C, Yuan P. Increased risk of hepatitis B virus infection amongst individuals with diabetes mellitus. Biosci Rep. 2019;39(3):BSR20181715. doi:10.1042/BSR20181715.
- Kesavadev J, Misra A, Das AK, Saboo B, Basu D, Thomas N, Joshi SR, Unnikrishnan AG, Shankar A, Krishnan G, et al. Suggested use of vaccines in diabetes. Indian J Endocrinol Metab. 2012;16(6):886–93. doi:10.4103/2230-8210.102982.
- Garrouste-Orgeas M, Azoulay E, Ruckly S, Schwebel C, de Montmollin E, Bedos J-P, Souweine B, Marcotte G, Adrie C, Goldgran-Toledano D, et al. Diabetes was the only comorbid condition associated with mortality of invasive pneumococcal infection in ICU patients: a multicenter observational study from the Outcomerea research group. Infection. 2018;46(5):669–77. doi:10.1007/s15010-018-1169-6.
- Ishigami J, Sang Y, Grams M, Coresh J, Chang A, Matsushita K. Effectiveness of Influenza vaccination among older adults across kidney function: pooled analysis of 2005-2006 through 2014-2015 influenza seasons. Am J Kidney Dis. 2020;75(6):887–96. doi:10.1053/j.ajkd.2019.09.008.
- Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11(3):229. doi:10.1186/ar2669.
- Trinh Q, Nguyen H, Nguyen V, Nguyen T, Sintchenko V, Marais B. Tuberculosis and HIV co-infection—focus on the Asia-Pacific region. Int J Infect Dis. 2015;32:170–8. doi:10.1016/j.ijid.2014.11.023.
- Platt L, French CE, McGowan CR, Sabin K, Gower E, Trickey A, McDonald B, Ong J, Stone J, Easterbrook P, et al. Prevalence and burden of HBV co-infection among people living with HIV: a global systematic review and meta-analysis. J Viral Hepat. 2020;27(3):294–315. doi:10.1111/jvh.13217.
- Kim YC, Ahn JY, Kim JM, Kim YJ, Park DW, Yoon YK, Song JY, Kim SW, Lee JS, Choi BY. Human immunodeficiency virus (HIV) and hepatitis virus coinfection among HIV-infected Korean patients: the Korea HIV/AIDS cohort study. Infect Chemother. 2017;49(4):268–74. doi:10.3947/ic.2017.49.4.268.
- Rolston KVI. Infections in cancer patients with solid tumors: a review. Infect Dis Ther. 2017;6(1):69–83. doi:10.1007/s40121-017-0146-1.
- Chopra A. Disease burden of rheumatic diseases in India: COPCORD perspective. Ind J Rheumatol. 2015;10(2):70–7. doi:10.1016/j.injr.2015.04.002.
- Fatoye F, Gebrye T, Mbada C. Global and regional prevalence and incidence of systemic lupus erythematosus in low-and-middle income countries: a systematic review and meta-analysis. Rheumatol Int. 2022;42(12):2097–107. doi:10.1007/s00296-022-05183-4.
- Misra DP, Agarwal V, Negi VS. Rheumatology in India: a bird’s eye view on organization, epidemiology, training programs and publications. J Korean Med Sci. 2016;31(7):1013–19. doi:10.3346/jkms.2016.31.7.1013.
- Shroff S. Current trends in kidney transplantation in India. Indian J Urol. 2016;32(3):173–4. doi:10.4103/0970-1591.185092.
- Kulkarni U, George B. Access to hematopoietic stem-cell transplantation in India. J Postgrad Med. 2019;65(1):1–4. doi:10.4103/jpgm.JPGM_391_18.
- Varma PP. Prevalence of chronic kidney disease in India - where are we heading? Indian J Nephrol. 2015;25(3):133–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4446915/.
- Varughese S, Abraham G. Chronic kidney disease in India: a clarion call for change. Clin J Am Soc Nephrol. 2018;13(5):802–4. doi:10.2215/CJN.09180817.
- Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442–9. doi:10.2174/1573399815666191024085838.
- Huissoon AP, Krishna MT. Does this patient have an immunodeficiency? Clin Med (Lond). 2011;11(4):380–4. doi:10.7861/clinmedicine.11-4-380.
- UNAIDS. Global HIV & AIDS statistics - 2020 fact sheet. [accessed 2021 Jan 20]. https://www.unaids.org/en/resources/fact-sheet. Published 2020.
- Joshi RK, Mehendale SM. Determinants of consistently high HIV prevalence in Indian districts: a multi-level analysis. PLoS One. 2019;14(5):e0216321. doi:10.1371/journal.pone.0216321.
- National Aids Control Organisation (NACO). HIV facts and figures. [accessed 2022 Sep 21]. http://naco.gov.in/sites/default/files/Facts_figure_page.pdf. Published 2019.
- Paranjape RS, Challacombe SJ. HIV/AIDS in India: an overview of the Indian epidemic. Oral Dis. 2016;22(Suppl 1):10–14. doi:10.1111/odi.12457.
- Frank TD, Carter A, Jahagirdar D, Biehl MH, Douwes-Schultz D, Larson SL, Arora M, Dwyer-Lindgren L, Steuben KM, Abbastabar H, et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, injuries, and risk factors study 2017. Lancet HIV. 2019;6(12):e831–e59. doi:10.1016/s2352-3018(19)30196-1.
- Sahu D, Kumar P, Chandra N, Rajan S, Shukla DK, Venkatesh S, Nair S, Kumar A, Singh J, Reddy S, et al. Findings from the 2017 HIV estimation round & trend analysis of key indicators 2010-2017: evidence for prioritising HIV/AIDS programme in India. Indian J Med Res. 2020;151(6):562–70. doi:10.4103/ijmr.IJMR_1619_19.
- Mallath MK, Taylor DG, Badwe RA, Rath GK, Shanta V, Pramesh CS, Digumarti R, Sebastian P, Borthakur BB, Kalwar A, et al. The growing burden of cancer in India: epidemiology and social context. Lancet Oncol. 2014;15(6):e205–e12. doi:10.1016/s1470-2045(14)70115-9.
- Sinha R, Pati S. Addressing the escalating burden of chronic diseases in India: need for strenthening primary care. J Family Med Prim Care. 2017;6(4):701–8. doi:10.4103/jfmpc.jfmpc_1_17.
- Das S, Mukhopadhyay A, Ray T. Economic Cost of HIV and AIDS in India. HIV and AIDS in South Asia; 2009. p. 123–154.
- Duraisamy P, Ganesh AK, Homan R, Kumarasamy N, Castle C, Sripriya P, Mahendra V, Solomon S. Costs and financial burden of care and support services to PLHA and households in South India. AIDS Care. 2006;18(2):121–7. doi:10.1080/09540120500159359.
- National portal of India. Ayushman Bharat - national health protection mission. [accessed 2022 Dec 1]. https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission. Published 2018.
- Kolobova I, Nyaku MK, Karakusevic A, Bridge D, Fotheringham I, O’Brien M. Burden of vaccine-preventable diseases among at-risk adult populations in the US. Hum Vaccin Immunother. 2022;18(5):2054602. doi:10.1080/21645515.2022.2054602.
- Li Q, Chen SY, Burstin SJ, Levin MJ, Suaya JA. Cost of herpes zoster in patients with selected immune-compromised conditions in the United States. Open Forum Infect Dis. 2016;3(2):ofw067. doi:10.1093/ofid/ofw067.
- Weycker D, Farkouh RA, Strutton DR, Edelsberg J, Shea KM, Pelton SI. Rates and costs of invasive pneumococcal disease and pneumonia in persons with underlying medical conditions. BMC Health Serv Res. 2016;16(1):182. doi:10.1186/s12913-016-1432-4.
