ABSTRACT
Vaccine hesitancy has become a threat to public health, especially as it is a phenomenon that has also been observed among healthcare professionals. In this study, we analyzed the relationship between endorsement of complementary and alternative medicine (CAM) and vaccination attitudes and behaviors among healthcare professionals, using a cross-sectional sample of physicians with vaccination responsibilities from four European countries: Germany, Finland, Portugal, and France (total N = 2,787). Our results suggest that, in all the participating countries, CAM endorsement is associated with lower frequency of vaccine recommendation, lower self-vaccination rates, and being more open to patients delaying vaccination, with these relationships being mediated by distrust in vaccines. A latent profile analysis revealed that a profile characterized by higher-than-average CAM endorsement and lower-than-average confidence and recommendation of vaccines occurs, to some degree, among 19% of the total sample, although these percentages varied from one country to another: 23.72% in Germany, 17.83% in France, 9.77% in Finland, and 5.86% in Portugal. These results constitute a call to consider health care professionals’ attitudes toward CAM as a factor that could hinder the implementation of immunization campaigns.
Even though vaccinations are one of the most beneficial medical advances in human history, they have been subject to controversy since the first mass vaccination campaigns—e.g., the numerous anti-vaccination leagues that emerged in the U.S. during the last quarter of the 19th century.Citation1,Citation2 Vaccine hesitancy is a complex phenomenon that encompasses various types and degrees of negative attitudes and behaviors—e.g., outright rejection, delay, or reluctant acceptance of vaccination.Citation3 There are several sources of vaccine hesitancy among the general population, such as complacency, distrust, and conspiracy beliefs,Citation4 which vary depending on the socio-political context and the type of vaccination. For example, complacency (i.e., unwillingness to get vaccinated due to low perceived risk of vaccine-preventable diseases) is particularly salient in relation to the influenza vaccine,Citation5 whereas conspiracy beliefs and science-related populism tend to manifest during threatening and politically charged events, such as the COVID-19 pandemic.Citation6,Citation7 Numerous studies have also observed vaccine hesitant attitudes among health care professionals (HCPs), which are reflected in lower rates of self-vaccination and vaccine recommendation to patients.Citation8
Prior studies among the general population and nurses suggest that complementary and alternative medicine (CAM) is positively related to vaccine hesitancy.Citation9–14 CAM is defined by the World Health Organization as “a broad set of health care practices that are not part of that country’s own traditional or conventional medicine and are not fully integrated into the dominant health care system”Citation15—in Western societies: homeopathy, acupuncture, energy and crystal healing, reflexology, magnet therapy, or anthroposophic medicine.Citation16–18 Due to its potential effect on willingness to recommend and receive vaccines, the analysis of the relationship between vaccine hesitancy and CAM endorsement among physicians is particularly relevant due to their direct contact with the general public and vulnerable populations, as well as to their key role in patients’ vaccine-related decision-making processes.Citation19,Citation20
CAM endorsement and vaccine hesitancy
Despite studies reflecting physicians’ general dissatisfaction with the state of knowledge and research about CAM,Citation21,Citation22 a literature review of 21 survey-based studies in Canada and the U.S. found that a substantial number of HCPs express positive attitudes toward CAM and recommend, or would consider recommending, CAM to their patients—e.g., between 6% and 80% used CAM in their clinical practice, with these results varying depending on the definition of CAM and sampling methods used in the study.Citation23 In fact, one systematic review suggested that HCPs are equally, or even more likely, than the general population to use CAM.Citation24 Another systematic review, this time of surveys with British physicians, found that the mean prevalence of personal use of CAM among physicians was 20.6%, with an average referral rate to CAM of 39%, even though only 10.3% of these physicians had received specific training in CAM.Citation25 Other studies conducted in European countries show a similar scenario. For example, in the study by Berretta et al.Citation26 55% of the sample of Italian physicians recommended CAM to their patients, whereas in the German sample analyzed in the study by Linde et al.Citation27 23% of family physicians, 6% of internists, and 31% of orthopedist personally used four or more forms of CAM frequently, and 68% reported using homeopathy to treat patients.
The link between CAM endorsement and negative attitudes toward vaccines has been documented in previous research among the general public. A systematic review, which categorized arguments against vaccines retrieved from peer-reviewed articles and debunking texts published by international fact checking agencies, identified a category of arguments largely based on alternative health beliefs related to CAM.Citation28 This category was the third most common in the scientific and fact-checking literature. Furthermore, anti-vaccination arguments related to CAM were also among the most endorsed arguments by individuals from the British general population in a study by Holford et al.Citation29 These results suggest that CAM beliefs play an important role in individuals’ justification of their hesitant attitudes toward vaccines for both adults and children.Citation30 Bryden et al.,Citation31 Soveri et al.,Citation12 Lewandowsky et al.,Citation11 and Hornsey et al.Citation10 analyzed samples from the Australian, Finnish, American, and Spanish general populations and found that positive attitudes toward CAM were related to negative attitudes toward vaccines. In a recent large-scale study in 18 European countries, parental consultation with homeopaths was associated with higher vaccine hesitancy than consultation with pediatricians or nurses.Citation32 Moreover, in a systematic review, Wardle et al.Citation33 found that CAM use tended to be positively associated with lower childhood immunization – see the work by Bleser et al.Citation34 and Frawley et al.Citation35 for more recent results from the U.S. and Australia.
Overview of the present study
We report an unprecedent quantitative examination of the link between CAM endorsement and vaccine-related attitudes and behaviors among HCPs from four European countries (France, Portugal, Finland, and Germany). Given that a substantial number of HCPs use and prescribe CAM, and there is a known positive link between CAM and vaccine hesitancy in the general population, we hypothesized that:
H1:
CAM endorsement among medical practitioners with vaccination responsibilities will predict negative vaccination attitudes and behaviors.
