ABSTRACT
Despite widespread availability of vaccines against SARS-CoV-2 virus, the cause of Coronavirus Disease 2019 (COVID-19), its uptake in many Arab countries is relatively low. This literature review aimed to scope evidence on COVID-19 vaccine hesitancy (VH) in the Arab world. A total of 134 articles reporting prevalence of COVID-19 VH and associated factors, conducted in any of the 22 Arab League countries, were reviewed. COVID-19 VH prevalence ranged from 5.4% to 83.0%. Female gender, young age, low education level and lack of previous influenza vaccine uptake were most commonly reported to be associated with COVID-19 VH. The most-reported personal concerns contributing toward VH were related to the rapid development, safety and side effects of vaccine, as well as an overall lack of trust in government policies toward pandemic control and widespread conspiracy theories. Tailored interventions to enable the distribution of trusted information and enhance public acceptance of immunization are warranted.
Introduction
During December 2019, several cases of acute pneumonia of unknown etiology were diagnosed in Wuhan-China, with spread and severity so substantial that it rapidly drew global attention. Consequently, the new virus genome sequence was identified as severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2), causing the ongoing COVID-19 pandemic.Citation1 The pandemic has infected over 758 million confirmed cases worldwide and caused over 6.86 million deaths as of February 2023.Citation2
As different measures were taken to curb the worst effect of virus, pharmaceutical industries were also urged to develop vaccines immediately to limit the escalating infection rates.Citation3 The new awaited vaccines were predicted to reduce incidence, virulence, and morbidity. However, despite the eager anticipation of vaccine availability worldwide, the urgency of the development, coupled with the unknown side effects, triggered vaccine hesitancy, refusal, and antivaccine movements.Citation4 According to WHO, vaccine hesitancy (VH) is defined as a “delay in the acceptance or refusal of vaccination despite the availability of vaccination services.”Citation4 Even long before the COVID-19 pandemic, vaccine hesitancy has hindered the global effort to control outbreaks affecting thousands of vulnerable individuals to the extent that the World Health Organization (WHO) considers it as one of the top public health challenges, that needs to be tackled, along with poverty and HIV.Citation5 The scope of vaccine acceptance ranges from accepting the vaccine without any doubts to rejecting it altogether. Accepting and taking some, refusing others, and delaying vaccination are all counted toward VH.Citation6
With a total population of over 440 million, the Arab world comprises 22 countries extending from the Arabian Sea in the east to the Atlantic Ocean in the west.Citation7 Despite the significant disparities in cultural, environmental, and socio-economic determinants of health in the Arab world, it has been affected by the COVID-19 in a way similar to that of the rest of the world. The pandemic has infected over 14.1 million individuals and caused around 173.3 thousand deaths as of February 2023 in the Arab world.Citation8 Several types of vaccines have been introduced in the region to control the pandemic (refer to Table S1 for vaccines used in each country), including RNA-based vaccines such as Pfizer-BioNTech and Moderna, non replicated viral vector vaccines such as Oxford-AstraZeneca, Jcovden, CanSino, Sputnik V and Sputnik Light, whole inactivated virus-based vaccines such as Sinopharm, Sinovac, Covaxin and Valneva and protein subunit based vaccines such as Recombinant-SARSCoV-2 Vaccine.Citation9 The expedited production and approval processes, along with wide variations in the vaccine brands, have led to an increase in uncertainty regarding effectiveness of the vaccines. In addition, the distribution of vaccines in the Arab world faced some initial challenges, especially with supply, accessibility, and storage, that were overcome to ensure availability for all individuals.Citation10
Despite the wide availability and accessibility of vaccines in most of the countries in the Arab world, VH was very common, particularly in the initial phases of vaccination campaigns.Citation11,Citation12 Early cross-sectional surveys showed variable attitudes toward COVID-19 vaccination ranging from high acceptance rates in some countries to increased hesitancy rates in others.Citation10,Citation12 Sociodemographic factors that could have contributed to VH and personal views that might influence vaccination decisions were investigated.Citation11 Several reviews have been carried out within the last three years summarizing the COVID-19 vaccination uptake and affecting factors in several regions of the world.Citation13,Citation14 However with the emergence of more studies in relation to this topic, targeting different populations and using different models, there is a consistent need to review the findings of these papers to provide policy makers with latest evidence on best vaccination programs and approaches. This scoping review summarizes evidence from the published literature investigating prevalence of the hesitancy toward vaccination against COVID-19 and/or factors associated with the hesitancy in the Arab world. The review also explores the most common personal perspectives acting as barriers, leading to hesitancy against vaccination to COVID-19 in this region.
Materials and methods
Search strategy
This review was conducted and is reported in accordance to the guidelines set by Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR).Citation15 Refer to Table S2 for PRISMA-ScR checklist. The protocol for the review was registered with Open Science Framework (OSF; Digital Object Identifier https://doi.org/10.17605/OSF.IO/K83ZX). Review was performed following five key steps of Arksey O’Malley framework.Citation16 PubMed, Scopus, and Embase databases were searched between October 2021 and February 2023, for articles with studies based on cross-sectional design, reporting prevalence of hesitancy against vaccination to COVID-19. A search strategy using appropriate combination of key words and MESH terms, developed by the authors and reviewed by expert librarian was used. Search terms related to COVID-19, vaccine, and vaccine hesitancy, in addition to the list of the 22 Arab countries (Algeria, Bahrain, Comoros, Djibouti, Egypt, Iraq, Jordan, Kuwait, Lebanon, Libya, Mauritania, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, United Arab Emirates (UAE), and Yemen) were included. Refer to Table S3 for the search strategy used in the PubMed. Study search was conducted by two independent reviewers (SM, ZA).
Eligibility criteria
Articles were included if they were based on a study with cross-sectional design, with a primary aim to investigate the prevalence of COVID-19 vaccination; and/or factors associated with vaccine hesitancy, in any of 22 Arab countries, regardless of the studied population (refer to Table S4 for the eligibility criteria). Articles published in Arabic or English language were considered eligible. Mixed method studies were included if the quantitative component in the study was based on a cross sectional design. Articles based on studies in non-Arabic countries, with other than cross-sectional study designs, and those addressing VH for non-COVID-19 viruses were excluded. Only articles reporting VH and associated factors and attitudes among adults were included, with those addressing parents’ views regarding VH among children excluded. Articles were eligible if they were published from October 2021, as the vaccine was widely available for the majority of the populations by that time. Original peer-reviewed articles were included whereas conference proceedings and abstracts with incomplete data were excluded.
Study selection and data extraction
After removal of duplicate records, titles and abstracts of the retrieved articles were screened for their full or potential eligibility. Full texts of the eligible articles were screened and assessed for inclusion against the pre-set inclusion criteria. Title/abstract screening and full-text screening were carried out by two reviewers (SM, ZA) independently and any conflicts were resolved by mutual discussion or involvement of the third reviewer (IE). The bibliography of the included articles was also hand-searched for any additional eligible studies that might have been missed in the database search.
From the articles that were deemed eligible for inclusion, data were extracted using a predetermined extraction tool. The extraction tool included fields on the basic characteristics of studies as well as methodological aspects, such as author and year of publication, study setting, type of population, sample size, and mode of data collection. Study outcomes in terms of calculated or calculable data on the prevalence of and factors associated with hesitancy against COVID-19 vaccination as well as personal beliefs leading to VH acting as barriers for vaccine uptake were also extracted. Only data on factors found to be statistically significant as reported in the studies, based on regression modeling were included. Data on the outcomes were then summarized narratively.
Results
Study selection
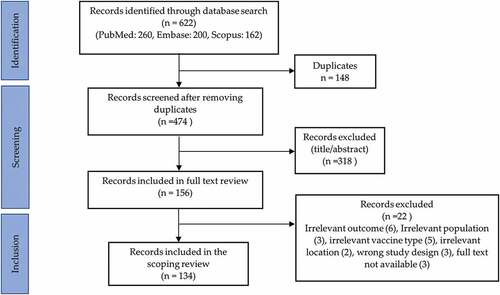
A total of 622 articles were identified from the database search, including PubMed (260), Embase (200) and Scopus (162) (). After removal of duplicates and screening the records for title/abstract and full text, 156 articles remained. 22 records were excluded via full-text screening due to irrelevant outcomes i.e., parents’ hesitancy toward vaccination of children (6), irrelevant populations such as Arab immigrants in non-Arabic countries (3), wrong vaccine types such as that for Influenza (5), irrelevant geographical locations (2), wrong study design i.e., qualitative (3) and nonavailability of full text (3). Resultingly, 134 articles met the inclusion criteria and were included in the review.