- Yanni EA, Ferreira G, Guennec M, El Hahi Y, El Ghachi A, Haguinet F, Espie E, Bianco V. Burden of herpes zoster in 16 selected immunocompromised populations in England: a cohort study in the clinical practice research datalink 2000–2012. BMJ Open. 2018;8(6):e020528. doi:10.1136/bmjopen-2017-020528.
- Dutta AK, Swaminathan S, Abitbol V, Kolhapure S, Sathyanarayanan S. A comprehensive review of meningococcal disease burden in India. Infect Dis Ther. 2020;9(3):537–59. doi:10.1007/s40121-020-00323-4.
- Ghia CJ, Rambhad GS. Meningococcal disease burden in India: a systematic review and meta-analysis. Microbiol Insights. 2021;14:11786361211053344. doi:10.1177/11786361211053344.
- John TJ, Gupta S, Chitkara AJ, Dutta AK, Borrow R. An overview of meningococcal disease in India: knowledge gaps and potential solutions. Vaccine. 2013;31(25):2731–7. doi:10.1016/j.vaccine.2013.04.003.
- Shah M, Kamboj M. Immunizing cancer patients: which patients? Which vaccines? When to give? [accessed 2022 Nov 8]. https://www.cancernetwork.com/view/immunizing-cancer-patients-which-patients-which-vaccines-when-give. Published 2018.
- Molander V, Elisson C, Balaji V, Backhaus E, John J, Vargheese R, Jayaraman R, Andersson R. Invasive pneumococcal infections in Vellore, India: clinical characteristics and distribution of serotypes. BMC Infect Dis. 2013;13(1):532. doi:10.1186/1471-2334-13-532.
- Centers for Disease Control and Prevention. Hepatitis A questions and answers for the public. Office of the associate director for communication, digital media branch, division of public affairs. 2018 Jun 26 [accessed 2021 Jun 26]. https://www.cdc.gov/hepatitis/hav/afaq.htm. Published 2020.
- Miller L, Arakaki L, Ramautar A, Bodach S, Braunstein S, Kennedy J, Steiner-Sichel L, Ngai S, Shepard C, Weiss D. Elevated risk for invasive meningococcal disease among persons with HIV. Ann Intern Med. 2014;160(1):30–7. doi:10.7326/0003-4819-160-1-201401070-00731.
- Crum-Cianflone NF, Wallace MR. Vaccination in HIV-infected adults. AIDS Patient Care STDS. 2014;28(8):397–410. doi:10.1089/apc.2014.0121.
- von Mollendorf C, Hellferscee O, Valley-Omar Z, Treurnicht FK, Walaza S, Martinson NA, Lebina L, Mothlaoleng K, Mahlase G, Variava E, et al. Influenza viral shedding in a prospective cohort of HIV-infected and uninfected children and adults in 2 provinces of South Africa, 2012–2014. J Infect Dis. 2018;218(8):1228–37. doi:10.1093/infdis/jiy310.
- Be in the Know. At a glance: HIV in India. Brighton; [accessed 2022 May 10]. https://www.beintheknow.org/understanding-hiv-epidemic/data/glance-hiv-india. Published 2021.
- Rathi A, Sharma S. Vaccine preventable diseases in Indian adults-burden & prevention. Infect Dis Diag Treat. 2017;J102. Accessed ** The authors the obstacles and opportunities of for vaccination in India.
- Roush SW, Murphy TV. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298(18):2155–63. doi:10.1001/jama.298.18.2155.
- Leidner AJ, Murthy N, Chesson HW, Biggerstaff M, Stoecker C, Harris AM, Acosta A, Dooling K, Bridges CB. Cost-effectiveness of adult vaccinations: a systematic review. Vaccine. 2019;37(2):226–34. doi:10.1016/j.vaccine.2018.11.056.