Following the well-established theory of planned behavior, according to which behaviors are influenced by previous attitudes in a process of sense-making,Citation36 we also hypothesized that negative attitudes toward vaccines associated with CAM endorsement would constitute a motivational context in which physicians’ willingness to recommend and receive vaccinations is reduced:
H2:
Attitudes toward vaccines will mediate the relationship between CAM endorsement and vaccine-related behaviors.
Methods
Sample
In Germany, GPs, pediatricians, and gynecologists were recruited between 03/31/2022 and 04/24/2022 via Schlesinger Group Germany. In Portugal, GPs and pediatricians were recruited between 04/06/2022 and 05/06/2022 through invitations sent to the mailing list of the Portuguese Society of Pediatricians and the Portuguese Association of General Practice and Family Medicine. In France, GPs were recruited between 03/18/2022 and 04/27/2022 through invitations sent to the mailing list of National Association of General Practitioners. Finally, in Finland, GPs and pediatricians were recruited between 04/25/2022 and 05/16/2022 through invitations sent to the mailing list of the Finnish Medical Association. We received responses from 2,875 physicians, of which 88 were excluded due to missing values on one or more variables of interest, thus resulting in a final sample of 2,787 participants.
Measures
All the sociodemographic questions and scales used in this study were adapted to the context of each country by the research team, and then translated and back-translated by professional translators.
CAM endorsement
Participants’ attitudes toward CAM were assessed using a 5-item scale measuring CAM rejection developed by Lewandowsky et al.Citation11 with 2 items taken from Hyland et al.Citation37 The polarity of the scores of the first and third items was reversed for analysis such that higher mean scores indicate endorsement of CAM practices. Sample items: “complementary medicine builds up the body’s own defenses, so leading to a permanent cure” and “complementary medicine is superior to conventional medicine in treating chronic ailments such as allergies, headaches, and back pains”. Confirmatory factor analysis of the one-factor model used in previous studies,Citation11,Citation14 including a residual correlation between items 1 and 3, resulted in adequate fit indices (χ2 (4) = 15.328, p > .01; CFI = 0.99, TLI = 1; RMSEA = 0.03 (CI: 0.016–0.050); SRMR = 0.01), with all the factor loadings above 0.30.
Vaccine-related attitudes
We administered the international version of the Professionals Vaccine Confidence and Behaviors Questionnaire (I-Pro-VC-Be). All the four country-specific adaptations of the I-Pro-VC-Be used in this study have been previously validated for use in those countries,Citation38 and are composed of 33 items to measure psychosocial determinants of HCPs’ attitudes toward vaccines. Following previous work by Verger et al.Citation39 the items of the I-Pro-VC-Be were grouped into six constructs:
Confidence in Vaccines, composed of items reflecting perceived risks of vaccines (i.e., how safe HCPs perceive certain vaccines to be), complacency (i.e., the perception of lack of usefulness of vaccines), perceived benefit-risk balance of vaccines (i.e., the degree to which HCPs perceive that the benefits of vaccines outweigh their potential risks), and perceived collective responsibility (i.e., the extent to which HCPs recommend vaccines to contribute to community immunity). Sample items: “vaccines against human papillomaviruses are safe” and “the benefits of the vaccine against measles outweigh its potential risks.”
Trust in Authorities (i.e., trust in institutions and health authorities to provide reliable vaccine information and to define the vaccination strategy). Sample items: “I trust the information provided by the [relevant national institution] about the risks and benefits of vaccines” and “I trust the [relevant national institution] to establish the vaccination strategy.”
Perceived Constraints (i.e., perceived practical constraints, such as cost of or access to vaccines). Sample items: “the cost of some vaccines is a problem for some patients and can keep me from prescribing them” and “the lack of availability of certain vaccines in my country is sometimes a problem that can keep me from prescribing them to my patients.”
Proactive Efficacy, composed of items reflecting commitment to vaccination (i.e., the extent to which HCPs are proactive in motivating their patients to accept vaccinations) and self-efficacy (i.e., how prepared HCPs feel in terms of knowledge and skills to address vaccination with patients). Sample items: “I am committed to developing the skills needed to communicate better with my patients about vaccination” and “I feel comfortable discussing vaccines with my patients who are highly hesitant about vaccination.”
Reluctant Trust (i.e., the “leap of faith” to trust vaccines and policies even if HCPs have doubts). Sample items: “I may sometimes recommend vaccines from the official schedule even if I feel I am not sufficiently informed” and “I may sometimes recommend the vaccines on the official schedule even in cases where I have doubts about their safety.”
Openness to patients. These items express positive attitudes toward hesitant patients, such as viewing their concerns regarding vaccination as legitimate, letting patients to delay the immunization of children, and a neutral approach to informing patients about the benefits of vaccines. Sample items: “patients who are hesitant about the benefits and risks of vaccines have legitimate questions” and “I am open to patients delaying immunization of their children.”
Vaccine-related behaviors
Following precedents in previous studies,Citation38,Citation39 we used three variables to assess participants’ vaccine-related behaviors:
Vaccine Recommendation (i.e., HCPs’ tendency to recommend vaccines to their patients). Participants indicated how often they recommend seven vaccines included in the immunization plans of their respective countries to patients without contraindications (e.g., “when you treat adults who have not had the COVID-19 vaccine, what is the percentage of these patients for whom you actively recommend the vaccine?”). The option “I do not treat patients within this age/target group” was available. If participants chose this option, they were asked to answer the question as if they were in the given situation and to state their intention to recommend the given vaccine to the given target group (e.g., “please imagine you are treating an adult who has not had the COVID-19 vaccine and has no contraindications. How likely is it that you would recommend the vaccine to the patient?”). Both questions were merged to obtain a measure of vaccine recommendation frequency and intention for each type of vaccine, and then a total mean across all types of vaccines was calculated.
Self-Vaccination (i.e., HCPs’ personal vaccine uptake). We asked HCPs about their vaccination status against COVID-19 and influenza during the previous three years.