Characteristics of the included studies
Characteristics of the included studies are summarized in , with detail of individual studies provided in . Overall most of the studies (132) were cross-sectional, with two of mixed method design.Citation77,Citation87 Of the included articles, 123 addressed hesitancy against primary COVID-19 vaccination whereas 10 addressed against that of booster vaccination and one addressed both.Citation106 Studies were conducted in 18 (81.8%) out of the 22 Arab countries. The majority of the included studies were conducted in Saudi Arabia (29.8%), followed by Egypt and Jordan (11.9% each), multiple countries (11.1%), Lebanon (5.2%), Iraq, Qatar and UAE (4.5% each), Kuwait (3.7%), Palestine (3.0%), Sudan (2.2% each), Algeria and Oman (1.5% each), Morocco, Somalia, Syria, Yemen, Tunisia and Libya (0.7% each), ().
Table 1. Summary of the included studies based on characteristics.
Table 2. Summary of 124 articles with studies reporting hesitancy against primary COVID-19 vaccination.
Table 3. Summary of 11 articles with studies reporting hesitancy against COVID-19 booster vaccination.
Number of participants in the included studies ranged from 111–36,220.Citation35,Citation81 The general public was the most commonly addressed population (76 studies), followed by healthcare workers (HCWs) including physicians, nurses and dentists (32 studies), university students (14 studies) and pregnant/lactating women (14 studies). Other populations subgroups addressed in the studies included patients with cancer and chronic illnesses, refugees, older adults, dental patients and air travelers. Participants suffering from chronic diseases included those with diabetes, rhematic disease, HIV and on hemodialysis.Citation61,Citation119,Citation129,Citation139
For data collection, the majority of the studies used online surveys (122), whereas few used printed questionnaires (14). Telephone calls and in-person interviews were also used for data collection sparingly.Citation35,Citation36,Citation47,Citation111 Most of the questionaries used in the survey were self-developed by the researchers or based on those used in previous studies. However, few studies developed their questionnaires on validated existing tools such as the WHO-SAGE survey tool,Citation72–77 the GRA Vax scaleCitation21,Citation22 and the 5C scale.Citation31,Citation85 Few included studies also used Health Belief Model (HBM) to guide data collection.Citation24,Citation67,Citation93,Citation127
Prevalence of hesitancy toward vaccination against COVID-19
Study-based prevalence of hesitancy against primary COVID-19 vaccination is described in whereas that against booster vaccination in . COVID-19 VH varied considerably across the 130 articles reporting VH, included in this review. Hesitancy levels ranged from as high as 83.0% in a large multinational survey of 22 Arab countriesCitation82 to just 5.4% among the general population in Saudi Arabia.Citation130 Some articles included studies focused on the attitude toward vaccination and did not report data about the hesitancy ratesCitation26,Citation56,Citation57,Citation85 (). Reported VH ranged between 12%-83% for general population, 14%-79% for HCWs, 20.1%-49.1% for pregnant and lactating mothers, 13%-65.1% for students, 10.4%-75.6% for refugees, 45% for cancer patients and 37–63.8% for patients suffering from chronic diseases. When summarized on the basis of geographical location, VH prevalence was found to be 5.4%-63.8% (Saudi Arabia), 12%-79% (Egypt), 10.4%-80.1% (Jordan), 16.7%-74.3% (Kuwait), 13%-78.9% (Lebanon), 27.9%-62.2% (Palestine), 26%-57.3% (Qatar), 31.8%-57% (UAE), 57%-60.1% (Oman), 31.4%-44.2% (Sudan), 38.3%-49.9% (Yemen), 20.4% (Libya), 34.7% (Tunisia), 36%(Morocco), 47% (Algeria) and 24.5%-83% (multiregional). VH was found to be 9.6%-83% in articles published in 2021, 5.4%-81.0% in articles in 2022 and 20%-38.3% in articles in 2023. 11 articles including studies that measured COVID-19 booster vaccine hesitancy found it to be 21.8% − 55.4%.Citation106–141–Citation150
Factors associated with hesitancy and acceptance toward vaccination against COVID-19
The factors most commonly reported to be associated with hesitancy toward vaccination against COVID-19 in the majority of the studies were female gender, young age, rural background, low level of educational attainment, low-income level, lack of previous Influenza vaccine uptake, lack of acquaintance with someone having suffered from COVID-19 infection, low COVID-19 vaccine knowledge, less fear and worry of contracting the infection and low risk perception. Other less commonly reported associated factors leading to low VH, identified from the studies, included healthcare sector-related profession, preexisting chronic disease, positive attitude toward general vaccination, COVID-19 vaccine access and price and migrant status. For healthcare workers, years of experience, practice setting, previous provision of care for COVD-19 patient and mode of contact (direct versus indirect) with patients were found to be associated with VH in the included studies. For pregnant and lactating women, pregnant or breastfeeding status, knowledge of other pregnant and breastfeeding women being infected with COVID-19 or having had the vaccine and recommendation by obstetrician/gynecologist were important predictors for VH.
Few articles based on studies assessing hesitancy via HBM showed that it was consistently associated with constructs including preventive measures, perceived benefit, perceived barriers, cues to action and subjective norms. Studies also reported that attitudinal scores and protective measure adherence scores were also associated with COVID-19 VH.Citation25,Citation42,Citation71,Citation77 In terms of personal perspectives leading to COVID-19 VH, the worry regarding vaccine side effects, insufficient time for vaccine testing, belief in natural immunity, belief that symptomatic cases are the only infection carriers, mistrust in government authorities, healthcare system and pharmaceutical companies, concerns on vaccine safety and effectiveness, experience of contracting infection after previous vaccine, belief in origin of the pandemic, conspiracy theories related to COVID-19 vaccine development, belief in community responsibility and vaccine compulsion for all citizens, were identified from the included studies. For communication and sources of information, studies reported that participants relying on a trusted source of information were less vaccine hesitant compared to those dependant on social media for updated information regarding the vaccines. Acquiring online information through nonscientific resources was found to reduce the acceptability of the vaccine.Citation64,Citation90
Discussion
This review documented a wide variation (5.4% − 83%) of COVID-19 vaccine hesitancy among countries of the Arab world. Variations were obvious in studies conducted in different countries as well as among the studies conducted in the same country. Hesitancy for booster dose was found to be comparatively less (21.8% − 55.4%). The most commonly reported factors associated with hesitancy included female gender, younger age, previous influenza vaccine uptake, and low education and income level. The most-reported personal concerns were related to the rapid development, safety, and long-term side effects of the vaccine. Moreover, overall lack of trust in government policies toward pandemic control, widespread conspiracy theories about vaccines, and different misconceptions increased the probability of COVID-19 vaccine hesitancy among population in these countries.
With the emergence of COVID-19 virus and infections, vaccine hesitancy became a hot research topic that has been studied extensively all around the globe. Vaccine acceptance ranges from as high as 90% in China to just 55% in Russia, while countries like the USA and Canada reported acceptance rates of 69% and 76.5%, respectively.Citation151 Similar considerable disparity in vaccine acceptance rates in the Arab world was reported in our article. The willingness to receive the vaccine was higher in studies from Saudi Arabia and Kuwait compared to other Arab countries.Citation34,Citation63 The regional and worldwide variations could be attributed to the countries’ differences in the effectiveness of the health systems in dealing with the pandemic, severity of the infection, the number of cases, and the mortality rates across the countries.Citation10 On the other hand, political instability, unfavorable legislation, and financial issues as well as educational status of the people may adversely affect people’s opinions regarding vaccination as evident from differences in VH prevalence between Arabic and Western countries.Citation11,Citation12 Other reasons may include conspiracy theories rooted in religious concerns and misinformation disseminated through various media platforms.Citation14,Citation152 Variations in vaccine hesitancy were also evident from studies within the same country. For example, studies in Egypt reported hesitancy rates ranging from 12%Citation21 to 79%Citation18 depending on the studied area, such as urban or rural background, and the studied population (general population vs university students).
