ABSTRACT
Vaccination attitudes and uptake can spread within social networks. This study aims to understand the perceived social contagion mechanisms of vaccination uptake in the context of COVID-19 pandemic. Eleven semi-structured interviews were conducted following a purposive sampling of three hesitant, three anti- COVID-19 vaccine and five pro- COVID-19 vaccine (27% females). Thematic Analysis suggested two general themes reflecting the type of contagion: 1) information contagion and 2) behavior contagion. Transcending these themes was the notion of ownership of choice/decision. Almost all participants used the media and experts as the main source of information regarding vaccination. They influenced – and they were being influenced by – friends and family members with whom they share similar traits and attitudes and have a close relationship of trust and intimacy. Also, being exposed to positive attitudes and beliefs toward vaccination and COVID-19 vaccines, enhanced vaccination behaviors. However, the vaccination decision-making process was not perceived as a passive process – there was ownership over the decisions made. This study highlights the perceived mechanisms of social contagion. It also suggests that the meaning individuals pose on their social world is crucial on their decision-making. Policymakers are advised to consider including social networks of individuals and trusted sources (i.e. healthcare providers) when delivering interventions or educational campaigns on vaccinations.
Plain Language Summary
The social contagion theory suggests that people’s attitudes and behaviors can spread from one individual to another in different types of social networks such as families, schools and communities. This study explores how this theory can be applied in vaccination for COVID-19 using a series of interviews with individuals in Cyprus that hold differing views about vaccinations. Participants were screened first on their attitudes toward vaccines and therefore purposively recruited individuals who hold positive, negative and hesitant views toward vaccines. A sample of 11 interviews were included for analysis. Study participants first provided information on their exposure to information about vaccines mainly from the media and the web and most discussed their concerns with a healthcare provider whom they consider the most trusted source of information irrespective of their personal views about vaccines. They further elaborated that other influences such as politicians were not perceived as experts. Participants were mostly influenced on their decision to vaccinate by their family and friends thus those with whom they trusted more and felt more intimate with or they share similar views with. Participants finally demonstrated that exposure to positive attitudes had an impact on themselves and contributed to vaccination. Therefore the meaning people pose on their surrounding world is of utmost importance on their decision-making. In terms of policymaking this study suggests that public health interventions could include trusted sources when delivering campaigns and interventions.
Introduction
Vaccination hesitancy can be contagious, and the attitudes of an individual’s network can be an important facet of one’s decision to vaccinate.Citation1 This phenomenon is referred to as Social Contagion and is defined as “the spread of affect, attitude, or behavior from person A (the ‘initiator’) to person B (the ‘recipient’).”Citation2(p275) Vaccination attitudes can spread within networks and an individual can exhibit behavior modeled by another person or adopt the attitudes of members of their social network.Citation3,Citation4 Examining the influence of social networks on vaccination attitudes and uptake within and beyond the COVID-19 pandemic is vital, as it can inform public health interventions and policies.
As of April 2023, there have been 765,222,932 confirmed cases and 6,921,614 deaths due to COVID-19 globally.Citation5 One of the strategies suggested for preventing the coronavirus spread is the uptake of vaccines.Citation6 Hesitancy toward these vaccines constitutes a public health threat.Citation7 Vaccine hesitancy is defined as a delay in acceptance or refusal of vaccination, despite the availability of vaccines and vaccination services.Citation8 Attitudes (i.e., as being safe or not) regarding hesitancy are suggested to be socially contingent.Citation9
The Social Contagion theory has been applied in various contexts. For example, there have been studies examining the contagion of food choices, obesity, smoking and depression.Citation10–13 Social distancing behaviors during the COVID-19 pandemic were suggested to be contagious, as the contact patterns of people in a given region were significantly influenced by the policies and behaviors of people in other regions.Citation14 Vaccination attitudes and uptake can be similarly spread within social networks. For instance, parents who hold more positive vaccination attitudes have a greater likelihood to get vaccinated or vaccinate their child when they are frequently exposed to positive attitudes.Citation1
There are some theoretical mechanisms that specifically describe how social contagion works. The mechanism of exposure suggests that affect, attitude and behavior may diffuse within groups. For instance, people exposed to positive attitudes and beliefs toward the vaccines, are more likely to get vaccinated.Citation1,Citation15 Homophily – the predisposition to interact with culturally similar others – also plays a role in shaping vaccine attitudes, as individuals are more likely to influence or be influenced by culturally similar others.Citation1 The mechanism of strength of ties, suggests that individuals share their thoughts and intentions mainly with those with whom they have enduring relationships and are inclined to adopt practices from people they trust.Citation16,Citation17 These mechanisms imply that people learn through significant and enduring relationships with others who are like-minded.
However, contagion models have been criticized for conceiving of cultural transmission as a simple and straight-forward interpersonal process.Citation9 What is missing from these explanations, is peoples’ meaning-making.Citation18 This is important, as the perceived value of adopting a cultural practice depends on how it is interpreted (i.e., those exposed to the same information might still behave differently).Citation9,Citation19 Also, the Theory of Associative Diffusion states that there are two stages/cognitive mechanisms that affect a person’s propensity to reenact an observed behavior.Citation9 Firstly, the person interprets another individual’s behavior and then evaluates that behavior.Citation19 A qualitative approach will enable an understanding of meaning-making regarding how people perceive vaccines. To our knowledge, there is no study to date examining the social contagion mechanisms of attitudes and behaviors related to COVID-19 vaccines.