General Vaccination Behavior: These questions reflect behaviors included in the usual protocols of practitioners, such as how often HCPs check the vaccination status of their patients, bring up the subject of vaccination, and recommend the indicated vaccines. Sample items: “how often do you check that your patients have received the vaccines recommended for them (whether from records or asking)?” and “how often do you bring up the subject of vaccination?.”
The HCPs’ responses were averaged within each construct to create a single variable representing each construct. The psychometric characteristics, internal consistency, and descriptive statistics of the scales used in the study are displayed in . Analogous tables for each country are available in Supplementary Material.
Table 1. Psychometric characteristics, internal consistency, and descriptive statistics of the variables included in the study.
Results
Sociodemographic characteristics of the sample
The sociodemographic characteristics of the general sample are reported in . The majority of the participating physicians had vaccination responsibilities and were GPs or pediatricians. Most physicians had children and were French, whereas the Finnish physicians were the least represented in the sample. Age and gender distributions were balanced.
Table 2. Sociodemographic characteristics of the sample.
Sociodemographic differences in CAM endorsement
Sociodemographic differences regarding country, age, gender, children, and profession in CAM endorsement were analyzed with a series of independent-samples t-tests and one-way between-subjects ANOVAs. Given our sample size (N = 2,787), our data would be sufficient to reliably detect small effects of d = 0.13 and F = 0.06, with 80% power (α = 0.05, two-tailed). Variable means and standard deviations are displayed in . The results showed that there were statistically significant differences in CAM endorsement between countries, age groups, and professions, however not between genders nor households with or without children. CAM endorsement was lowest in Finland and highest in Germany. CAM endorsement was also highest in the oldest age group (>50) and lowest in the youngest (<40) age group. CAM endorsement was lowest among pediatricians and highest among gynecologists – however, it is worth noting that, in this case, country may be acting as a confounder as only the German sample included gynecologists. Follow-up and country-specific analyses assessing these sociodemographic differences can be found in Supplementary Material.
First hypothesis: predictive power of CAM endorsement for vaccine-related attitudes and behaviors
To assess the predictive power of CAM endorsement for vaccine-related attitudes and behaviors, we conducted linear mixed effects model analyses in R (v. 4.2.2) using the lme4 package,Citation40 as well as the lmerTest package to calculate the statistical significance of effects,Citation41 and the performance package to obtain model fit, VIF, and tolerance statistics.Citation42 There are currently no agreed standards for conducting sensitivity and post-hoc power analyses for linear mixed effect models, since this is a developing area. However, our large sample of 2,787 participants is sensitive to detecting very small effects in both the ANOVAs (reported in the previous section) and the linear regressions (reported in Supplementary Material), which gives confidence that it is sufficiently powered to reliably detect the observed effect sizes in the mixed effect models as well. We ran separate models for nine outcome variables (Confidence in Vaccines, Proactive Efficacy, Trust in Authorities, Reluctant Trust, Perceived Constraints, General Recommendation Behavior, Vaccine Recommendation, Self-Vaccination, and Openness to Patients), with CAM Endorsement and the sociodemographic variables age, gender, children, and profession as the independent variables, and country as a random intercept. These results are displayed in and support our hypothesis that CAM endorsement among medical practitioners with vaccination responsibilities predicts negative vaccination attitudes and behaviors, although we did not find an association with General Recommendation Behavior. Model specifications and analogous country-specific analyses can be found in Supplementary Material.
Table 3. Linear mixed effect models with CAM endorsement and sociodemographic variables as independent variables, country as a random intercept, and vaccine-related attitudes and behaviors as dependent variables.
Second hypothesis: mediational models between CAM endorsement and vaccine-related behaviors
In order to assess the role of vaccine attitudes in the relationship between CAM Endorsement and the two vaccine-related behaviors negatively predicted by CAM Endorsement in the linear mixed effects models (i.e., Vaccine Recommendation and Self-Vaccination), we used the PROCESS macro (v. 3.4) for SPSS (v. 27) to conduct targeted mediation analyzes estimating the indirect effect via bootstrapping (95% confidence intervals; number of bootstrap samples: 5000). Mediation analysis tests if a third variable can explain the relationship between the independent and dependent variable, thus outlining a sequence whereby the independent variable indirectly predicts the outcome on the dependent variable via the mediator – the so-called “indirect effect.”Citation43 Given our sample size (N = 2,787), the regression model would be sensitive to small effects of β = 0.003and R2 = 0.003, with 80% power (α = 0.05). To simplify the analyses and avoid reporting marginal effects, we selected Confidence in Vaccines as the mediator variable since it was the only measure of vaccine-related attitudes with a medium-sized association with CAM endorsement (β > 0.30).
A graphical representation of the mediation analyses can be found in . The results indicate that Confidence in Vaccines constitutes a significant mediator and that its mediational role is particularly strong for the relationship between CAM Endorsement and Vaccine Recommendation, accounting for 84% of the association (R2 = 0.27). Furthermore, Confidence in Vaccines accounts for 56% of the association between CAM Endorsement and Self-Vaccination (R2 = 0.16). These mediations were robust across countries, albeit the indirect effects were particularly strong in Germany (see Supplementary Material), and support our hypothesis that attitudes toward vaccines mediate the relationship between CAM Endorsement and vaccine-related behaviors.
Figure 2. Graphical representation of mediation analyses. Values represent standardized β coefficients. Mediational effects were tested by analyzing the indirect effect via bootstrapping (95% confidence intervals; number of bootstrap samples: 5000). CAM = CAM endorsement, CV = Confidence in Vaccines, VR = Vaccine Recommendation, S-V = Self-Vaccination. * = p < .001.