Interestingly, the high levels of vaccine hesitancy were not reflected in the vaccination rates. For instance, in the UAE, despite relatively high hesitancy rates (31.8% −75.6%), the vaccination rates are very high.Citation72 This could be related to the carefully planned and implemented effective policies that ensured vaccination of all community members.Citation153 The reviewed studies listed various factors that influence vaccine hesitancy among the studied populations. It was found that younger age, female gender or low levels of education are associated with high hesitancy levels, while previous intake of Influenza vaccine was perceived to increase the motivation to accept COVID-19 vaccination. Other reasons for the increased uptake of COVID-19 vaccines such as working in healthcare related profession, preexisting chronic diseases, good knowledge of COVID-19 disease and immigrant status, were also reported in a previous review on global hesitancy.Citation151
Previous studies have found a clear association between the female gender and hesitancy. It is suggested that the influence of gender on the decision is most probably related to high anxiety levels in females in general and fear of needles in particular.Citation157 Moreover, pregnancy and breastfeeding are sensitive health matters that require careful considerations and decisions for vaccine uptake in this population. The higher vaccine hesitancy rates in younger individuals may be related to the focus of the vaccination campaign on the elderly, providing false assurance for the younger generation that they are immune to the disease.Citation62 Previous Influenza vaccination uptake was found to be associated with increased COVID-19 vaccine acceptance in this review, as reported in another study conducted in the UK.Citation154 A recent review summarizing the coverage of Influenza vaccine in sixteen countries of WHO Eastern Mediterranean region informed that the vaccine was available free of charge to general public or at risk groups in most (81%) of these countries. However, the availability depended upon the resources and socioeconomic status of the country.Citation155
A commonly stated concern related to the vaccines was emergency authorizations of vaccines which may have triggered questions about the unknown long-term side effects. Other worries were related to mistrust in the governments in general, especially after the chaotic situation that challenged the health systems and exposed all the deficiencies in emergency planning. Some surveys reported that people believe in conspiracy theories related to vaccines’ efficacy and safety, production sites of the vaccines, and the uncertainties around the origin of the disease.Citation29,Citation81 Moreover, self-perception of poor health triggered hesitancyCitation25,Citation114 in contrast to people with chronic illness (hypertension, diabetes, etc.) who were more willing to get vaccinated.Citation51,Citation58,Citation123
Many countries in the Arab region have encountered enormous disasters and tragedies including wars, political conflicts, and natural disasters. COVID-19 pandemic has further deteriorated the conditions of poverty and accessibility to medical treatment as well as vaccination services.Citation156 However, in a study that examined older Syrian refugees living in Lebanon, it was found that the intention to receive the COVID-19 vaccine is higher among those living inside refugee camps compared to those living outside the tented settlement. The study also argued that the vaccination and educational campaigns are overlooking many of those who are not registered informal refugee camps.Citation35
Despite the inclusion of many high-quality studies in this review, there were some limitations, inconsistencies were noted with the definition and scope of hesitancy, classifying hesitancy and refusal separately in many studies conducted in the Arab world, as the standard definition developed by WHO for hesitancy was not followed. However, in this review, we have reported hesitancy as defined by WHO and prevalence might not be very precise given the large variation in the reported data. Another limitation is that most of the surveys conducted in the studies included in this review were carried out online, which is justifiable given the social distancing measures. However, this means that a large number of individuals from the Arab population were underrepresented such as those who do not have internet access, those from the low socio-economic strata especially people with low levels of education and older adults. Future studies are warranted to investigate the prevalence of COVID-19 vaccine hesitancy and associated factors in all subgroups of the population. Critical appraisal of the included studies, as well as meta-analysis to measure strength of association between VH and its predictors was not conducted. It would have added further to the evidence, yet with the coverage of extensive number of studies and given objective of the review, it was not feasible. Additionally, the review did not address parents’ attitudes toward vaccination in the children. These limitations could potentially be addressed in future reviews.
Conclusion
In summary this review provided an overview of evidence on COVID-19 VH levels in the countries of Arab world and most commonly reported factors associated with it. Results suggested varied COVID-19 VH prevalence across different Arab countries. Most common factors associated with COVID-19 VH as reported in the studies included female gender, young age, low educational level and lack of previous vaccination against Influenza. Strategies for proper information dissemination and clarification of misconceptions regarding the vaccine are required. This will lead to improvement in vaccination uptake, thus preventing mortality and morbidity from the infection when acquired, in the future.
CRediT authorship contribution statement
ZA: Literature search, data extraction, data analysis, initial manuscript drafting, revision of manuscript; SM: Literature search, data extraction, data analysis, initial manuscript drafting; JN: Critical review; R Al-R: Critical review, LA: Critical review; IE: Concepualisation, Supervision, Critical review.
Supplemental Material
Download PDF (227.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2245720.
Additional information
Funding
References
- Anka AU, Tahir MI, Abubakar SD, Alsabbagh M, Zian Z, Hamedifar H, Sabzevari A, Azizi G. Coronavirus disease 2019 (COVID-19): an overview of the immunopathology, serological diagnosis and management. Scand J Immunol. 2021;93(4):e12998. doi:10.1111/sji.12998.
- Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, Roser M. Coronavirus pandemic (COVID-19). Our World Data; 2023 [accessed 2023 Feb 25]. https://ourworldindata.org/coronavirus.
- Li Y-D, Chi W-Y, Su J-H, Ferrall L, Hung C-F, Wu T-C. Coronavirus vaccine development: from SARS and MERS to COVID-19. J Biomed Sci. 2020;27(1). doi:10.1186/s12929-020-00695-2.
- Macdonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–16. doi:10.1016/j.vaccine.2015.04.036.
- World Health Organization. Ten Threats to global health in 2019. 2019 [accessed 2021 Nov 21]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1763–73. doi:10.4161/hv.24657.
- Worldometer. Demographics of world population. 2021 [accessed 2023 Feb 15]. https://www.worldometers.info/population/.
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf Dis. 2020;20(5):533–4. doi:10.1016/S1473-3099(20)30120-1.
- Basta NE, Moodie EMM VIPER (vaccines, infectious disease prevention, and epidemiology research) group COVID-19 vaccine development and approvals tracker team. COVID-19 vaccine development and approvals Tracker. 2022. https://covid19.trackvaccines.org/trials-vaccines-by-country/#approvals.
- Mallah SI, Ghorab OK, Al-Salmi S, Abdellatif OS, Tharmaratnam T, Iskandar MA, Sefen JAN, Sidhu P, Atallah B, El-Lababidi R, et al. COVID-19: breaking down a global health crisis. Ann Clin Microbiol Antimicrob. 2021;20(1):35. doi:10.1186/s12941-021-00438-7.
- Aw J, Seng JJB, Seah SSY, Low LL. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines (Basel). 2021;9(8):900. doi:10.3390/vaccines9080900.
- Tagoe ET, Sheikh N, Morton A, Nonvignon J, Sarker AR, Williams L, Megiddo I. COVID-19 vaccination in lower-middle income countries: national stakeholder views on challenges, barriers, and potential solutions. Front Public Health. 2021;9:709127. doi:10.3389/fpubh.2021.709127.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021 Feb 16;9(2):160. doi:10.3390/vaccines9020160.
- Biswas MR, Alzubaidi MS, Shah U, Abd-Alrazaq AA, Shah Z. A scoping review to find out worldwide COVID-19 vaccine hesitancy and its underlying determinants. Vaccines. 2021 Oct 25;9(11):1243. doi:10.3390/vaccines9111243.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005 Feb 1;8(1):19–32. doi:10.1080/1364557032000119616.
- El-Sokkary RH, El Seifi OS, Hassan HM, Mortada EM, Hashem MK, Gadelrab M, Tash RME. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: a cross-sectional study. BMC Infect Dis. 2021;21(1):762. doi:10.1186/s12879-021-06392-1.
- Elgendy MO, Abdelrahim MEA. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J Med Virol. 2021;93(12):6535–43. doi:10.1002/jmv.27199.
- Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 vaccination perception and attitude among healthcare workers in Egypt. J Prim Care Community Health. 2021;12:21501327211013303. doi:10.1177/21501327211013303.
- Omar DI, Hani BM. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J Infect Public Health. 2021;14(10):1481–8. doi:10.1016/j.jiph.2021.06.019.
- Saied SM, Saied EM, Kabbash IA, Abdo SAEF. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. Journal Of Medical Virology. 2021;93(7):4280–91. doi:10.1002/jmv.26910.