This study aims to qualitatively explore the mechanisms of social contagion of vaccination uptake in the context of COVID- 19. The primary research question is:
How and in what way does the social environment affect an individual’s choice to get vaccinated or not?
The secondary and explanatory research questions are:
(2) What are people’s perceptions about the importance of vaccines?
(3) What are the barriers to COVID-19 vaccine acceptance?
Method
Design
This was a qualitative study drawing on one-to-one interviews. Qualitative methods allow for an in-depth understanding of participant’s thoughts and feeling in a realistic scenario.Citation20 The study was approved by the Cyprus National Bioethics Committee (ΕΕΒΚ ΕΠ 2019.01.131) and informed consent was obtained from all participants.
Context
The data were collected from May to July 2022. In March 2022 the administration of the 3rd dose of the vaccine begun and in April 2022, people aged 60 and above could receive the booster/4th dose. In April 2022, those without a vaccination history had to do a rapid test (72 hours) or a PCR test (72 hours).Citation21
Participants
Purposive snowball sampling was followed, in terms of age and vaccine hesitancy. Participants received a direct invitation via telephone. We aimed to recruit around 15 interviews, as this number is suggested to provide data saturation.Citation22 There is recent evidence that an individual who is hesitant toward COVID-19 vaccines is generally of younger age.Citation7,Citation23–25 Therefore, participants were purposively recruited from a range of age groups. Participants were given a pseudonym. Inclusion criteria were: i) 18 years old and above, ii) living in Cyprus and fluent in Greek and iii) with the capacity to provide informed consent.
Screening
Participants were screened using the Vaccine Hesitancy Scale (VHS) which was adapted for adults by Shen et al.Citation26 prior to being invited for an interview (). The VHS was translated and adapted from English to Greek using a standard front and back-translation procedure. The VHS was used to ensure that the sample included participants with a range of attitudes toward COVID-19 vaccines. “Strongly disagree” and “disagree” were the expressions of vaccine hesitancy in questions 1, 2, 3, 4, 6, 7 and 8 and “strongly agree” and “agree” were the expressions of hesitancy in questions 5, 9 and 10. ‘Neither agree nor disagree’ was also perceived as an expression of hesitancy. Participants were categorized as ‘anti-vaccine’ if they expressed vaccine hesitancy in the VHS and were not vaccinated and ‘hesitant’ if they expressed vaccine hesitancy in the VHS and were vaccinated. They were categorized as ‘pro-vaccine’ if they received the vaccine and did not show expressions of vaccine hesitancy in the VHS. Therefore, based on participant responses, they were characterized as hesitant, pro-vaccine, or anti-vaccine toward COVID-19 vaccines. The aim was to have a balance of participants based on their responses to the VHS.
Interview
A semi-structured interview was developed for the purposes of this study (Appendix C). The questions focused on how participants perceived the role of vaccines, what were the factors that made them hesitant pro-vaccine or anti-vaccine, how their environment influenced their decisions and how in return they potentially had influenced their environment. The interview was piloted with three individuals for testing the appropriateness of the questions in terms of addressing the study’s objectives. Each interview lasted approximately 45 minutes.
Procedure
The interviews took place in a quiet room and on arrival, participants were given the consent form and an information sheet to read and sign. They were further provided with a sociodemographic questionnaire, including questions regarding vaccination history (Appendix A). Participants were reimbursed for their time with €20.
Data analysis
Data were analyzed using Thematic Analysis (TA).Citation27 TA allows the interpretation of participants’ thoughts and feelings in a realistic context.Citation27 An attempt was made to take a critical realist epistemological position, allowing analysis to take the data for what it was (be data driven), and considering that people construct their own understanding of the world. Transcripts were both inductively and deductively coded, as they were informed predominantly by the study objectives focusing on social contagion mechanisms (deductive approach), although novel views expressed by participants were also allowed to be captured (inductive approach). The codes are illustrated in Appendix D.
The codes were clustered together and transformed into more analytical sub-themes. The subthemes were then grouped into themes. To ensure credibility, themes and subthemes were discussed and refined between four researchers (CK, APK, PC and NM). Finally, themes were illustrated with relevant extracts from the data set developing a thematic narrative.
Results
Participants
Eleven participants – three females and eight males participated in the study by which point data saturation was reached.Citation22 None of the participants belonged to the same family. Participants ranged between 23–60 years of age. One participant refused to mention her exact age, therefore, the mean and standard deviation were calculated for the rest (Mean age = 36.50, SD = 13.66). Based on responses to VHS, three participants who received the vaccine were defined as being hesitant, three were anti-vaccine and five were pro-vaccine. presents the full demographic characteristics of the participants.
Table 1. Demographics of the participants (proportions may not add up to 100% due to rounding).
Findings from the thematic analysis
The TA that follows refers to the perceived mechanisms of social contagion identified in the study. Before presenting the TA, the attitudes and perceptions of participants regarding the pandemic and the COVID-19 vaccines are briefly presented. Whilst for a minority of participants the pandemic was perceived as a teachable moment to appreciate the simple things, almost all referred to challenges and expressed their desire to return to their ‘normal lives’. Therefore, they perceived the vaccine as a ‘passport to freedom’. However, almost all seemed to worry about the long-term effectiveness of the vaccines and believed that the vaccine is not needed by everyone (i.e., older people may need it more).