Latent profiles among physicians
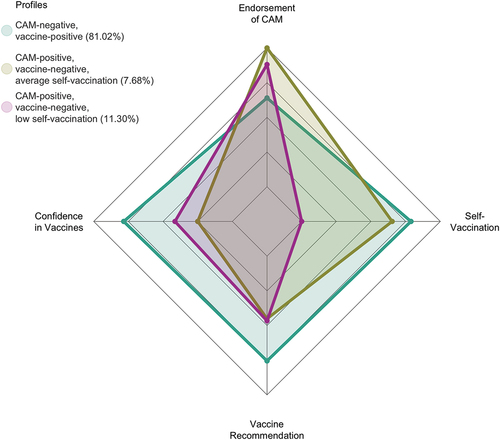
A Latent Profile Analysis (LPA) was conducted using the tidyLPA package for R (v. 4.2.2),Citation44 to quantify the number of participants expressing higher-than-average CAM Endorsement and lower-than-average Confidence in Vaccines, Vaccine Recommendation, and Self-Vaccination. LPA is a person-centered analytic tool that offers a classification of each participant in the most probable profile based on a set of observable variables.Citation45 A range of indices determine the most reliable separation of latent profiles: lower values for the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample-size adjusted BIC (SABIC), as well as an entropy value above 0.80. These fit indices can be expected to function adequately in samples larger than 300 participants, as is the case for all our national subsamples.Citation46 shows the fit indices of models with 1–5 profiles. We selected the 3-profile model, which exhibited the lowest AIC, BIC, and SABIC among models with an optimal entropy parameter (>0.80).
Table 4. Fit of latent profile models.
The standardized means of the resulting three latent profiles are displayed in . The first profile, labeled as “CAM-negative, vaccine-positive,” includes 2,258 physicians (81.02%) exhibiting negative attitudes toward CAM (i.e., below the sample average in CAM Endorsement) and positive toward vaccines (i.e., above the sample average in Vaccine Confidence, Vaccine Recommendation, and Self-Vaccination). This majority profile reflects the expected attitude among physicians inclined to base their clinical practice on the available scientific evidence. The second profile, labeled as “CAM-positive, vaccine-negative, average self-vaccination,” comprises 214 physician (7.68%) who reported above-average CAM Endorsement and below-average confidence in, and recommendation of, vaccines, with average levels of Self-Vaccination. Finally, the third profile, labeled as “CAM-positive, vaccine-negative, low self-vaccination” accounts for 315 physicians (11.30%) expressing above-average CAM Endorsement and below-average confidence in, and recommendation of, vaccines, but this time with below-average Self-Vaccination. In sum, 19% of the surveyed physicians were classified as having above-average CAM Endorsement and below-average confidence in, and recommendation of, vaccines.
Specific LPAs for each participating country are reported in Supplementary Material. While for all countries, the analysis identified a profile with higher CAM Endorsement and lower Vaccine Recommendation, the number of profiles of the most reliable model varied from one country to another. A fourth profile emerged in France, accounting for physicians with positive attitudes toward both CAM and vaccination (9.25% of the French sample), whereas in the 2-profile model of the Portuguese sample the profile that combines higher CAM Endorsement and average Self-Vaccination was not identified. The percentage of physicians expressing higher-than-average CAM Endorsement and lower-than-average Vaccine Confidence and Vaccine Recommendation also varied between countries: Germany (23.72%), France (17.83%), Finland (9.77%), and Portugal (5.86%).
Discussion
In line with our hypotheses, we found evidence in an international sample of physicians with vaccination responsibilities that positive attitudes toward CAM were associated with negative vaccine-related behaviors, such as greater propensity not to self-vaccinate and recommend vaccines included in their national immunization schedules. However, we did not find an association with general behaviors that may be less subject to HCP’s own judgment, such as checking the vaccination status of patients or bringing up the subject with them, which are routinely performed by physicians in the surveyed countries. Our results also indicated that the associations between attitudes to CAM and vaccination behaviors were mediated by lower confidence in vaccines, meaning that physicians who endorse CAM had a higher likelihood of having both lower confidence in vaccines and proneness to recommend vaccines. Moreover, a person-centered analysis (LPA) revealed that larger CAM endorsement occurred together with more negative vaccine attitudes and less vaccine recommendations in 19% of our total sample. As reported in the Supplementary Material, the main results were relatively robust across the four participating countries, although the percentage of physicians exhibiting higher levels of endorsement of CAM and lower willingness to recommend vaccinations varied from one country to another, being larger in Germany and smaller in Portugal.