- Hammam N, Tharwat S, Shereef RRE, Elsaman AM, Khalil NM, Fathi HM, Salem MN, El-Saadany HM, Samy N, El-Bahnasawy AS, et al. Rheumatology university faculty opinion on coronavirus disease-19 (COVID-19) vaccines: the vaXurvey study from Egypt. Rheumatol Int. 2021;41(9):1607–16. doi:10.1007/s00296-021-04941-0.
- Abdulah DM. Prevalence and correlates of COVID‐19 vaccine hesitancy in the general public in Iraqi Kurdistan: A cross‐sectional study. J Med Virol. 2021 Dec;93(12):6722–31. doi:10.1002/jmv.27255.
- Al‐Metwali BZ, Al‐Jumaili AA, Al‐Alag ZA, Sorofman B. Exploring the acceptance of COVID‐19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021 Oct;27(5):1112–22. doi:10.1111/jep.13581.
- Al‐Rawashdeh S, Rababa M, Rababa M, Hamaideh S. Predictors of intention to get COVID‐19 vaccine: a cross‐sectional study. InNursing Forum. 2022 Mar;57(2):277–87. doi:10.1111/nuf.12676.
- Abu Farha RK, Alzoubi KH, Khabour OF, Alfaqih MA. Exploring perception and hesitancy toward COVID-19 vaccine: a study from Jordan. Hum Vaccin Immunother. 2021;17(8):2415–20. doi:10.1080/21645515.2021.1888633.
- Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a middle Eastern population. Front Public Health. 2021;9:632914. doi:10.3389/fpubh.2021.632914.
- El-Elimat T, AbuAlsamen MM, Almomani BA, Al-Sawalha NA, Alali FQ, Di Gennaro F. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021 Apr 23;16(4):e0250555. doi:10.1371/journal.pone.0250555.
- Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, Al-Haidar A, Yaseen A, Ababneh NA, Assaf A, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among University students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. doi:10.3390/ijerph18052407.
- Al-Ayyadhi N, Ramadan MM, Al-Tayar E, Al-Mathkouri R, Al-Awadhi S. Determinants of hesitancy towards COVID-19 vaccines in state of Kuwait: an exploratory internet-based survey. Risk Manag Healthc Policy. 2021 Dec;14:4967–81. doi:10.2147/RMHP.S338520.
- Al-Sanafi M, Sallam M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: a cross-sectional study using the 5C and vaccine conspiracy beliefs scales. Vaccines. 2021 Jun 25;9(7):701. doi:10.3390/vaccines9070701.
- Alawadhi E, Zein D, Mallallah F, Haider NB, Hossain A. Monitoring COVID-19 vaccine acceptance in kuwait during the pandemic: results from a national serial study. Risk Manag Healthc Policy. 2021;14:1413–29. doi:10.2147/RMHP.S300602.
- Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, Almansouri W, Alzalzalah S, Ziyab AH. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30(3):262–71. doi:10.1159/000514636.
- Burhamah W, AlKhayyat A, Oroszlányová M, AlKenane A, Jafar H, Behbehani M, Almansouri A. The SARS-CoV-2 vaccine hesitancy among the general population: a large cross-sectional study from Kuwait. Cureus. 2021 Jul 8;13(7). doi:10.7759/cureus.16261.
- Salibi N, Abdulrahim S, El Haddad M, Bassil S, El Khoury Z, Ghattas H, McCall SJ. COVID-19 vaccine acceptance in older Syrian refugees: preliminary findings from an ongoing study. Prev Med Rep. 2021 Dec 1;24:101606. doi:10.1016/j.pmedr.2021.101606.
- Moujaess E, Zeid NB, Samaha R, Sawan J, Kourie H, Labaki C, Chebel R, Chahine G, Karak FE, Nasr F, et al. Perceptions of the COVID-19 vaccine among patients with cancer: a single-institution survey. Future Oncol. 2021 Jul;17(31):4071–9. doi:10.2217/fon-2021-0265.
- Bou Hamdan M, Singh S, Polavarapu M, Jordan TR, Melhem NM. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol Infect. 2021;149:e242. doi:10.1017/S0950268821002314.
- Kasrine Al Halabi C, Obeid S, Sacre H, Akel M, Hallit R, Salameh P, Hallit S. Attitudes of lebanese adults regarding COVID-19 vaccination. BMC Public Health. 2021 May 27;21(1):998. doi:10.1186/s12889-021-10902-w.
- Nasr L, Saleh N, Hleyhel M, El-Outa A, Noujeim Z. Acceptance of COVID-19 vaccination and its determinants among lebanese dentists: a cross-sectional study. BMC Oral Health. 2021 Dec;21(1):1–0. doi:10.1186/s12903-021-01831-6.
- Elhadi M, Alsoufi A, Alhadi A, Hmeida A, Alshareea E, Dokali M, Abodabos S, Alsadiq O, Abdelkabir M, Ashini A, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross-sectional study. BMC Public Health. 2021 May 20;21(1):955. doi:10.1186/s12889-021-10987-3.
- Khamis F, Badahdah A, Al Mahyijari N, Al Lawati F, Al Noamani J, Al Salmi I, Al Bahrani M. Attitudes towards COVID-19 vaccine: a survey of health care workers in Oman. J Epidemiol Global Health. 2022 Mar;12(1):1–6. doi:10.1007/s44197-021-00018-0.
- Zawahrah HJ, Saca-Hazboun H, Melhem SS, Adwan R, Sabateen A, Abu-Rmeileh NM. Acceptance of COVID-19 vaccines in Palestine: a cross-sectional online study. BMJ Open. 2021 Oct 1;11(10):e053681. doi:10.1136/bmjopen-2021-053681.
- Maraqa B, Nazzal Z, Rabi R, Sarhan N, Al-Shakhra K, Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: a call for action. Prev Med. 2021 Aug 1;149:106618. doi:10.1016/j.ypmed.2021.106618.
- Zaidi A, Elmasaad A, Alobaidli H, Sayed R, Al-Ali D, Al-Kuwari D, Al-Kubaisi S, Mekki Y, Emara MM, Daher-Nashif S. Attitudes and intentions toward COVID-19 vaccination among Health professions students and faculty in Qatar. Vaccines. 2021 Nov;9(11):1275. doi:10.3390/vaccines9111275.
- Al-Mulla R, Abu-Madi M, Talafha QM, Tayyem RF, Abdallah AM. COVID-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines. 2021 Jun 18;9(6):665. doi:10.3390/vaccines9060665.
- Alabdulla M, Reagu SM, Al‐Khal A, Elzain M, Jones RM. COVID‐19 vaccine hesitancy and attitudes in Qatar: a national cross‐sectional survey of a migrant‐majority population. Influenza Other Respir Viruses. 2021 May;15(3):361–70. doi:10.1111/irv.12847.
- Khaled SM, Petcu C, Bader L, Amro I, Al-Hamadi AM, Al Assi M, Ali AA, Le Trung K, Diop A, Bellaj T, et al. Prevalence and potential determinants of COVID-19 vaccine hesitancy and resistance in Qatar: results from a nationally representative survey of Qatari nationals and migrants between December 2020 and January 2021. Vaccines. 2021 May 7;9(5):471. doi:10.3390/vaccines9050471.
- Kumar R, Alabdulla M, Elhassan NM, Reagu SM. Qatar healthcare workers’ COVID-19 vaccine hesitancy and attitudes: a national cross-sectional survey. Public Health Front. 2021 Aug 25;9:727748. doi:10.3389/fpubh.2021.727748.
- Samannodi M. COVID-19 vaccine acceptability among women who are pregnant or planning for pregnancy in Saudi Arabia: a cross-sectional study. Patient Prefer Adherence. 2021 Nov 23;15:2609–18. doi:10.2147/PPA.S338932.
- Narapureddy BR, Muzammil K, Alshahrani MY, Alkhathami AG, Alsabaani A, AlShahrani AM, Dawria A, Nasir N, Kalyan Viswanath Reddy L, Alam MM. COVID-19 vaccine acceptance: beliefs and barriers associated with vaccination among the residents of KSA. J Multidisciplin Healthcare. 2021 Nov 24;Volume 14:3243–52. doi:10.2147/JMDH.S340431.
- Barry M, Temsah MH, Alhuzaimi A, Alamro N, Al-Eyadhy A, Aljamaan F, Saddik B, Alhaboob A, Alsohime F, Alhasan K, et al. COVID-19 vaccine confidence and hesitancy among health care workers: a cross-sectional survey from a MERS-CoV experienced nation. PLoS One. 2021 Nov 29;16(11):e0244415. doi:10.1371/journal.pone.0244415.