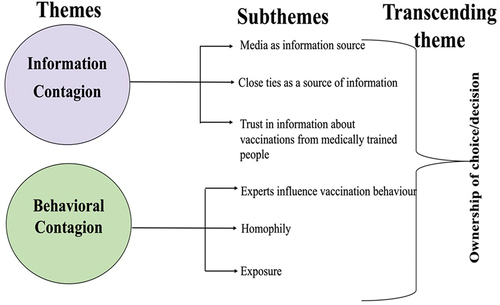
The themes and subthemes identified are organized into a ‘thematic map’ (). Participant’s responses were conceptualized into two general themes on contagion type: 1) Information contagion and 2) Behavior contagion. The transcending theme was the notion of ownership of choice/decision, which pervaded many of the quotes for both types of contagion.
Theme 1: information contagion
The first theme highlights that the information participants received from several sources in their social networks and the processing they did, contributed toward their vaccination decision.
Media as information source
Many used media (i.e., TV) and the internet as sources of information on vaccines (e.g., “Mainly from the internet, social media, Facebook, ‘health news’, newspaper articles etc.” [P3, male, 30 years old, pro-vaccine]). For P6, the statistics/data had an impact on whether he would get the vaccine or not and highlighted that this makes the source and information more credible:
The incentives behind my decision were some statistics I had seen on TV, in commercials. There were doctors talking using statistics … because they were using statistics – they can’t lie. [P6, male, 23 years old, pro-vaccine]
When statistical information is presented especially by experts, participants feel that some truth is imparted. For P10 the side-effects worked as a source of reassurance and justification regarding her decision to stay unvaccinated:
I had found studies on the internet showing the results of vaccinations from the population in Israel, and they had since then presented a lot of problems. Along the way, it appeared in the rest of the countries that they had these problems too, thus I was feeling even better about my decision not to get it! [P10, female, 40–50 years old, anti-vaccine]
For P9, the negative representations justified her choice, in terms of the type of vaccine to get:
I saw a girl on Facebook who got the vaccine and had a blood clot and she posted it and then she died. I was scared. I think she got AstraZeneca and there was no chance for me to get that one.’ [P9, female, 26 years old, hesitant]
However, whilst many relied on the media to get information, P7 stated:
For some, it’s in their best interest to maintain this topic. I am always cautious when it comes to the media, because I know that the media is a very … dirty thing. [P7, male, 33 years old, anti-vaccine]
Close ties as information source
Almost half of the participants evoked that they share information and adopt practices from people they trusted and felt emotionally attached to. Two parents in the sample stated that they had unintentionally influenced their children (20–30 years old):
I believe I influenced my children. If I was strongly against it, I might have influenced them not to get it…. A parent’s opinion counts just because of his or her role as a parent. [P5, female, 56 years old, pro-vaccine]
Some younger participants mentioned that they trusted their parents’ decision to vaccinate because “They would never risk something they weren’t sure about.” [P6, male, 23 years old, pro-vaccine]. P1 said:
When she [his mother] told me “Go get it”, she definitely influenced me. [P1, male, 27 years old, hesitant]
The reason, as he continued saying, is “because you trust your friends and family” highlighting that trust depends on people with whom having a special affinity.
Information contagion was further identified in a sample of coworkers.
They [co-workers] were telling me to get Pfizer because AstraZeneca has side effects. They influenced. When I went to book the vaccine appointment, they told me to get AstraZeneca and I said ‘I’m not getting that.’ Give me Pfizer, otherwise don’t give me any’. [P2, male, 51 years old, pro-vaccine]
He continued saying“I have more intimacy with them,” highlighting why he was being influenced by them.
Unvaccinated participants also mentioned that they mainly discussed with people they considered close to them:
As I discuss everything with my friends and family, we also discussed about the vaccines. It’s easier to discuss with people you know. [P8, male, 29 years old, anti-vaccine]
Trust in information about vaccinations from medically trained people
Participants seemed to also rely for information on medically trained professionals as a source of information. Mostly, to cross-check what they knew and to remain up-to-date.
I asked my General Practitioner (GP) several questions about what I read on the internet, on social media, or the discussions I had with people who had negative views. [P5, female, 56 years old, pro-vaccine]
Confidence and trust were expressed toward healthcare providers (HPs):
It’s their job, they have the knowledge, so you definitely trust them. [P11, male, 60 years old, pro-vaccine]
and they stated that they generally followed what the HPs advised them:
If the doctor tells me I must do that, I’ll do it. [P2, male, 51 years old, pro-vaccine]
Communication from HPs and experts has also positively contributed to their knowledge and decisions:
My friends who are studying Medicine said that it is better to get the vaccine. They sat and read and told me the negatives, the positives and influenced me. [P1, male, 27 years old, hesitant]
P7 mentioned that his cousin who is a microbiologist was his source of information and was reassuring him by telling him “not to worry.” Despite his reliance on him, he seems to distrust the motives of the HPs:
I trust myself. What will the developer tell you? “Go buy property.” Likewise, the doctor will tell you “Get the vaccine!” [P7, male, 33 years old, anti-vaccine]
Participants were exposed to information from the media to enhance their knowledge around vaccinations. However, one anti-vaccine participant mentioned that he does not trust media’s intentions. Contagion was evident through filtering and exchanging information. Most discussed vaccination concerns with people they trust, and this was evident among participants regardless of whether they were hesitant or not toward vaccination. Most of them and particularly those who were hesitant or pro-vaccine discussed vaccination concerns with medically trained individuals. Those who were anti-vaccine, evoked that they avoided discussions on vaccinations, and instead, they trusted themselves.