ErnstCitation47 proposed several potential causes for the observed relationship between vaccine hesitancy and CAM.Citation9–12,Citation14,Citation48 Since CAM use occurs more frequently at the poles of the disease spectrum (i.e., in cases of minor or life-threatening illness), CAM use has been identified as a marker of both misperception of risk and frustration with regular healthcare (e.g., negative prognosis or lack of remission of symptoms).Citation49 Accordingly, CAM-related health conceptions could be motivating HCPs to be more reluctant to recommend and receive vaccinations both for illnesses that are perceived as minor and in cases of severe clinical pictures. There are also reasons related to the potential alignment between CAM and the ideology or worldview of the HCP, such as their distrust in “Big Pharma” or a general disregard for scientific knowledge.Citation50 Along the same lines, Attwell et al.Citation51 found in semi-structured interviews with vaccine hesitant Australian parents that the main reasons for their preference for CAM included a greater affinity between CAM, their do-it-yourself approach to health care, and their sympathy for natural and harm-free products in contrast to medications marketed by pharmaceutical companies, which were perceived as ineffective, “toxic” and “adulterating.”Citation52
Besides these implicit reasons, some CAM traditions are theoretically incompatible with vaccination and portrayed as a valid, or even superior, alternative to scientific knowledge.Citation51 A quantitative study found that pro-CAM and anti-vaccination attitudes both reflect beliefs contrary to basic scientific knowledge, such as “an imbalance between energy currents lies behind many illnesses” and “an illness should be treated with a medicine that has properties similar to those of the illness.”Citation31,Citation53 An example of these CAM-related beliefs that contradict the theoretical basis of vaccinations is “homeopathic immunization” through so-called “nosodes” – orally administered extreme dilutions of infectious agents.Citation54 Similarly, Rudolf Steiner and Ryke Geerd Hamer, promoters of anthroposophic medicine and German new medicine, respectively, have sown doubts about vaccinations based on their conceptions of the etiology and treatment of diseases.Citation55 Consequently, strong science denial and vaccine hesitancy can be found within these communities,Citation56,Citation57 and outbreaks of vaccine-preventable diseases, such as measles and whooping cough, have been reported in educational centers linked to anthroposophy.Citation58
Considering recurrent cases of suboptimal vaccine uptake and the risks associated with CAM use,Citation59,Citation60 as well as the spread of CAM-related misinformation during the COVID-19 pandemic,Citation61 the reported results have relevant implications for clinical practice. As the most trusted source of health information,Citation19,Citation20 physicians play a key role in countering vaccine hesitancy among patients.Citation62 However, alternative health beliefs among physicians could be hindering productive face-to-face interactions, which constitute the best opportunity to discuss patients’ vaccine objections by effectively rebutting their misconceptions around vaccinations. It would therefore be recommendable to deploy interventions to tackle the implicit and explicit reasons that may lead physicians to endorse CAM. Among these potential interventions are inoculation or empathetic-refutational techniques.Citation63,Citation64
Despite the fact that the rates of physicians exhibiting higher-than-average CAM endorsement and lower-than-average vaccine confidence and recommendation identified in our LPA have no direct precedents, the resulting patterns mirror the results from previous studies investigating CAM use among HCPs and the general population. As we mentioned in the introductory section, HCPs tend to be equally likely than the general population to use CAM,Citation24 even though some studies have found strikingly high rates of CAM use and referral among HCPs—e.g., 39% in a study by Posadzki et al.Citation25 55% in a study by Berretta et al.Citation26 and 68% in a study by Linde et al.Citation27 A survey on the use of several CAM techniques, such as acupuncture, massage, homeopathy, and spiritual healing, during the last 12 months among the general European population showed an overall average rate of CAM use of 25.9%, with Portugal exhibiting the lowest rate of CAM use (12.9%) and Germany the highest (39.5%) among the four countries included in the present study—31.2% in France and 35.3% in Finland.Citation65
The higher rates observed in Germany may be explained by a greater integration of CAM into the German health system, as this country has recognized natural health practitioners (heilpraktiker) since the late 1930s,Citation66 and it is also common for German medical doctors to provide CAM – around 60% in some surveys.Citation27,Citation67 Natural health practitioners only require an examination on basic medical knowledge at a local public health office to become accredited, so university medical education and advanced training are not necessary for CAM practitioners in Germany. Even though these CAM practitioners are allowed to provide a wide variety of CAM techniques, only a few of these interventions are reimbursed under the German statutory health insurance.Citation68 CAM is also integrated into the French medical system, especially acupuncture and homeopathy. Both CAM-only practitioners and physicians who occasionally practice CAM can prescribe homeopathic products, but these products have no longer been reimbursed by the National Health Insurance Fund since 1 January 2021. However, patients may receive reimbursement of 70% for acupuncture as long as they seek treatment from a registered CAM practitioner.Citation69 In contrast, CAM is not officially integrated into the Finnish healthcare system. The Finnish Health Professionals Act establishes that “a person is not acting as a health professional when providing alternative therapies, even if he or she is trained as a health professional. A health professional providing alternative therapies must ensure that clients understand that they are receiving non-medical care when providing services.”Citation70 Finally, in Portugal, the participating country with the lowest rates of CAM endorsement, practitioners of acupuncture, phytotherapy, traditional Chinese medicine, osteopathy, and chiropractic must have completed university studies accredited by the Agency for Accreditation of Higher Education to receive accreditation from the Central Administration of the Health System. Homeopathy remains a controversial issue and accreditation is not currently issued, so homeopaths in Portugal act without regulation. Despite being strictly regulated and with the only exception of acupuncture for the treatment of pain, CAM is not available in Portuguese public health facilities and CAM treatments are not reimbursed under the national health insurance. Thus, Portuguese regulation focuses more on patient protection than on facilitating or increasing access to CAM.Citation71
The reported study has great strengths, such as the use of large samples from multiple countries, multivariate analyses considering potential sociodemographic confounders, and validated tools for measurements. The statistical methods used in this study can be prone to overfitting if sample sizes are small and assumptions about the sample distributions are not met. However, we did not observe these issues within our analyses. Indeed, post-hoc sensitivity analyses confirmed that the sample was unlikely to be underpowered. However, there are several limitations that constrain the interpretation of our results. First, despite being large and allowing the analysis of a range of sociodemographic differences, the samples are not fully representative of the medical populations of the countries included in the study—e.g., the Portuguese sample is particularly young compared to the population from which it was collected. Therefore, the generalization of these results at the national level should be approached with some caution. Second, although the reported mediation analyses cannot confirm causal relationships between the tested variables due to the correlational nature of our data, they can guide future experimental research due to its compatibility with a causal interpretation (i.e., association does not imply causation, but causation implies association in cross-sectional samples with proper size and variability). Third, the four countries included in the study are Western, Educated, Industrialized, Rich, and Democratic (WEIRD).Citation72 Given that public policies integrating CAM into the national health system tend to be more prevalent among developing countries,Citation15 caution is also required when these outcomes are extrapolated to non-WEIRD countries. Fourth, our psychometric approach to CAM endorsement was general, so we have not measured differences between CAM techniques. Future studies may wish to replicate these analyses at the level of specific techniques.
Concluding remarks
Cross-sectional data collected from 2,787 physicians with vaccination responsibilities from four European countries demonstrated a consistent positive relationship between CAM endorsement and vaccine hesitancy, with around 1/5 of the surveyed physicians manifesting this relationship to a greater or lesser extent. The associations between CAM endorsement and a lower propensity to recommend and receive vaccinations, in which low confidence in vaccines plays a mediational role, are particularly relevant due to its potential negative impact on immunization campaigns. We have argued that, from a theoretical point of view, this situation may be explicable by reasons that are both implicit (i.e., CAM would fit better with certain worldviews and ideological standpoints that conflict with the epistemology and values that underlies scientific knowledge) and explicit (i.e., some CAM techniques are doctrinally opposed to the use of vaccines). Although we have outlined these potential explanations for the observed relationships, more research is needed to better understand the underlying mechanisms.