- Altulahi N, AlNujaim S, Alabdulqader A, Alkharashi A, AlMalki A, AlSiari F, Bashawri Y, Alsubaie S, AlShahrani D, AlGoraini Y. Willingness, beliefs, and barriers regarding the COVID-19 vaccine in Saudi Arabia: a multiregional cross-sectional study. BMC Fam Pract. 2021 Dec;22(1):1–1. doi:10.1186/s12875-021-01606-6.
- AlSaeed AA, Rabbani U. Explaining COVID-19 vaccine rejection using social cognitive theory in Qassim, Saudi Arabia. Vaccines. 2021 Nov 9;9(11):1304. doi:10.3390/vaccines9111304.
- Alghamdi AA, Aldosari MS, Alsaeed RA. Acceptance and barriers of COVID-19 vaccination among people with chronic diseases in Saudi Arabia. J Infect Dev Ctries. 2021 Nov 30;15(11):1646–52. doi:10.3855/jidc.15063.
- Aldosary AH, Alayed GH. Willingness to vaccinate against Novel COVID-19 and contributing factors for the acceptance among nurses in Qassim, Saudi Arabia. Eur Rev Med Pharmacol Sci. 2021 Oct 1;25(20):6386–96. doi:10.26355/eurrev_202110_27012.
- Alamer E, Hakami F, Hamdi S, Alamer A, Awaf M, Darraj H, Abutalib Y, Madkhali E, Alamer R, Bakri N, et al. Knowledge, attitudes and perception toward COVID-19 vaccines among adults in Jazan Province, Saudi Arabia. Vaccines. 2021 Nov 1;9(11):1259. doi:10.3390/vaccines9111259.
- Alshahrani NZ, Alshahrani SM, Farag S, Rashid H. Domestic Saudi Arabian travellers’ understanding about Covid-19 and its vaccination. Vaccines. 2021 Aug 12;9(8):895. doi:10.3390/vaccines9080895.
- Al-Hanawi MK, Alshareef N, El-Sokkary RH. Willingness to receive COVID-19 vaccination among older adults in Saudi Arabia: a community-based survey. Vaccines. 2021 Nov;9(11):1257. doi:10.3390/vaccines9111257.
- Al-Mansour K, Alyahya S, AbuGazalah F, Alabdulkareem K. Factors affecting COVID-19 vaccination among the general population in Saudi Arabia. Healthcare. 2021 Sep 16;9(9):1218. doi:10.3390/healthcare9091218.
- Al-Mohaithef M, Padhi BK, Ennaceur S. Socio-demographics correlate of COVID-19 vaccine hesitancy during the second wave of COVID-19 pandemic: a cross-sectional web-based survey in Saudi Arabia. Public Health Front. 2021 Jun 24;9:698106. doi:10.3389/fpubh.2021.698106.
- Aldossari KK, Alharbi MB, Alkahtani SM, Alrowaily TZ, Alshaikhi AM, Twair AA. COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Diabetes Metab syndr. 2021 Sep 1;15(5):102271. doi:10.1016/j.dsx.2021.102271.
- Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines. 2021 Mar 5;9(3):226. doi:10.3390/vaccines9030226.
- Almaghaslah D, Alsayari A, Kandasamy G, Vasudevan R. COVID-19 vaccine hesitancy among young adults in Saudi Arabia: a cross-sectional web-based study. Vaccines. 2021 Apr 1;9(4):330. doi:10.3390/vaccines9040330.
- Almalki MJ, Alotaibi AA, Alabdali SH, Zaalah AA, Maghfuri MW, Qirati NH, Jandali YM, Almalki SM. Acceptability of the COVID-19 vaccine and its determinants among university students in Saudi Arabia: a cross-sectional study. Vaccines. 2021 Aug 25;9(9):943. doi:10.3390/vaccines9090943.
- Alshahrani SM, Dehom S, Almutairi D, Alnasser BS, Alsaif B, Alabdrabalnabi AA, Bin Rahmah A, Alshahrani MS, El-Metwally A, Al-Khateeb BF, et al. Acceptability of COVID-19 vaccination in Saudi Arabia: a cross-sectional study using a web-based survey. Hum Vaccin Immunotherap. 2021 Oct 3;17(10):3338–47. doi:10.1080/21645515.2021.1936869.
- Magadmi RM, Kamel FO. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021 Dec;21(1):1–8. doi:10.1186/s12889-021-11501-5.
- Mahmud I, Kabir R, Rahman MA, Alradie-Mohamed A, Vinnakota D, Al-Mohaimeed A. The health belief model predicts intention to receive the COVID-19 vaccine in Saudi Arabia: results from a cross-sectional survey. Vaccines. 2021 Aug 5;9(8):864. doi:10.3390/vaccines9080864.
- Noushad M, Nassani MZ, Koppolu P, Alsalhani AB, Samran A, Alqerban A, Abusalim GS, Barakat A, Alshalhoub MB, Rastam S. Predictors of COVID-19 vaccine intention among the saudi arabian population: a cross-sectional survey. Vaccines. 2021 Aug 12;9(8):892. doi:10.3390/vaccines9080892.
- Qattan AM, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021 Mar 1;8:644300. doi:10.3389/fmed.2021.644300.
- Zahid HM, Alsayb MA. Assessing the knowledge and attitude toward COVID-19 vaccination in Saudi Arabia. Inter J Environ Res Public Health. 2021 Aug 2;18(15):8185. doi:10.3390/ijerph18158185.
- Ahmed MA, Colebunders R, Gele AA, Farah AA, Osman S, Guled IA, Abdullahi AA, Hussein AM, Ali AM, Siewe Fodjo JN. COVID-19 vaccine acceptability and adherence to preventive measures in Somalia: results of an online survey. Vaccines. 2021 May 21;9(6):543. doi:10.3390/vaccines9060543.
- Mohamad O, Zamlout A, AlKhoury N, Mazloum AA, Alsalkini M, Shaaban R. Factors associated with the intention of Syrian adult population to accept COVID-19 vaccination: a cross-sectional study. BMC Public Health. 2021 Dec;21(1):1–0. doi:10.1186/s12889-021-11361-z.
- Ahamed F, Ganesan S, James A, Zaher WA. Understanding perception and acceptance of Sinopharm vaccine and vaccination against COVID–19 in the UAE. BMC Public Health. 2021 Dec;21(1):1–1. doi:10.1186/s12889-021-11620-z.
- Albahri AH, Alnaqbi SA, Alshaali AO, Alnaqbi SA, Shahdoor SM. COVID-19 vaccine acceptance in a sample from the United Arab Emirates general adult population: a cross-sectional survey, 2020. Public Health Front. 2021;9:1075. doi:10.3389/fpubh.2021.614499.
- Albahri AH, Alnaqbi SA, Alnaqbi SA, Alshaali AO, Shahdoor SM. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in primary healthcare centers in Dubai: a cross-sectional survey, 2020. Public Health Front. 2021 Jul 28;9:617679. doi:10.3389/fpubh.2021.617679.
- Alremeithi HM, Alghefli AK, Almadhani R, Baynouna AlKetbi LM. Knowledge, attitude, and practices toward SARS-COV-2 infection in the United Arab Emirates population: an online community-based cross-sectional survey. Public Health Front. 2021;9:687628.
- Alzubaidi H, Samorinha C, Saddik B, Saidawi W, Abduelkarem AR, Abu-Gharbieh E, Sherman SM. A mixed-methods study to assess COVID-19 vaccination acceptability among university students in the United Arab Emirates. Hum Vaccin Immunotherap. 2021 Nov 2;17(11):4074–82. doi:10.1080/21645515.2021.1969854.
- Harapan H, Anwar S, Yufika A, Sharun K, Gachabayov M, Fahriani M, Husnah M, Raad R, Abdalla RY, Adam RY, et al. Vaccine hesitancy among communities in ten countries in Asia, Africa, and South America during the COVID-19 pandemic. Pathog Glob Health. 2022 May 19;116(4):236–43. doi:10.1080/20477724.2021.2011580.
- Anjorin AA, Odetokun IA, Abioye AI, Elnadi H, Umoren MV, Damaris BF, Eyedo J, Umar HI, Nyandwi JB, Abdalla MM, et al. Will Africans take COVID-19 vaccination? PLoS One. 2021;16(12):e0260575. doi:10.1371/journal.pone.0260575.
- Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Glob Health Res Policy. 2021 Dec;6(1):1–7. doi:10.1186/s41256-021-00202-6.
- Abu-Farha R, Mukattash T, Itani R, Karout S, Khojah HM, Al-Mahmood AA, Alzoubi KH. Willingness of middle Eastern public to receive COVID-19 vaccines. Saudi Pharm J. 2021 Jul 1;29(7):734–9. doi:10.1016/j.jsps.2021.05.005.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021 Jan 12;9(1):42. doi:10.3390/vaccines9010042.
- Qunaibi EA, Helmy M, Basheti I, Sultan I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. Elife. 2021 May 27;10:e68038. doi:10.7554/eLife.68038.
- Qunaibi E, Basheti I, Soudy M, Sultan I. Hesitancy of Arab healthcare workers towards COVID-19 vaccination: a large-scale multinational study. Vaccines. 2021 May 2;9(5):446. doi:10.3390/vaccines9050446.
- Abdou MS, Kheirallah KA, Aly MO, Ramadan A, Elhadi YAM, Elbarazi I, Deghidy EA, El Saeh HM, Salem KM, Ghazy RM, et al. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: an online survey in 13 Arab countries. PLoS One. 2021;16(11):e0260321. doi: 10.1371/journal.pone.0260321.
- Sitarz R, Forma A, Karakuła K, Juchnowicz D, Baj J, Bogucki J, Rog J, Tee ML, Tee CA, Ly-Uson JT, et al. To vaccinate or not to vaccinate—reasons of willingness and reluctance of students against SARS-CoV-2 vaccination—an International experience. Intl J Env Res Public Health. 2022 Oct 27;19(21):14012. doi:10.3390/ijerph192114012.
- Waheed A, Bakr Elsaid NM A, Ghweeba M, Elmaraghy N, Al-Touny SA, Nemr N, Kishk RM, Aly HM. Determinants of coronavirus disease 2019 vaccine acceptance, hesitancy, and barriers among healthcare workers in Ismailia, Egypt: a mixed methods study. J Egypt Public Health Assoc. 2022 Dec;97(1):1–3. doi:10.1186/s42506-022-00122-4.
- El-Hneiti M, Shaheen A, Malak MZ, Al-Hussami R, Al-Hiary SS, Elfalah M, Al-Hussami M. The Willingness of the healthcare professionals working in healthcare Institutions to accept the First dose of COVID-19 vaccine in Jordan: a national survey. Vaccines. 2022 Jul 17;10(7):1138. doi:10.3390/vaccines10071138.
- Saikarthik J, Saraswathi I, Senthil Kumar K, Al Assaf A, Al Jabr A, Anand P, Suresh M, Hawsah YM, Aldawish AS. Contrasting association between COVID-19 vaccine hesitancy and mental health status in India and Saudi Arabia-A preliminary evidence collected during the second wave of COVID-19 pandemic. Front Med. 2022 May;4:1172.
- Amer SA, Shah J, Abd-Ellatif EE, El Maghawry HA. COVID-19 vaccine uptake among physicians during the second wave of COVID-19 pandemic: attitude, intentions, and determinants: a cross-sectional study. Public Health Front. 2022;10. doi:10.3389/fpubh.2022.823217.
- Majer J, Elhissi JH, Mousa N, Kostandova N. COVID-19 vaccination in the Gaza Strip: a cross-sectional study of vaccine coverage, hesitancy, and associated risk factors among community members and healthcare workers. Confl Health. 2022 Dec;16(1):1–31. doi:10.1186/s13031-022-00477-7.
- Baklouti M, Ben Ayed H, Maamri H, Ketata N, Yaich S, Karray R, Jdidi J, Mejdoub Y, Kassis M, Feki H, et al. Prevalence and factors affecting Willingness to accept or refuse vaccination against COVID-19 among healthcare professionals in Southern Tunisia. Hosp Top. 2022 Aug;10:1–0. doi:10.1080/00185868.2022.2111287.
- Ali Z, Perera SM, Garbern SC, Diwan EA, Othman A, Ali J, Awada N. Variations in COVID-19 vaccine attitudes and acceptance among refugees and Lebanese nationals pre-and post-vaccine rollout in Lebanon. Vaccines. 2022 Sep 15;10(9):1533. doi:10.3390/vaccines10091533.
- Noushad M, Al-Awar MS, Al-Saqqaf IS, Nassani MZ, Alrubaiee GG, Rastam S. Lack of access to coronavirus disease 2019 vaccines could be a greater threat than vaccine hesitancy in low-income and conflict nations: the case of Yemen. Clin Infect Dis. 2022 Nov 15;75(10):1827–33. doi:10.1093/cid/ciac088.
- El-Ghitany EM, Ashour A, Omran EA, Farghaly AG, Hassaan MA, Azzam NF. COVID-19 vaccine acceptance rates and predictors among the Egyptian general population and healthcare workers, the intersectionality of age and other factors. Sci Rep. 2022 Nov 18;12(1):19832. doi:10.1038/s41598-022-23825-2.
- Al-Hatamleh MA, Hatmal MM, Mustafa SH, Alzu’bi M, AlSou’b AF, Abughanam SN, Olaimat AN, Kateeb ET, Mohamud R. Experiences and perceptions of COVID-19 infection and vaccination among Palestinian refugees in Jerash camp and Jordanian citizens: a comparative cross-sectional study by face-to-face interviews. Infect Dis Poverty. 2022 Dec;11(1):1–20. doi:10.1186/s40249-022-01047-y.
- Al-Qerem W, Jarab AS, Qarqaz R, Hayek MA. Attitudes of a sample of Jordanian young adults toward different available COVID-19 vaccines. Vacunas (English Edition) 2022 Aug 1;23:55–62.
- Mahmud I, Al Imam MH, Vinnakota D, Kheirallah KA, Jaber MF, Abalkhail A, Alasqah I, Alslamah T, Kabir R. Vaccination intention against COVID-19 among the unvaccinated in Jordan during the Early Phase of the vaccination drive: a cross-sectional survey. Vaccines. 2022 Jul 21;10(7):1159. doi:10.3390/vaccines10071159.
- Shehata WM, Elshora AA, Abu-Elenin MM. Physicians’ attitudes and acceptance regarding COVID-19 vaccines: a cross-sectional study in mid Delta region of Egypt. Environ Sci Pollut Res. 2022 Mar;1:1–1.
- Elbadawi MH, Altayib LS, Birier AB, Ali LE, Hasabo EA, Esmaeel MA, Elmahi OK, Group of collaborators. Beliefs and barriers of COVID-19 vaccination hesitancy among sudanese healthcare workers in Sudan: a cross sectional study. Hum Vaccin Immunother. 2022 Nov 30;18(6):2132082. doi:10.1080/21645515.2022.2132082.
- Lataifeh L, Al-Ani A, Lataifeh I, Ammar K, AlOmary A, Al-Hammouri F, Al-Hussaini M. Knowledge, attitudes, and practices of healthcare workers in Jordan towards the COVID-19 vaccination. Vaccines. 2022 Feb 9;10(2):263. doi:10.3390/vaccines10020263.
- Sharaf M, Taqa O, Mousa H, Badran A. COVID-19 vaccine acceptance and perceptions among dental teaching staff of a governmental university in Egypt. J Egypt Public Health Assoc. 2022 Apr 21;97(1):9. doi:10.1186/s42506-022-00104-6.
- Boshra MS, Hussein RR, Mohsen M, Elberry AA, Altyar AE, Tammam M, Sarhan RM. A battle against COVID-19: vaccine hesitancy and awareness with a comparative study between Sinopharm and AstraZeneca. Vaccines. 2022 Feb 15;10(2):292. doi:10.3390/vaccines10020292.
- Al Awaidy ST, Al Siyabi H, Khatiwada M, Al Siyabi A, Al Mukhaini S, Dochez C, Giron DM, Langrial SU, Mahomed O. Assessing COVID-19 vaccine’s acceptability amongst Health Care workers in Oman: a cross-sectional study. J Infect Public Health. 2022 Aug 1;15(8):906–14. doi:10.1016/j.jiph.2022.06.005.
- Abdelkader FA, Alkubati SA, Alsabri M, McClean C, Albagawi B, Alsaqri SH, Al-Areefi M, Abo Seada AI. COVID-19 vaccination knowledge, perception, and reason for adherence and nonadherence among Nursing students in Egypt. SAGE Open Nurs. 2022 Nov;8:23779608221141234. doi:10.1177/23779608221141234.