Theme 2: behavioral contagion
This theme reflects how the vaccination behavior of others had an impact on participants’ vaccination behavior.
Experts influence vaccination behavior
P7 lacks trust toward politicians and seeing them get vaccinated led him to do the opposite:
When the politicians were giving incentives to go and get the vaccine, I said there is 0% chance to get it… I was convinced that I wouldn’t get it … If the politicians tell me something, I’ll do the opposite. You don’t trust them! [P7, male, 33, anti-vaccine]
P10 expanded that politicians are not ‘experts’:
It’s not a political issue for me, it’s a health issue, so journalists and politicians shouldn’t have an opinion and try to convince me. [P10, female, 40–50, anti-vaccine]
On the flip side, for P3 it was HPs who had a negative attitude toward the vaccines that made him skeptical, as they seem to act as “role models” when it comes to vaccination behavior:
We also heard about the nurses being negative and doctors not wanting to get vaccinated … you think about it… ‘he is a doctor, he knows something more than I do. Why doesn’t he get it?’ It makes you think twice about it … . [P3, male, 30, pro-vaccine]
Homophily
Individuals who interact with culturally similar others are exposed to similar attitudes and traits (McPherson, Smith-Lovin & Cook, 2001). Homophily was reflected in the following quote:
A friend of mine asked me whether I would get the vaccine and we discussed the pros and cons. I was closer to deciding to get vaccinated, and I told her, and she said, “me too.” With this girl, we are quite similar in many things. We have known each other since high school and we have common opinions, etc. [P9, female, 26, hesitant]
P9 further expressed that she possibly influenced her friends’ decision:
I think I may have influenced her, without doing it on purpose. She got vaccinated too. [P9, female, 26, hesitant]
Exposure
Vaccination behaviors and preferences may also diffuse within groups. P5 presented a hypothetical scenario to reflect that she would be more skeptical if people from her close environment were against vaccination.
If everyone was against it and the doctor told me to get it, he could make me think twice and three times about getting vaccinated. Because most of my friends got the vaccine, I felt I made a balanced decision. [P5, female, 56, pro-vaccine]
Similarly, P3 said:
I just got it because they all got it before me … my older siblings, my father, my mother … if someone didn’t, maybe it would have affected me. [P3, male, 30, pro-vaccine]
Whilst P10 had greater exposure to anti-vaccine social circle, she said that her choice of not vaccinating was independent of what her social network did:
I had decided from the beginning that I wouldn’t get it and most people I know didn’t get it. [P10, female, 40–50, anti-vaccine]
Participants’ behaviors seemed to be influenced by trust toward the ‘experts’, distrust toward politicians, and the influence of friends and family members with whom they share similar views and attitudes. Exposure to positive attitudes and beliefs toward vaccination contributed to vaccination, whereas more negative views influenced non-vaccination choices.
Transcending Τheme: ownership of choice/decision
Transcending the two themes was the notion of ownership of choice/decision. Participants stated that they wanted to investigate the topic themselves:
Although they [doctors] would give me an opinion, I had to look it up myself. I wouldn’t do whatever they told me. I trust them but up to a point. It was an unknown topic to everyone. [P10, female, 40–50, anti-vaccine]
Similarly, P11 evoked ownership in terms of choosing his sources of information and concluded that he decided for himself:
I was choosing who and what I would listen to. I listened to my doctor and decided for myself. [P11, male, 60, pro-vaccine]
P8 believed in his ability to critically think:
My friends who studied Medicine definitely influenced my thinking, although I think I have critical thinking to think on my own. [P8, male, 29, anti-vaccine]
P2 further took responsibility for his action:
If I don’t get it and I get sick, it’s my fault. [P2, male, 51, pro-vaccine]
Whilst participants relied on various sources of information and their decisions were influenced by external forces, the decision-making process was not perceived as being passive. Instead, there was perceived ownership over the decisions being made, thus participants were reflected as being more active. This transcending theme was apparent in the accounts of almost all participants.
Discussion
This study aimed to understand the perceived social contagion mechanisms of vaccination uptake in the context of COVID-19 pandemic. The strength of ties emerged, as participants evoked that they are inclined to adopt practices from people that they trust and feel emotionally attached to. Also, expertise and knowledge were perceived as important, as individuals tend to evaluate the credibility of the source. Homophily also emerged as two participants were influenced – and they were being influenced by – friends with whom they share similar traits and attitudes. The mechanism of exposure is further evident, since individuals are more likely to get vaccinated if their network includes people who are pro-vaccine. Similarly, negative attitudes are transmitted within networks.