Authors’ contributions
A.F.: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, and Visualization.
L.K.: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing, and Visualization.
P.V.: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision, Project administration.
O.M.: Formal analysis, Data curation, Writing – original draft, Writing – review & editing, and Visualization.
F.T.: Formal analysis, Data curation, Writing – original draft, Writing – review & editing, and Visualization.
A.G.: Conceptualization, Methodology, Investigation, Data curation, and Writing – review & editing.
P.S.: Conceptualization, Methodology, Investigation, Data curation, and Writing – review & editing.
D.L.H.: Conceptualization, Methodology, Writing – review & editing, and Visualization.
S.L.: Conceptualization, Methodology, Writing – review & editing, Supervision, Project administration, and Funding acquisition.
F.R.: Investigation, Resources, Supervision, and Project administration.
C.B.: Investigation, Supervision, and Project administration.
A.S.: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision, and Project administration.
All authors read and approved the final manuscript.
Ethics approval and consent to participate
Informed consent was obtained from all participants prior to their participation. All study methods were performed in accordance with the relevant guidelines and regulations approved by the Research Ethics Committees:
France (South-Eastern Health Regional Observatory): 2021-12-16-01.
Finland (University of Turku): 1/2022.
Portugal (University of Coimbra): 093-CE-2021.
Germany (University of Erfurt): 20210713.
Supplemental Material
Download PDF (1.2 MB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All the datasets, codes, and materials used in this study are publicly available in the Open Science Framework repository: https://osf.io/d6uvg/. The recruitment strategies were pre-registered in 3 of the participating countries (Portugal: https://osf.io/j7as2, Germany: https://aspredicted.org/CTZ_N1B, Finland: https://osf.io/586jb).
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2242748.
Additional information
Funding
References
- Dubé È, Ward JK, Verger P, MacDonald NE. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu Rev Public Health. 2021;42(1):175–12. doi:10.1146/annurev-publhealth-090419-102240.
- Dubé È, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–73. doi:10.4161/hv.24657.
- MacDonald N. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi:10.1016/j.vaccine.2015.04.036.
- Geiger M, Rees F, Lilleholt L, Santana AP, Zettler I, Wilhelm O, Betsch C, Böhm R. Measuring the 7Cs of vaccination readiness. Eur J Psychol Assess. 2021;38(4):261–9. doi:10.1027/1015-5759/a000663.
- Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. Barriers of influenza vaccination intention and behavior – a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. 2017;12(1):e0170550. doi:10.1371/journal.pone.0170550.
- Kohler S, Koinig I. The effect of science-related populism on vaccination attitudes and decisions. J Behav Med. 2022;46(1–2):229–38. doi:10.1007/s10865-022-00333-2.
- Stasielowicz L. A continuous time meta-analysis of the relationship between conspiracy beliefs and individual preventive behavior during the COVID-19 pandemic. Sci Rep. 2022;12:11508. doi:10.1038/s41598-022-15769-4.
- Verger P, Botelho-Nevers E, Garrison A, Gagnon D, Gagneur A, Gagneux-Brunon A, Dubé E. Vaccine hesitancy in health-care providers in Western countries: a narrative review. Expert Rev Vaccin. 2022;21(7):909–27. doi:10.1080/14760584.2022.2056026.
- Guay M, Gosselin V, Petit G, Baron G, Gagneur A. Determinants of vaccine hesitancy in Quebec: a large population-based survey. Hum Vaccin Immunother. 2019;15:2527–33. doi:10.1080/21645515.2019.1603563.
- Hornsey M, Lobera J, Díaz-Catalán C. Vaccine hesitancy is strongly associated with distrust of conventional medicine, and only weakly associated with trust in alternative medicine. Soc Sci Med. 2020;255:113019. doi:10.1016/j.socscimed.2020.113019.
- Lewandowsky S, Woike J, Oberauer K. Genesis or evolution of gender differences? Worldview-based dilemmas in the processing of scientific information. J Cognit. 2020;3(1):9. doi:10.5334/joc.99.
- Soveri A, Karlsson LC, Mäki O, Antfolk J, Waris O, Karlsson H, Karlsson L, Lindfelt M, Lewandowsky S. Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. PLoS One. 2020;15(7):e0236527. doi:10.1371/journal.pone.0236527.
- Wong L, Wong P, AbuBakar S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: the way forward for Malaysia, a Southeast Asian country. Hum Vaccin Immunother. 2020;16:1511–20. doi:10.1080/21645515.2019.1706935.
- Soveri A, Karlsson LC, Antfolk J, Lindfelt M, Lewandowsky S. Unwillingness to engage in behaviors that protect against COVID-19: the role of conspiracy beliefs, trust, and endorsement of complementary and alternative medicine. BMC Public Health. 2021;21(1):684. doi:10.1186/s12889-021-10643-w.
- World Health Organization. WHO global report on traditional and complementary medicine. 2019 [accessed 2023 Jun 6]. https://apps.who.int/iris/handle/10665/312342.
- Ernst E. Is reflexology an effective intervention? A systematic review of randomised controlled trials. MJA. 2009;191(5):263–6. doi:10.5694/j.1326-5377.2009.tb02780.x.
- Ernst E, Canter P. A systematic review of systematic reviews of spinal manipulation. J R Soc Med. 2006;99:192–6. doi:10.1177/014107680609900418.
- Shang A, Huwiler-Müntener K, Nartey L, Jüni P, Dörig S, Sterne JA, Pewsner D, Egger M. Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy. Lancet. 2005;366(9487):726–32. doi:10.1016/S0140-6736(05)67177-2.