- Dhar R, Ghoshal AG, Guleria R, Sharma S, Kulkarni T, Swarnakar R, Samaria J, Chaudhary S, Gaur S, Christopher D et al. Clinical practice guidelines 2019: Indian consensus-based recommendations on influenza vaccination in adults. Lung India. 2020;37(Supplement):S4–S18. doi:10.4103/lungindia.lungindia_270_20.
- Indian Medical Association. Life course immunization guidebook. A quick reference guide https://www.ima-india.org/ima/pdfdata/IMA_LifeCourse_Immunization_Guide_2018_DEC21.pdf. 2019.
- Public Health England. Immunisation of individuals with underlying medical conditions. The Stationery Office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/857279/Greenbook_chapter_7_Immunsing_immunosupressed.pdf. Published 2020.
- Centers for Disease Control and Prevention. Chickenpox (varicella). Office of the associate director for communication, digital media branch, division of public affairs. 2018 Jun 26 [accessed 2021 May 10]. https://www.cdc.gov/chickenpox/hcp/index.html#:~:text=Immunocompromised%20people%20who%20get%20varicella,encephalitis%2C%20and%20disseminated%20intravascular%20coagulopathy. Published 2018.
- Centers for Disease Control and Prevention. Diabetes type 1 and type 2 and adult vaccination. Office of the associate director for communication, digital media branch, division of public affairs. 2018 [accessed 2021 May 10]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/diabetes.html. Published 2016.
- Centers for Disease Control and Prevention. HIV infection and adult vaccination. Office of the associate director for communication, digital media branch, division of public affairs. 2018 Jun 26. Recommended Vaccines for Adults Web site. [accessed 2021 Jun 26]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/hiv.html. Published 2016.
- Centers for Disease Control and Prevention. Renal Disease and Adult Vaccination. Office of the associate director for communication, digital media branch, division of public affairs. 2018 Jun 26 [accessed 2021 Jul]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/renal-disease.html. Published 2016.
- Centers for Disease Control and Prevention. Weakened Immune System and Adult Vaccination. Office of the associate director for communication, digital media branch, division of public affairs. 2018 Jun 26 [accessed 2021 May 10]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/weakened-immune.html. Published 2016.
- Expert Group of the Association of Physicians of India on Adult Immunization in India. The association of physicians of India evidence-based clinical practice guidelines on adult immunization. J Assoc Physicians India. 2009;57:345–56.
- World Health Organization. Human papillomavirus vaccines: WHO position paper, December 2022. Vaccine. 2022;50(97):645–72. https://www.who.int/publications/i/item/who-wer9750-645-672.
- World Health Organization. Measles vaccines:WHO position paper, April 2017–recommendations. Vaccine. 2019;37(2):219–22. doi:10.1016/j.vaccine.2017.07.066.
- World Health Organization. Pneumococcal vaccines: WHO position paper—2012. Wkly Epidemiol Rec. 2012;87(14):129–44.
- World Health Organization. Tetanus vaccines: WHO position paper, February 2017–recommendations. Vaccine. 2018;36(25):3573–5. doi:10.1016/j.vaccine.2017.02.034.
- World Health Organization. Hepatitis B vaccines: WHO position paper, July 2017–Recommendations. Vaccine. 2019;37(2):223–5. doi:10.1016/j.vaccine.2017.07.046.
- World Health Organization. Vaccines against influenza WHO position paper—November 2012. Wkly Epidemiol Rec. 2012;87(47):461–76.
- Public Health England. Pneumococcal. The stationery office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/857267/GB_Chapter_25_pneumococcal_January_2020.pdf. Published 2020.
- Public Health England. Shingles (herpes zoster). The Stationery Office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1012943/Green_book_of_immunisation_28a_Shingles.pdf. Published 2021.
- Public Health England. Human papillomavirus (HPV). The Stationery Office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/828868/Greenbook_chapter_18a.pdf. Published 2019.