Perceiving the information around COVID-19 vaccines as safe and accurate, depends on the source. Family and friends/peers have more influence on individuals’ attitudes and vaccination uptake than other members of social networks (i.e., HPs and neighbors).Citation1 Also, mothers have a crucial role in transmitting their own health behaviors, beliefs, and values to their children and relevant research reflects that adolescent girls seem to trust their mothers more than their HPs when making decisions about the HPV vaccine.Citation28,Citation29 Similar trends were observed in the data of our study, as younger participants mentioned that they trusted their parents, because they perceived they wouldn’t risk their children’s health. Our study further evokes how family and friends influence vaccination attitudes and uptake. Specifically, trust and intimacy when discussing vaccination concerns with others and to also be influenced by others were influential in decision-making, highlighting that strength of ties strongly influences social contagion.Citation17 This mechanism was evident among almost all participants.
Apart from the factors of trust and intimacy, expertise and knowledge were also mentioned, as participants were influenced by HPs in their COVID-19 vaccination decisions.Citation30 HPs were perceived as credible sources by older and younger participants, who were mainly pro-vaccine and hesitant. However, two of the anti-vaccine participants similarly expressed that, but simultaneously highlighted that they trusted themselves. An anti-vaccine participant seemed to distrust the motives of the HPs, as he was suspicious. Credibility of source is one of the Behavioral Change Techniques (BCTs) in the BCT taxonomy.Citation31 It refers to the present verbal or visual communication from a source deemed as credible which is in favor or against a behavior. Moreover, the BCT refers to the ‘pros and cons’ – when the person is advised to identify and compare the pros and cons of changing their behavior. Some participants compared the pros and cons, in order to reach a decisional balance.
The importance of expertise was also highlighted, as many said that politicians are not ‘experts’, thus they do not trust the politicians and the media.Citation32–34 The 7C model of psychological antecedents to vaccination specifies seven components predicting the likelihood that a person will be willing to receive a vaccine including conspiracy.Citation35 Conspiracy refers to the belief in misinformation and the tendency to endorse conspiratorial beliefs about vaccination. Conspiracy beliefs were reflected in this study – mainly by anti-vaccines – as low belief in vaccination was associated with suspiciousness toward the media and politicians. Also, those participants were unwilling to adhere to public health measures and recommendations.Citation36,Citation37
Homophily was also identified in this study by two participants: a hesitant female and a female who was pro-vaccine. Konstantinou et al.Citation1 suggested that homophily influences the transmission of vaccination attitudes and uptake within social networks. Parents were more likely to vaccinate their child if they were influenced by people having the same race/ethnicity (African Americans, Muslims, Hausa), gender (females), marital status (married), similar educational level (no formal education) and being parents themselves. This study suggests some additional factors to sociodemographics, associating homophily with behavior attitudes and traits, such as sharing common opinions. Behavioral traits (i.e., generosity, trust, etc.) were associated with homophily in previous studies but those studies did not focus on vaccinations – they focused on educational and career paths and included mainly students.Citation38–40
Exposure as a mechanism of contagion was highlighted by three of the total participants; two who were pro-vaccine and an anti-vaccine participant. Those were pro-vaccine, evoked that because they were exposed to positive attitudes and beliefs toward the vaccines, they also decided to get vaccinated.Citation15 A participant who did not receive the vaccine, reflected that negative attitudes and lower vaccination uptake can also be transmitted within networks.Citation1 However, one could argue that social contagion mechanisms may be more complex. For instance, this participant said that her vaccination decision was independent of what her social network did. Therefore, the mechanism of homophily may also be evident, as she might have chosen to cluster with friends with similar vaccination attitudes and behavioral traits (i.e., self-selecting into friendship networks).Citation41
Almost all participants in our study engaged in a comparison and weighing of different opinions, whilst trying to reach certainty about the right vaccination decision. Information about the safety and side effects of the vaccine has a strong impact on a person’s behavior.Citation42–44 Participants’ accounts suggesting the need for increased health literacy through evidence-informed vaccination decision making. Health literacy refers to the skills of individuals to ‘gain access to, understand and use information so that they improve their health’.Citation45 Health literacy may empower people to think critically about information, thus making informed choices. In addition, the Theory of Associative Diffusion suggests that a person firstly interprets another one’s behavior and then evaluates that behavior.Citation9,Citation19 Almost all participants evoked this process of evaluating other’s behavior and information, thus highlighting the notion of ownership of choice/decision. For instance, many tended to use the first person (i.e., “I made the decision”, “I was choosing”). Also, they reflected that they wanted to be informed, without a conscious effort to influence others and even if they may have influenced some people, they were distancing themselves from that.
Strengths & limitations
The main strength of this research is that it used qualitative methods to study participants’ views and experiences regarding COVID-19 vaccines, thus capturing a more realistic, all- rounded perspective. Moreover, the study benefitted from using both vaccinated people as well as unvaccinated, thus enabling an exploration of the differences between the two groups.