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6. doi:10.1016/j.vaccine.2016.10.042.
- Siddiqui M, Salmon D, Omer S. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother. 2013;9(12):2643–8. doi:10.4161/hv.27243.
- Hoon Chang K, Brodie R, Choong MA, Sweeney KJ, Kerin MJ. Complementary and alternative medicine use in oncology: a questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11(1):196. doi:10.1186/1471-2407-11-196.
- Bjerså K, Stener Victorin E, Fagevik Olsén M. Knowledge about complementary, alternative and integrative medicine (CAM) among registered health care providers in Swedish surgical care: a national survey among university hospitals. BMC Complement Altern Med. 2012;12(1):42. doi:10.1186/1472-6882/12/42.
- Sewitch M, Cepoiu M, Rigillo N, Sproule D. A literature review of health care professional attitudes toward complementary and alternative medicine. J Evid-Based Integr Med. 2008;13(3):139–54. doi:10.1177/153321010832554.
- Johnson P. Personal use of complementary and alternative medicine (CAM) by U.S. Health Serv Res. 2012;47(1pt1):211–27. doi:10.1111/j.1475-6773.2011.01304.x.
- Posadzki P, Alotaibi A, Ernst E. Prevalence of use of complementary and alternative medicine (CAM) by physicians in the UK: a systematic review of surveys. Clin Med J. 2012;12(6):505–12. doi:10.7861/clinmedicine.12-6-505.
- Berretta M. Physician attitudes and perceptions of complementary and alternative medicine (CAM): a multicentre Italian study. Front Oncol. 2020;28:594. doi:10.3389/fonc.2020.00594.
- Linde K, Alscher A, Friedrichs C, Wagenpfeil S, Karsch-Völk M, Schneider A. Belief in and use of complementary therapies among family physicians, internists and orthopaedists in Germany – cross-sectional survey. Fam Pract. 2015;32(1):62–8. doi:10.1093/fampra/cmu071.
- Fasce A, Schmid P, Holford DL, Bates L, Gurevych I, Lewandowsky S. A taxonomy of anti-vaccination arguments: systematic literature review and text modeling. Nat Hum Behav. 2023 Jul 31:22. doi:10.1038/s41562-023-01644-3.
- Holford D, Fasce A, Costello TH, Lewandowsky S. Psychological profiles of anti-vaccination argument endorsement. Sci Rep. 2023 Jul 17:12. doi:10.1038/s41598-023-30883-7.
- Smith L, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059–69. doi:10.1016/j.vaccine.2017.09.046.
- Bryden G, Browne M, Rockloff M, Unsworth C. Anti-vaccination and pro-CAM attitudes both reflect magical beliefs about health. Vaccine. 2018;9(9):1227–34. doi:10.1016/j.vaccine.2017.12.068.
- Hadjipanayis A, van Esso D, Del Torso S, Dornbusch HJ, Michailidou K, Minicuci N, Pancheva R, Mujkic A, Geitmann K, Syridou G, et al. Vaccine confidence among parents: large scale study in eighteen European countries. Vaccine. 2020;38(6):1505–12. doi:10.1016/j.vaccine.2019.11.068.
- Wardle J, Frawley J, Steel A, Sullivan E. Complementary medicine and childhood immunisation: a critical review. Vaccine. 2016;34(38):4484–500. doi:10.1016/j.vaccine.2016.07.026.
- Bleser W, Elewonibi BR, Miranda PY, BeLue R. Complementary and alternative medicine and influenza vaccine uptake in US children. Pediatrics. 2016;138(5):e20154664. doi:10.1542/peds.2015-4664.
- Frawley J, Foley H, McIntyre E. The associations between medical, allied and complementary medicine practitioner visits and childhood vaccine uptake. Vaccine. 2018;36(6):866–72. doi:10.1016/j.vaccine.2017.12.036.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;5(2):179–211. doi:10.1016/0749-5978(91)90020-T.
- Hyland M, Lewith G, Westoby C. Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Complement Ther Med. 2003;11:33–8. doi:10.1016/S0965-2299(02)00113-9.
- Garrison A, Karlsson, L, Fressard, L, Fasce A, Rodrigues F, Schmid P, Taubert F, Holford D, Lewandowsky L, Nynäs P, et al. International adaptation and validation of the Pro-VC-Be: the JITSUVAX project. 2023 Jul 28:53. doi:10.1080/14760584.2023.2242479.
- Verger P, Fressard L, Soveri A, Dauby N, Fasce A, Karlsson L, Lewandowsky S, Schmid P, Dubé E, Gagneur A, et al. An instrument to measure psychosocial determinants of health care professionals’ vaccination behavior: validation of the Pro-VC-Be questionnaire. Expert Rev Vaccines. 2022;21(5):693–709. doi:10.1080/14760584.2022.2046467.
- Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. doi:10.18637/jss.v067.i01.
- Kuznetsova A, Brockhoff P, Christensen R. lmerTest package: tests in linear mixed effects models. J Stat Soft. 2017;82(13):1–26. doi:10.18637/jss.v082.i13.
- Lüdecke D, Ben-Shachar M, Patil I, Waggoner P, Makowski D. Performance: an R package for assessment. J Open Source Softw. 2021;6(60):3139. doi:10.21105/joss.03139.
- MacKinnon D, Fairchild A, Fritz M. Mediation analysis. Ann Rev Psychol. 2007;58:593–614. doi:10.1146/annurev.psych.58.110405.085542.
- Rosenberg J, Beymer P, Anderson D, van Lissa CJ, Schmidt J. tidyLPA: an R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. J Open Source Softw. 2018;3(30):978. doi:10.21105/joss.00978.
- Berlin K, Williams N, Parra G. An introduction to latent variable mixture modeling (Part 1): overview and cross-sectional latent class and latent profile analyses. J Pediatr Psychol. 2014;39:174–87. doi:10.1093/jpepsy/jst084.