- Abuhammad S. Attitude of pregnant and lactating women toward COVID-19 vaccination in Jordan: a cross-sectional study. J Perinat Med. 2022 Sep 1;50(7):896–903. doi:10.1515/jpm-2022-0026.
- Noushad M, Nassani MZ, Al-Awar MS, Al-Saqqaf IS, Mohammed SO, Samran A, Yaroko AA, Barakat A, Elmi OS, Alsalhani AB, et al. COVID-19 vaccine hesitancy associated with vaccine iniequity among healthcare workers in a low-income Fragile Nation. Public Health Front. 2022;10. doi:10.3389/fpubh.2022.914943.
- Talafha QM, Al-Haidose A, AlSamman AY, Abdallah SA, Istaiteyeh R, Ibrahim WN, Hatmal MM, Abdallah AM. COVID-19 vaccine acceptance among vulnerable Groups: Syrian refugees in Jordan. Vaccines. 2022 Sep 28;10(10):1634. doi:10.3390/vaccines10101634.
- Shareef LG, Al-Hussainy AF, Hameed SM. COVID-19 vaccination hesitancy among Iraqi general population between beliefs and barriers: an observational study. F1000Res. 2022;11. doi:10.12688/f1000research.110545.2.
- Nemr N, Kishk RM, Soliman NH, Farghaly RM, Kishk SM, Louis N. Perception of COVID-19 and vaccine acceptance among healthcare workers. Iran J Pediatr Hematol Oncol. 2022 Dec 2;2022:1–13. doi:10.1155/2022/1607441.
- Tharwat S, Nassar DK, Nassar MK, Saad AM, Hamdy F. Attitude towards COVID-19 vaccination among healthcare workers: a cross sectional study from Egypt. BMC Health Serv Res. 2022 Dec;22(1):1–2. doi:10.1186/s12913-022-08751-3.
- Jam M, Alqahtani M, Amer KA, Althubait B, Aldosari AAS, Al Mudawi AAM.COVID-19 and vaccine hesitancy: individual determinants among Saudis in Asir region. Cureus. 2022 Feb 17;14(2):e22331. doi:10.7759/cureus.22331.
- Raja SM, Osman ME, Musa AO, Hussien AA, Yusuf K, Patel SKS. COVID-19 vaccine acceptance, hesitancy, and associated factors among medical students in Sudan. PLoS One. 2022 Apr 7;17(4):e0266670. doi:10.1371/journal.pone.0266670.
- Luma AH, Haveen AH, Faiq BB, Stefania M, Leonardo EG. Hesitancy towards Covid-19 vaccination among the healthcare workers in Iraqi Kurdistan. Public Health Pract. 2022 Jun 1;3:100222. doi:10.1016/j.puhip.2021.100222.
- Abdullah M, Shahait AD, Qaisieh R, Al-Ramahi M, Bader G, AbuRajab MO, Haddad TA, Al-Omari AY, Issa MS, Bader T, et al. Perspectives on COVID-19 vaccines and its hesitancy among jordanian population. Cureus. 2022 Jun 26;14(6). doi:10.7759/cureus.26337.
- Darweesh O, Khatab N, Kheder R, Mohammed T, Faraj T, Ali S, Ameen M, Kamal-Aldin A, Alswes M, Al-Jomah N, et al. Assessment of COVID-19 vaccination among healthcare workers in Iraq; adverse effects and hesitancy. PLoS One. 2022 Nov 18;17(11):e0274526. doi:10.1371/journal.pone.0274526.
- Nusair MB, Arabyat R, Khasawneh R, Al-Azzam S, Nusir AT, Alhayek MY. Assessment of the relationship between COVID-19 risk perception and vaccine acceptance: a cross-sectional study in Jordan. Hum Vaccin Immunother. 2022 Jan 31;18(1):2017734. doi:10.1080/21645515.2021.2017734.
- Yassin EO, Faroug HA, Ishaq ZB, Mustafa MM, Idris MM, Widatallah SE, El-Raheem A, Hamad GO, Suliman MY. COVID-19 vaccination acceptance among healthcare staff in Sudan, 2021. J Immun Res. 2022 Feb 9;2022:1–11. doi:10.1155/2022/3392667.
- El Kibbi L, Metawee M, Hmamouchi I, Abdulateef N, Halabi H, Eissa M, El Rakawi M, Masri B, Abutiban F, Hamdi W, et al. Acceptability of the COVID-19 vaccine among patients with chronic rheumatic diseases and health-care professionals: a cross-sectional study in 19 Arab countries. Lancet Rheumatol. 2022 Mar 1;4(3):e160–3. doi:10.1016/S2665-9913(21)00368-4.
- Kacimi SE, Klouche-Djedid SN, Riffi O, Belaouni HA, Yasmin F, Essar MY, Taouza FA, Belakhdar Y, Fellah SC, Benmelouka AY, et al. Determinants of COVID-19 vaccine engagement in Algeria: a population-based study with systematic review of studies from Arab countries of the MENA region. Public Health Front. 2022;10. doi:10.3389/fpubh.2022.843449.
- Kurdee Z, Al-Shouli S, AlAfaleq N, Meo SA, Alshahrani A, Alshehri A, Alkathiri N, Bin Saiedan S, Alzahrani Y. Public perception towards the COVID-19 vaccine in Riyadh, Saudi Arabia. Vaccine. 2022 May 28;10(6):867. doi:10.3390/vaccines10060867.
- Salman M, Mallhi TH, Tanveer N, Shehzadi N, Khan HM, Mustafa ZU, Khan TM, Hussain K, Mohamed MS, Maqbool F, et al. Evaluation of conspiracy beliefs, vaccine hesitancy, and Willingness to Pay towards COVID-19 vaccines in Six countries from Asian and African regions: a large multinational analysis. Vaccines. 2022 Nov 4;10(11):1866. doi:10.3390/vaccines10111866.
- Othman SS, Alsuwaidi A, Aseel R, Alotaibi R, Bablgoom R, Alsulami G, Alharbi R, Ghamri R. Association between social media use and the acceptance of COVID-19 vaccination among the general population in Saudi Arabia–a cross-sectional study. BMC Public Health. 2022 Feb 21;22(1):375. doi:10.1186/s12889-022-12757-1.
- Okmi EA, Almohammadi E, Alaamri O, Alfawaz R, Alomari N, Saleh M, Alsuwailem S, Moafa NJ. Determinants of COVID-19 vaccine acceptance among the general adult population in Saudi Arabia based on the health belief model: a web-based cross-sectional study. Cureus. 2022 Aug 23;14(8). doi:10.7759/cureus.28326.
- Faqihi E, Altwirki A, Mijlad W, Alzarie M, Alqumaizi F, Iqbal M, Alshahrani A, Alzahrani F, Alaqidi M, Alqarni M, et al. Awareness, knowledge, attitudes, and practices before the second wave of the COVID-19 pandemic in Saudi Arabia. Eur Rev Med Pharmacol Sci. 2022 Jan 1;26(13):4926–46. doi:10.26355/eurrev_202207_29217.
- Saddik B, Al-Bluwi N, Shukla A, Barqawi H, Alsayed HA, Sharif-Askari NS, Temsah MH, Bendardaf R, Hamid Q, Halwani R. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: a cross-sectional study from the United Arab Emirates. Hum Vaccin Immunother. 2022 Jan 31;18(1):1–9. doi:10.1080/21645515.2021.1994300.
- Khalafalla HE, Tumambeng MZ, Halawi MH, Masmali EM, Tashari TB, Arishi FH, Shadad RH, Alfaraj SZ, Fathi SM, Mahfouz MS. COVID-19 vaccine hesitancy prevalence and predictors among the students of Jazan University, Saudi Arabia using the health belief model: a cross-sectional study. Vaccines. 2022 Feb 14;10(2):289. doi:10.3390/vaccines10020289.
- Alshahrani SM, Alotaibi A, Almajed E, Alotaibi A, Alotaibi K, Albisher S. Pregnant and breastfeeding women’s attitudes and Fears regarding COVID-19 vaccination: a nationwide cross-sectional study in Saudi Arabia. Int J Women Health. 2022 Dec;31:1629–39. doi:10.2147/IJWH.S387169.