However, there are several limitations, including problems with sample representativeness. The sample size was quite small, thus limiting the generalizability of the results. A greater number of participants would enable a more representative sample to be used. The study also included mainly males and people who were vaccinated and all participants were Greek Cypriots living in Cyprus. There may be important cultural differences between Cyprus and other countries, limiting results’ applicability. Also, even though data saturation was reached, it is unclear whether theoretical saturation was achieved (i.e., with a more heterogeneous sample). Social desirability bias may also be a limitation of the study. As vaccination is a personal topic, the participants’ responses may have been affected due to the presence of the interviewer, as to provide responses that they would be better accepted. However, in order to avoid social desirability bias, the researchers framed open-ended questions to encourage participants to express their honest thoughts. Also, the interviewer held an accepting, empathic and open stance toward all the participants. Finally, intercoder reliability – the degree to which independent coders assign similar codes to specific extracts – was not calculated.Citation46
Implications and directions for future research
As participants influenced – and they were being influenced by – friends and family members with whom they have a close relationship of trust and intimacy, clinicians and policymakers could develop and provide educational family-based programs on COVID-19 vaccinations. Also, the interventions and campaigns could include the experts (i.e., HPs giving the statistics), as trust in HPs seems to contribute to higher willingness to get vaccinated and the statistics make the source and information more credible. Health authorities need to provide scientific information to assure people of the COVID-19 vaccine safety. The above suggestions could have a positive impact and thus be used when promoting vaccination uptake beyond the context of COVID-19 as well. However, the COVID-19 pandemic is still an unknown disease and a daily changing situation (i.e., there are novel variants such as Delta etc.) and COVID-19 vaccine was rapidly developed. Therefore, it would be interesting to examine the social contagion mechanisms and any potential differences when it comes to other infectious diseases (i.e., hepatitis, influenza, HIV etc.) and routine vaccinations. Also, considering that it was conducted for a specific period of time, future studies could focus on the long-term sustainability of COVID-19 vaccination behaviors influenced by social contagion.
Longitudinal studies could be conducted in order to study social networks dynamically over time.Citation1,Citation47 Additionally, as Cyprus is a collectivist culture,Citation48 it would also be beneficial to replicate this study with participants from other countries. Based on our study data, there may be benefit in investigating if people from more individualist cultures would reflect the same social contagion mechanisms (i.e., collectivism implies higher tendency to do what is in the best interest of the community regarding vaccination) and if they similarly trust their families when it comes to vaccination decisions.
Conclusion
Participants were mainly exposed to information from the media and the internet and most of them discussed vaccination concerns with the HPs, as they are the most trusted source of information. Study participants further followed HPs advice. Politicians, on the other hand, were not perceived to be ‘experts’, concluding that low vaccine confidence can be driven by a distrust in elites. This is important for deciding on future pandemics the source of messages provided to the people so that they can more easily trust the information provided. Moreover, this study found that during the COVID-19 pandemic individuals were influenced – and they were influenced by – friends and family members with whom they shared similar traits and attitudes (homophily) and shared a close relationship of trust and intimacy (strength of ties). Also, study participants perceived being exposed to positive attitudes and beliefs toward the vaccines, enhancing their own positive vaccination behaviors (exposure). Regarding the behavioral differences between the three groups of participants, anti-vaccines were more suspicious and unwilling to adhere to public health measures and recommendations and avoided discussions on vaccinations. Those who were hesitant and pro-vaccine discussed vaccination concerns with medically trained individuals (i.e., compared the pros and cons). Whilst the Social Contagion Theory mechanisms were evident, this study sheds light on the importance of meaning people give to their world. Specifically, almost all, mentioned that they evaluated other’s behavior and the information they receive, thus demonstrating a sense of a stronger degree of responsibility and agency. Policymakers could consider including social networks of individuals as well as trusted sources (i.e., HPs) when delivering interventions or educational campaigns on vaccinations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data supporting the publication are available after reasonable request to the corresponding author.
Additional information
Funding
References
- Konstantinou P, Georgiou K, Kumar N, Kyprianidou M, Nicolaides C, Karekla M, Kassianos AP. Transmission of vaccination attitudes and uptake based on social contagion theory: a scoping review. Vaccines. 2021 Jun 5;9(6):607. doi:10.3390/vaccines9060607.
- Levy DA, Nail PR. Contagion: a theoretical and empirical review and reconceptualization. Genet Soc Gen Psychol Monogr. 1993;119:233–13.
- Christakis NA, Fowler JH, Sporns O. Social network sensors for early detection of contagious outbreaks. PloS One. 2010 Sep 15;5(9):e12948. doi:10.1371/journal.pone.0012948.
- Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Stat Med. 2013 Feb 20;32(4):556–77. doi:10.1002/sim.5408.
- World Health Organisation. WHO coronavirus dashboard. 2022 [accessed 2023 Jan 22]. https://covid19.who.int.
- Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020 Sep;26:100495. doi:10.1016/j.eclinm.2020.100495.
- Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020 Sep;21(7):977–82. doi:10.1007/s10198-020-01208-6.
- MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–4. doi:10.1016/j.vaccine.2015.04.036.
- Goldberg A, Stein SK. Beyond social contagion: associative diffusion and the emergence of cultural variation. Am Sociol Rev. 2018 Jul 16;83(5):897–932. doi:10.1177/0003122418797576.
- Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011 Nov;101(11):2170–7. doi:10.2105/AJPH.2011.300282.
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007 Jul 26;357(4):370–9. doi:10.1056/NEJMsa066082.
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008 May 22;358(21):2249–58. doi:10.1056/NEJMsa0706154.
- Rosenquist JN, Fowler JH, Christakis NA. Social network determinants of depression. Mol Psychiatry. 2011 Mar;16(3):273–81. doi:10.1038/mp.2010.13.