- Nylund-Gibson K, Choi A. Ten Frequently asked questions about latent class analysis. Transl Issues Psychol Sci. 2018;4:440–61. doi:10.1037/tps0000176.
- Ernst E. Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination. Vaccine. 2001;20:S90–S3. doi:10.1016/S0264-410X(01)00290-0.
- Thomire A, Raude J. The role of alternative and complementary medical practices in vaccine hesitancy among nurses: A cross-sectional survey in Brittany. Infect Dis Now. 2021;51:159–63. doi:10.1016/j.medmal.2020.09.021.
- Hwang J. The use of complementary and alternative medicine by Korean breast cancer women: is it associated with severity of symptoms? Evid-Based Complementary Altern Med. 2015;2015:1–7. doi:10.1155/2015/182475.
- Browne M. Epistemic divides and ontological confusions: The psychology of vaccine scepticism. Hum Vaccin Immunother. 2018;14:2540–2. doi:10.1080/21645515.2018.1480244.
- Attwell K, Ward PR, Meyer SB, Rokkas PJ, Leask J. “Do-it-yourself”: vaccine rejection and complementary and alternative medicine (CAM). Soc Sci Med. 2018;196:106–14. doi:10.1016/j.socscimed.2017.11.022.
- Cameron D. “Imagine the perfect vaccine”: homeopathic vaccine alternatives and vaccine discourse in English Canada. Can Bull Med Hist. 2021;38:32–62. doi:10.3138/cbmh.445-052020.
- Lindeman M, Keskivaara P, Roschier M. Assessment of magical beliefs about food and health. J Health Psychol. 2000;5:195–209. doi:10.1177/135910530000500210.
- Rieder M, Robinson JL. ‘Nosodes’ are no substitute for vaccines. Paediatr Child Health (Oxford). 2001;20(4):219–20. doi:10.1093/pch/20.4.219.
- News. “HIV ist eine ganz normale Allergie”: “Wunderheiler” Hamer im NEWS-interview. 2010 Sep 13 [accessed 2023 Jul 28]. https://www.news.at/a/hiv-allergie-wunderheiler-hamer-news-interview-259588.
- Bory P, Giardullo P, Tosoni S, Turrini V. ‘We will multiply the fires of resistance’: The catalysts of dissent against institutional science and their interplay with refused knowledge communities. Public Underst Sci. 2022;32(1):2–19. doi:10.1177/09636625221113524.
- Sobo E. Social cultivation of vaccine refusal and delay among Waldorf (Steiner) school parents. Med Anthropol Q. 2015;29:381–99. doi:10.1111/maq.12214.
- Ernst E. Anthroposophy: a risk factor for noncompliance with measles immunization. Pediatr Infect Dis J. 2011;30:187–9. doi:10.1097/inf.0b013e3182024274.
- Niggermann B, Grüber C. Side-effects of complementary and alternative medicine. Allergy. 2003;58(8):707–16. doi:10.1034/j.1398-9995.2003.00219.x.
- Wardle J, Adams J. Indirect and non-health risks associated with complementary and alternative medicine use: an integrative review. Eur J Integr Med. 2014;6:409–22. doi:10.1016/j.eujim.2014.01.001.
- Recuero R, Soares F, Polarization ZG. Polarization, hyperpartisanship and echo chambers: how the disinformation about Covid-19 circulates on Twitter. Contracampo. 2021;40(1):2238–577. doi:10.22409/contracampo.v40i1.45611.
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012;12(1):154. doi:10.1186/1471-2431/12/154.
- Lewandowsky S, van der Linden S. Countering misinformation and fake news through inoculation and prebunking. Eur J Soc Psychol. 2021;25:217–22. doi:10.1080/10463283.2021.1876983.
- Holford D, Schmid P, Fasce A, Lewandowsky S. The empathetic refutational interview to tackle vaccine misconceptions and improve vaccine acceptance. forthcoming.
- Kemppainen L, Kemppainen TT, Reippainen JA, Salmenniemi ST, Vuolanto PH. Use of complementary and alternative medicine in Europe: Health-related and sociodemographic determinants. Scand J Public Health. 2018;46(4):448–55. doi:10.1177/1403494817733869.
- Heudorf U, Carstens A, Exner M. Naturopathic practitioners and the public health system. Legal principles as well as experience from naturopathic practitioner candidate tests and hygiene inspections of naturopathic practitioner’s practices in the Rhine-Main area in 2004-2007. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2010;53:245–57. doi:10.1007/s00103-009-1024-0.
- Joos S, Musselmann B, Szecsenyi J. Integration of complementary and alternative medicine into family practices in Germany: results of a national survey. Evid-Based Complementary Altern Med. 2011;2011:1–8. doi:10.1093/ecam/nep019.
- Krug K, Kraus KI, Herrmann K, Joos S. Complementary and alternative medicine (CAM) as part of primary health care in Germany–comparison of patients consulting general practitioners and CAM practitioners: a cross-sectional study. BMC Complement Altern Med. 2016;16:409. doi:10.1186/s12906-016-1402-8.
- Cadet C Étude de prévalence du recours aux médecines alternatives et complémentaires (MAC) chez les patients consultant en médecine générale à La Réunion (Avril-Juillet 2022) [ dissertation]. La Réunion (France): Université de La Réunion; 2023.
- The Finnish Medical Association. Uskomushoidot. 2021 [accessed 2021 Jul 28]. https://www.laakariliitto.fi/laakarin-etiikka/potilas-laakarisuhde/uskomushoidot/.
- Amaral P, Fronteira I. Regulation of non-conventional therapies in Portugal: lessons learnt for strengthening human resources in health. Hum Resour Health. 2021;19:114. doi:10.1186/s12960-021-00655-3.
- Henrich J, Heine S, Norenzayan A. The weirdest people in the world? Behav Brain Sci. 2010;33:61–83. doi:10.1017/S0140525X0999152X.