- Public Health England. Measles. The Stationery Office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/855154/Greenbook_chapter_21_Measles_December_2019.pdf. Published 2019.
- Public Health England. Varicella. The Stationery Office. [accessed 2022 Feb 17]. https://www.gov.uk/government/publications/varicella-the-green-book-chapter-34. Published 2019.
- Public Health England. Hepatitis B. The Stationery Office. [accessed 2022 Feb 17]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/628602/Greenbook_chapter__18.pdf. Published 2017.
- Centers for Disease Control and Prevention. HPV vaccination recommendations. Vaccines and preventable diseases web site. [accessed 2021 May 10]. https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html. Published 2021.
- Ariza-Heredia EJ, Chemaly RF. Practical review of immunizations in adult patients with cancer. Hum Vaccin Immunother. 2015;11(11):2606–14. doi:10.1080/21645515.2015.1062189.
- Woodfield MC, Pergam SA, Shah PD. Cocooning against COVID-19: the argument for vaccinating caregivers of patients with cancer. Cancer. 2021;127(16):2861–3. doi:10.1002/cncr.33598.
- Varghese L, Curran D, Bunge E, Vroling H, van Kessel F, Guignard A, Casabona G, Olivieri A. Contraindication of live vaccines in immunocompromised patients: an estimate of the number of affected people in the USA and the UK. Public Health. 2017;142:46–9. doi:10.1016/j.puhe.2016.10.013.
- Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328(7443):807–10. doi:10.1136/bmj.328.7443.807.
- World Health Organization. Evaluation of seasonal influenza vaccination policies and coverage in the WHO European Region: results from the 2008/2009 and 2009/2010 influenza seasons. WHO Regional Office for Europe. [accessed 2022 Feb 17]. https://apps.who.int/iris/handle/10665/350536. Published 2014.
- Dhillon PK, Jeemon P, Arora NK, Mathur P, Maskey M, Sukirna RD, Prabhakaran D. Status of epidemiology in the WHO South-East Asia region: burden of disease, determinants of health and epidemiological research, workforce and training capacity. Int J Epidemiol. 2012;41(3):847–60. doi:10.1093/ije/dys046.
- Limaye D, Limaye V, Fortwengel G. A study to assess the vaccination coverage of university students in Mumbai, India. IJPSR. 2017;8(6):2667–76.
- Ministry of Health and Family Welfare. Universal Immunization Programme (UIP). Ministry of health and family welfare. [accessed 2021 Feb 17]. https://main.mohfw.gov.in/sites/default/files/Universal.pdf. Published 2023.
- Ghungrud D, Sharma R. Awareness on vaccinations among chronic kidney disease patients in rural India. IJCRR. 2020;12(21):56–63. doi:10.31782/IJCRR.2020.12213.
- Isahak I. Adult immunization–a neglected issue in Southeast Asia. Southeast Asian J Trop Med Public Health. 2000;31(1):173–84. Published 2000 Oct 7.
- Pharmabiz. New survey finds adult vaccination knowledge gaps in India. Saffron Media Private Limited. [accessed 2021 Mar 3]. http://pharmabiz.com/NewsDetails.aspx?aid=105384&sid=2. Published 2017.
- Salim F. Culture, politics, and religion: exploring resistance to vaccinations in South Asia. Human Welfare. 2012;1(1):91–103.
- Bahl S, Kumar R, Menabde N, Thapa A, McFarland J, Swezy V, Tangermann RH, Jafari HS, Elsner L, Wassilak SGF, et al. Polio-free certification and lessons learned–South-East Asia region, March 2014. Morb Mortal Wkly Rep. 2014;63(42):941–6. https://pubmed.ncbi.nlm.nih.gov/25340910.
- Singh K, Verma A, Lakshminarayan M. India’s efforts to achieve 1.5 billion COVID-19 vaccinations: a narrative review. Osong Public Health Res Perspect. 2022;13(5):316–27. doi:10.24171/j.phrp.2022.0104.