- Holtz D, Zhao M, Benzell SG, Cao CY, Rahimian MA, Yang J, Allen J, Collis A, Moehring A, Sowrirajan T, et al. Interdependence and the cost of uncoordinated responses to COVID-19. Proc Natl Acad Sci USA. 2020;117(33):19837–43. doi:10.1073/pnas.2009522117.
- Nyhan B, Reifler J, Richey S. The role of social networks in influenza vaccine attitudes and intentions among college students in the Southeastern United States. J Adolesc Health. 2012 Sep;51(3):302–4. doi:10.1016/j.jadohealth.2012.02.014.
- Cowan SK. Secrets and misperceptions: the creation of self-fulfilling illusions. Sociol Sci. 2014 Nov;1:466–92. doi:10.15195/v1.a26.
- Centola D. An experimental study of homophily in the adoption of health behavior. Science. 2011 Dec 2;334(6060):1269–72. doi:10.1126/science.1207055. PMID: 22144624.
- Hargadon AB, Douglas Y. When innovations meet institutions: Edison and the design of the electric light. Adm Sci Q. 2001 Sept;46(3):476–501. doi:10.2307/3094872.
- Goldberg A. Mapping shared understandings using relational class analysis: the case of the cultural omnivore reexamined. AJS. 2011;116:1397–436. doi:10.1086/657976.
- Willig C. Introducing qualitative research in Psychology: adventures in theory and method. 2nd ed. Berkshire, England: Open University Press; 2009.
- COVID-19 Vaccines and Treatment Protocols. Coronavirus. 2022 [accessed 2023 Jan 20]. https://www.pio.gov.cy/coronavirus/eng/categories/vaccines-en.
- Baker S, Edwards R. How many qualitative interviews is enough? Expert voices and early career reflections on sampling and cases in qualitative research. National Centre for Research Methods Review Paper; 2017.
- Kyprianidou M, Konstantinou P, Alvarez-Galvez J, Ceccarelli L, Gruszczyńska E, Mierzejewska-Floreani D, Loumba N, Montagni I, Tavoschi L, Karekla M, et al. Profiling hesitancy to COVID-19 vaccinations in six European countries: behavioral, attitudinal and demographic determinants. Behav Med. 2022 May;11:1–12. doi:10.1080/08964289.2022.2071198.
- Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020 Oct 21;38(45):7002–6. doi:10.1016/j.vaccine.2020.09.041.
- Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. Adults. Ann Intern Med. 2020 Dec 15;173(12):964–73. doi:10.7326/M20-3569.
- Shen X, Dong H, Feng J, Jiang H, Dowling R, Lu Z, Lv C, Gan Y. Assessing the COVID-19 vaccine hesitancy in the Chinese adults using a generalized vaccine hesitancy survey instrument. Hum Vaccin Immunother. 2021 Nov 2;17(11):4005–12. doi:10.1080/21645515.2021.1953343.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa.
- Goodwin PY, Garrett DA. Women and family health: the role of mothers in promoting family and child health. Int J Glob Health And Health Disp. 2005;4:30–42.
- Karafillakis E, Peretti-Watel P, Verger P, Chantler T, Larson HJ. ‘I trust them because my mum trusts them’: exploring the role of trust in HPV vaccination decision-making among adolescent girls and their mothers in France. Vaccine. 2022 Feb 16;40(8):1090–7. doi:10.1016/j.vaccine.2022.01.028.
- Viskupič F, Wiltse DL, Meyer BA. Trust in physicians and trust in government predict COVID-19 vaccine uptake. Soc Sci Q. 2022 May;103(3):509–20. doi:10.1111/ssqu.13147.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013 Aug;46(1):81–95. doi:10.1007/s12160-013-9486-6.
- Pomares TD, Buttenheim AM, Amin AB, Joyce CM, Porter RM, Bednarczyk RA, Omer SB. Association of cognitive biases with human papillomavirus vaccine hesitancy: a cross-sectional study. Hum Vaccin Immunother. 2020 May 3;16(5):1018–23. doi:10.1080/21645515.2019.1698243.
- Frederiksen LSF, Zhang Y, Foged C, Thakur A. The long road toward COVID-19 herd immunity: vaccine platform technologies and mass immunization strategies. Front Immunol. 2020 Jul 21;11:1817. doi:10.3389/fimmu.2020.01817.
- Van Oost P, Yzerbyt V, Schmitz M, Vansteenkiste M, Luminet O, Morbée S, Van den Bergh O, Waterschoot J, Klein O. The relation between conspiracism, government trust, and COVID-19 vaccination intentions: the key role of motivation. Soc Sci Med. 2022 May;301:114926. doi:10.1016/j.socscimed.2022.114926. Epub 2022 Mar 17. PMID: 35344775; PMCID: PMC8928706.
- Geiger M, Rees F, Lilleholt L, Santana AP, Zettler I, Wilhelm O, Betsch C, Böhm R. Measuring the 7Cs of vaccination readiness. Eur J Psychol Assess. 2022;38(4):261–9. doi:10.1027/1015-5759/a000663.
- Constantinou M, Kagialis A, Karekla M. COVID-19 scientific facts vs. Conspiracy theories: is science failing to pass its message? Int J Environ Res Public Health. 2021 Jun 11;18(12):6343. doi:10.3390/ijerph18126343.