- Mohamed R, White TM, Lazarus JV, Salem A, Kaki R, Marrakchi W, Kheir SG, Amer I, Ahmed FM, Khayat MA, et al. COVID-19 vaccine acceptance and associated factors among people living with HIV in the middle East and North Africa region. South Afr J HIV Med. 2022;23(1). doi:10.4102/sajhivmed.v23i1.1391.
- Almeshari M, Abanomy A, Alzamil Y, Alyahyawi A, Al-Thomali AW, Alshihri AA, Althomali OW. Public acceptance of COVID-19 vaccination among residents of Saudi Arabia: a cross-sectional online study. BMJ Open. 2022 Oct 1;12(10):e058180. doi:10.1136/bmjopen-2021-058180.
- Alshareef N. COVID-19 vaccine acceptance and associated factors among women in Saudi Arabia: a cross-sectional study. Vaccines. 2022 Oct 31;10(11):1842. doi:10.3390/vaccines10111842.
- Abou-Arraj NE, Maddah D, Buhamdan V, Abbas R, Jawad NK, Karaki F, Alami NH, Geldsetzer P. Perceptions of, and obstacles to, SARS-CoV-2 vaccination among adults in Lebanon: cross-sectional Online survey. JMIR Form Res. 2022 Dec 14;6(12):e36827. doi:10.2196/36827.
- Habib SS, Alamri MS, Alkhedr MM, Alkhorijah MA, Jabaan RD, Alanzi MK. Knowledge and attitudes of medical students toward COVID-19 vaccine in Saudi Arabia. Vaccines. 2022 Mar 31;10(4):541. doi:10.3390/vaccines10040541.
- Nour MO, Natto HA. COVID-19 vaccination acceptance and trust among adults in Makkah, Saudi Arabia: a cross-sectional study. J Egypt Public Health Assoc. 2022 Sep 26;97(1):17. doi:10.1186/s42506-022-00116-2.
- Al-Kafarna M, Matar SG, Almadhoon HW, Almaghary BK, Zaazouee MS, Elrashedy AA, Wafi DS, Jabari SD, Salloum OH, Ibrahim EA, et al. Public knowledge, attitude, and acceptance toward COVID-19 vaccines in Palestine: a cross-sectional study. BMC Public Health. 2022 Dec;22(1):1–9. doi:10.1186/s12889-022-12932-4.
- Salem GM, Said RM, Abdelsalam AE. Acceptance rate of COVID-19 vaccination and its predictors in Egypt: an online survey. J Infect Dev Ctries. 2022 Jun 30;16(6):993–1000. doi:10.3855/jidc.15603.
- Ghamri RA, Othman SS, Alhiniah MH, Alelyani RH, Badawi AM, Alshahrani AA. Acceptance of COVID-19 vaccine and associated factors among pregnant women in Saudi Arabia. Patient Prefer Adherence. 2022 Apr 2;Volume 16:861–73. doi:10.2147/PPA.S357653.
- Benayad FZ, Razine R, Haroun AE, Oubaasri A, El Fahim E, Abouqal R, Obtel M. Prevalence and predictive determinants of adherence to vaccination against COVID-19 among mothers who gave birth in the last two years in Morocco. Clin Epidemiol Global Health. 2023 Mar 1;20:101241. doi:10.1016/j.cegh.2023.101241.
- Reagu S, Jones RM, Alabdulla M. COVID-19 vaccine hesitancy and personality traits; results from a large national cross-sectional survey in Qatar. Vaccines. 2023 Jan 16;11(1):189. doi:10.3390/vaccines11010189.
- Al-Ghuraibi M, Dighriri IM, Elrggal ME, Obaid NA. The socio-cultural factors behind the Saudi attitude toward COVID-19 vaccination: a survey-based study. Public Health Front. 2023 Jan 9;10:5293. doi:10.3389/fpubh.2022.1026252.
- Al-Qerem W, Al Bawab AQ, Hammad A, Ling J, Alasmari F. Willingness of the jordanian population to receive a COVID-19 booster dose: a cross-sectional study. Vaccines. 2022 Mar 9;10(3):410. doi:10.3390/vaccines10030410.
- Abullais SS, Arora S, Parveen S, Mahmood SE, Baba SM, Khalid I, Khader MA, Elgib MF. Perceptions, motivation factors, and barriers to a COVID-19 booster immunization in a subpopulation of KSA: a cross-sectional study. Medicine. 2022 Nov 25;101(47):e31669. doi:10.1097/MD.0000000000031669.
- Taybeh EO, Alsharedeh R, Hamadneh S. Mothers’ impressions and beliefs about taking a booster dose for COVID-19 vaccine during pregnancy and Lactation. Cureus. 2022 Dec 15;14(12):e32561. doi:10.7759/cureus.32561.
- Al-Qerem W, Hammad A, Alsajri AH, Al-Hishma SW, Ling J, Mosleh R. COVID-19 vaccination acceptance and its associated factors among the Iraqi population: a cross sectional study. Patient Prefer Adherence. 2022 Feb;5:307–19. doi:10.2147/PPA.S350917.
- Lounis M, Bencherit D, Rais MA, Riad A. COVID-19 vaccine booster hesitancy (VBH) and its drivers in Algeria: national cross-sectional survey-based study. Vaccines. 2022 Apr 15;10(4):621. doi:10.3390/vaccines10040621.
- Abullais SS, Arora S, Al Shahrani M, Khan AA, Al Shahrani W, Mahmood SE, Al Qahtani S, Maqbool M, Saib Jameel A, Saluja P. Knowledge, perception, and acceptance toward the booster dose of COVID-19 vaccine among patients visiting dental clinics in Aseer region of KSA. Hum Vaccin Immunother. 2022 Nov 30;18(6):2095162. doi:10.1080/21645515.2022.2095162.
- Al‐Mugheed K, Al Rawajfah O, Bani‐Issa W, Rababa M. Acceptance, attitudes, and barriers of vaccine booster dose among nursing students: a multicounty survey. J Nurs Manag. 2022 Oct;30(7):3360–7. doi:10.1111/jonm.13791.
- Abouzid M, Ahmed AA, El-Sherif DM, Alonazi WB, Eatmann AI, Alshehri MM, Saleh RN, Ahmed MH, Aziz IA, Abdelslam AE, et al. Attitudes toward receiving COVID-19 booster dose in the middle East and North Africa (MENA) region: a cross-sectional study of 3041 fully vaccinated participants. Vaccines. 2022 Aug 6;10(8):1270. doi:10.3390/vaccines10081270.
- Alobaidi S, Alsolami E, Sherif A, Almahdy M, Elmonier R, Alobaidi WY, Akl A. COVID-19 booster vaccine hesitancy among hemodialysis patients in Saudi Arabia using the Health belief model: a Multi-Centre experience. Vaccines. 2022 Dec 31;11(1):95. doi:10.3390/vaccines11010095.
- Vellappally S, Naik S, Alsadon O, Al-Kheraif AA, Alayadi H, Alsiwat AJ, Kumar A, Hashem M, Varghese N, Thomas NG, et al. Perception of COVID-19 booster dose vaccine among healthcare workers in India and Saudi Arabia. Int J Env Res Public Health. 2022 Jul 22;19(15):8942. doi:10.3390/ijerph19158942.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8. doi:10.1038/s41591-020-1124-9.
- Ullah I, Khan KS, Tahir MJ, Ahmed A, Harapan H. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. 2021 May 1;22(2):93–7. doi:10.1016/j.vacun.2021.01.001.
- Suliman DM, Nawaz FA, Mohanan P, Modber M, Musa MK, Musa MB, El Chbib D, Elhadi YAM, Essar MY, Isa MA, et al. UAE efforts in promoting COVID-19 vaccination and building vaccine confidence. Vaccines. 2021;39(43):6341–5. doi: 10.1016/j.vaccine.2021.09.015.
- Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, Rubin GJ, Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVaccs), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021 Jun 3;17(6):1612–21. doi:10.1080/21645515.2020.1846397.
- Attia R, Abubakar A, Bresee J, Mere O, Khan W. A review of policies and coverage of seasonal influenza vaccination programs in the WHO Eastern Mediterranean region. Influenza Resp Viruses. 2023 Mar 21;17(3):e13126. doi:10.1111/irv.13126.
- Howard S, Krishna G. The world’s refugees remain last in line for COVID-19 vaccines. BMJ. 2022;376:o703. doi:10.1136/bmj.o703.
- Mclenon J, Rogers M. The fear of needles: a systematic review and meta-analysis. J Adv Nurs. 2019;75(1):30–42. doi:10.1111/jan.13818.