- Constantinou M, Gloster AT, Karekla M. I won’t comply because it is a hoax: conspiracy beliefs, lockdown compliance, and the importance of psychological flexibility. J Contextual Behav Sci. 2021 Apr;20:46–51. doi:10.1016/j.jcbs.2021.03.001.
- Kosse F, Tincani MM. Prosociality predicts labor market success around the world. Nat Commun. 2020 Oct 20;11(1):5298. doi:10.1038/s41467-020-19007-1.
- Jackson M, Nei S, Snowberg E, Yariv L. The dynamics of networks and homophily; 2022 Oct 24. doi:10.3386/w30815.
- Bhargava P, Chen DL, Sutter M, Terrier C. Homophily and transmission of behavioral traits in social networks. IZA Discussion Paper No.15840. Institute of Labor Economics (IZA); 2022.
- Rosenquist JN, Murabito J, Fowler JH, Christakis NA. The spread of alcohol consumption behavior in a large social network. Ann Intern Med. 2010 Apr 6;152(7):426–33, W141. doi:10.7326/0003-4819-152-7-201004060-00007.
- Al-Hasan A, Khuntia J, Yim D. Does seeing What others do through social media influence vaccine uptake and help in the herd immunity through vaccination? A cross-sectional analysis. Front Public Health. 2021 Nov 2;9:715931. doi:10.3389/fpubh.2021.715931.
- Wang J, Ji Q, Dong S, Zhao S, Li X, Zhu Q, Long S, Zhang J, Jin H. Factors influencing vaccine hesitancy in China: a qualitative study. Vaccines. 2021 Nov 7;9(11):1291. doi:10.3390/vaccines9111291.
- Lockyer B, Islam S, Rahman A, Dickerson J, Pickett K, Sheldon T, Wright J, McEachan R, Sheard L, The Bradford Institute for Health Research COVID-19 Scientific Advisory Group. Understanding COVID-19 misinformation and vaccine hesitancy in context: findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021;24:1158–67. doi:10.1111/hex.13240.
- Rowlands G. Health literacy. Hum Vaccin Immunother. 2014;10(7):2130–5. doi:10.4161/hv.29603. PMID: 25424830; PMCID: PMC4370358.
- Tinsley HEA, Weiss DJ. Interrater reliability and agreement In: HEA T, Brown S, editors. Handbook of applied multivariate statistics and mathematical modeling. London: Academic Press; 2000. p. 95–124. doi:10.1016/B978-012691360-6/50005-7.
- McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol. 2001;27(1):415–44. doi:10.1146/annurev.soc.27.1.415.
- Zalaf A, Egan V. Cyprus versus UK: cultural differences of attitudes toward animals based on personality and sensational interests. Anthrozoös. 2017 Feb 9;30(1):47–60. doi:10.1080/08927936.2017.1270592.
Appendices Appendix A
Vaccine Hesitancy Scale (VHS) – Adjusted version for adults (Shen et al.Citation26)
Appendix C
Interview guide
Questions:
How do you experience life with COVID?
Are there any challenges?
What are they?
How do you deal with them?
What was the most difficult thing you have encountered and why?
Have you got vaccinated?
When?
What triggered you to do so?
In what ways?
What are the motives/ incentives behind your decision?
Did you have specific thoughts and feelings about a specific vaccine (e.g., Pfizer, AstraZeneca etc.)?
Why?
What were they?
What were your thoughts and feelings about COVID-19 vaccines when you first heard about the vaccine?
Did you experience any negative or positive feelings/thoughts?
What were they?
Did you experience any doubt or concern about the vaccine?
What were they?
Why do you think some people refuse to vaccinate?
What has influenced your negative/ positive attitudes towards vaccinations?
In what ways?
How do you currently feel about COVID-19 vaccines?
What do you think has contributed towards this change? (If they state that their feeling and thoughts changed).
What contributed to lack of change if they didn’t.
What does it mean for you to get vaccinated? For example, why do you think vaccines are needed/ not needed from your point of view?
Why is it important/ not important for you?
How effective do you think vaccines are?
When you hear about a negative story related to vaccinations, what do you do?
Do you ever hear any positive vaccination stories?
What are they?
Who experienced that?
Ηave the vaccination decisions and views of your friends influenced your thoughts and decisions about vaccinations?
In what ways?
Ηave the vaccination decisions and views of your family influenced your thoughts and decisions about vaccinations?
In what ways?
What is the most common information source you turn to for information about vaccines?
Who do you discuss important issues with?
Why?
Do you feel that discussing those issues is helpful?
Who do you trust the most?
Why?
Are you comfortable with discussing your vaccination concerns with your doctor/ healthcare providers?
Why? Why not?
Are you comfortable with discussing your vaccination concerns with people you know?
Why? Why not?
Have you heard or read on social media or media opinions or advice on vaccines?
Who was giving the advice?
What did you hear?
What did they discuss?
How did you feel?
Have you ever talked to people you know about your opinion on COVID-19 vaccinations?
To whom (e.g., friends, family, your doctor, etc.)
What have you discussed?
What did the others say?
How would you describe your communication with other people regarding vaccinations?
Are there any obstacles/ barriers?
Are there any enablers? Is there anything that helps the communication?
Do you feel that you may have an impact on others regarding whether to vaccinate or not?
To whom?
In what ways?
Is there is anything that you would like to add about COVID-19?
Closure: Thank the participant and say some words for using the data collected.